Abstract
Background/Objective:
Tilt and recline variable position seating systems are most commonly used for pressure relief to decrease potential for skin breakdown. This study provides quantitative information on the magnitudes of loading on the seat and back during phases of tilt, recline, and standing. The objective of this study was to show that the amount of force reduction at the seat would differ across these 3 methods within their respective clinical ranges.
Participants:
Six able-bodied (AB) subjects (2 men, 4 women) with a median age of 25 years, and 10 subjects (8 men, 2 women) with spinal cord injury (SCI) with a median age of 35.5 years.
Methods:
Subjects sat on a power wheelchair with Tekscan pressure mats placed underneath a foam backrest and cushion. Data were collected at 5 positions for each method. Order of position and method tested were randomized. Linear regressions were used to calculate the relationships of normalized seat and backrest forces to seat and backrest angles for each chair configuration.
Results:
Normalized seat loads had strong linear relationships with the angles of change in tilt, recline, and standing for both groups. Maximum decreases in seat load occurred at full standing and full recline in the SCI subjects and in full standing in the AB subjects. Loads linearly increased on the back during tilt and recline and linearly decreased during standing for both groups.
Conclusions:
Standing and recline offered similar seat load reductions at their respective terminal positions. Standing also reduced loading on the backrest. Recognizing that each method had clinical benefits and drawbacks, the results of this study indicate that tilt, recline, and standing systems should be considered as a means of weight shifting for wheelchair users.
Keywords: Wheelchair, design; Spinal cord injuries; Seating systems; Pressure ulcer; Prevention
INTRODUCTION
The development of pressure ulcers is a constant concern for people with limited mobility and/or altered sensation. People with spinal cord injuries (SCIs) are at high risk of skin breakdown because both limited mobility and sensation are commonly associated with such injuries. Researchers have estimated that 50% to 85% of individuals with SCI will develop a pressure ulcer in their lifetime (1–3). Annual treatment costs in the United States for pressure ulcers in this population are approximately 1.3 billion, accounting for 25% of the total cost of medical care after SCI (4). The lower part of the body accounts for 95% of pressure ulcer occurrence (5). Most common areas of skin breakdown for people with SCI are over bony prominences, such as the sacrum, ischial tuberosities, and heels (6). Thus, during rehabilitation, people with SCIs are taught preventative weight shifts, or pressure reliefs, to relieve pressure off of the buttocks while seated to minimize the potential for skin breakdown. If a person is physically able, a lift, forward lean, or side-to-side weight shift can be routinely performed. However, when upper extremity or trunk weakness, spasticity, joint limitations, or other physical conditions prevent a person from physically performing adequate weight shifts consistently throughout the day, a variable position seating system is one option that may be recommended.
Variable position systems include tilt, recline, and standing. As they progress through their ranges of movement, pressure relief occurs as body weight is supported on surfaces other than the buttocks (eg, back, feet). Each type of system has benefits and limitations. Powered or manual tilt and/or recline are the commonly prescribed systems for people who are unable to independently perform pressure reliefs.
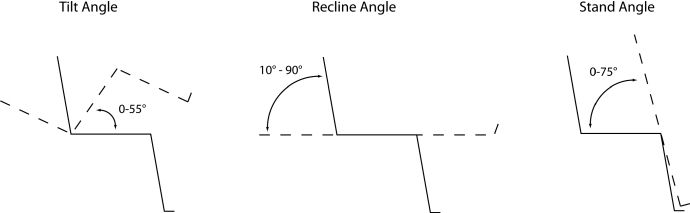
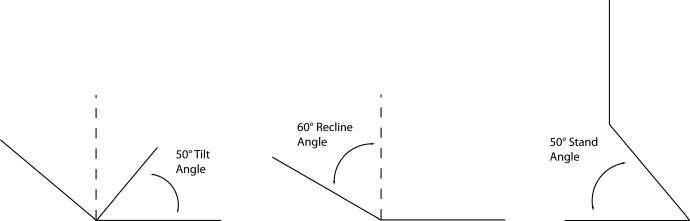
Tilt systems maintain constant hip and knee angles while tilting the whole system rearward (Figure 1). The intent of a tilt system is to redistribute body weight from the seat in upright sitting to the backrest in a tilted position. Most tilt systems rotate rearward to achieve a seat angle of 45° to 60° from the horizontal. People who have trouble tolerating static joint positions (hip/knee) throughout the day or those who have difficulty with bladder drainage while tilted may not tolerate this method of variable position. Tilting reduces the frictional forces at the seat interface (7) and permits consistent positioning and switch access throughout the range of movement.
Figure 1.
Tilt, recline, and stand angle configurations.
Recline systems move the person from a sitting position to nearly supine position by opening the seat-to-back angle and elevating the footrests (Figure 1). The intent is to redistribute body weight from the seat to the backrest and leg rests. Recline systems have an added benefit of assisting with bladder drainage and management. However, some people cannot use a recline system for pressure relief because of increased spasticity during recline (8). The increased shear forces (7) or postural displacement (9) that occur when opening the seat to back angle can lead to shear stresses, which is a risk factor for the development of pressure ulcers (10–12). Change in posture during reclining can impair switch access and interfere with postural support placement. Combination tilt and recline systems are also available and may address some of the issues stated above.
Manual or power stand systems are also commercially available. Standing systems transition a person from a seated position into a semistanding position and some permit wheelchair mobility in the standing position (Figure 1). Typically, standing systems are used to perform activities of daily living and/or school- and work-related activities. In the United States, standing systems have not typically been prescribed as a means of redistributing pressure off of the buttocks, although intuitively, this type of postural change should provide similar weight shift as recline and tilt.
Several studies have characterized the changes in seat pressure and/or force during tilt and recline. Aissaoui et al (9) studied pressure distribution and sliding on 10 able-bodied (AB) subjects assuming 12 postures on a simulator chair. The system tilt angle ranged from 0° to 45° of posterior tilt, and the back angle (recline) varied from 90° to 120°. A flat foam cushion was used on the seat and back, and 2 force sensing arrays (Vista Medical, Winnipeg, Manitoba, Canada) measured the interface pressure at the seat and back. Mean pressure, peak pressure, and peak pressure gradient was calculated for all positions. A 40.2% maximum reduction in peak pressure under the ischial tuberosities were found at a tilt of 45° and a recline of 120°.
Using a Tekscan F-Scan system (Tekscan, Boston, MA) to measure interface pressure, Henderson et al (13) evaluated 3 measures to relieve pressure in 10 subjects with SCI. Subjects were tested in their own chairs and cushions. A 27% decrease in maximum pressure over the ischial tuberosities was observed with a 35° tilt, a 47% reduction with a 65° tilt, and a 78% reduction with a forward lean weight shift.
Hobson (7) studied the effects of seated postures, body orientation, and presence of injury on pressure distribution and shear with 10 AB subjects and 12 subjects with SCI. The subjects sat on the same test chair and flat foam cushion. An Oxford pressure monitor (Talley Group Ltd, Ramsey, Hants., UK) was used to collect pressure data at the body–seat interface. Average pressure, maximum pressure, and peak pressure gradient data were collected. Forward and lateral trunk flexion, 110° and 120° back recline, and 10° and 20° system tilt were evaluated. A 12% reduction in maximum pressures occurred with 120° recline, and an 11% reduction was found with 20° of system tilt. Shear forces increased, respectively, by 7% and 25% at 110° and 120° of backrest recline. Extrapolation of Hobson's data suggested that tilting to approximately 25° reduces shear to near 0.
Burns and Betz (14) studied seated pressures under the ischial tuberosities of 16 subjects with SCI sitting in their own wheelchairs on 3 different cushions (dry flotation, fluid, and dynamic) in an upright position and at 45° degrees of tilt (dry flotation and fluid only). The Tekscan Clinseat pressure sensor (Tekscan, Boston, MA) placed between the subject and cushion was used to collect data. A 33% reduction in pressures at the ischial tuberosities was found on both the dry flotation and fluid cushion at 45° of tilt.
The studies mentioned above used interface pressure mapping to investigate effects of seated pressure on tilt and recline combinations. The studies used different pressure mapping systems, different subject types, simulators vs personal wheelchairs, varying cushions, and varying isolated degrees of tilt and/or recline and therefore are difficult to compare. Despite these differences, the studies found that increasing the angle of tilt and recline or combination of both will increase the redistribution of pressure off the buttocks. To date, no studies have measured the changes in loads on the seat during full ranges of tilt, recline, and standing using the same cohort of subjects.
This study investigated the redistribution of load at the seat and backrest during phases of tilt, recline, and standing. The study hypothesis was that the amount of force reduction at the seat would differ across these 3 methods within their respective clinical ranges. This study will provide quantitative information on the magnitudes of loading on the body across clinical ranges of tilt, recline, and standing. As a secondary analysis, the rates of seat unloading were compared between AB persons and those with SCI.
METHODS
Subjects
A convenience sample of 6 AB subjects and 10 subjects with SCI were included in the study. The AB subjects were recruited from students and employees at a university. The subjects with SCI were recruited from a SCI outpatient program at a rehabilitation hospital. Because of the test wheelchair seat depth limitations, inclusion criteria included a height above 160 cm (5 feet, 3 in). Subjects with SCI were medically cleared with a physician's consent before participation in the study. Subjects with insufficient range of motion, presence of pressure ulcers limiting sitting/standing times, or other medical contraindications to passive tilt, recline, or standing were excluded from the study. All subjects reviewed and signed an informed consent approved by the university's and hospital's Research Review Committees.
The ages of AB subjects (2 men, 4 women) averaged 29 ± 9.1 (SD) years, and the mean age of the SCI subjects (8 men, 2 women) was 36.9 ± 14.7 years. Time since injury averaged 12.9 ± 14.5 months, and the levels of injury ranged from C4 to T12 and included levels A to D of the ASIA impairment scale. The mean mass of AB subjects was 65.5 ± 8.2 kg, and the mean mass of the subjects with SCI was 77.8 ± 11.5 kg. t test analysis indicated that the ages of both groups were not different (P = 0.25) but that SCI subjects with SCI had greater body mass (P = 0.04). One AB subject originally identified for the study was excluded because of the height requirement.
Instrumentation
At the time of the study, no wheelchair existed that could achieve full clinical ranges of tilt, recline, and stand. To standardize all support surfaces and seat and backrest articulations, we decided to use a single seating system to compare variable positioning methods. Therefore, a Levo Combi power wheelchair (Levo USA, Brooklyn Park, MN) that reclined from 0° to 180° and permitted up to 75° of stand was used for the study. The wheelchair base was secured to an external tilt frame, and the wheelchair and frame were tilted together from 0° to 55° (Figure 2). The range of angles for each configuration was based on the available systems on the market. The upright position was set with a 0° seat angle and a 100° seat-to-back angle, relative to the horizontal. A 1-in flat foam cushion was placed over the wooden backrest, and a 2-in flat foam seat cushion was used.
Figure 2.

External tilt frame.
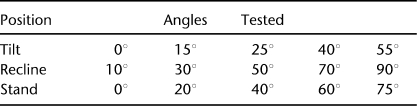
Data were collected at 5 different angles, including upright, for each of the 3 different configurations (ie, tilt, recline, and stand; Table 1). Tilt and standing angles were measured from the horizontal axis to the seat (Figure 1). Recline angles were measured from a vertical axis to the backrest (Figure 1).
Table 1.
Angles Tested Per Configuration
Two sensor mats (CONFORMAT 5315QL; TEKSCAN, Boston, MA) were used to record force data. The 5315QL mats were selected for the study because they allow simultaneous calibration and data collection. Each mat contains a grid of 42 × 48 sensors with a maximum possible active area of 42.7 × 48.8 cm. The mats were calibrated before each subject's data collection. Because the mats were being used as a force scale, they could be placed under the backrest and seat cushions because forces above and below the cushions are equal. This position allowed the subjects to maintain a consistent and typical interface with the seat and backrest cushions. Testing during protocol development confirmed that no difference in force was measured when mats were simultaneously placed atop and below the cushion.
Procedures
Subject seat depth and lower leg length were measured, and the wheelchair seat was adjusted to the correct dimensions accordingly. The subjects were transferred to the power wheelchair with assistance as needed. Subjects were seated with their sacrum against the backrest and their arms across their chest. A lap belt and chest strap were secured for each subject. The order of data collection was randomized across variable positioning methods and angles within each method. An investigator changed positions for each configuration while subjects were asked to sit passively. Data were collected after subjects were positioned for 1 minute at each angle (15,16). The mats were unweighted between position changes to minimize potential creep effects of the mat and cushion. Subjects were provided assistance in unweighting as necessary.
Data Analysis
Force on the mats was calculated by multiplying total mat pressure by total mat area. For each subject, the recorded seat and backrest forces were normalized using the highest load obtained within a given configuration (tilt, recline, or stand). This normalization provided a common means for comparison of relative load for each subject regardless of their weight.
Linear regressions were used to calculate the relationships of normalized seat and backrest forces (% of maximum load) to the angle of tilt, recline, and stand. The slope of the regression line is reported to reflect the rate of loading change per angle. A general linear model was configured to compare seat forces across subject type and angle within and across configurations. Statistical significance was defined at the P = 0.05 level.
RESULTS
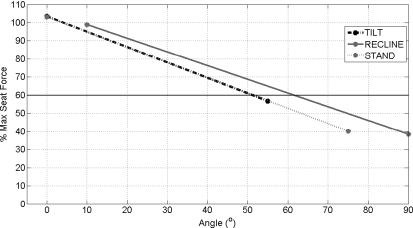
Seat Forces
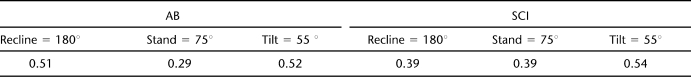
The rates of seat unloading as indicated by the slopes of the regression are shown in Figure 3. The normalized seat loads were linearly related to the angles of tilt, recline, and standing with R2 values exceeding 90% in all configurations for SCI subjects and 78% for AB subjects (Table 2). The unloading slopes were significantly different (P = 0.002), but the only significant paired difference using repeated measures analysis found recline to be less than standing (P = 0.045; Table 2). Rates of unloading were greater for SCI subjects compared with AB subjects (P = 0.003). The greater range of the standing and recline maneuvers resulted in a greater unweighting of the seat surface compared with tilt (P = 0.000). In both groups, full standing (seat angle = 75°) and recline (backrest angle at 90°) resulted in greater unloading than full tilt (seat angle = 55°). Maximum unloading in the SCI group occurred in full standing and recline, whereas standing offered the greatest unweighting in the AB group (Table 3).
Figure 3.
Rate of loading change per angle of seat forces for subjects with SCI.
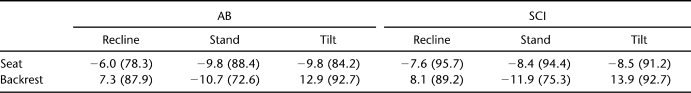
Table 2.
Regression Slopes Presented as Rate of Loading Change per Angle (R2)
Table 3.
Normalized Seat Forces at Terminal Positions
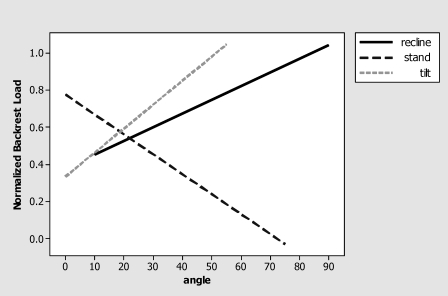
Backrest Forces
The results of loading on the back also followed a linear relationship for both groups in tilt, recline, and standing (Table 2). As expected, tilt and recline resulted in a linear increase of backrest force, whereas the standing maneuver linearly decreased load on the backrest (Figure 4). Each configuration had a significantly different slope (P = 0.000), meaning that the rate of change in backrest force differed across configuration. The slopes of the regression lines were similar across subject types (P = 0.38).
Figure 4.
Rate of loading change per angle of back forces for subjects with SCI.
DISCUSSION
This study provided a comprehensive picture of changes in loading on the body during transitions from an upright seated position into tilt, recline, and standing. Not surprisingly, loads decreased on the seat with increasing amounts of tilt, recline, and stand. As expected, the rate of increased loading on the backrest was higher with tilt than recline (Table 2). Standing was the only configuration that decreased loads off of the seat and backrest simultaneously (Figures 3 and 4).
When recommending a variable position seating system to people with SCI, clinicians consider pressure relief as well as practical and functional concerns. With respect to pressure relief, both the rate of redistribution (amount of unweighting per angle change) and the maximum buttock unloading are considered.
Analysis supported the hypothesis that seat forces at the respective terminal positions differ. For SCI subjects, a 46% decrease in seat load was found at full tilt with 61% decreases in full recline and stand. Standing and recline, with ranges of 75° and 90°, respectively, have a larger range of travel than the 55° of tilt; therefore, it is not surprising that those 2 systems result in a larger decrease in seat load at the terminal positions than tilt. Figure 3 graphically shows the respective changes in seat forces. To reduce seat forces to 60% of maximum, a person would have to tilt to 50°, stand to 50°, or recline the backrest to 60°. These analogous positions are shown in Figure 5.
Figure 5.
Tilt, recline, and stand positions to reduce maximum seat force to 60%.
Power tilt and recline are most commonly prescribed to permit independent weight shifts. As stated earlier, both of these methods have benefits and drawbacks. Fully reclining the backrest offloaded the seat 15 percentage points more than tilting the seat to 55°. Combination tilt and recline units are also available so may offer different load redistribution capabilities but were not a part of this study.
Some wheelchair users may be at risk of skin breakdown at sites contacting both the seat and backrest. Only standing unloaded both of these contact surfaces so it can be considered if this need presents. However, standing requires a change in posture and the resultant shear has not been adequately studied. Nevertheless, based on the results of this study, evaluation for a standing feature can be justified for wheelchair users at risk for skin breakdown. In addition, performing a standing maneuver as a weight shift may be more socially accepted and requires less space than a full tilt or recline, for example, in school or work settings. Standing also provides a functional position from which to continue daily activities while unloading the seat and back, unlike terminal tilt and recline positions.
The slopes differed for AB compared with SCI subjects, indicating that load redistribution differed across these 2 groups. These findings are generally consistent with other studies that identified differences in interface pressures between SCI and AB subject populations (17–19). The high linearity of the responses means that no threshold point (eg, 45° of tilt) beyond which the load dropped dramatically occurred in any of the 3 variable positioning methods. Thus, the results cannot be used to define an “effective” tilt, recline, or stand pressure relief. Determining how much of a weight shift is needed to prevent the onset of pressure ulcers is difficult and well beyond the scope of this study.
This study measured forces on the seat and backrest during variable positioning maneuvers. This obviates the ability to use the results to track pressure changes at specific body locations and limits the ability to precisely compare results from studies that measured interface pressures. The decision to report force changes was made to insure reliable measurement and to avoid any interaction between the presence of an interface mat and the redistribution of load throughout the respected ranges of positioning. Because force on the seat and backrest is independent of cushion type, these results are able to generalize across cushions. Because only normal force was measured, the impact of friction and shear was not quantified. Measuring the amount of shear during each position change would have provided a fuller picture of the potential impacts of each system on the buttocks and back.
Because no wheelchair could sequence through all configurations, we had to choose between the use of a single wheelchair and an external tilt mechanism and the use of multiple wheelchairs. We chose to use a single Levo wheelchair to insure a consistent body support interface over all configurations and angles. The use of an external tilt frame did not alter the relationship between the line of gravity and the support surface compared with tilting seating systems. Commercial recline and standing devices differ in system articulation. Therefore, some difference in how weight is shifted may occur over their respective ranges.
This article reported a difference in redistribution of seat forces within SCI vs AB subjects. Normalized forces were used to accommodate difference in individual's body mass and posture. Therefore, the fact that the SCI subjects were heavier than AB subjects was not addressed in the analysis. If force normalization was impacted by group differences in mass, generalization of the results would be impacted.
CONCLUSION
Tilt and recline are common methods of weight shifts among wheelchair users. This study investigated the magnitude of load redistribution during tilt, recline, and stand, and results concur with that in the previous literature that load reduction off of the buttocks occurs as the angle of tilt or recline increases. Standing and recline reduced load on the seat to 40% of load in an erect position with tilt reducing load to 55% of maximum. Standing also reduced loading on the backrest. The results indicate that tilt, recline, and standing may be considered as options to shift body weight off the seat surface.
REFERENCES
- Richardson RR, Meyer PR., Jr Prevalence and incidence of pressure sores in acute spinal cord injuries. Paraplegia. 1981;19(4):235–247. doi: 10.1038/sc.1981.47. [DOI] [PubMed] [Google Scholar]
- Salzberg CA, Byrne DW, Cayten CG, van Niewerburgh P, Murphy JG, Viehbeck M. A new pressure ulcer risk assessment scale for individuals with spinal cord injury. Am J Phys Med Rehabil. 1996;75(2):96–104. doi: 10.1097/00002060-199603000-00004. [DOI] [PubMed] [Google Scholar]
- Young KC, Railton R, Harrower AD, Brookes RW. Transcutaneous oxygen tension measurements as a method of assessing peripheral vascular disease. Clin Phys Physiol Meas. 1981;2(2):147–151. doi: 10.1088/0143-0815/2/2/007. [DOI] [PubMed] [Google Scholar]
- Byrne DW, Salzberg CA. Major risk factors for pressure ulcers in the spinal cord disabled: a literature review. Spinal Cord. 1996;34(5):255–263. doi: 10.1038/sc.1996.46. [DOI] [PubMed] [Google Scholar]
- Thomas DR. Prevention and treatment of pressure ulcers: what works? what doesn't. Cleve Clin J Med. 2001;68(8):704–707. 710–714, 717–722. doi: 10.3949/ccjm.68.8.704. [DOI] [PubMed] [Google Scholar]
- National Spinal Cord Injury Statistical Center. The 2006 NSCISC Statistical Annual Report for the Model Spinal Cord Injury Care Systems. Birmingham, AL: National Spinal Cord Injury Statistical Center, University of Alabama; 2006. [Google Scholar]
- Hobson DA. Comparative effects of posture on pressure and shear at the body-seat interface. J Rehabil Res Dev. 1992;29(4):21–31. doi: 10.1682/jrrd.1992.10.0021. [DOI] [PubMed] [Google Scholar]
- Sprigle S, Sposato B. Physiologic effects and design considerations of tilt-and-recline wheelchairs. Orthop Phys Ther Clin N Am. 1997;6(1):99–121. [Google Scholar]
- Aissaoui R, Lacoste M, Dansereau J. Analysis of sliding and pressure distribution during a repositioning of persons in a simulator chair. IEEE Trans Neural Syst Rehabil Eng. 2001;9(2):215–224. doi: 10.1109/7333.928581. [DOI] [PubMed] [Google Scholar]
- Bennett L, Lee BY. Pressure versus shear in pressure sore causation. In: Lee BY, editor. Chronic Ulcers of the Skin. New York: McGraw Hill; 1985. pp. 39–56. [Google Scholar]
- Bennett L, Patel H. Transferring load to flesh: part IX. Cushion stiffness effects. Bull Prosthet Res. 1979;10–31:14–37. [PubMed] [Google Scholar]
- Goldstein B, Sanders J. Skin response to repetitive mechanical stress: a new experimental model in pig. Arch Phys Med Rehabil. 1998;79(3):265–272. doi: 10.1016/s0003-9993(98)90005-3. [DOI] [PubMed] [Google Scholar]
- Henderson JL, Price SH, Brandstater ME, Mandac BR. Efficacy of three measures to relieve pressure in seated persons with spinal cord injury. Arch Phys Med Rehabil. 1994;75(5):535–539. [PubMed] [Google Scholar]
- Burns SP, Betz KL. Seating pressures with conventional and dynamic wheelchair cushions in tetraplegia. Arch Phys Med Rehabil. 1999;80(5):566–571. doi: 10.1016/s0003-9993(99)90201-0. [DOI] [PubMed] [Google Scholar]
- Stinson M, Porter A, Eakin P. Measuring interface pressure: a laboratory-based investigation into the effects of repositioning and sitting. Am J Occup Ther. 2002;56(2):185–190. doi: 10.5014/ajot.56.2.185. [DOI] [PubMed] [Google Scholar]
- Maurer CL, Sprigle S. Effect of seat inclination on seated pressures of individuals with spinal cord injury. Phys Ther. 2004;84(3):255–261. [PubMed] [Google Scholar]
- Aissaoui R, Kauffmann C, Dansereau J, de Guise JA. Analysis of pressure distribution at the body-seat interface in able-bodied and paraplegic subjects using a deformable active contour algorithm. Med Eng Phys. 2001;23(6):359–367. doi: 10.1016/s1350-4533(01)00052-2. [DOI] [PubMed] [Google Scholar]
- Sprigle S, Chung KC, Brubaker CE. Reduction of sitting pressures with custom contoured cushions. J Rehabil Res Dev. 1990;27(2):135–140. doi: 10.1682/jrrd.1990.04.0135. [DOI] [PubMed] [Google Scholar]
- Swain I, Peters E. Evaluation Report MDA/97/20. Salisbury, UK: Medical Devices Agency; 1997. The effects of posture, body mass index and wheelchair adjustment on interface pressure; pp. 29–31. [Google Scholar]