Abstract
Objective: To evaluate the impact of a programme of integrated social and medical care among frail elderly people living in the community.
Design: Randomised study with 1 year follow up.
Setting: Town in northern Italy (Rovereto).
Subjects: 200 older people already receiving conventional community care services.
Intervention: Random allocation to an intervention group receiving integrated social and medical care and case management or to a control group receiving conventional care.
Main outcome measures: Admission to an institution, use and costs of health services, variations in functional status.
Results: Survival analysis showed that admission to hospital or nursing home in the intervention group occurred later and was less common than in controls (hazard ratio 0.69; 95% confidence interval 0.53 to 0.91). Health services were used to the same extent, but control subjects received more frequent home visits by general practitioners. In the intervention group the estimated financial savings were in the order of £1125 ($1800) per year of follow up. The intervention group had improved physical function (activities of daily living score improved by 5.1% v 13.0% loss in controls; P<0.001). Decline of cognitive status (measured by the short portable mental status questionnaire) was also reduced (3.8% v 9.4%; P<0.05).
Conclusion: Integrated social and medical care with case management programmes may provide a cost effective approach to reduce admission to institutions and functional decline in older people living in the community.
Key messages
Responsibility for management of care of elderly people living in the community is poorly defined
Integration of medical and social services together with care management programmes would improve such care in the community
In a comparison of this option with a traditional and fragmented model of community care the integrated care approach reduced admission to institutions and functional decline in frail elderly people living in the community and also reduced costs
Introduction
Improving the ability of health care systems to respond to the demands of older people is among the greatest challenges of our time. Most elderly people, even with considerable disability, prefer to stay at home,1 and hospitals are shortening lengths of stay. Community care has therefore acquired greater relevance.2–6 Responsibility among various health professionals for care management of older people living in the community, however, remains poorly defined, and patients falling between primary and secondary health care and social services are at risk of being forgotten.7 A possible solution may be the integration of medical and social services in a continuum of care with case management programmes.7,8 None the less, the cost effectiveness of this approach remains untested.
We conducted a randomised trial to evaluate the impact of such an integrated programme on admissions to institutions, use and costs of health services, and functional decline among frail elderly people living in the community.
Subjects and methods
During the early 1990s, to comply with the national health plan, the health agency of Rovereto, a town in northern Italy of nearly 35 000, created a broad array of health services for older people. These ranged from a hospital geriatric evaluation unit to a skilled nursing facility and a home health agency. However, no coordination of these components nor integration with social services in the municipality was considered.
Subjects
In 1995 we identified all people aged 65 and over who were recipients of home health services or home assistance programmes (n=224). Usually, patients were receiving these services because of multiple geriatric conditions (for example, dementia, immobility, incontinence, and stroke deficits), but the evaluation preceding care planning was not based on a comprehensive geriatric assessment. Among the total number 24 declined to participate: six were not interested in the project; nine had been advised against it by relatives; and nine had been advised against it by their general practitioner. The remaining subjects were randomly stratified by age and sex according to a computer generated list. One hundred subjects (control group) received primary and community care with the conventional and fragmented organisation of services—that is, general practitioner’s regular ambulatory and home visits, nursing and social services, home aids, and meals on wheels. Another hundred subjects (intervention group) received case management and care planning by the community geriatric evaluation unit and general practitioners. All the services considered necessary were provided in an integrated fashion after a formal agreement between the municipality and the local health agency. Twenty one of 24 general practitioners agreed to participate in the trial and to be involved in care planning, meetings, and emergency situations. Informed consent was obtained from all patients. The study was approved and monitored by the steering committee of the National Research Council’s aging project and the local state authority (Provincia Autonoma of Trento).
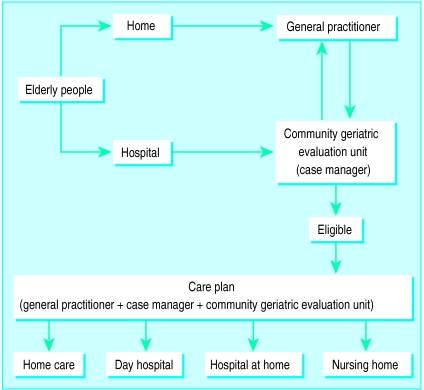
In addition to general practitioners, the community geriatric evaluation unit included a geriatrician, a social worker, and several nurses. All professionals were already employees of the municipality or health agency. Two case managers were selected among the trainees of a course on case management and comprehensive geriatric assessment9 and represented the operational arm of general practitioners and community geriatric evaluation unit (fig 1). Case managers performed the initial assessment soon after randomisation and every 2 months thereafter. Also, they were constantly available to deal with problems, monitor the provision of services, and to guarantee extra help as requested by patients and general practitioners.
Figure 1.
Integrated network of services designed for intervention
Patients were evaluated with a modified version of the British Columbia long term care programme application and assessment form10 in its validated translation.11 Physical function was measured with a six item scale of activities of daily living (ranging from 0 independent to 6 total dependence) and a seven item scale of instrumental activities of daily living (scoring 0 to 7). Cognitive function and mood were assessed with the short portable mental status questionnaire12 and the geriatric depression scale.13 Finally, the assessment included a complete list of diagnoses and drug treatments and the number of home visits provided by general practitioners. Case managers did not perform physical examinations but relied on general practitioners’ evaluation.14 Case managers reported the initial assessment to the geriatric evaluation unit, which determined the services that patients were eligible for and designed and implemented individualised care plans in agreement with general practitioners. The multidisciplinary team discussed problems emerging from home visits during weekly meetings.
Outcomes and expenditure
Main outcomes included admission to an institution, use and related costs of health services, and physical and cognitive function. Information on outcomes such as admission and use of health services was collected every 2 months by a research assistant unaware of patients’ assignments. In the event of admission to hospital or a nursing home patients remained in the study. Vital status was obtained from general practitioners and confirmed by the National Death Registry.
We estimated total expenditures for health services from the average cost per type of service from national official statistics, applying it to the units (days or visits) each individual required. We also considered the annual salary of case managers and the costs of the team work in the intervention group. Other costs, such as the opportunity and direct costs of informal care givers, were not considered.
Subjects in the control group were evaluated with the same assessment instrument only at the beginning and the end of follow up. Baseline and final assessments were performed by national research council staff, previously trained as case managers but not involved in assessment and treatment of the intervention group. A high inter-rater agreement between case managers and research council staff has already been shown.9
Statistical analysis
Quantitative parameters are presented as means (SD). The impact of intervention on functional outcomes was evaluated by analysis of covariance with follow up measures adjusted for baseline values. The impact of the intervention on time to admission to hospital or a nursing home was tested by comparing the survival curves obtained with the Kaplan-Meier method. Differences between curves were evaluated with the log rank test. A P<0.05 level was chosen for significance. Statistical analysis was performed with sas and spss software.
Results
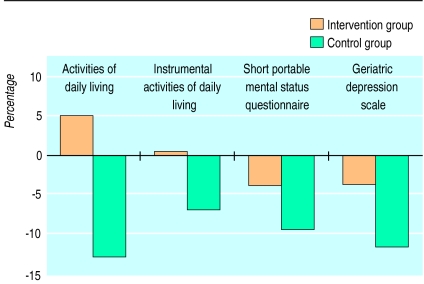
There were no significant differences at baseline in the intervention and control groups across several functional and clinical variables (table 1). No difference in 1 year mortality was observed; 12 subjects in the intervention group died compared with 13 in the control group (hazard ratio 0.99; 95% confidence interval 0.89 to 1.09). Figure 2 shows changes in functional outcomes. In the control group all functional indices deteriorated (activities of daily living −13.0%; instrumental activities of daily living −6.9%; mental status −9.4%; depression −11.8%). In the intervention group less consistent changes were observed (5.1%; unchanged; −3.8%; −4.0%, respectively). Differences between intervention and control groups were all significant (table 2). Also the adjusted mean number of medications was reduced in the intervention group (4.7 (0.2) v 5.4 (0.2); P<0.05).
Table 1.
Baseline characteristics of subjects in intervention and control groups. Figures are numbers of subjects unless stated otherwise
| Characteristic | Intervention (n=99) | Control |
|---|---|---|
| (n=100) | ||
| Mean (SD) age (years) | 80.7 (7.1) | 81.3 (7.4) |
| Women | 70 | 71 |
| Marital status: | ||
| Never married | 20 | 13 |
| Married | 26 | 21 |
| Widowed | 52 | 65 |
| Living alone | 50 | 50 |
| Availability of informal care | 68 | 76 |
| Adequate financial status | 81 | 87 |
| Mean (SD) scores on assessment*: | ||
| Activities of daily living (0-6) | 2.0 (2.1) | 2.3 (2.3) |
| Instrumental activities of daily living (0-7) | 3.8 (2.2) | 4.4 (2.2) |
| Short portable mental status questionnaire (0-10) | 2.7 (3.0) | 3.1 (3.3) |
| Geriatric depression scale (0-30) | 10.1 (5.3) | 11.2 (6.5) |
| Mean (SD) No of medical conditions | 4.7 (2.1) | 4.8 (1.7) |
| Mean (SD) No of medications | 4.5 (2.2) | 4.3 (2.2) |
For all scores higher number indicates greater impairment.
Figure 2.
Percentage change in functional outcomes after 1 year of follow up
Table 2.
Functional outcomes after 1 year of follow up
| Score |
Adjusted mean (SE)*
|
P value | |
|---|---|---|---|
| Intervention | Control | ||
| Activities of daily living | 2.0 (0.1) | 2.6 (0.1) | <0.001 |
| Instrumental activities of daily living | 4.1 (0.1) | 4.4 (0.1) | <0.05 |
| Short portable mental status questionnaire | 2.8 (0.2) | 3.4 (0.2) | <0.05 |
| Geriatric depression scale | 10.9 (0.5) | 12.8 (0.5) | <0.05 |
Means from covariance models adjusted for baseline measures.
The benefit obtained in the intervention group was achieved without increases in use of health services. Use of home support (intervention group 120 (20) v 154 (29) hours/patient/year), nursing care (13 (3) v 12 (3) hours/patient/year), and meals on wheels (54 (12) v 39 (10) meals/patient/year) was not significantly different, although the lack of differences might be due to insufficient sample size. Conversely, more home visits by general practitioners were needed in the control group (10.2 (1.1) v 13.1 (0.8); P=0.04).
Thirty six subjects in the intervention group and 51 in the control group were admitted at least once to acute hospital (P<0.05). The hazard ratio was 0.74 (0.56 to 0.97), while that for visits to an emergency room was 0.64 (0.48 to 0.85) compared with control group (table 3). Furthermore, patients in the control group had a trend toward a higher rate of admission to nursing homes, although this was not significant. The cumulative number of days per year spent in either nursing home (1087 v 2121) or acute hospital (894 v 1376) was reduced by up to half in the intervention group.
Table 3.
Relative risk of being admitted to nursing home, acute hospital, or emergency room during follow up
| Place of admission | Intervention (n=99) | Control (n=100) | Hazard ratio (95% CI) | P value |
|---|---|---|---|---|
| Nursing home | 10 | 15 | 0.81 (0.57 to 1.16) | 0.3 |
| Acute hospital | 36 | 51 | 0.74 (0.56 to 0.97) | <0.05 |
| Nursing home or hospital | 38 | 58 | 0.69 (0.53 to 0.91) | <0.01 |
| Emergency room | 6 | 17 | 0.64 (0.48 to 0.85) | <0.025 |
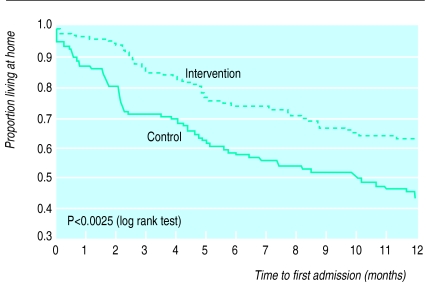
Results of survival analyses on the basis of time to first admission to hospital or nursing home are shown in figure 3. Thirty eight subjects in the intervention group and 58 subjects in the control group were admitted at least once (hazard ratio 0.69; 0.53 to 0.91). Even when subjects in the intervention group entered hospital or nursing homes, they did so later (and less often) than control subjects (P<0.003).
Figure 3.
Proportion of subjects admitted to hospital or nursing home in intervention and control groups
Finally, we calculated total per capita health care costs over the follow up period. The intervention group accounted for 23% less than the control group. The overall saving, after addition of salaries of case managers, was estimated at around £1125 per person per year. Apart from reductions in community health services costs (£744 v £919; −19%), intervention group savings resulted mainly from substantial decreases in nursing home (£644 v £1244; −48%) and hospital expenses (£1763 v £2688; −34%).
Discussion
Our study shows that an integrated community care programme implemented by an interdisciplinary team including a general practitioner and a case manager reduced the risk of hospital admission and length of stay in either hospital or nursing home. Despite a similar use of supportive home care resources, subjects in the intervention group showed less physical and cognitive decline; total health care costs per capita were also reduced.
Some features of our study may explain these results. Firstly, we intensively trained case managers, providing them with case management skills and geriatric assessment technology.9 This determined the ability to design care plans and coordinate all available agencies, thus assuring integrated care.15
Secondly, in our model the community geriatric evaluation unit represented the gatekeeper to health services. This provided a unique community based setting for the referral of patients, regardless of specific needs. Importantly, the role of case managers was to support and integrate the activity of general practitioners who, by law, retained full responsibility of the patient. This is consistent with previous recommendations7 and has been suggested by the public policy committee of the American Geriatrics Society.16
Finally, the close collaboration between case managers, community geriatric evaluation unit, and general practitioners was critical to the success of the intervention; this may determine the effectiveness of any community based programmes.17
Although randomised, our study could not be performed with the rigid criteria of a clinical trial. Because of the nature of the intervention (that is, a change in the provision of care) all the professionals concerned were aware of the assignment of patients to either group. Also, as a consequence of the informed consent, patients and physicians were aware of the ongoing project. Case managers, however, performed the assessment simply as a part of their routine activities; both patients and professionals remained blind about the outcomes under study and the length of follow up. This greatly limited the risk of introducing a bias. Furthermore, differences in functional outcomes collected by case managers were consistent with the objective outcomes based on medical record review (that is, number of medications and admissions to nursing homes and hospital). In this respect, our study is no different from many others of elderly patients.18 Also, general practitioners who followed both control and intervention participants may have introduced a contamination bias, though the ratio of physicians to patients (1:5) rendered a directional bias unlikely. Moreover, the higher number of visits in the control group was inconsistent with less intensive treatment in these patients. We believe that a more critical consideration is that the benefits of an integrated care approach can be achieved only in circumstances where all the parties concerned are sufficiently motivated.
Acknowledgments
We thank F Lattanzio and L Manigrasso for collecting data of the control group. We also thank: L Maffei, L Spagnolli, D Tarter, E Vicentini (Centro ADI-Rovereto); S Chiasera, A Cunial, D Fontanari, B Boninsegna, M Piccolroaz, D Slanzi (Comune di Rovereto); Z Bellotti, U Pitton, M Tomasoni, L Zanella (USL Vallagarina); E Lorenzini, P Giudici (Provincia Autonoma di Trento); F Bernardi, A Pitteri (Ospedale di Rovereto); L Iannielli, E Sfredda, R Tomasini, G Rinoldi (Casa Soggiorno di Rovereto); R Gregori (Cooperativa la Casa); and all general practitioners and staff involved in the project for their countless efforts. The invaluable help of K Lapane in the statistical analysis is also acknowledged.
Footnotes
Funding: Progetto Finalizzato Invecchiamento, National Research Council.
Conflict of interest: None.
References
- 1.Salvage AV, Jones DA, Vetter NJ. Options of people aged over 75 years on private and local authority residential care. Age Ageing. 1989;18:380–386. doi: 10.1093/ageing/18.6.380. [DOI] [PubMed] [Google Scholar]
- 2.Kane RL, Kane RA. Long-term care. JAMA. 1995;273:1690–1691. [PubMed] [Google Scholar]
- 3.Hing E, Bloom B. Long-term care for the functionally dependent elderly. Am J Public Health. 1991;81:223–225. doi: 10.2105/ajph.81.2.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stuck AE, Aronow HU, Steiner A, Alessi CA, Bula C, Gold MN, et al. A trial of annual in-home comprehensive geriatric assessment for elderly people living in the community. N Engl J Med. 1995;333:1184–1189. doi: 10.1056/NEJM199511023331805. [DOI] [PubMed] [Google Scholar]
- 5.Steel K. Home care for the elderly: the new institution. Arch Int Med. 1991;151:439–442. [PubMed] [Google Scholar]
- 6.Coleman BJ. European models of long-term care in the home and community. Int J Health Serv. 1995;25:455–474. doi: 10.2190/FYP6-DLWY-WKKT-6NNJ. [DOI] [PubMed] [Google Scholar]
- 7.Black D, Bowman C. Community institutional care for frail elderly people [editorial] BMJ. 1997;315:441–442. doi: 10.1136/bmj.315.7106.441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Khaw KT. Public health and epidemiology: infrastructure under threat. Lancet. 1997;350:53–54. [Google Scholar]
- 9.Landi F, Sgadari A, Cipriani L, Pahor M, Carbonin PU, Bernabei R. A simple program to train case managers in community elderly care. Aging Clin Exp Res. 1996;8:211–218. doi: 10.1007/BF03339679. [DOI] [PubMed] [Google Scholar]
- 10.Hollander MJ, Pallan P. The British Columbia continuing care system: service delivery and resource planning. Aging Clin Exp Res. 1995;7:94–109. doi: 10.1007/BF03324298. [DOI] [PubMed] [Google Scholar]
- 11.Abate G, Cavoni MA, Bottone L. Validazione di una scheda per l’assistenza domiciliare. In: Antico L, Bernabei R, Carbonin PU, Caretta F, Petrini M, editors. Realtà e prospettive dei sistemi di valutazione dell’anziano nei servizi sociali e sanitari in Italia. Rome: CNR; 1992. pp. 53–97. [Google Scholar]
- 12.Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc. 1975;3:433–441. doi: 10.1111/j.1532-5415.1975.tb00927.x. [DOI] [PubMed] [Google Scholar]
- 13.Yesavage JA, Brink TL, Rose TL. Development and validation of geriatric depression scale. J Psychiatr Res. 1983;17:37–49. doi: 10.1016/0022-3956(82)90033-4. [DOI] [PubMed] [Google Scholar]
- 14.Rubenstein LZ. An overview of comprehensive geriatric assessment: rationale, history, program models, basic components. In: Rubenstein LZ, Wieland D, Bernabei R, editors. Geriatric assessment technology: state of the art. Milan: Kurtis; 1995. pp. 1–4. [Google Scholar]
- 15.Applebaum RA, Wilson NL. Training needs of case managers serving long-term care channelling demonstration. Gerontologist. 1988;28:172–176. doi: 10.1093/geront/28.2.172. [DOI] [PubMed] [Google Scholar]
- 16.American Geriatrics Society Public Policy Committee. Care management. J Am Geriatr Soc. 1991;39:429–430. [PubMed] [Google Scholar]
- 17.Bula CJ, Alessi CA, Aronow HU, Yuhas K, Gold M, Nisenbaum R, et al. Community physicians’ cooperation with a program of in-home comprehensive geriatric assessment. J Am Geriatr Soc. 1995;43:1016–1020. doi: 10.1111/j.1532-5415.1995.tb05566.x. [DOI] [PubMed] [Google Scholar]
- 18.Black N. Why we need observational studies to evaluate the effectiveness of health care. BMJ. 1996;312:1215–1218. doi: 10.1136/bmj.312.7040.1215. [DOI] [PMC free article] [PubMed] [Google Scholar]