Abstract
Objectives. We evaluated the quality of snacks and beverages served at YMCA after-school programs before and after the programs' participation in a YMCA Learning Collaborative.
Methods. We collected data on the types and brands of snacks and beverages (including fresh fruits and vegetables, whole grains, foods with trans fats, water, and sugar-sweetened beverages) served daily during 3 different time periods spanning 14 months in total, and the components of the healthy eating standards. We compared snack and beverage quality before and after the intervention.
Results. Weekly servings of fresh fruits and vegetables (1.3 vs 3.9; P = .02) and weekly servings of fruits and vegetables as a whole (1.9 vs 5.2; P = .009) increased from baseline to postintervention; weekly servings of desserts (1.3 vs 0.5; P = .049), foods with added sugars (3.9 vs 2.4; P = .03), and foods containing trans fats (2.6 vs 0.7; P = .01) decreased. After the intervention, all YMCAs offered water daily, and none served sugar-sweetened beverages. The percentage of calories from fruits and vegetables significantly increased after the intervention, whereas the percentage of calories from foods containing trans fats and added sugars decreased.
Conclusions. A learning collaborative can disseminate healthy eating standards among participating organizations and facilitate improvements in the quality of after-school snacks and beverages.
Although after-school programs can influence children's food intake and physical activity, they have been underused in efforts to improve dietary patterns and reduce obesity risk. After-school programs serve approximately 6.5 million children in the United States each year,1 a disproportionate number of whom are from low-income, Hispanic, or African American households,2 which are at higher than average risk for obesity.3
Evidence suggests that children's dietary patterns contribute to energy imbalances. Approximately 17% of US children aged 6 to 11 years are obese (i.e., above the 95th percentile with respect to body mass index [BMI; defined as weight in kilograms divided by height in meters squared]).4 Recent research indicates that excess weight gain may reflect daily sustained energy imbalances of 110 to 165 calories among children and youths.5 In addition, children's dietary quality is suboptimal, characterized by inadequate consumption of fruits and vegetables6,7 and excessive consumption of sugar-sweetened beverages,8–10 sweets, sweetened grains,9 and trans fats.11 Increasing children's fruit, vegetable, and fiber consumption and decreasing their intake of sugar-sweetened beverages, low-nutrient-density foods, and trans fat would improve their dietary quality and help protect them against obesity and chronic disease risk.12–18
After-school programs offer approximately 3 hours of programming each day and typically provide snacks and drinks on site. Because snacks represent 24% of children's total daily energy intake19 and childhood dietary habits often carry over into adolescence and adulthood,20–23 the quality and types of snacks served at after-school programs deserve serious attention.
Very few descriptive studies, however, have focused on the quality or types of snacks and beverages served at after-school programs.24 Although 4 studies, to our knowledge, have tested environmental after-school interventions, these studies did not specify what foods were served.25–28 The results of a fifth policy intervention study showed improvements in fruit but not vegetable offerings.29 We evaluated evidence of improvements in the quality of snacks and beverages served in 7 YMCA after-school programs participating in an organizational change intervention.
METHODS
The YMCA is the nation's largest private, nonprofit provider of early and school-age child care. An estimated 400 000 children attend approximately 10 000 YMCA after-school programs nationwide. In 2005, 14 after-school programs from 9 YMCAs in 7 states began participation in a YMCA Learning Collaborative (YLC). The YLC was an organizational change initiative that, among other aims, focused on improving the quality of snacks and beverages served. The after-school programs were located in public schools and staffed by YMCA employees.
We performed baseline (fall 2005), midperiod (spring 2006), and post-YLC (fall 2006) assessments with each program serving as its own control. Our primary hypothesis was that the quality of snack menus, as defined by the Environmental Standards for Healthy Eating30 (hereafter “healthy eating standards”), would improve post-YLC relative to baseline. The primary study contrast was between menu data collected at baseline and after the YLC intervention. We also present midperiod data to illustrate progress toward the goals of the standards.
In our primary analysis, we examined 7 after-school programs at 5 YMCAs located in 5 states with complete baseline, midperiod, and post-YLC data. Of the 14 original sites, we excluded 1 that closed during baseline and 2 that did not provide data according to our protocol. Four other sites that provided only baseline and midperiod data were included in a subanalysis assessing whether there was bias with respect to reporting compliance.
Intervention
The YLC was a multifaceted organizational change initiative managed by a national team affiliated with the YMCA. The YLC design was based on the Breakthrough Series learning collaboratives, developed by the Institute for Healthcare Improvement to help health care workers identify performance gaps and implement evidence-based, cost-effective improvements.31 YMCA of the USA developed program practice goals for the collaborative, and participating YMCAs used the Breakthrough Series model to work toward these goals in an intensive, yearlong process that included engaging the target audience, devising and evaluating small tests (“experiments”) of process changes, and integrating successful experiments into standard practices.
The key YLC processes have been described in detail elsewhere.32 During the preintervention phase, YLC coordinators helped interested YMCAs assess their readiness for YLC participation. Subsequently, 9 YMCAs signed on and committed to the YLC goals, including the healthy eating standards, articulated in a charter and change package (a document outlining the ideal vision of the YMCAs' role in reaching out to those in the community who want to adapt healthy habits and specific changes).
The after-school component of the YLC aimed to integrate health promotion and enhanced communication practices into existing programs. Specific health promotion goals were to foster physical activity and promote healthy eating among children by changing program practices. We evaluated the implementation of 5 YLC-specified healthy eating standards: (1) offering fresh fruit or vegetable options daily, (2) not serving foods with trans fats, (3) offering water as the primary beverage daily, (4) not serving sugar-sweetened beverages, and (5) serving more whole grains instead of processed grains (including cookies and desserts). YMCAs were further advised to offer 100% juice and low-fat or skim milk 2 or 3 times each per week.
These standards, adapted from guidelines developed by the Harvard Health Prevention Research Center, were grounded in current scientific evidence about healthy diets.30 Their goal was to improve overall snack quality through implementation of relatively simple changes. The intervention also specified social contextual supports, including role modeling by staff, child involvement in food preparation and cleanup, and parent engagement; we did not evaluate these program components in this analysis.
The YLC held 3 learning sessions (each 2 or 3 days in length) to facilitate expert-to-staff and staff-to-staff learning in several areas (e.g., the improvement model and charter and change package content, peer experiences in experimentation and data-driven decision making, monitoring of progress, and team development). Local YMCA executive staff, including association and branch managers, attended all 3 learning sessions (which took place in December 2005, March 2006, and September 2006); YMCA after-school program site directors attended the second and third sessions. These YMCA representatives were expected to engage their local staff members with respect to implementing charter and change packet processes and the healthy eating standards at their home sites.
Classification of After-School Snacks and Beverages
YMCA staff were asked to use a standardized data collection spreadsheet to record snack and beverage menus for each day throughout the 2005–2006 school year and the first half of the 2006–2007 school year. These detailed daily menu reports were submitted electronically to the researchers each month. The menu reports included information on specific food types and brands served; whether fruits and vegetables were fresh, canned, dried, or frozen; and types of milk, juice, and water served.
Beverages were classified into 1 of 4 categories: water or noncaloric seltzer water, 100% fruit juice, sugar-sweetened beverages (e.g., non-100% juices, powdered drink mixes, punch), or milk (reduced-fat, low-fat, or skim white milk; no other milk types were served). Programs were instructed to report serving water if it was served at the snack table but not if it was available only from a water fountain.
Foods were classified into major and low-nutrient-density groups.33,34 Major food groups were fruits and vegetables (fresh, frozen, canned, dried), grains (e.g., breads, cereals, tortillas), dairy foods (e.g., yogurt, cheese), and meats, beans, and nuts (e.g., nonprocessed meats, dry or canned beans, peanut butter). Grains were subcategorized into higher (2.5 grams of fiber or more per serving)35 and lower (less than 2.5 grams of fiber per serving) fiber grains. We used higher fiber grains as a proxy for “whole grains” in our analyses. Whole grains may contribute to health through sources other than fiber (e.g., vitamins, minerals36), but the major objectives of the whole-grain recommendation were to promote fiber consumption and reduce consumption of processed grains.
Low–nutrient-density food groups were salty snacks (e.g., pretzels, crackers, tortilla chips, snack mixes), desserts (e.g., cookies, pies, snack cakes, cereal bars, granola bars), sweeteners (e.g., candy, flavored ice pops, jam), and added “visible” fats (e.g., butter, salad dressing, mayonnaise). Mixed dishes (but not individual foods) were classified into more than 1 food group (e.g., quesadillas were classified as both grain and dairy).
Nutrient Analysis
For each food type and brand, nutrient and ingredient information was obtained from product or grocery store37 Web sites or from digital photographs of package labels if information was unavailable online. In the case of generic items or unreported brands, nutrient information was obtained from the US Department of Agriculture (USDA) Nutrient Database38; data from similar brand-name foods were used to determine the presence of partially hydrogenated oils and added sugars.
When food types were not detailed (e.g., “fruit,” “crackers”), the average of the 3 most frequently served types of that food among all 7 YMCA after-school sites was assigned (e.g., values for “crackers” were averages of Ritz, Saltines, and Wheat Thins). For a few foods without brand or USDA nutrient data (e.g., “vegetarian beans”), we obtained nutrient information from top-selling similar brands on the grocery store Web site.37 Data for mixed foods (e.g., burritos, pizza) were obtained from the USDA database or individual components of simple mixed foods (e.g., peanut butter and jelly sandwich); if information was unavailable from either of these sources, we gathered it from a Web site on which the USDA database is used to calculate the nutrient content of various recipes (e.g., tuna casserole).39
Foods were defined as containing trans fats if their ingredients included partially hydrogenated oil. Foods and beverages were defined as containing added sugar if a caloric sweetener (e.g., corn syrup, brown sugar) was among the first 3 ingredients. Serving sizes were as specified on product or grocery Web sites or food labels, or (in the case of data obtained from the USDA database or recipe Web sites) they were assigned according to USDA's food guide pyramid.40
Statistical Analysis
The baseline assessment period comprised the first 9 weeks of the 2005–2006 school year, before the first learning session. Midperiod follow-up occurred after the second learning session and included the final 9 weeks of the 2005–2006 school year. Post-YLC follow-up included the 9 weeks after the third learning session in the fall of the 2006–2007 school year. We obtained data on 30 to 45 days of snack menus per site for each 9-week time period (totaling 258, 283, and 307 days for the baseline period, midperiod, and post-YLC period, respectively); data on 90% of possible days were reported across the 3 periods. Missing data typically reflected after-school program closings for holidays and vacations (accounting for 48 days across all sites and periods); however, there were 18 days on which staff members did not report snack and beverage data and 32 days on which they did not clearly specify what snack was served (i.e., “potluck” or “leftovers”).
We calculated average servings per week for each food and beverage group and estimated daily averages for calories and fiber content. We estimated servings per week of specific food groups at each site by calculating servings per day and standardizing these data to a 5-day school week. For example, we summed all servings of fruits for site 1 at baseline, divided by the number of days of available data, and multiplied by 5 to estimate standardized servings per week. We assessed the reliability of these measures using intraclass correlation across sites for the averages of the food and beverage components of the healthy eating standards and calories.41 Estimated reliabilities were 0.47 for higher fiber grains, 0.97 for snacks containing trans fat, 0.98 for fresh fruits and vegetables, 0.99 for sugar-sweetened beverages, 0.99 for total calories, and 1.00 for water.
Our primary comparison was between baseline and post-YLC snack and beverage quality; we compared the baseline period and midperiod to determine progress. We used paired t tests to assess the statistical significance of changes in serving frequency and nutrient content between baseline and each follow-up. Study site zip codes were used to derived community demographic data from US census tables.42 We used SAS version 9.0 (SAS Institute Inc, Cary, NC) in conducting all of our analyses.
RESULTS
Baseline site characteristics are shown in Table 1. Programs served an estimated 445 children from kindergarten through 8th grade. The average median family income among these children exceeded the US average. At baseline, each site had achieved at least 1 of the healthy eating standards: 4 served water as the primary beverage daily, 6 did not serve sugar-sweetened beverages, and 1 served a fresh fruit or vegetable daily.
TABLE 1.
Baseline Characteristics of After-School Program Sites: 7 YMCA Learning Collaborative (YLC) sites, United States, 2005–2006
| Grades of Attendees | Maximum Enrollmenta | % White Children Aged 5–14 Years in Zip Code of Site Locationb | Median Annual Household Income in Zip Code of Site Location,c $ | No. of Snack Days Analyzed |
Healthy Eating Standards Achieved at Baseline | ||||
| Site Location | Baseline | Mid-Period | Post-YLC Period | Total | |||||
| Ann Arbor, MI | 1–4 | 45 | 77 | 61 809 | 44 | 43 | 43 | 130 | Water served daily, SSBs not served |
| Boise, ID | K–1 | 60 | 90 | 36 536 | 45 | 43 | 39 | 127 | SSBs not served |
| St. Louis, MO (1) | K–6 | 20 | 98 | 48 394 | 44 | 39 | 31 | 114 | SSBs not served |
| St. Louis, MO (2) | K–6 | 20 | 98 | 48 394 | 44 | 32 | 30 | 106 | SSBs not served |
| Rochester, NY (1) | K–6 | 30 | 92 | 59 192 | 45 | 45 | 43 | 133 | Water served daily, SSBs not served, fresh fruit or vegetables served daily |
| Rochester, NY (2) | K–6 | 90 | 91 | 51 888 | 42 | 36 | 37 | 115 | Water served daily |
| Suffolk, VA | K–8 | 180 | 40 | 35 211 | 43 | 45 | 35 | 123 | Water served daily, SSBs not served |
| Total | 445 | 84d | 48 775d | 307 | 283 | 258 | 848 | ||
Note. SSB = sugar-sweetened beverage.
Estimated average size of each daily after-school program.
Zip code data derived from 2000 census; 61.3% of US children aged 5–14 years are White.
Zip code data derived from 2000 census; the 2000 annual median household income in the United States was $41 994.
Average value.
Specific data for snacks and beverages served at each time period are shown in Table 2. Mean baseline weekly servings of water (2.9), fresh fruits and vegetables (1.3), and higher fiber grains (our proxy for whole grains; 0.2) were low relative to the healthy eating standards. Conversely, snacks containing trans fats were served relatively frequently (2.6 servings per week on average). Number of servings of sugar-sweetened beverages (0.4 per week) was low, nearly achieving the standard. The average number of servings of 100% fruit juice (3.2 per week) exceeded the recommended 2 to 3 servings per week, whereas the number of servings of low-fat milk (1.2 per week) fell short of that recommendation.
TABLE 2.
Average Baseline and Postintervention Snack and Beverage Servings per Week: 7 YMCA Learning Collaborative (YLC) sites, United States, 2005–2006
| No. of Servings/Weeka at Baseline, Mean (SD) | No. of Servings/Weeka Post-YLC, Mean (SD) | Mean Change in No. of Servings/Week | Post-YLC vs Baseline Pb | |
| Beverages | ||||
| Water | 2.9 (2.7) | 5.0 (0.0) | 2.1 | .08 |
| 100% fruit juice | 3.2 (2.4) | 1.8 (2.4) | −1.4 | .26 |
| Sugar-sweetened beverages | 0.4 (0.9) | 0.0 (0.0) | −0.4 | .36 |
| Low-fat milk | 1.2 (2.1) | 1.8 (2.4) | 0.6 | .18 |
| Major food groups | ||||
| Fruits and vegetables | 1.9 (2.2) | 5.2 (1.8) | 3.3 | .009 |
| Fruits | 1.2 (1.6) | 3.2 (1.4) | 2.0 | .02 |
| Vegetables | 0.7 (0.6) | 1.9 (1.3) | 1.2 | .048 |
| Fresh fruits/vegetables | 1.3 (1.8) | 3.9 (1.8) | 2.6 | .02 |
| Dried, canned, frozen | 0.6 (0.6) | 1.3 (0.8) | 0.7 | .14 |
| Grains | 1.4 (0.7) | 1.3 (0.4) | −0.1 | .93 |
| Higher fiber grains | 0.2 (0.2) | 0.4 (0.3) | 0.2 | .25 |
| Lower fiber grains | 1.2 (0.7) | 1.0 (0.2) | −0.2 | .45 |
| Meats, beans, nuts | 0.5 (0.5) | 0.8 (0.3) | 0.3 | .17 |
| Dairy foods | 0.8 (1.0) | 1.0 (0.3) | 0.2 | .47 |
| Low–nutrient-density foods | ||||
| Desserts | 1.3 (1.0) | 0.5 (0.4) | −0.8 | .049 |
| Salty snacks | 2.1 (2.1) | 1.2 (0.5) | −0.9 | .33 |
| Sweeteners | 0.3 (0.3) | 0.2 (0.3) | −0.1 | .87 |
| Visible fats | 0.2 (0.3) | 0.5 (0.5) | 0.3 | .31 |
| Foods with trans fats or added sugars | ||||
| Foods with trans fats | 2.6 (1.5) | 0.7 (0.3) | −1.9 | .01 |
| Foods with added sugars | 3.9 (1.1) | 2.4 (1.1) | −1.5 | .03 |
| Foods other than fruit with added sugars | 3.7 (1.0) | 2.0 (0.9) | −1.7 | .007 |
Standardized to 5 after-school days.
P values reflect differences from paired t tests.
The most frequently served foods at baseline were salty snacks (2.1 servings per week on average), desserts (1.3 servings per week), fresh fruits and vegetables (1.3 servings per week), and lower fiber grains (1.2 servings per week). Although not a food group, snacks with added sugars (including fruit canned in syrup) were served frequently (3.9 times per week).
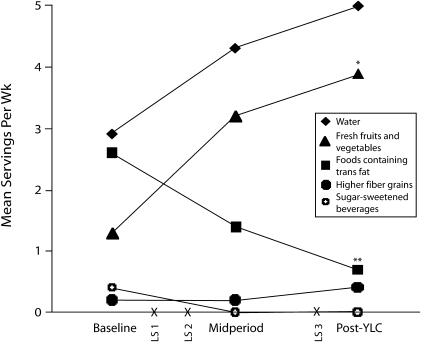
Significant improvements were observed in most food and beverage targets for the healthy eating standards, major food groups, and low-nutrient-density foods from baseline to post-YLC. There were marked increases in servings of fresh fruits and vegetables (from 1.3 to 3.9 servings per week; P = .02), and servings of snacks containing trans fat decreased significantly (from 2.6 to 0.7 servings per week; P = .01). Progress toward 4 food and beverage targets of the healthy eating standards clearly followed site exposure to the YLC (Figure 1). In addition to improvements in components of the healthy eating standards, the total number of fruit and vegetable servings (including canned and frozen) increased substantially (from 1.9 to 5.2 servings per week; P = .009); moreover, there were significant individual increases in both servings of fruit (from 1.2 to 3.2 servings per week; P = .02) and servings of vegetables (0.7 to 1.9 servings per week; P = .048).
FIGURE 1.
Across-period changes in average servings of snack and beverage components of the healthy eating standards: 7 YMCA Learning Collaborative (YLC) sites, United States, 2005–2006.
Note. LS = learning session.
*P < .05; **P = .01.
In the case of low–nutrient-density foods, baseline to post-YLC declines were observed for desserts (from 1.3 to 0.5 servings per week; P = .049) and foods with added sugars (from 3.9 to 2.4 servings per week; P = .03). When fruits prepared with added sugars were excluded, there was a more substantial decline in servings of these foods from 3.7 to 2.0 servings per week (P = .007). All sites had eliminated sugar-sweetened beverages by midperiod and maintained this target through the post-YLC period (P = .36), and each site was serving water as a primary beverage each day by the post-YLC period (P = .08); however, these improvements did not achieve statistical significance.
Snacks and beverages contained an average of 300.3 kcal (SD = 104.4) at baseline and 266.9 kcal post-YLC (SD = 123.3; P = .27), a decrease that was not statistically significant (Table 3). Daily snack and beverage profiles improved from baseline to post-YLC with respect to calorie quality and dietary fiber content. There were increases from baseline to post-YLC in the percentages of daily snack and beverage calories derived from total servings of fruits and vegetables (from 7.6% to 22.7%; P = .01) and from servings of fresh fruits and vegetables (from 4.7% to 15.6%; P = .01).
TABLE 3.
Average Baseline and Postintervention Daily Calorie Contributions of Snacks and Beverages: 7 YMCA Learning Collaborative (YLC) sites, United States, 2005–2006
| Baseline Daily Calories, Mean (SD) | Post-YLC Daily Calories, Mean (SD) | Mean Calorie Change/Day | Post-YLC vs Baseline Pa | Contribution to Total Snack and Beverage Calories at Baseline, % | Contribution to Total Snack and Beverage Calories Post-YLC, % | |
| Total | 300.3 (104.4) | 266.9 (123.3) | −33.0 | .27 | … | … |
| Beverages, major food groups, and low–nutrient-density foods | ||||||
| 100% juice | 81.1 (61.6) | 44.0 (56.7) | −37.1 | .23 | 27.0 | 16.5 |
| Total fruits/vegetables | 22.7 (28.5) | 60.6 (22.9) | 37.9 | .01 | 7.6 | 22.7 |
| Fresh fruits/vegetables | 14.2 (21.7) | 41.8 (26.5) | 27.6 | .01 | 4.7 | 15.6 |
| Salty snacks | 50.7 (53.1) | 26.2 (11.7) | −24.5 | .31 | 16.9 | 9.8 |
| Desserts | 35.8 (27.6) | 12.7 (10.8) | −23.1 | .05 | 11.9 | 4.8 |
| Foods with trans fats or added sugars | ||||||
| Foods with trans fats | 64.9 (40.2) | 16.4 (5.8) | −48.5 | .02 | 21.6 | 6.1 |
| Foods with added sugars | 102.3 (27.1) | 67.0 (33.9) | −35.0 | .03 | 34.1 | 25.1 |
| Foods other than fruit with added sugars | 97.4 (21.9) | 57.6 (26.1) | −39.8 | .003 | 32.5 | 21.6 |
Note. All calorie values are kilocalories. Percentages do not sum to 100% because mixed foods were placed into more than 1 category.
P values reflect differences from paired t tests.
Conversely, the percentage of calories from desserts declined (from 11.9% to 4.8%; P = .05). Calorie contributions from foods containing trans fats (P = .02) and foods with added sugars (P = .03) also declined. When fruits with added sugars were excluded, the proportion of calories from foods with added sugars declined even more substantially (P = .003). Average daily dietary fiber content increased (reflecting the increases in servings of fruits and vegetables) from 2.0 g (SD = 1.3) to 3.5 g (SD = 1.4; P = .01; data not shown). Progress toward the healthy eating standards varied across and within after-school program sites according to outcome. All 7 sites achieved or sustained at least 1 of the standards.
During the YLC intervention, 2 after-school programs participated in another health promotion intervention (CATCH Kids Club)25 with overlapping goals that emphasized serving fruits, vegetables, and whole grains. Average improvements in servings of fruits, vegetables, and whole grains at these sites were not significantly different from improvements at other after-school program sites (data not shown; P > .05 for all).
Of the 11 original sites, 4 did not submit snack menus post-YLC. As a check for reporting bias, we reanalyzed baseline and midperiod results comparing the 4 sites with 1 follow-up and the 7 sites with 2 follow-ups. There was no evidence that changes in servings of snacks and beverages differed systematically in these 2 groups.
DISCUSSION
Snacks served at after-school programs provide a critical nutrition bridge between lunch and dinner for millions of American children, yet little is known about their quality. In this study, we documented that the quality of snacks and beverages served by after-school programs improved during and after their participation in a learning collaborative. All 7 study sites achieved 2 healthy eating standards post-YLC: offering water as a primary beverage each day and not serving sugar-sweetened beverages. Safe and clean tap water is an inexpensive option for keeping children hydrated as well as decreasing their consumption of empty calories from sugar-sweetened beverages, yet tap water has not been a focused recommendation for after-school programs.43
Significant improvements were observed with respect to increasing servings of fresh fruits and vegetables and decreasing servings of foods containing trans fats. Progress toward increasing servings of whole grains and decreasing servings of processed grains was not evident. It may be that sites were not certain how to choose products that met the definition of whole grain. This lack of progress may also have reflected our measurement standards; we defined higher fiber grains as those with 2.5 g of fiber or more per serving, whereas some whole-grain foods do not meet this threshold (e.g., whole-grain cereals with 1.5 g of dietary fiber per serving). Relative to baseline values, total fruit and vegetable servings increased post-YLC, whereas dessert servings decreased significantly.
Our baseline data indicated that snacks and beverages served in after-school programs merit closer scrutiny owing to their potential impact on children's diets in terms of nutritional quality and energy balance. Fruits and vegetables were served less than twice per week, whereas low–nutrient-density foods (salty snacks, desserts, and foods containing trans fats or added sugars) were served frequently. Consistent with our findings, a recent descriptive study in 1 state showed that the carbohydrate content of after-school program snacks was often high and that fruits and vegetables were served infrequently.24
Dietary risks associated with consumption of low–nutrient-density foods include higher energy intake and lower intake of foods from major food groups.18 Trans fats increase the risk of coronary heart disease44 and diabetes.45 Foods with added sugars are associated with dental caries,46–48 and high levels of consumption of such foods may compromise micronutrient intakes.49–51 In our study, the estimated calorie content of snacks and beverages was 300.3 kcal per day at baseline, with standard deviations suggesting that some menus approached 400 kcal daily. Children aged 6 to 11 years consume an average of 243 kcal per snacking occasion,19 and energy imbalances underlie obesity development; thus, an empirically derived ceiling on calories per snacking occasion may make sense but would require additional research.
Average servings of low-fat dairy beverages, important for bone growth52,53 and potentially obesity prevention,54,55 were low at our YMCA study sites. Sugar-sweetened beverages, associated with weight gain and obesity,16,56–58 were rarely served at baseline and apparently were easily eliminated from sites' snack menus.
Follow-up data suggested that participation in the YLC facilitated after-school programs' progress toward increasing total fruit and vegetable servings as well as servings of fresh fruits and vegetables. Fresh fruits and vegetables were the most frequently served snack post-YLC. Total fruit and vegetable servings numbered more than 5 per week post-YLC, accompanied by significant increases in dietary fiber.
Increasing fruit, vegetable, and fiber intake may reduce children's risk of obesity,59–62 possibly by enhancing satiety63 and substituting for higher calorie foods with little nutritional value.64 However, US children aged 4 to 13 years consume an average of only 2.3 to 2.6 servings per day of fruits and nonstarchy vegetables,65 far below the USDA minimum recommendation of 5 to 8 servings.66 Although the standard was for fresh fruits or vegetables, a broader guideline for minimally processed canned, frozen, or dried products may be more easily attainable with little nutritional compromise. Decreases in foods containing trans fats and low–nutrient-density foods accompanied increases in servings of fruits and vegetables.
Snack quality improved post-YLC relative to baseline, as evidenced by the significantly increased proportion of calories from fruits and vegetables and the decreased proportion of calories from foods containing trans fats and added sugars. In addition, a sizable decrease in calories from desserts approached statistical significance. Shifting toward an increase in caloric contributions from healthier foods helps improve children's overall dietary patterns.
Strengths and Limitations
Our study had a number of notable strengths. For example, the multiple days of menu data provided reliable measures of the healthy eating standard components and calories; reliability assessments for these measures averaged 0.90. Our baseline data consisted of an average of 44 days over 7 sites, a robust assessment of preintervention menus. Also, we collected information on brand-name snacks and beverages, enabling us to capture variations in food composition.
Methodological limitations of the study need to be considered. For instance, we did not select a random sample of after-school sites overall or of YMCA after-school programs; this was an observational study of sites participating in a broader intervention. Furthermore, because of the absence of a control group, we cannot exclude the possibility that factors other than participation in the YLC led to the improvements observed. Influences from the media, parents, or community may have been influential at all after-school program sites. Nonetheless, the changes measured were consistent with the healthy eating standards, and there was temporal congruence from baseline to midperiod and post-YLC, suggesting that the YLC was probably a key driver of change.
Other limitations include the fact that we did not systematically validate menu reports, and item substitutions may have occurred. Also, the methods we used to impute missing information on food brands and types may have introduced error. We obtained trans fat and nutrient data between May 2006 and April 2007 and applied the same values to snacks and beverages at all time periods. We lacked data on changes in manufacturer food composition that occurred during the intervention. Some formulations may have changed because of modifications to trans-fat labeling laws in January 2006, and thus more products potentially contained trans fats at baseline. If so, we may have underestimated the reductions that occurred during the intervention.
Finally, we evaluated the snacks and beverages served as opposed to what children actually consumed. Although children are more likely to consume foods that are available and accessible,67 this distinction must be kept in mind when interpreting our findings.
Conclusions
Despite these limitations, our study is a unique contribution to the sparse literature on snack and beverage quality in after-school programs. To our knowledge, no descriptive data have been published on the quality or types of snacks served in these programs. Furthermore, intervention studies focusing on after-school programs have not evaluated specific snacks and beverages served before and after the intervention,25–28 and in 1 study improvements were observed only in fruit offerings.29 Our findings suggest that participation in a learning collaborative with specific attention devoted to assessing and aiming for relatively simple healthy eating standards in after-school food environments may lead to overall improvements in snack and beverage quality.
Additional studies involving broader samples of after-school programs within and outside of YMCA programs are needed to provide an enhanced understanding of snack and beverage quality. After-school programs operate under a range of programmatic and regulatory guidelines with varying attention to nutrition standards. Some guidelines provide virtually no specificity; for example, the National AfterSchool Association's accreditation standards simply require that programs serve “healthy foods.”68 Others, such as those of the USDA Child and Adult Care Food Program,69 are more explicit about food patterns but do not provide guidance on specific foods and beverages that should be served or avoided on the basis of their nutritional quality. In light of the childhood obesity epidemic and the possible contribution of children's dietary patterns to energy imbalances,70 our findings suggest that attention to promoting healthy eating standards in after-school programs is warranted and feasible.
Acknowledgments
Evaluation activities were supported by gifts to the Harvard School of Public Health from the Pritzker Foundation and the Pritzker Traubert Family Foundation, by a contract with YMCA of the USA, and by a cooperative agreement from the Centers for Disease Control and Prevention (U48/DP00064).
We are indebted to YMCA Learning Collaborative Management Team members Lynne Vaughan, Jerry Glashagle, Tom Horsley, Tracy Muckey, John Noland, and Carrie Phelps, who did not participate in the development of this article. We are grateful to all of the YMCA staff members who assisted with snack menu data collection. We express thanks and gratitude to the following individuals for their work and dedication: Teresa Wood-Adams, Treasure Valley Family YMCA; Laura Fasano, YMCA of Greater Rochester; the Ann Arbor YMCA staff; Lynn Skeele-Flynn, YMCA of South Hampton Roads; Rick Matthews, Suffolk YMCA; Mary L. Kampschroeder, Four Rivers Area Family YMCA; and all of the YMCA staff who participated in the YMCA Learning Collaborative. Jeff Hansen of the Harvard School of Public Health (HSPH) contributed to the analysis, and Jessica Barrett of HSPH reviewed the SAS code.
Note. The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Human Participant Protection
No protocol approval was needed for this study.
References
- 1.Afterschool Alliance America After 3 PM: executive summary. Available at: http://www.afterschoolalliance.org/documents/AA%203%20pm_Executive_Summary.pdf. Accessed August 29, 2009
- 2.Carver PR, Iruka IU, Chapman C. National Household Education Surveys Program of 2005: After-School Programs and Activities Washington, DC: National Center for Education Statistics; 2006 [Google Scholar]
- 3.Health 2006, With Chartbook on Trends in the Health of Americans Hyattsville, MD: National Center for Health Statistics; 2006 [PubMed] [Google Scholar]
- 4.Ogden CL, Carroll MD, Flegal KM. High body mass index for age among US children and adolescents, 2003–2006. JAMA 2008;299:2401–2405 [DOI] [PubMed] [Google Scholar]
- 5.Wang YC, Gortmaker SL, Sobol AM, Kuntz KM. Estimating the energy gap among US children: a counterfactual approach. Pediatrics 2006;118:e1721–e1733 [DOI] [PubMed] [Google Scholar]
- 6.Munoz KA, Krebs-Smith SM, Ballard-Barbash R, Cleveland LE. Food intakes of US children and adolescents compared with recommendations. Pediatrics 1997;100:323–329 [DOI] [PubMed] [Google Scholar]
- 7.Brady LM, Lindquist CH, Herd SL, Goran MI. Comparison of children's dietary intake patterns with US dietary guidelines. Br J Nutr 2000;84:361–367 [PubMed] [Google Scholar]
- 8.Nielsen SJ, Popkin BM. Changes in beverage intake between 1977 and 2001. Am J Prev Med 2004;27:205–210 [DOI] [PubMed] [Google Scholar]
- 9.Guthrie JF, Morton JF. Food sources of added sweeteners in the diets of Americans. J Am Diet Assoc 2000;100:43–48, 51 [DOI] [PubMed] [Google Scholar]
- 10.Wang YC, Bleich SN, Gortmaker SL. Increasing caloric contribution from sugar-sweetened beverages and 100% fruit juices among US children and adolescents, 1988–2004. Pediatrics 2008;121:e1604–e1614 [DOI] [PubMed] [Google Scholar]
- 11.Allison DB, Egan SK, Barraj LM, Caughman C, Infante M, Heimbach JT. Estimated intakes of trans-fatty and other fatty acids in the US population. J Am Diet Assoc 1999;99:166–174 [DOI] [PubMed] [Google Scholar]
- 12.American Dietetic Association Fruit and vegetable intake and childhood overweight. Available at: http://www.adaevidencelibrary.com/topic.cfm?cat=1054. Accessed August 29, 2009
- 13.Patrick K, Norman GJ, Calfas KJ, et al. Diet, physical activity, and sedentary behaviors as risk factors for overweight in adolescence. Arch Pediatr Adolesc Med 2004;158:385–390 [DOI] [PubMed] [Google Scholar]
- 14.Hanley AJ, Harris SB, Gittelsohn J, Wolever TM, Saksvig B, Zinman B. Overweight among children and adolescents in a Native Canadian community: prevalence and associated factors. Am J Clin Nutr 2000;71:693–700 [DOI] [PubMed] [Google Scholar]
- 15.Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics 2007;120(suppl 4):S164–S192 [DOI] [PubMed] [Google Scholar]
- 16.Ludwig DS, Peterson KE, Gortmaker SL. Relation between consumption of sugar-sweetened drinks and childhood obesity: a prospective, observational analysis. Lancet 2001;357:505–508 [DOI] [PubMed] [Google Scholar]
- 17.Malik VS, Schulze MB, Hu FB. Intake of sugar-sweetened beverages and weight gain: a systematic review. Am J Clin Nutr 2006;84:274–288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kant AK. Reported consumption of low-nutrient-density foods by American children and adolescents: nutritional and health correlates, NHANES III, 1988 to 1994. Arch Pediatr Adolesc Med 2003;157:789–796 [DOI] [PubMed] [Google Scholar]
- 19.Jahns L, Siega-Riz AM, Popkin BM. The increasing prevalence of snacking among US children from 1977 to 1996. J Pediatr 2001;138:493–498 [DOI] [PubMed] [Google Scholar]
- 20.Lien N, Lytle LA, Klepp KI. Stability in consumption of fruit, vegetables, and sugary foods in a cohort from age 14 to age 21. Prev Med 2001;33:217–226 [DOI] [PubMed] [Google Scholar]
- 21.te Velde SJ, Twisk JW, Brug J. Tracking of fruit and vegetable consumption from adolescence into adulthood and its longitudinal association with overweight. Br J Nutr 2007;98:431–438 [DOI] [PubMed] [Google Scholar]
- 22.Lytle LA, Seifert S, Greenstein J, McGovern P. How do children's eating patterns and food choices change over time? Results from a cohort study. Am J Health Promot 2000;14:222–228 [DOI] [PubMed] [Google Scholar]
- 23.Kelder SH, Perry CL, Klepp KI, Lytle LL. Longitudinal tracking of adolescent smoking, physical activity, and food choice behaviors. Am J Public Health 1994;84:1121–1126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Coleman KJ, Geller KS, Rosenkranz RR, Dzewaltowski DA. Physical activity and healthy eating in the after-school environment. J Sch Health 2008;78:633–640 [DOI] [PubMed] [Google Scholar]
- 25.Kelder S, Hoelscher DM, Barroso CS, Walker JL, Cribb P, Hu S. The CATCH Kids Club: a pilot after-school study for improving elementary students' nutrition and physical activity. Public Health Nutr 2005;8:133–140 [DOI] [PubMed] [Google Scholar]
- 26.Robinson TN, Killen JD, Kraemer HC, et al. Dance and reducing television viewing to prevent weight gain in African-American girls: the Stanford GEMS pilot study. Ethn Dis 2003;13(suppl 1):S65–S77 [PubMed] [Google Scholar]
- 27.Yin Z, Gutin B, Johnson MH, et al. An environmental approach to obesity prevention in children: Medical College of Georgia FitKid Project year 1 results. Obes Res 2005;13:2153–2161 [DOI] [PubMed] [Google Scholar]
- 28.Story M, Sherwood NE, Himes JH, et al. An after-school obesity prevention program for African-American girls: the Minnesota GEMS pilot study. Ethn Dis 2003;13(suppl 1):S54–S64 [PubMed] [Google Scholar]
- 29.Cassady D, Vogt R, Oto-Kent D, Mosley R, Lincoln R. The power of policy: a case study of healthy eating among children. Am J Public Health 2006;96:1570–1571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Harvard School of Public Health Harvard School of Public Health Prevention Research Center youth nutrition and physical activity guidelines for out-of-school time (OST) programs. Available at: http://www.hsph.harvard.edu/prc/proj_YMCA_guidelines_jun06.pdf. Accessed August 29, 2009
- 31.Institute for Healthcare Improvement The Breakthrough Series: IHI's collaborative model for achieving breakthrough improvement. Available at: http://www.ihi.org/NR/rdonlyres/3F1925B7-6C47-48ED-AA83-C85DBABB664D/0/TheBreakthroughSeriespaper.pdf. Accessed August 29, 2009
- 32.Wiecha J, Nelson T, Roth B, Glashagel J, Vaughan L. Disseminating health promotion practices in afterschool programs through YMCA learning collaboratives. Am J Health Promot In press [DOI] [PubMed] [Google Scholar]
- 33.Kant AK, Block G, Schatzkin A, Ziegler RG, Nestle M. Dietary diversity in the US population, NHANES II, 1976–1980. J Am Diet Assoc 1991;91:1526–1531 [PubMed] [Google Scholar]
- 34.Kant AK, Schatzkin A, Block G, Ziegler RG, Nestle M. Food group intake patterns and associated nutrient profiles of the US population. J Am Diet Assoc 1991;91:1532–1537 [PubMed] [Google Scholar]
- 35. 21 CFR 101.54 (2006)
- 36.Slavin J, Jacobs D, Marquart L. Whole-grain consumption and chronic disease: protective mechanisms. Nutr Cancer 1997;27:14–21 [DOI] [PubMed] [Google Scholar]
- 37. Peapod Web site. Available at: http://www.peapod.com. Accessed August 29, 2009.
- 38.USDA National Nutrient Database for Standard Reference, Release 20 Washington, DC: US Dept of Agriculture; 2007 [Google Scholar]
- 39. Recipezaar Web site. Available at: http://www.recipezaar.com. Accessed August 29, 2009.
- 40.Center for Nutrition Policy and Promotion US Dept of Agriculture. How much are you eating? Dietary guidelines for Americans. Home Garden Bull 2002;267:1–6 [Google Scholar]
- 41.Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull 1979;86:420–428 [DOI] [PubMed] [Google Scholar]
- 42.US Census Bureau American Fact Finder. Available at: http://www.factfinder.census.gov. Accessed August 29, 2009
- 43.Alliance for a Healthier Generation. Web site. Available at: http://www.healthiergeneration.org. Accessed August 29, 2009.
- 44.Ascherio A, Katan MB, Zock PL, Stampfer MJ, Willett WC. Trans-fatty acids and coronary heart disease. N Engl J Med 1999;340:1994–1998 [DOI] [PubMed] [Google Scholar]
- 45.Hu FB, Manson JE, Stampfer MJ, et al. Diet, lifestyle, and the risk of type 2 diabetes mellitus in women. N Engl J Med 2001;345:790–797 [DOI] [PubMed] [Google Scholar]
- 46.Bibby BG. The cariogenicity of snack foods and confections. J Am Dent Assoc 1975;90:121–132 [DOI] [PubMed] [Google Scholar]
- 47.Walker AR, Cleaton-Jones PE. Sugar intake and dental caries. Br Dent J 1992;172:7. [DOI] [PubMed] [Google Scholar]
- 48.Moynihan P, Petersen PE. Diet, nutrition and the prevention of dental diseases. Public Health Nutr 2004;7:201–226 [DOI] [PubMed] [Google Scholar]
- 49.Overby NC, Lillegaard IT, Johansson L, Andersen LF. High intake of added sugar among Norwegian children and adolescents. Public Health Nutr 2004;7:285–293 [DOI] [PubMed] [Google Scholar]
- 50.Bowman S. Diets of individuals based on energy intakes from added sugars. Fam Econ Nutr Rev 1999;12:31–38 [Google Scholar]
- 51.Britten P, Basiotis PP, Davis CA, Anand R.Is intake of added sugars associated with diet quality? Available at: http://www.usda.gov/cnpp. Accessed September 14, 2009.
- 52.Boot AM, de Ridder MA, Pols HA, Krenning EP, de Muinck Keizer-Schrama SM. Bone mineral density in children and adolescents: relation to puberty, calcium intake, and physical activity. J Clin Endocrinol Metab 1997;82:57–62 [DOI] [PubMed] [Google Scholar]
- 53.Cadogan J, Eastell R, Jones N, Barker ME. Milk intake and bone mineral acquisition in adolescent girls: randomised, controlled intervention trial. BMJ 1997;315:1255–1260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Tanasescu M, Ferris AM, Himmelgreen DA, Rodriguez N, Perez-Escamilla R. Biobehavioral factors are associated with obesity in Puerto Rican children. J Nutr 2000;130:1734–1742 [DOI] [PubMed] [Google Scholar]
- 55.Rockett HR, Berkey CS, Field AE, Colditz GA. Cross-sectional measurement of nutrient intake among adolescents in 1996. Prev Med 2001;33:27–37 [DOI] [PubMed] [Google Scholar]
- 56.Phillips SM, Bandini LG, Naumova EN, et al. Energy-dense snack food intake in adolescence: longitudinal relationship to weight and fatness. Obes Res 2004;12:461–472 [DOI] [PubMed] [Google Scholar]
- 57.Berkey CS, Rockett HR, Field AE, Gillman MW, Colditz GA. Sugar-added beverages and adolescent weight change. Obes Res 2004;12:778–788 [DOI] [PubMed] [Google Scholar]
- 58.Nicklas TA, Yang SJ, Baranowski T, Zakeri I, Berenson G. Eating patterns and obesity in children: the Bogalusa Heart Study. Am J Prev Med 2003;25:9–16 [DOI] [PubMed] [Google Scholar]
- 59.Wang Y, Ge K, Popkin BM. Why do some overweight children remain overweight, whereas others do not? Public Health Nutr 2003;6:549–558 [DOI] [PubMed] [Google Scholar]
- 60.Lin BH, Morrison RM. Higher fruit consumption linked with lower body mass index. Food Rev 2002;25:28–32 [Google Scholar]
- 61.Neumark-Sztainer D, Story M, Resnick MD, Blum RW. Correlates of inadequate fruit and vegetable consumption among adolescents. Prev Med 1996;25:497–505 [DOI] [PubMed] [Google Scholar]
- 62.Ludwig DS, Pereira MA, Kroenke CH, et al. Dietary fiber, weight gain, and cardiovascular disease risk factors in young adults. JAMA 1999;282:1539–1546 [DOI] [PubMed] [Google Scholar]
- 63.Howarth NC, Saltzman E, Roberts SB. Dietary fiber and weight regulation. Nutr Rev 2001;59:129–139 [DOI] [PubMed] [Google Scholar]
- 64.Epstein LH, Gordy CC, Raynor HA, Beddome M, Kilanowski CK, Paluch R. Increasing fruit and vegetable intake and decreasing fat and sugar intake in families at risk for childhood obesity. Obes Res 2001;9:171–178 [DOI] [PubMed] [Google Scholar]
- 65.Guenther PM, Dodd KW, Reedy J, Krebs-Smith SM. Most Americans eat much less than recommended amounts of fruits and vegetables. J Am Diet Assoc 2006;106:1371–1379 [DOI] [PubMed] [Google Scholar]
- 66.US Dept of Agriculture MyPyramid. Available at: http://www.mypyramid.gov. Accessed August 29, 2009
- 67.Patrick H, Nicklas TA. A review of family and social determinants of children's eating patterns and diet quality. J Am Coll Nutr 2005;24:83–92 [DOI] [PubMed] [Google Scholar]
- 68. National AfterSchool Association Web site. Available at: http://www.naaweb.org. Accessed August 29, 2009.
- 69.Food and Nutrition Service, US Dept of Agriculture Afterschool care snacks and suppers. Available at: http://www.fns.usda.gov/cnd/care/Regs-Policy/Snacks/Afterschool_Snacks_Suppers.htm. Accessed August 29, 2009
- 70.Stallings VA, Yaktine AL. Nutrition Standards for Foods in Schools: Leading the Way Toward Healthier Youth Washington, DC: National Academies Press; 2007 [Google Scholar]