Abstract
Objectives. We examined trends in smoking prevalence from 2002 through 2006 in 4 Asian communities served by the Racial and Ethnic Approaches to Community Health (REACH) intervention.
Methods. Annual survey data from 2002 through 2006 were gathered in 4 REACH Asian communities. Trends in the age-standardized prevalence of current smoking for men in 2 Vietnamese communities, 1 Cambodian community, and 1 Asian American/Pacific Islander (API) community were examined and compared with nationwide US and state-specific data from the Behavioral Risk Factor Surveillance System.
Results. Prevalence of current smoking decreased dramatically among men in REACH communities. The reduction rate was significantly greater than that observed in the general US or API male population, and it was greater than reduction rates observed in the states in which REACH communities were located. There was little change in the quit ratio of men at the state and national levels, but there was a significant increase in quit ratios in the REACH communities, indicating increases in the proportions of smokers who had quit smoking.
Conclusions. Smoking prevalence decreased in Asian communities served by the REACH project, and these decreases were larger than nationwide decreases in smoking prevalence observed for the same period. However, disparities in smoking prevalence remain a concern among Cambodian men and non–English-speaking Vietnamese men; these subgroups continue to smoke at a higher rate than do men nationwide.
Studies show that heart disease is the leading cause of death in all US racial/ethnic groups, except for Asian American/Pacific Islander (API) populations.1 For this group, cancer is the number 1 killer, with lung and bronchus cancer as the leading deadly cancers.1,2 Cigarette smoking is the principal risk factor for lung cancer, and it is the most preventable cause of illness and death.3 Some national surveys conducted in English have indicated that APIs as an aggregated group had a lower overall smoking prevalence than other racial/ethnic groups, suggesting that there might be less of a need for tobacco control, intervention, and prevention in these populations.4 However, when genders and ethnic groups are considered separately, there are large variations in smoking prevalence among APIs.5 Studies in local communities have found high smoking rates in Vietnamese, Cambodian, Laotian, Korean, and Filipino American men, especially when surveys were conducted in Asian languages in addition to English.6
Over the past 40 years, there has been an overall decline in smoking prevalence in the United States as the result of nationwide interventions.3 However, macro-level smoking interventions have not been implemented uniformly across all communities. The extent to which smoking intervention strategies are successful among racial/ethnic minority groups remains unclear.3,7,8 Relatively few tobacco intervention studies have been conducted in Asian communities.8,9 In fact, no multiyear continuous surveillance data are available for Asian communities.
The Racial and Ethnic Approaches to Community Health (REACH) project is a Centers for Disease Control and Prevention (CDC) program to eliminate racial and ethnic disparities in health.10 REACH supports community coalitions in designing, implementing, and evaluating community-driven strategies to eliminate disparities in various diseases and conditions. We examined 5-year trends in prevalence of smoking among men in Asian communities served by REACH, and we compared the trends observed in these communities to national and state-specific trends.
METHODS
In 1999, CDC launched the REACH project to help minority communities eliminate health disparities in 42 communities across the United States. In each of the 42 communities, REACH targeted at least 1 of the following racial/ethnic groups: African Americans, Hispanic Americans, APIs, and American Indians/Alaska Natives.10
Logic Model
Although local strategies varied, intervention and evaluation in each community followed a logic model developed by CDC that included the following stages.11
Capacity building.
Community-based coalitions were formed or expanded to address community health issues. Each coalition comprised a community-based organization and at least 3 other organizations, of which at least 1 was either a local or state health department, university, or research organization. These coalitions were primarily led by residents of the community at every stage of the program, including planning, implementation, and evaluation. The coalitions met regularly to discuss contexts and causes of health disparities as well as solutions for disparities. Coalitions chose 1 or more of the following health priority areas to focus on: cardiovascular disease, diabetes mellitus, breast and cervical cancer, infant mortality, immunizations, and HIV/AIDS.
Targeted actions.
Interventions included culturally tailored, language-appropriate health communication campaigns, education, and health promotion programs. Examples included local radio and cable TV talk shows, newsletters, distribution of educational audiotapes and CDs to low-literacy populations, posters, and fact sheets distributed in stores, restaurants, houses of worship, community meetings, health fairs, worksites, health clinics, and senior centers. Educational classes, seminars, and workshops were also offered to community members.
Community and systems change.
REACH focused on reducing the barriers to health care and health promotion information for the poor and underserved. Some coalitions focused on ensuring nondiscriminatory health care and culturally competent health education and treatment. Communities also conducted continuing education on disease prevention for health care providers. Many hospitals and health clinics provided free health information and education sessions. One intervention strategy aimed to create change among change agents (i.e., changing knowledge, attitudes, beliefs, and behaviors of influential people or groups with the intent of diffusing similar changes to a broader community population). Change agents included community health advocates and advisors, lay health workers, health promoters, ministers, Buddhist monks, and even beauty salon and barbershop operators. Using the social-ecological model, REACH projects also emphasized changes in policy and community environments, with the intention of effecting widespread change in risk or protective behaviors and reducing health disparities.
REACH Risk Factor Survey
As part of the REACH project evaluation, CDC conducted annual risk factor surveys in each of the 5 project years from 2002 through 2006.12 Data were collected in 27 communities that targeted cardiovascular diseases, diabetes, or breast and cervical cancer. For our study we examined data from 4 API communities served by REACH: 2 Vietnamese communities (1 in Los Angeles County and Orange County, California, and 1 in Santa Clara County, California) that targeted breast and cervical cancer; a Cambodian community in Lowell, Massachusetts, that targeted cardiovascular disease; and an API community in King County, Washington, that targeted diabetes.
The surveys were conducted by telephone (except for 2002 in Lowell, where interviews were conducted in person). Sampling designs were customized for each community by geography and by density of the targeted racial/ethnic groups. In the telephone surveys, a dual-frame sample design (i.e., a combination of random-digit-dial frame and listed-telephone frame) was used, except in Santa Clara County, where only the listed-telephone frame was used. In the Vietnamese and Cambodian communities, listed telephone frames were the lists of telephone numbers listed under Vietnamese or Cambodian surnames in area telephone directories. For 2002 in Lowell, an area probability sample was drawn. An average of 900 minority residents aged 18 years or older were interviewed in each community each year. The mean response rate was 65% for household screening (interviews with an adult to determine eligibility of the household and its members) and 59% for interviews with eligible family members.
A uniform questionnaire was used in all communities and in all survey years. Interviews were conducted in Vietnamese, Khmer, Cantonese, Mandarin, English, or Spanish. The respondents were first asked, “Have you smoked at least 100 cigarettes in your entire life?” If they answered “yes,” they were then asked, “Do you now smoke cigarettes every day, some days, or not at all?”
Data from the REACH Risk Factor Survey were compared with data from the 50 states and the District of Columbia in the Behavioral Risk Factor Surveillance System (BRFSS).13 The BRFSS survey uses multistage random-digit dialing to gather a representative sample from each state's noninstitutionalized residents aged 18 years or older. The BRFSS survey is conducted continuously, and its results are compiled and released annually. The main language used in the BRFSS interviews was English, but Spanish was also used in some states. In BRFSS, APIs are an aggregate of various ethnic subgroups. The median cooperation rates for BRFSS ranged from 74% to 77% between 2002 and 2006.
Data Analysis
Persons who had smoked at least 100 cigarettes in their entire life were defined as ever smokers. Those who currently smoked cigarettes every day or some days were defined as current smokers. Those who had smoked at least 100 cigarettes but currently did not smoke were defined as former smokers. Quit ratio, an indicator of proportion of smokers quitting, was defined as the percentage of former smokers among ever smokers.14 The 3 smoking status prevalences were age-standardized to the 2000 US Census.
We used the χ2 test to compare baseline characteristics of persons in the 2002 REACH Risk Factor Survey with baseline characteristics of persons in the 2002 BRFSS. Logistic regression, adjusting for 5 age groups, was used to examine the secular trends in the prevalence of current smoking and in the quit ratio from 2002 through 2006. The 2-sided z test was used to compare the 2 beta coefficients of the year term, derived from the logistic regressions, to determine whether the 2 comparison linear trends were significantly different. The secular trends in REACH communities were compared with persons in the US general population and with APIs nationwide, as well as with the general population in the specific state (California, Massachusetts, or Washington) where the REACH community was located.
The 2 California REACH projects targeted Vietnamese communities, and data from these 2 communities were pooled and labeled as “Vietnamese.” The REACH project in King County, Washington, targeted 3 racial/ethnic groups (African Americans, Hispanic Americans, and APIs), but only API respondents were included in the analysis. Respondents from this community were members of various ethnic subgroups, such as Chinese, Japanese, Korean, Filipino, Asian Indian, Vietnamese, Cambodian, Laotian, Thai, and others. They are reported as 1 group labeled Asian. Current smoking was uncommon in women in the survey communities (rates ranged from 1% to 7%); therefore, only data from men are presented in this report. All analyses were performed using SUDAAN to account for the complex sampling designs in both REACH and BRFSS.
RESULTS
Table 1 shows the baseline characteristics of Vietnamese, Cambodian, and Asian REACH respondents, and US and API respondents to the BRFSS, in 2002. Among Vietnamese and Cambodian respondents, less than one third of the interviews were administered in English, except in King County, Washington, where English was used in three fourths of the interviews because the survey was only provided in 3 Asian languages (Chinese, Vietnamese, and Khmer). The data show that, in general, Cambodian men were younger than were the general US population of men, and Asian men in King County, Washington, were older than were the general US population. Cambodian men had the lowest education level. Men in all 3 of the REACH groups had markedly lower annual family income than did the BRFSS US and API men. Obesity was uncommon in REACH communities and in BRFSS API men. Half of the Cambodian men and nearly one third of the Vietnamese respondents were current smokers, whereas about one fourth of the general US population respondents smoked.
TABLE 1.
Characteristics of Adult Men in Asian Communities Targeted by REACH and Participating in the BRFSS: United States, 2002
| 2002 REACH Risk Factor Survey |
2002 BRFSS |
||||
| Characteristics | Vietnamese (n = 1055), % (SE) | Cambodian (n = 418), % (SE) | Asian (n = 184), % (SE) | United States (n = 96 549), % (SE) | US API (n = 3282), % (SE) |
| English-speaking | 29.1 (1.7) | 32.6 (7.5) | 75.4 (5.1) | 94.3a (0.2) | 99.2a (0.4) |
| Age, y | |||||
| 18–34 | 28.3 (1.8) | 39.9 (4.9) | 48.5 (6.7) | 33.4 (0.2) | 47.2 (1.9) |
| 35–44 | 26.6 (1.7) | 32.1 (5.9) | 23.1 (5.5) | 21.5 (0.2) | 23.3 (1.6) |
| 45–54 | 19.6 (1.5) | 16.1 (4.6) | 14.1 (4.7) | 18.7 (0.2) | 15.9 (1.4) |
| 55–64 | 12.7 (1.2) | 4.6 (1.0) | 2.3 (0.7) | 12.4 (0.1) | 9.2 (1.1) |
| ≥ 65 | 12.8 (1.1) | 7.3 (2.5) | 12.0 (4.5) | 14.1 (0.1) | 4.4 (0.8) |
| Education level | |||||
| < High school | 18.6 (1.4) | 40.2 (6.5) | 11.9 (4.1) | 12.6 (0.2) | 5.0 (0.8) |
| High school graduate | 23.6 (1.6) | 42.2 (6.7) | 22.3 (5.3) | 30.2 (0.3) | 16.4 (1.5) |
| Some college | 25.6 (1.7) | 14.5 (2.7) | 19.4 (5.2) | 25.5 (0.3) | 19.8 (1.8) |
| College graduate | 32.3 (1.9) | 3.1 (1.0) | 46.4 (6.8) | 31.7 (0.3) | 58.8 (2.0) |
| Annual family income, $ | |||||
| < 24 999 | 49.2 (2.0) | 45.6 (5.6) | 42.9 (7.1) | 25.2 (0.3) | 23.1 (2.0) |
| 25 000–49 999 | 27.9 (1.8) | 43.4 (7.2) | 25.7 (6.1) | 32.5 (0.3) | 24.2 (1.7) |
| 50 000–74 999 | 11.4 (1.2) | 2.3 (0.7) | 14.2 (5.2) | 18.2 (0.2) | 17.7 (1.7) |
| ≥ 75 000 | 11.5 (1.2) | 8.8 (3.5) | 17.2 (5.4) | 24.1 (0.3) | 35.0 (2.2) |
| Weightb | |||||
| Normal | 75.1 (1.6) | 67.7 (6.6) | 56.1 (6.8) | 33.1 (0.3) | 53.2 (2.1) |
| Overweight | 23.3 (1.6) | 28.9 (6.7) | 39.8 (6.7) | 44.6 (0.3) | 37.7 (2.1) |
| Obese | 1.6 (0.4) | 3.4 (0.8) | 4.0 (2.6) | 22.3 (0.2) | 9.2 (1.1) |
| Smoking status | |||||
| Current smoker | 31.0 (1.7) | 50.1 (5.4) | 23.4 (5.6) | 25.3 (0.3) | 19.3 (1.6) |
| Past smoker | 11.3 (1.1) | 8.7 (3.7) | 29.3 (6.4) | 27.9 (0.2) | 18.6 (1.7) |
| Never | 57.7 (1.9) | 41.1 (4.8) | 47.3 (6.7) | 46.8 (0.3) | 62.1 (2.0) |
Note. API = Asian American/Pacific Islander; BRFSS = Behavioral Risk Factor Surveillance System; REACH = Racial and Ethnic Approaches to Community Health. Vietnamese data was pooled for 2 Vietnamese communities in southern California targeted by REACH. Cambodian data was from a Cambodian community in Lowell, MA, targeted by REACH. Asian data was pooled for members of various Asian American/Pacific Islander ethnic subgroups in King County, WA.
Information not available for 2002; data for 2003 were used instead.
Normal, overweight, and obese weight categories were defined by body mass index (weight in kilograms divided by height in meters squared). Normal < 25 kg/m2, overweight = 25-29.99 kg/m2, and obese ≥ 30 kg/m2.
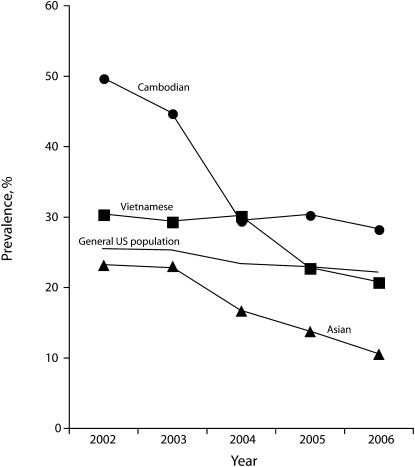
Figure 1 presents 5-year trends in age-standardized prevalence of current smoking in REACH Vietnamese, Cambodian, and Asian men and in BRFSS US men. Table 2 shows the results of logistic regression analyses on these data. A significant downward trend in the age-standardized prevalence of current smoking (ranging from −2.58% per year in the Vietnamese community to −5.73% per year in the Cambodian community) was observed in men from all 3 REACH communities. A significant downward trend (–0.91% per year; P < .01) was also observed in the general US population of men; however, the decline was greater in the REACH communities than in the nation. The negative values of the beta coefficient for the year term in logistic regression equations were significantly smaller when comparing either Vietnamese or Cambodians to the general US population of men (P < .05). The difference between Asians in REACH and the general US population of men was borderline statistically significant (P = .08) because of the small sample sizes of Asians in King County.
FIGURE 1.
Five-year trends of age-standardized prevalence of current smoking among adult men in the US general population and in 4 US Asian communities: REACH, 2002–2006.
Note. API = Asian American/Pacific Islander; BRFSS = Behavioral Risk Factor Surveillance System; REACH = Racial and Ethnic Approaches to Community Health. Vietnamese data were pooled for 2 Vietnamese communities in southern California targeted by REACH. Cambodian data were from a Cambodian community in Lowell, MA, targeted by REACH. Asian data were pooled for members of various API ethnic subgroups in King County, WA. General US population data were collected by the BRFSS. Data for Asian men collected by the BRFSS are not shown. Smoking prevalence among BRFSS Asian men was on average 7.4% lower than that among BRFSS US men, but the temporal changes were similar between the 2 groups.
TABLE 2.
Logistic Regression Analysis Examining Trends of Current Smoking Among Men in Asian Communities Targeted by REACH Compared With the General US, General US Asian, and California, Washington, and Massachusetts General State Populations: BRFSS and REACH, 2002–2006
| Average Sample Size Each Year | B Pair Comparisons |
||||
| B (SE) | Slopea | Comparison Group | P | ||
| REACH | |||||
| Vietnamese | 906 | −0.12* (0.03) | −2.58 | General US population | .02 |
| Cambodian | 334 | −0.28* (0.07) | −5.73 | General US population | <.01 |
| Asian | 182 | −0.22* (0.09) | −3.42 | General US population | .08 |
| National BRFSS | |||||
| General US population | 115 000 | −0.05* (0.01) | −0.91 | ||
| API | 2 870 | −0.09* (0.03) | −1.13 | ||
| State-Specific BRFSS | |||||
| CA | 2 000 | −0.02 (0.02) | −0.35 | REACH Vietnamese | .01 |
| MA | 3 500 | −0.02 (0.02) | −0.31 | REACH Cambodian | <.01 |
| WA | 6 700 | −0.07* (0.02) | −1.08 | REACH Asian | .12 |
Note. API = Asian American/Pacific Islander; BRFSS = Behavioral Risk Factor Surveillance System; REACH = Racial and Ethnic Approaches to Community Health. Vietnamese data was pooled for 2 Vietnamese communities in southern California targeted by REACH. Cambodian data was from a Cambodian community in Lowell, MA, targeted by REACH. Asian data was pooled for members of various Asian American/Pacific Islander ethnic subgroups in King County, WA.
Percentage change per year.
P < .01; B significantly different from zero.
As a result of these diverse trends, the smoking disparity between Cambodian and the general US population of men decreased from 2002 through 2006. Smoking prevalence among Cambodian men exceeded that of US men by 24 percentage points and 6 percentage points in 2002 and 2006, respectively. Smoking prevalence among Vietnamese men was 4.9 percentage points higher than that among US men in 2002 but was 1.3 percentage points lower than that among US men in 2006 (Figure 1).
The secular trend of current smoking among men in each REACH community was also compared with the male general population in the same states (Table 2). Gradual decreases in smoking prevalence (–0.35% to −1.08% per year), paralleling the national trend, were observed in these 3 states. The rate of decrease in smoking was larger in the REACH Vietnamese and Cambodian communities than in the comparison states. The difference between Asian men in King County and men in Washington did not reach statistical significance, however (P = .12). Because of these diverse trends, the smoking disparity between Cambodian men and men in Massachusetts decreased from 2002 through 2006. Smoking prevalence among Cambodian men exceeded that of Massachusetts men by 29 percentage points and 8 percentage points in 2002 and 2006, respectively. Smoking prevalence among Vietnamese men exceeded that among men in California by 11 percentage points and 2 percentage points in 2002 and 2006, respectively.
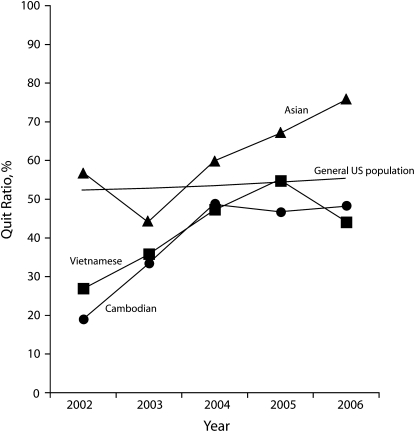
There was a small increasing trend of never smoking (0.30% to 2.38% per year) in the 3 REACH communities. To examine whether the downward trends in the prevalence of current smoking in REACH communities were the result of the increase in smokers quitting, the quit ratios (percent of ever smokers who had quit) were calculated; the results are presented in Figure 2. Significant upward trends of quit ratios were apparent among all 3 Asian groups in the REACH communities. For example, in year 1 (2002), 19% of Cambodian men who had ever been smokers had quit. By year 5 (2006), this proportion had increased to 48%. In contrast, the quit ratio changed only a little (0.75% per year) in the same time period among the male US general population. The quit ratio among men in the 3 states where the REACH communities were located was on average 5% to 6% higher than was the national average. In contrast to the REACH communities with dramatic increases in quit ratios, there were only small changes (–0.41% to +1.04% per year) among the 3 comparison states.
FIGURE 2.
Five-year trends of quit ratios among adult men in the US general population and in 4 US Asian communities: REACH, 2002–2006.
Note. API = Asian American/Pacific Islander; BRFSS = Behavioral Risk Factor Surveillance System; REACH = Racial and Ethnic Approaches to Community Health. Vietnamese data were pooled for 2 Vietnamese communities in southern California targeted by REACH. Cambodian data were from a Cambodian community in Lowell, MA, targeted by REACH. Asian data were pooled for members of various API ethnic subgroups in King County, WA. General US population data were collected by the BRFSS. Data for Asian men collected by the BRFSS are not shown.
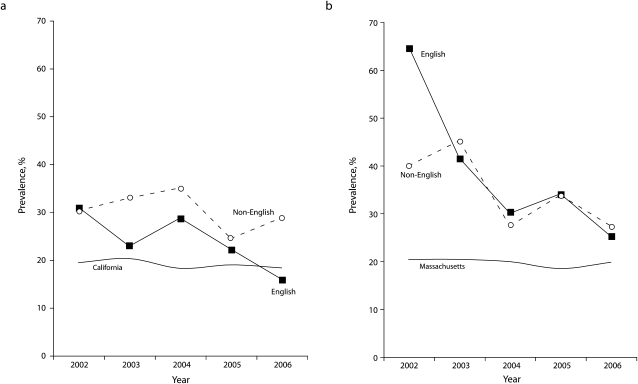
To examine the influence of American acculturation on smoking trends, we stratified the analysis by language used during the interview (English versus non-English; Figure 3). Because of the limited sample size of Asians in King County, Washington, stratified analysis (i.e., stratified by language used in the interview) was not performed for this group. In the 2 Vietnamese communities, the prevalence of current smoking decreased more rapidly in men who spoke English than it did in men who spoke Vietnamese (P < .01). However, there was no significant difference in change in prevalence by language in Cambodian men (P = .11). Figure 3 also shows that at year 5 of the project, prevalence of current smoking was still 10.5 percentage points higher among non–English-speaking Vietnamese in the REACH communities in California (28.8%) than that in the California male general population (18.3%). The difference in prevalence of current smoking between Cambodian men in Lowell, Masachusetts, (26.2%) and the Massachusetts male general population (19.7%) was about 6.5 percentage points.
FIGURE 3.
Five-year trends of age-standardized prevalence of current smoking among adult men, by language used during interviews with (a) Vietnamese respondents and the California general population and (b) Cambodian respondents and the Massachusetts general population: REACH, 2002–2006.
Note. BRFSS = Behavioral Risk Factor Surveillance System; REACH = Racial and Ethnic Approaches to Community Health; Vietnamese data were pooled for 2 Vietnamese communities in southern California targeted by REACH. California data were state-specific data collected by the BRFSS. Cambodian data were from a Cambodian community in Lowell, MA, targeted by REACH. Massachusetts data were state-specific data collected by the BRFSS.
DISCUSSION
In contrast to the slow decreases in prevalence of current smoking between 2002 and 2006 among the general US population of men, the API population of men nationwide, and men in the comparison states, there were dramatic reductions in smoking among men in API communities served by REACH. Smoking disparities between men in REACH Asian communities and the general US population of men (or men in the comparison states) decreased significantly. The marked increase in the quit ratio among men in the REACH Asian communities contrasted sharply with the small changes in quit ratios in their national and state counterparts. The current data also show that prevalence of current smoking decreased more rapidly among English-speaking Vietnamese men than among non–English-speaking Vietnamese men. However, the decrease in smoking prevalence was not significantly different between the English-speaking and non–English-speaking Cambodian men.
Members of racial/ethnic minority groups and individuals of low socioeconomic status remain at high risk for tobacco use and suffer disproportionately from tobacco-related illness and death.3 Our data show a very high prevalence of smoking among Vietnamese and Cambodian men (30% and 50%, respectively, at baseline), which was consistent with other studies.6 At the completion of the 5-year study, prevalences of current smoking were still higher among Cambodian men (28%) and non–English-speaking Vietnamese men (29%) than they were among the general US population of men nationwide (22%). Quit ratios were still about 15% lower among Vietnamese and Cambodian men than among California and Massachusetts men.
Smoking is a social and cultural norm for men in Asian countries.15 A review of tobacco industry documents has demonstrated that the tobacco industry has targeted and developed specific strategies to promote tobacco use among Asian immigrants to the United States16 and in Asian American communities.17 Although great strides have been made in reducing tobacco use in the United States, our knowledge of effective strategies for some racial/ethnic minority groups is limited.8 A literature search of tobacco interventions that reported smoking cessation outcomes (including quit rates) among US minority populations for the period 1985 through 2001 revealed that among 22 studies found, only 3 had been implemented in Asian communities.8 These 3 interventions, conducted in the 1990s, reported mixed results.18–20 It is encouraging that a recent smoking cessation intervention among Chinese immigrants living in New York City indicated that community-based tailored tobacco control interventions may reduce smoking prevalence rates beyond the reduction achieved by public policies.21 Two ongoing community-based participatory research projects focused on tobacco control are currently being conducted: a project in the San Francisco Bay Area that focuses on Chinese populations,22 and a project in the Delaware Valley region of Pennsylvania and New Jersey that focuses on Chinese, Korean, Vietnamese, and Cambodian populations.23
REACH was not designed as a tobacco intervention trial; tobacco control was only 1 of the education components of the project. A unique feature of REACH was that the project did not use a standardized intervention protocol focusing on the same singular behavior or disease. Rather, the project was sufficiently flexible to allow community choices. Building capacity by forming or expanding a community-based coalition was the common foundation of the REACH project.11 This model helped mobilize communities and created a sense of ownership, empowerment, and synergy of action. REACH has created stronger, more resilient communities capable of sustaining various health-improvement efforts. Although different communities selected different diseases and conditions as their priority areas, the overall goal was the same: to build a healthy community through overall increase in knowledge and motivation to live a healthy lifestyle. Smoking is a risk factor for many of the selected diseases; thus, many interventions addressed it in that light.
The actions taken by the coalitions were coordinated with various health education and intervention efforts, such as antismoking campaigns, nutrition education, promotion of physical activity, adult immunization, and screening for blood pressure, glucose, cholesterol, and breast and cervical cancer. REACH coalitions made special efforts to reach the most disadvantaged segments of their communities (e.g., people who were new immigrants, faced language barriers, or had low socioeconomic status). In addition to a general mass-media campaign, lay health workers were instrumental in reaching these disadvantaged groups.
Our analysis stratified by language use indicates that significant downward trends of smoking prevalence were observed in both English speakers and in non-English speakers or less acculturated groups in some REACH Asian communities. However, in the 2 Vietnamese REACH communities, we observed a slower decline in smoking prevalence among the Vietnamese speakers. Previous research has found that Asian men with lower English proficiency were more likely to be smokers than were Asian men with higher English proficiency.24 These findings reemphasize the importance of language-specific interventions and services in API communities.
Unlike a typical tobacco intervention trial, we did not have control communities. Therefore, the association between the significant decline in smoking prevalence observed in the REACH Asian communities and the net effect of intervention cannot be established. The REACH project was a combination of public health practice and scientific research that was conducted in 42 communities across the nation. Delineating and establishing causation was not the aim of this project. Nonetheless, comparison with the BRFSS data reveals that significant reductions in smoking disparities between the general US population of men and male API population occurred during 2002–2006 in the REACH Asian communities, when the REACH community-based intervention projects were being conducted in these communities.
This study has several limitations. We evaluated the community intervention through the annual telephone survey of representative samples of the community; thus, households without telephone service or with wireless-only telephones were excluded. Adults with wireless-only service are more likely to be current smokers.25 However, such bias existed in the comparison data from BRFSS as well.
Eliminating health disparities related to tobacco use is a major public health challenge facing Asian communities. Some researchers have said they believe that community-based programs have yet to demonstrate an influence on behavioral or health status outcomes.26 The decline in smoking prevalence observed at the population level in the REACH Asian communities indicates otherwise and highlights the value of working with communities to improve the health and well-being of minority community members. Despite the decline in the prevalence of smoking in these API communities, smoking disparities remain particularly high among non–English-speaking Vietnamese and English-speaking and non–English-speaking Cambodians. Clearly, eliminating tobacco use and health disparities must involve engaging local leaders, building community partnerships, recognizing cultural influences, creating sustainable programs, leveraging resources, and empowering individuals and communities.
Acknowledgments
The authors wish to acknowledge the following organizations that participated in the REACH Risk Factor Survey: Division of Adult and Community Health, National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention, Atlanta, GA; Lowell Community Health Center, Lowell, MA; Seattle–King County Department of Public Health, WA; Orange County Asian and Pacific Islander Community Alliance, Garden Grove, CA; and the Vietnamese Community Health Promotion Project (Suc Khoe La Vang!) at the University of California, San Francisco, and the Vietnamese Reach for Health Coalition in Santa Clara County, CA.
Human Participant Protection
This project was approved by the institutional review board of the Centers for Disease Control and Prevention.
References
- 1.Heron M. Death: Leading Causes for 2004 Hyattsville, MD: National Center for Health Statistics; 2007 [PubMed] [Google Scholar]
- 2.Miller BA, Chu KC, Hankey BF, Ries LA. Cancer incidence and mortality patterns among specific Asian and Pacific Islander populations in the United States. Cancer Causes Control 2008;19(3):227–256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reducing Tobacco Use: A Report of the Surgeon General Atlanta, GA: Centers for Disease Control and Prevention, US Dept of Health and Human Services; 2000 [Google Scholar]
- 4.Centers for Disease Control and Prevention Cigarette smoking among adults—United States, 2006. MMWR Morb Mortal Wkly Rep 2007;56(44):1157–1161 [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention Prevalence of cigarette use among 14 racial/ethnic populations—United States, 1999–2001. MMWR Morb Mortal Wkly Rep 2004;53(3):49–52 [PubMed] [Google Scholar]
- 6.Kim SS, Ziedonis D, Chen KW. Tobacco use and dependence in Asian Americans: a review of the literature. Nicotine Tob Res 2007;9(2):169–184 [DOI] [PubMed] [Google Scholar]
- 7.Doolan DM, Froelicher ES. Efficacy of smoking cessation intervention among special populations: review of the literature from 2000 to 2005. Nurs Res 2006;55(suppl 4):S29–S37 [DOI] [PubMed] [Google Scholar]
- 8.Lawrence D, Graber JE, Mills SL, Meissner HI, Warnecke R. Smoking cessation interventions in US racial/ethnic minority populations: an assessment of the literature. Prev Med 2003;36(2):204–216 [DOI] [PubMed] [Google Scholar]
- 9.Chen MS, Jr, Tang H. Review of smoking cessation research among Asian Americans: the state of the research. Nicotine Tob Res 2007;9(suppl 3):485–493 [DOI] [PubMed] [Google Scholar]
- 10.Giles WH, Tucker P, Brown L, et al. Racial and ethnic approaches to community health (REACH 2010): an overview. Ethn Dis 2004;14(3, suppl. 1):S5–S8 [PubMed] [Google Scholar]
- 11.Tucker P, Liao Y, Giles WH, Liburd L. The REACH 2010 logic model: an illustration of expected performance. Prev Chronic Dis 2006;3(1):A21. [PMC free article] [PubMed] [Google Scholar]
- 12.Liao Y, Tucker P, Okoro CA, Giles WH, Mokdad AH, Harris VB. REACH 2010 surveillance for health status in minority communities—United States, 2001–2002. MMWR Surveill Summ 2004;53(6):1–36 [PubMed] [Google Scholar]
- 13.Mokdad AH, Stroup DF, Giles WH. Public health surveillance for behavioral risk factors in a changing environment. Recommendations from the Behavioral Risk Factor Surveillance Team. MMWR Recomm Rep 2003;52(RR–9):1–12 [PubMed] [Google Scholar]
- 14.Reducing the Health Consequences of Smoking: 25 Years of Progress. A Report of the Surgeon General. Atlanta, GA: Centers for Disease Control and Prevention, US Dept of Health and Human Services; 1989 [Google Scholar]
- 15.Corrao MAGG, Sharma N, Shokoohi DF, Tobacco Control Country Profiles Atlanta, GA: American Cancer Society; 2000 [Google Scholar]
- 16.Acevedo-Garcia D, Barbeau E, Bishop JA, Pan J, Emmons KM. Undoing an epidemiological paradox: the tobacco industry's targeting of US immigrants. Am J Public Health 2004;94(12):2188–2193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Muggli ME, Pollay RW, Lew R, Joseph AM. Targeting of Asian Americans and Pacific Islanders by the tobacco industry: results from the Minnesota Tobacco Document Depository. Tob Control 2002;11(3):201–209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McPhee S, Jenkins CN, Wong C, et al. Smoking cessation intervention among Vietnamese Americans: a controlled trial. Tob Control 1995;4(suppl 1):S16–S24 [Google Scholar]
- 19.Jenkins CN, McPhee SJ, Le A, Pham GQ, Ha NT1, Stewart S. The effectiveness of a media-led intervention to reduce smoking among Vietnamese American men. Am J Public Health 1997;87(6):1031–1034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen MS., Jr The status of tobacco cessation research for Asian Americans and Pacific Islanders. Asian Am Pac Isl J Health 2001;9(1):61–65 [PubMed] [Google Scholar]
- 21.Shelley D, Fahs M, Yerneni R, et al. Effectiveness of tobacco control among Chinese Americans: a comparative analysis of policy approaches versus community-based programs. Prev Med 2008;47(5):530–536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wong CC, Tsoh JY, Tong EK, Hom FB, Cooper B, Chow EA. The Chinese community smoking cessation project: a community sensitive intervention trial. J Community Health 2008;33(6):363–373 [DOI] [PubMed] [Google Scholar]
- 23.Ma GX, Toubbeh JI, Su X, Edwards RL. ATECAR: An Asian American community-based participatory research model on tobacco and cancer control. Health Promot Pract 2004;5(4):382–394 [DOI] [PubMed] [Google Scholar]
- 24.Tang H, Shimizu R, Chen MS., Jr English language proficiency and smoking prevalence among California's Asian Americans. Cancer 2005;104(suppl 12):2982–2988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Blumberg SJ, Luke JV, Cynamon ML. Telephone coverage and health survey estimates: evaluating the need for concern about wireless substitution. Am J Public Health 2006;96(5):926–931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Merzel C, D'Afflitti J. Reconsidering community-based health promotion: promise, performance, and potential. Am J Public Health 2003;93(4):557–574 [DOI] [PMC free article] [PubMed] [Google Scholar]