Abstract
We evaluated a community-based 12-week healthy lifestyle program in Moloka‘i, HI, called Ke ‘Ano Ola, which was developed to decrease chronic disease risk through health education emphasizing weight loss, exercise, and risk factor reduction. Program leaders' strong commitment and positive role modeling, along with social and group support and community involvement, were key elements. A pre–post evaluation of weight, blood pressure, total cholesterol, and blood sugar showed significant improvements for weight (mean change [Δ] = −7.4 lbs; P < .001), systolic blood pressure (Δ = –3.8 mm Hg; P = .027), diastolic blood pressure (Δ = –4.6 mm Hg; P < .001), and total cholesterol (Δ = –9.7 mg/dL; P < .001). Attrition was low, with 89% of participants attending all 12 sessions. Our findings show that lifestyle improvements in a predominantly Native Hawaiian community are achievable in a support group setting.
IN 2008, AN ESTIMATED 72.8% of the residents of Moloka‘i, HI, were overweight (body mass index [BMI; defined as mass in kilograms divided by height in meters squared] = 25–29 kg/m2) or obese (BMI ≥ 30 kg/m2); only an estimated 57.4% of Honolulu residents were similarly overweight. Native Hawaiians in the state were more than twice as likely as Whites to be obese (44.1% versus 21.3%, respectively).1 The prevalence of obesity among Hawaiians on Moloka‘i, a predominantly Hawaiian community, is in stark contrast to the entire state of Hawai‘i, which was ranked the second healthiest state in the nation in 2008.2 Hawaiians, especially those living on Moloka‘i, continue to experience significant health disparities and therefore need health interventions that are community driven and culturally appropriate.
KEY FINDINGS
Effects of the Ke 'Ano Ola intervention after 3 months:
▪Improved diastolic blood pressure,
▪Improved systolic blood pressure,
▪Decreased body weight,
▪Improved total cholesterol level,
▪Improved low-density lipoprotein level,
▪Improved high-density lipoprotein level, and
▪High participant satisfaction.
Several commercial weight-loss programs have come to Moloka‘i, with limited long-term success. In 2008, community members requested that Na Pu‘uwai, the island's Native Hawaiian health care system, whose mission is to improve the overall health and wellness of Hawaiians living on Moloka‘i, offer a weight-loss program that could be community driven and sustained long term. This request was made to the Na Pu‘uwai staff by persons participating in health-screening events or receiving regular monitoring of blood glucose and hypertension. A team of Na Pu‘uwai staff and off-island consultants—an epidemiologist, a registered dietician, a lifestyle interventionist, a medical director, a psychologist, 2 registered nurses, and 5 community health workers—developed a lifestyle intervention program. After considering the requests of community members and evaluating past lifestyle interventions, the team created Ke ‘Ano Ola (KAO). This name, which means healthy lifestyle, was suggested by a Moloka‘i Hawaiian-language expert and reflects the healthy lifestyle and community participation nature of the program.
Three important components of successful lifestyle interventions were incorporated into KAO: social support, group support, and community involvement. A previous study evaluated mediators of lifestyle behavior change in Native Hawaiians and found that social support was a key factor in moving participants from the preaction stage of change to the action–maintenance stage for improvements in dietary fat intake and exercise.3 Another study looked at group support as a component of weight-loss and maintenance programs and found that recruiting and treating teams of 3 friends with a strong social support intervention decreased the number of dropouts and markedly increased the percentage of participants who maintained their weight loss over the 6-month follow up period.4 It has been shown that community involvement is an important aspect of successful programs tailored for Native Hawaiians. This is exemplified by the Partnership for Improving Lifestyle Interventions project.5
The objective of KAO was to decrease risk factors for chronic disease—primarily obesity, hypertension, hypercholesterolemia, and diabetes—through nutrition, physical activity, and specific chronic disease prevention education in a support group setting.
Ke ‘Ano Ola participants and staff assistants preparing a healthy meal.
METHODS
We conducted a 12-week pilot test of our lifestyle intervention with the Na Pu‘uwai staff. We chose this group for the pilot because they represented a sample comparable to the ethnic and socioeconomic status of the Moloka‘i community that they have served for 17 years. Each week, participants met in a 1-hour support group for nutrition consultation and education. We administered health assessments before and after the program. Participants also completed a satisfaction survey.
Pilot participants recommended the following additions and modifications to the protocol: educational sessions by community health educators with expertise in various areas of preventive health, weekly cooking demonstrations, and an overall focus on chronic disease prevention through emphasis on healthy lifestyle modification rather than weight loss alone.
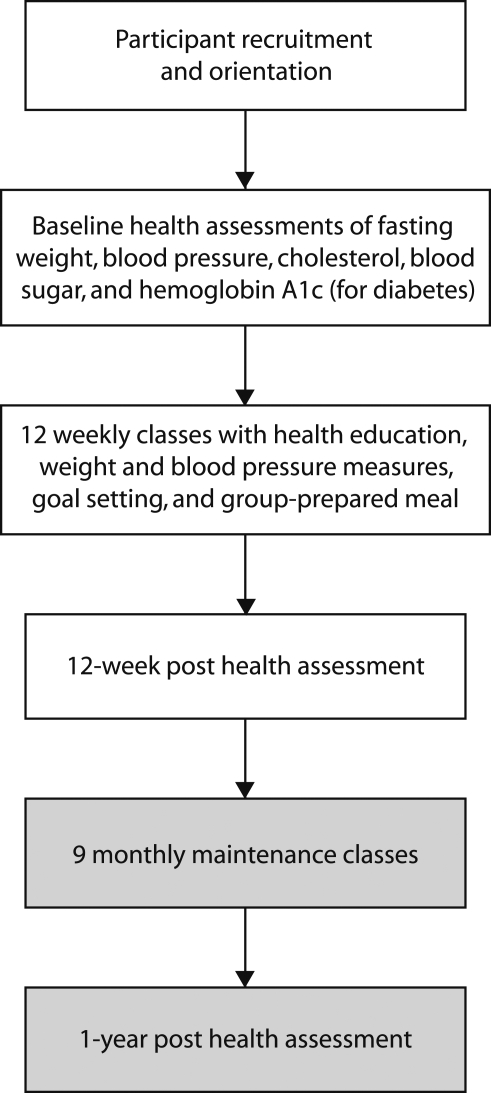
We recruited for the first KAO class in 2008 by posting flyers at 2 local grocery stores and encouraging potential participants to sign up during Na Pu‘uwai's annual health fair (Figure 1). Potential participants were invited to an orientation at the Na Pu‘uwai office, which is centrally located in the community. Sixty community members participated in the orientation, where they were provided with information about KAO. After describing the disparate health conditions among Native Hawaiians, the program's leader, an epidemiologist with a master's degree in public health, explained the protocol and the need for data collection and evaluation as components of a sustainable program. The program included a registration fee of $50, which covered all of the clinical measurements, 3 months of membership at Na Pu‘uwai's fitness center, a food scale, a pedometer, and the weekly educational classes, which included meals. At the orientation, participants requested that this program start immediately. In response to the initial excitement about the program, Na Pu'uwai staff began scheduling appointments for the following week.
FIGURE 1.
Steps in the Ke ‘Ano Ola healthy lifestyle program: Moloka‘i, HI, 2008.
The KAO staff completed baseline health assessments for each of the 74 participants, who obtained medical clearance from their primary care physician. These physicians were sent a description of the program and their patients' lab results. The preprogram health assessment measured weight, body fat, height, blood pressure, blood glucose, and blood lipids. Individuals previously diagnosed with diabetes were also tested for hemoglobin A1c levels. These clinical measurements were repeated after 12 weeks to determine overall changes and program effectiveness. KAO participants attended weekly 2-hour sessions (Table 1). Before each session, a group of 3 participant volunteers planned a healthy meal to prepare for the class. The KAO staff assisted with the meal preparation in the Na Pu‘uwai office kitchen. Each week, the program leader introduced an educator who would conduct an interactive educational session focusing on 1 aspect of chronic disease prevention. Next, a weekly goal was set by each of the participants with the support of the entire class. At the end of each class, a kupuna (elder) offered a prayer as the group prepared to enjoy the healthy meal together.
TABLE 1.
Curriculum of the Ke ‘Ano Ola Healthy Lifestyle Program: Moloka‘i, HI, 2008
| Week | Session Topic | Community Health Resource Educator |
| 1 | Understanding daily caloric needs | Community health worker who specializes in nutrition and physical activity |
| 2 | Incorporating physical activity into your new lifestyle | Fitness center manager/certified personal trainer |
| 3 | Modifying risk factors for diabetes | Registered nurse/certified diabetes educator |
| 4 | Group support to evaluate progress and challenges | Program leader |
| 5 | Preventing chronic kidney disease through diet modifications | Registered nurse |
| 6 | Moods and foods (focusing on emotional triggers around eating) | Clinical psychologist |
| 7 | Cancer-fighting foods | Community health worker who specializes in cancer education |
| 8 | Incorporating Hawaiian traditional medicine practices to treat chronic disease | Hawaiian traditional medicine (la‘au lapa‘au) group |
| 9 | Increasing physical activity to achieve the recommended 1 h/d, 5 d/wk | Fitness center manager/certified personal trainer |
| 10 | Meal planning | Registered dietician |
| 11 | Cardiovascular disease prevention | Community health worker specializing in cardiovascular disease |
| 12 | Final evaluations and transition into the maintenance program | Program leader |
Because exercise is a critical component of KAO, the second class focused on physical activity, introducing basic exercise concepts. After this introductory class, participants formed small exercise groups and attended an aerobic exercise class taught by the program leader at the Na Pu‘uwai fitness center.
We analyzed the baseline and postintervention clinical measures with SAS version 9.1 (SAS Institute Inc, Cary, NC). We used the paired t test to evaluate pre–post comparisons and set statistical significance at P < .05.
RESULTS
Among the first cohort of 74 participants, 62% were Native Hawaiian, 25% were Filipino, and 5% were White. This mirrored the Moloka'i population, which is approximately 64% Native Hawaiian. Participants were primarily women (92%), with an average age of 41 years. One of KAO's greatest successes was a low attrition rate, with 66 participants (89%) attending all 12 sessions. Comparisons of clinical measures (Table 2) at intake and at the end of 12 weeks showed statistically significant improvements for weight (Δ = –7.4 lbs; P < .001), systolic blood pressure (Δ = –3.8 mm Hg; P = .027), diastolic blood pressure (Δ = –4.6 mm Hg; P < .001), total cholesterol (Δ = –9.7 mg/dL; P < .001), and low-density lipoprotein (Δ = –11.1 mg/dL; P < .001).
TABLE 2.
Pre–Post Clinical Measures in the Ke ‘Ano Ola Healthy Lifestyle Program: Moloka‘i, HI, 2008
| Measure | Baseline, Mean (SD) | After Intervention, Mean (SD) | Change in the Mean (SD) | P |
| Fasting blood glucose, mg/dL (n = 54) | 103.5 (30.6) | 100.6 (26.4) | −3.0 (18.7) | .25 |
| Body weight, lbs (n = 61) | 211.7 (55.9) | 204.4 (53.8) | −7.4 (6.7) | <.001 |
| Systolic blood pressure, mm Hg (n = 61) | 127.2 (15.0) | 123.4 (13.1) | −3.8 (13.0) | .027 |
| Diastolic blood pressure, mm Hg (n = 61) | 83.1 (10.7) | 78.5 (8.2) | −4.6 (10.6) | .001 |
| Total cholesterol, mg/dL (n = 61) | 187.8 (37.2) | 178.0 (33.9) | −9.7 (22.0) | .001 |
| Low-density lipoprotein, mg/dL (n = 53) | 112.8 (33.2) | 101.7 (33.5) | −11.1 (20.6) | <.001 |
| High-density lipoprotein, mg/dL (n = 60) | 44.9 (15.9) | 45.6 (16.2) | 0.78 (10.5) | .57 |
| Triglycerides, mg/dL (n = 61) | 159.2 (118.4) | 133.8 (71.8) | −25.4 (86.1) | .025 |
For each measured variable, the majority of participants showed clinical improvements at the postintervention assessment. We observed decreases in diastolic blood pressure (55% of participants), systolic blood pressure (57%), blood glucose (57%), triglycerides (58%), total cholesterol (62%), low-density lipoprotein (75%), and body weight (90%). High-density lipoprotein increased in 53% of participants.
DISCUSSION
In a 6-month clinical trial, Pounds Off with Empowerment, an intensive lifestyle intervention, achieved an average weight loss of 2.6 kg (5.73 lbs); in comparison, KAO participants lost an average of 7.5 pounds in 3 months.6 KAO's low attrition rate may have been partially attributable to social support: each participant adopted a buddy or a small group to provide and receive support, in addition to encouragement from the larger support group. Many participants carpooled to classes and also made sure that their buddies were attending classes. We believe that their investment of time and money motivated participants to maximize the program's benefits by incorporating the KAO concepts in their lifestyle. Classes started on time and were filled with relevant and practical information. The staff was actively involved in the educational sessions. All meals were prepared from foods that were available in and affordable to this community, whose 13.5% unemployment rate is among the nation's highest.7 For example, venison or fish were the primary protein source for most meals.
Our pilot study did not have a control group and may have been subject to selection bias and the Hawthorne effect. Nevertheless, our findings demonstrate the contribution made by strong commitment and positive role modeling from program leaders, social and group support, and community involvement and feedback to a successful healthy lifestyle program in a predominantly Native Hawaiian community. Evaluations showed that satisfied participants (1) were more likely to use a buddy system as support, and (2) had significant improvements in clinical outcomes, including blood pressure, blood lipid control, and weight reduction.
Future KAO programs will incorporate a significant behavioral health component, which will feature goal setting and motivational interviews conducted by a psychologist to assess participants' level in Prochaska's stage-of-change model.8 The eating-profile questionnaire will be administered and evaluated.9 KAO meal plans and physical activity programs will be tailored to each participant's stage of readiness. Food diaries and recipes used for cooking demonstrations will be reviewed and evaluated by a registered dietitian. The community will participate in expansion of this program to other Na Pu‘uwai sites, and feedback from evaluations will be incorporated.
Early results from a culturally appropriate community-based lifestyle intervention found significant clinical improvements among 61 participants. This program could provide an example for other lifestyle intervention programs conducted in underserved minority communities.
Acknowledgments
This work was supported by Na Pu‘uwai, a Native Hawaiian health care system supported by the Department of Health and Human Services, Health Resources and Services Administration (grant H1CCS00015).
We acknowledge the support of the Na Pu‘uwai staff and the Moloka‘i community throughout all stages of this program. We also thank the medical community of Moloka‘i, who continue to support this program.
Human Participant Protection
No outside protocol approval was needed for this study because all participants were clients of Na Pu‘uwai, which obtains informed consent and follows its own human participant protection protocol.
References
- 1.State Department of Health Hawai‘i Behavioral Risk Factor Surveillance Survey. Available at: http://hawaii.gov/health/statistics/brfss/index.html. Accessed June 8, 2009
- 2.United Health Foundation America's health ratings. Available at: http://www.americashealthrankings.org/2008/states/hi.html. Accessed June 8, 2009
- 3.Mau MK, Glanz K, Severio R, Grove JS, Johnson B, Curb JD. Mediators of lifestyle behavior change in Native Hawaiians. Diabetes Care 2001;24(10):1770–1775 [DOI] [PubMed] [Google Scholar]
- 4.Wing RR, Jeffery RW. Benefits of recruiting participants with friends and increasing social support for weight loss and maintenance. J Consult Clin Psychol 1999;67(1):132–138 [DOI] [PubMed] [Google Scholar]
- 5.Nacapoy AH, Kaholokula JK, West MR, Dillard AY, Leake A, Kekauoha PK. Partnerships to address obesity disparities in Hawai‘i: the PILI ‘Ohana Project. Hawaii Med J 2008;67(9):237–241 [PMC free article] [PubMed] [Google Scholar]
- 6.Mayer-Davis EJ, D'Antonio AM, Smith SM, Kirkner G, Martin SL, Parra-Medina D. Pounds off with empowerment (POWER): a clinical trial of weight management strategies for Black and White adults with diabetes who live in medically underserved rural communities. Am J Public Health 2004;94(10):1736–1742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Department of Labor and Industrial Relations Hawai‘i workforce informer. Available at: http://www.hiwi.org/admin/uploadedPublications/1019_URATE_current.pdf. Accessed November 10, 2009
- 8.Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot 1997;12(1):38–48 [DOI] [PubMed] [Google Scholar]
- 9.Last C. The 5 Reasons Why We Overeat: How to Develop a Long-Term Weight Control Plan That's Right for You New York, NY: Carol Publishing Group; 1999 [Google Scholar]