Abstract
Objectives. We conducted a controlled trial of a public education and provider intervention to increase colorectal cancer (CRC) screening rates among Vietnamese Americans, who typically have lower rates than non-Hispanic Whites.
Methods. The public education intervention included a Vietnamese-language CRC screening media campaign, distribution of health educational material, and a hotline. The provider intervention consisted of continuing medical education seminars, newsletters, and DVDs. Vietnamese in Alameda and Santa Clara Counties, California, received the intervention from 2004 to 2006; Vietnamese in Harris County, Texas, were controls and received no intervention. A quasi-experimental study design with pre- and postintervention surveys of the same 533 participants was used to evaluate the combined intervention.
Results. The postintervention-to-preintervention odds ratio for having ever had a sigmoidoscopy or colonoscopy was 1.4 times greater in the intervention community than in the control community. Knowledge and attitudes mediated the effect of the intervention on CRC screening behavior. Media exposure mediated the effect of the intervention on knowledge.
Conclusions. Improving CRC knowledge through the media contributed to the effectiveness of the intervention.
Colorectal cancer (CRC) is the fourth most common cancer in the United States1 and the third most common among both Vietnamese men and women in California.2 Asian Americans have lower CRC screening rates than do non-Hispanic Whites, and there is variation in screening rates among Asian Americans.3 CRC screening is effective at reducing mortality both by removing premalignant polyps and detecting early cancers.4–9 The US Preventive Services Task Force recommends a fecal occult blood test (FOBT), sigmoidoscopy, or colonoscopy for adults, beginning at age 50 years and continuing until age 75 years.10
Despite these recommendations and the effectiveness of CRC screening, screening rates remain low. Among Americans aged 50 years or older, only 18.7% had an FOBT during the preceding year and only 50.6% had a sigmoidoscopy or colonoscopy during the preceding 10 years.11 Vietnamese Americans have lower CRC screening rates than do non-Hispanic Whites and some other Asian Americans.3,12–14 In California, the proportions who have ever had an FOBT, ever had a sigmoidoscopy or colonoscopy, had an FOBT in the past year, and had a sigmoidoscopy or colonoscopy in the past 5 years are significantly lower among Vietnamese Americans (29%, 36%, 18%, and 34%, respectively) than among non-Hispanic Whites (58%, 57%, 26%, and 52%, respectively).14
Vietnamese Americans are 1 of the fastest-growing US populations. From 1990 to 2000, their numbers grew by 83%, from 614 547 to 1 122 528.15,16 Those aged 50 years and older were almost all born in Vietnam and maintain their traditional culture and language.17 Vietnamese Americans are relatively poorer, more socially and economically disadvantaged, more medically underserved, and have more language barriers than do non-Hispanic Whites. Compared with non-Hispanic Whites nationally, Vietnamese are twice as likely to be living below the poverty level (16% versus 9%) and have only about two thirds the per capita income ($15 655 versus $23 918). In addition, 31% of Vietnamese Americans speak English not well or not at all and 46% of Vietnamese households are linguistically isolated (have no one aged 14 years or older who speaks English at least very well).18 In Santa Clara County, California, Vietnamese aged 50 to 74 years are significantly more likely not to have graduated from college (74% versus 53%), to be uninsured (11% versus 2%), to be unemployed or a homemaker (29% versus 12%), and to rate their health as fair or poor (52% versus 46%) than are non-Hispanic Whites.12 To reduce disparities in CRC screening, we conducted a controlled trial to increase CRC screening rates among Vietnamese Americans.
METHODS
Participants were drawn from a sampling frame of individuals listed in the study area telephone directories with the 37 most common Vietnamese surnames (Bui, Cao, Diep, Duong, Dao, Dang, Dinh, Doan, Do, Ha, Hoang, Huynh, Ho, Khuu, Lam, Le, Ly, Luong, Luu, Mai, Ngo, Nguyen, Pham, Phan, Phung, Quach, Quan, Ta, To, Ton, Tran, Trieu, Trinh, Truong, Vu, Vo, and Vuong) used in previous studies.19–24 Eligibility criteria included (1) self-identification as Vietnamese or Vietnamese American; (2) age 50 to 74 years; (3) residence in Alameda or Santa Clara Counties, California, or Harris County, Texas, and intention to stay in the study area for the 2 years of intervention; and (4) ability to understand either Vietnamese or English. The adjacent California counties of Alameda and Santa Clara comprised the intervention community because it has the second greatest concentration of Vietnamese Americans in the United States; has a developed Vietnamese-language print, radio, and television media market; and is close to the investigators. To reduce intervention cross-contamination, we chose an out-of-state community as the control (no intervention). The control community, Harris County, Texas, has the highest concentration of Vietnamese Americans outside of California and a developed Vietnamese-language media market; a prior study20 found that the demographic characteristics of its Vietnamese residents were similar to those of Vietnamese in Santa Clara County (mean age = 41.7 years versus 42.6 years; percentage of college graduates = 74% versus 72%, percentage speaking limited English [none, poor, or fair] = 77% versus 77%).
Study Design
We used a quasi-experimental study design and conducted pre- and postintervention surveys with the same 533 participants to evaluate the effectiveness of the intervention. The surveys were pilot tested prior to implementation for quality control. From July to September 2004, we conducted a 20-minute preintervention survey in either Vietnamese or English using a computer-assisted telephone interviewing system, with roughly equal numbers of participants in each community. The sources, questionnaire development process, and findings of the preintervention survey have been previously described.17 We conducted a 2-year intervention immediately after the preintervention survey. The postintervention survey, conducted from October 2006 to April 2007, was identical to the preintervention survey, except that the questions on birth year, gender, number of years in United States, and ability to speak English were not repeated. To reach respondents, a minimum of 10 call attempts were made to active telephone numbers at different times of day and days of the week. Each participant received $10 for completing the preintervention survey and $20 for the postintervention survey.
Theoretical Framework
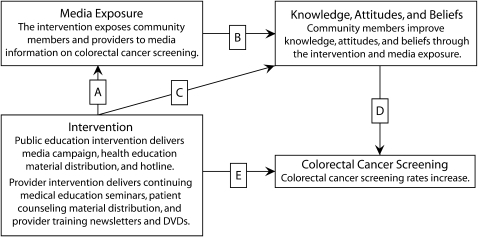
The pathways framework of Hiatt et al.25 provided the theoretical basis for the intervention. In applying this framework to cancer screening26 and Vietnamese Americans,27,28 McPhee et al.27 argued that Vietnamese Americans are more likely to be screened if their knowledge and attitudes are concordant with screening behaviors. In this study, we chose to focus on the public and provider pathways using a public education and provider intervention. As shown in Figure 1, the intervention was designed to expose community members and providers to media information on CRC screening (pathway A). We expected that community members would improve knowledge, attitudes, and beliefs through the intervention (pathway C) and media exposure (pathway B), and that improved knowledge, attitudes, and beliefs would lead to increases in CRC screening rates (pathway D). According to this framework, knowledge, attitudes, and beliefs mediate the effect of the intervention on CRC screening behavior (pathways C and D), and media exposure serves as a mediator (pathways A and B) between the intervention and knowledge, attitudes, and beliefs. Pathway E represents effects of the intervention other than those mediated by the knowledge, attitudes, and beliefs of community members—for example, increased recommendation of screening by Vietnamese physicians.
FIGURE 1.
Pathways to a framework of colorectal cancer screening among Vietnamese Americans: Alameda and Santa Clara Counties, CA, and Harris County, TX; 2004–2007.
Formative Research
To improve the cultural and linguistic competency of the intervention, we conducted focus groups to identify Vietnamese American health information sources and credibility, media use and preferences, and intervention approaches. The focus group findings have been previously reported.29 These findings were used to inform the development of the intervention, health education and promotional materials (booklet and penlight), and media campaign materials (6 print articles, 1 television talk show, 14 newspaper ads, 9 radio ads, and 4 television ads). All materials were produced in Vietnamese at a fifth-grade literacy level and cognitively tested with 23 Vietnamese Americans aged 50 years or older by trained bilingual and bicultural staff.
Intervention
The intervention had public education and provider components. The public education component included a media campaign on CRC screening, the production and distribution of health education and promotional material, and a hotline. We conducted the media campaign using established Vietnamese-language media outlets. We chose spokespersons in the ads (e.g., health care providers, cancer survivors, happy and healthy community members, and Vietnamese media personalities) on the basis of focus group participants' recommendations. We chose the media outlets based on the Vietnamese American community's preference as indicated in the preintervention survey. We printed ads in 729 newspaper issues, resulting in an estimated 5 346 000 consumer exposures; aired radio ads in 1323 radio spots, resulting in an estimated 26 730 000 consumer exposures; and broadcast television ads in 258 television spots, resulting in an estimated 8 515 000 consumer exposures. We produced a 32-page bilingual booklet, Kham Ruot Gia De Song Tho (For Long Life, Test the Colon) in 4 colors on 80-lb glossy stock and a promotional penlight with the same slogan. We distributed 6337 booklets and 1585 penlights to the public at community sites, such as community-based organizations, health and human services agencies, and businesses, as well as at community events, such as the Vietnamese Tet Lunar New Year celebration and health fairs. We staffed a bilingual hotline and answered 586 calls about CRC screening.
The provider component consisted of continuing medical education seminars and distribution of patient counseling materials, reminder items, provider training newsletters, and DVDs. We distributed 5290 booklets and 647 reminder penlights to hospitals, clinics, and physicians' offices to assist health care providers in counseling their patients and in reminding them to keep their CRC screening appointments. We also distributed 1000 copies of 4 issues of provider newsletters and 500 copies of provider training DVDs to Vietnamese American physicians. We held 2 continuing medical education seminars for Vietnamese American physicians in May and November 2005 in Santa Clara County. Forty-two physicians attended the first seminar and 35 attended the second seminar. At both seminars, most physicians were male, aged 50 years or older, in general internal medicine or family medicine, in solo or group private practice, and Vietnamese medical school graduates. The seminars were effective at increasing CRC knowledge among Vietnamese American physicians.30
Measures
Outcome variables were (1) having ever had an FOBT, (2) having ever had a sigmoidoscopy or colonoscopy, (3) having had a screening FOBT in the past year (defined as the calendar year before the interview), and (4) having had a screening sigmoidoscopy or colonoscopy in the past 5 years. A screening FOBT, sigmoidoscopy, or colonoscopy was defined as having a test specifically for screening for CRC and not for following up symptoms or previous abnormal test results. Sigmoidoscopy and colonoscopy were reported together because sizable portions of participants did not distinguish sigmoidoscopy from colonoscopy. Having a sigmoidoscopy or colonoscopy within the past 5 years was used as a measure of being up to date because this measurement has been used in previous studies.14
Independent variables included the following: demographic characteristics (age [50–64, 65–74 years], gender, marital status, education, income, employment status, years in the United States, English fluency, and self-perceived health status), health care access characteristics (health insurance coverage [private; public such as Medicare, Medicaid, or MediCal; access to county indigent care; or none], having a regular place of care, having a personal doctor, and having a Vietnamese personal doctor), knowledge (ever heard of FOBT, ever heard of sigmoidoscopy or colonoscopy, and ever heard of colon polyp), attitudes and beliefs (worrying about colon cancer, thinking one might get colon cancer, thinking one needs an FOBT even if feeling healthy, thinking one needs a sigmoidoscopy or colonoscopy even if feeling healthy, being afraid an FOBT might find cancer, being afraid a sigmoidoscopy or colonoscopy might find cancer, thinking a sigmoidoscopy or colonoscopy painful, and thinking sigmoidoscopy or colonoscopy preparation troublesome), and exposure to media elements regarding CRC (having seen a booklet, having read a newspaper article, having seen a newspaper ad, having heard a radio ad, and having seen a television ad). The choice of these independent variables was based on results of preintervention data analysis17 and other cancer screening studies in this population.23,31–34
Statistical Analysis
We analyzed the data using SAS versions 9.1 and 9.2 (SAS Institute Inc, Cary, North Carolina). In a retention analysis, the χ2 test was used to compare the demographic characteristics of retained and nonretained participants. The χ2 test was also used to assess the similarity of the study arms with respect to the demographic and health care access characteristics of retained participants. The effectiveness of the intervention was first evaluated by comparing the study arms with respect to changes from pre- to postintervention in CRC screening behaviors, knowledge, attitudes, beliefs, and exposure to media elements. The McNemar test was used to evaluate changes within each arm, and the z test that accounted for pre- and postintervention correlation was used to evaluate the differences between the study arms. We used multiple logistic regression models with repeated measures to assess the effects on each outcome of study arm, time (preintervention vs postintervention), and their interaction (representing the intervention effect), controlling for demographics and health care characteristics.
Generalized estimating equations were used to account for intraindividual correlation of responses. Using the method of Baron and Kenny,35 we performed mediation analysis for any outcome with a significant intervention effect. The following mediation mechanisms were posited: (1) knowledge, attitudes, and beliefs would mediate the effect of the intervention on outcome, and (2) media exposure would mediate the effect of the intervention on knowledge, attitudes, and beliefs. Repeated-measures multiple logistic regression models were used to assess the effects of the intervention on each knowledge, attitude, and belief variable; a proportional odds model36 was used to assess the effect of the intervention on media exposure (number of types of media reported). The potential mediators were then included as independent variables in models assessing intervention effects, as follows: (1) knowledge, attitudes, and beliefs were added to the outcome model, and then (2) media exposure was added to the models of knowledge, attitudes, and beliefs.
RESULTS
The preintervention survey response rate was 86%.17 By postintervention, of the 894 pilot and main study participants completing the preintervention survey, 100 respondents had dropped out, had moved, or no longer had a valid telephone number; 44 had disconnected numbers; 34 had a wrong number or could not be found; 51 refused the survey; and 116 were not available to be interviewed during the study period. A total of 549 pilot and main participants completed both the pre- and postintervention surveys, yielding a retention rate of 61%. After we excluded 16 pilot participants, 533 participants were included in the analysis. Comparisons of the characteristics of retained and nonretained participants showed there was an association with several baseline characteristics. Retained participants were significantly more likely to be high school or college graduates, be male, have an income of less than $20 000, have heard of colon polyps, agree that a healthy person needs an FOBT, agree that a healthy person needs a sigmoidoscopy or colonoscopy, have seen a newspaper ad about CRC, have ever had a sigmoidoscopy or colonoscopy, and have had a screening FOBT in the past year. However, differences between the study arms in retention rates were not statistically significant.
Comparison of the demographic and health care access characteristics of the control and intervention study participants retained at postintervention showed that intervention participants were more likely to have a household income of less than $20 000; to be unemployed; to have public insurance such as MediCal, Medicaid, or Medicare; to have a personal doctor; and were less likely to speak English fluently or well (see supplemental table, available in the online version of this article at http://www.ajph.org). Table 1 shows the CRC screening behaviors, knowledge, attitudes, and beliefs and exposure to media elements of Vietnamese American participants at pre- and postintervention, by community. The effectiveness of the intervention was first evaluated by comparing the study arms with respect to changes in CRC screening behaviors from pre- to postintervention. The differences in change between the intervention and control groups in the proportions of participants who reported changes in behaviors, knowledge, attitudes, and beliefs from pre- to postintervention were large and statistically significant: 11 percentage points for having ever had a screening sigmoidoscopy or colonoscopy, 10 percentage points for having had a screening sigmoidoscopy or colonoscopy in the past 5 years, 13 percentage points both for having ever heard of FOBT and having ever heard of colon polyps, 11 percentage points for thinking one needs a sigmoidoscopy or colonoscopy even if healthy, and –15 percentage points for thinking sigmoidoscopy or colonoscopy is painful.
TABLE 1.
Vietnamese Americans' Behaviors, Knowledge, Attitudes, and Beliefs Regarding Colorectal Cancer Screening and Exposure to Media Campaign on Colorectal Cancer Screening at Pre- and Postintervention: Alameda and Santa Clara Counties, CA and Harris County, TX; 2004–2007
| Control Community |
Intervention Community |
||||||
| Measure | Preintervention, % | Postintervention, % | Pa | Preintervention, % | Postintervention, % | Pa | Pb |
| Behavior | |||||||
| Ever had FOBT | 41 | 50 | .006 | 57 | 71 | <.001 | .254 |
| Ever had sigmoidoscopy or colonoscopy | 37 | 47 | <.001 | 44 | 65 | <.001 | .006 |
| Had screening FOBT in past yc | 21 | 26 | .096 | 27 | 36 | .003 | .301 |
| Had screening sigmoidoscopy or colonoscopy in past 5 yc | 16 | 30 | <.001 | 20 | 44 | <.001 | .035 |
| Knowledge | |||||||
| Ever heard of FOBT | 59 | 70 | .001 | 52 | 76 | <.001 | .007 |
| Ever heard of sigmoidoscopy or colonoscopy | 56 | 68 | .001 | 59 | 74 | <.001 | .522 |
| Ever heard of colon polyp | 56 | 67 | .001 | 53 | 77 | <.001 | .006 |
| Attitudes and beliefs | |||||||
| Worry about colon cancer | 27 | 43 | <.001 | 38 | 53 | <.001 | .833 |
| Think might get colon cancer | 29 | 27 | .547 | 27 | 33 | .056 | .076 |
| Think need FOBT even if feeling healthy | 48 | 55 | .088 | 48 | 65 | <.001 | .057 |
| Think need sigmoidoscopy or colonoscopy even if feeling healthy | 40 | 50 | .010 | 39 | 60 | <.001 | .047 |
| Afraid FOBT might find cancer | 13 | 11 | .446 | 16 | 10 | .039 | .348 |
| Afraid sigmoidoscopy or colonoscopy might find cancer | 12 | 10 | .398 | 17 | 9 | .001 | .075 |
| Think sigmoidoscopy or colonoscopy painful | 30 | 26 | .010 | 46 | 28 | <.001 | .001 |
| Think sigmoidoscopy or colonoscopy preparation troublesome | 38 | 30 | .033 | 39 | 31 | .026 | .986 |
| Exposure to media elements | |||||||
| Have seen booklet | 8 | 17 | .001 | 13 | 34 | <.001 | .002 |
| Have read newspaper article | 30 | 44 | <.001 | 33 | 54 | <.001 | .104 |
| Have seen newspaper ad | 30 | 48 | <.001 | 31 | 62 | <.001 | .01 |
| Have heard radio ad | 47 | 50 | .458 | 29 | 60 | <.001 | <.001 |
| Have seen television ad | 11 | 17 | .051 | 20 | 50 | <.001 | <.001 |
Note. FOBT = fecal occult blood test. The intervention community was Alameda and Santa Clara Counties, CA; the control community was Harris County, TX.
P from McNemar test.
Difference between intervention and control. P from z test (difference in change in proportion from pre- to postintervention).
A screening test is defined as a report of having a test specifically for screening for colorectal cancer and not for following-up symptoms or previous abnormal test results.
Comparisons of the study arms in exposure to media elements regarding CRC showed that the media campaign was effective in reaching the Vietnamese American participants in the intervention community by booklets and newspaper, radio, and television advertisements, although not by newspaper articles. Table 2 shows multiple logistic regression models of having ever had a sigmoidoscopy or colonoscopy. The postintervention to preintervention odds ratio (OR) for having ever had a sigmoidoscopy or colonoscopy was greater in the intervention community than in the control community (OR = 1.44; 95% confidence interval [CI] = 1.03, 1.99), after control for demographic and health care access characteristics. Having private and public health insurance coverage was associated with having ever had a sigmoidoscopy or colonoscopy. Multiple logistic regression models for the other 3 outcome variables did not yield significant intervention effects.
TABLE 2.
Multiple Logistic Regression Models of Vietnamese Americans Having Ever Had Sigmoidoscopy or Colonoscopy: Alameda and Santa Clara Counties, CA, and Harris County, TX; 2004–2007
| Variables | Basic Outcome Model, OR (95% CI) | Mediator Model, OR (95% CI) |
| Intervention effect | 1.44* (1.03, 1.99) | 1.20 (0.85, 1.69) |
| Health insurance coverage | ||
| Have private insurance | 2.15* (1.42, 3.27) | 2.04* (1.34, 3.12) |
| Have public insurance | 1.72* (1.15, 2.57) | 1.67* (1.10, 2.52) |
| Have access to county indigent care | 1.02 (0.64, 1.61) | 0.99 (0.61, 1.60) |
| Have regular place of care | 1.32 (0.99, 1.75) | 1.24 (0.92, 1.67) |
| Have personal doctor | 1.32 (0.87, 2.00) | 1.38 (0.88, 2.15) |
| Have Vietnamese personal doctor | 0.83 (0.58, 1.18) | 0.78 (0.53, 1.15) |
| Knowledge, attitudes, and beliefs | ||
| Have heard of colon polyps | NA | 1.73* (1.32, 2.27) |
| Worry about colon cancer | NA | 0.97 (0.75, 1.26) |
| Think might get colon cancer | NA | 1.43* (1.09, 1.88) |
| Think need sigmoidoscopy or colonoscopy even if feeling healthy | NA | 1.11 (0.87, 1.40) |
| Afraid sigmoidoscopy or colonoscopy might find cancer | NA | 0.72 (0.50, 1.04) |
| Think sigmoidoscopy or colonoscopy painful | NA | 0.68* (0.52, 0.90) |
| Think sigmoidoscopy or colonoscopy preparation troublesome | NA | 1.46* (1.14, 1.87) |
Note. CI = confidence interval; NA = not applicable to the basic outcome model; OR = odds ratio. Both the basic outcome model and the mediator model included terms for time, place, and intervention effect and adjusted for age (50–64, 65–74 years), gender, marital status, education, income, employment status, years in the United States, English fluency, health status, and having health insurance coverage, a regular place of care, a personal doctor, and a Vietnamese personal doctor. The Mediator Model also included knowledge, attitude, and belief variables.
*P < .05.
We performed mediation analysis using the method of Baron and Kenny.35 As shown in Table 2, when knowledge, attitude, and belief variables were added to the multiple logistic regression model of having ever had a sigmoidoscopy or colonoscopy, the OR for the intervention effect variable attenuated from 1.44 to 1.20, and 4 of the 7 knowledge, attitude, and belief variables, including having heard of colon polyps and thinking sigmoidoscopy or colonoscopy painful, were significant in the predicted direction. In addition, in the regression models of intervention on knowledge and attitudes (Table 3), intervention effects on having ever heard of colon polyps and thinking sigmoidoscopy or colonoscopy painful were statistically significant. Therefore, having heard of colon polyps and thinking sigmoidoscopy or colonoscopy painful mediated the effect of the intervention on having ever had a sigmoidoscopy or colonoscopy.
TABLE 3.
Regression Models of Colorectal Cancer Screening Knowledge, Attitudes, and Beliefs Among Vietnamese Americans: Alameda and Santa Clara Counties, CA and Harris County, TX; 2004–2007
| Basic Model: Intervention Effect, OR (95% CI) | Mediator Model: Intervention Effect, OR (95% CI) | Media Exposure,a OR (95% CI) | |
| Have heard of colon polyps | 1.87* (1.16, 3.01) | 1.42 (0.86, 2.36) | 1.43* (1.28, 1.60) |
| Worry about colon cancer | 0.85 (0.55, 1.32) | 0.69 (0.44, 1.10) | 1.28* (1.16, 1.40) |
| Think might get colon cancer | 1.43 (0.90, 2.29) | 1.16 (0.72, 1.89) | 1.28* (1.16, 1.42) |
| Think need sigmoidoscopy or colonoscopy if feeling healthy | 1.40 (0.88, 2.20) | 1.22 (0.76, 1.96) | 1.17* (1.07, 1.29) |
| Afraid sigmoidoscopy or colonoscopy will find colon cancer | 0.61 (0.30, 1.22) | 0.58 (0.28, 1.21) | 1.05 (0.91, 1.22) |
| Think sigmoidoscopy or colonoscopy painful | 0.54* (0.34, 0.84) | 0.52* (0.33, 0.83) | 1.02 (0.93, 1.13) |
| Think sigmoidoscopy or colonoscopy preparation troublesome | 0.98 (0.60, 1.58) | 1.04 (0.64, 1.69) | 0.93 (0.85, 1.03) |
Note. CI = confidence interval; OR = odds ratio.
Media exposure is defined as the number of types of media reported.
*P < .05.
As shown in Table 3, when media exposure was added to the regression model for ever having heard of colon polyps, the OR of the intervention effect variable attenuated from 1.87 to 1.42, and the media exposure variable was significant. In a separate regression model, media exposure was significantly affected by the intervention (OR = 2.95; 95% CI = 2.08, 4.18). Thus, media exposure mediated the effect of the intervention on having ever heard of colon polyps.
DISCUSSION
Our study has several significant findings. First, the intervention was effective at increasing sigmoidoscopy or colonoscopy screening rates among Vietnamese American men and women. Previous studies have demonstrated that breast and cervical cancer screening rates could be improved among Vietnamese American women.23,31,33,34 The rates of having had a screening FOBT within the past year and of having had a screening sigmoidoscopy or colonoscopy in the past 5 years at preintervention were comparable to the rates reported by Walsh et al.13 The rate of having ever had a sigmoidoscopy or colonoscopy at preintervention was comparable to the rates reported by Walsh et al.13 and Wong et al.14 Second, the effect size on the outcome of having ever had a sigmoidoscopy or colonoscopy was large (11 percentage points). We were not able to observe significant effects for up-to-date behaviors involving sigmoidoscopy or colonoscopy, possibly because we did not follow the study participants long enough for them make these behavior changes (the intervals for sigmoidoscopy and colonoscopy are 5 and 10 years, respectively). Future studies should have intervention and observation periods long enough for participants to be able to make these behavior changes. Increasing public and private insurance coverage would likely improve screening in this population. Third, CRC screening behavior changes did not occur as a direct result of the intervention but through intermediary steps involving media exposure and knowledge and attitudes.
This study's strengths lie in its formative research, cultural and linguistic competency, and analytical methods. Focus group research, cognitive testing, and the development of materials in-language (i.e., in the participants' native language) and at low literacy levels improved the cultural and linguistic competency of the intervention. Mediation analyses elucidated the pathways from intervention to behavior changes.
There are limitations to this study. First, the listed surname sample excluded households that did not have telephones or had unlisted telephone numbers. Second, the results of this study may not be generalizable to all Vietnamese in the United States, because the sample was drawn from 2 urban areas with high concentrations of Vietnamese Americans. Third, screening out persons who anticipated moving from the study areas in the next 2 years introduced a systematic bias against more mobile individuals. Fourth, the retention analysis revealed that retained participants had several characteristics favorable to CRC screening compared with nonretained participants; this fact may reduce the external validity of the findings.
Fifth, the study was not able to tease out the comparative effectiveness of each subtype of intervention (e.g., public education versus provider). Different mechanisms may be operating for different intervention components. However, prior research among Vietnamese Americans shows the effectiveness of a multifaceted intervention on cancer screening.22,23 Sixth, our measure of knowledge (having heard of colon polyps) was extremely limited. Seventh, secular trends—that is, exogenous changes at work in the communities, such as the natural diffusion of colorectal cancer screening—may have been stronger in the intervention area than in the control area, thereby inflating the apparent intervention effect. Eighth, testing (Hawthorne) effects (i.e., the effects of repeating the same questions) may have overestimated responses in the postintervention survey. However, secular trends and testing effects influenced both study arms. Analyses comparing the study arms for change between pre- and postintervention surveys and multivariate analyses accounted for these effects. Because this was not a randomized trial, there is always the possibility that secular trends in the intervention area were stronger than in the control area. Finally, the quasi-experimental design ensured that the study arms were not comparable in all respects at baseline, and pre–post differences may have been affected by regression to the mean. However, we accounted for community differences to the extent possible by controlling for demographic and health care access factors in our models.
The intervention was effective at increasing CRC screening among Vietnamese American men and women. The increases in CRC screening rates were large. Improving knowledge through use of the media was the key to the intervention's effectiveness. This successful intervention can be disseminated to reduce disparities in CRC screening among Vietnamese Americans and other racial/ethnic, poor, or immigrant communities and could be applied to the control of other forms of cancer, cardiovascular disease, or tobacco, diabetes, and obesity. Programs promoting or expanding CRC screening access should use in-language and culturally competent booklets along with newspaper, radio, and television advertisements in outreach. Expanding health insurance coverage may further increase CRC screening in this population. The elucidation of the pathways between intervention and behavior changes offers alternative health education strategies. Although media exposure alone may not directly change CRC screening behaviors, in conjunction with other complementary intervention activities it may affect these behaviors through changes in knowledge.
Acknowledgments
This research was supported by National Cancer Institute (grant R01 CA 100856).
This research was presented in part at the American Public Health Association annual meetings in Washington, DC, November 3–7, 2007, and San Diego, CA, October 25–29, 2008.
We thank Chi Nguyen for preparing and formatting the article for publication.
Human Participant Protection
The institutional review boards of the Northern California Cancer Center and the University of California, San Francisco, approved the research protocol.
References
- 1.Cancer Facts and Figures 2008 Atlanta, GA: America Cancer Society; 2008 [Google Scholar]
- 2.Cockburn M, Deapen M, Cancer Incidence and Mortality in California: Trends by Race/Ethnicity, 1988–2001 Los Angeles, CA: Los Angeles Surveillance Program, University of California; 2004 [Google Scholar]
- 3.Maxwell AE, Crespi CM. Trends in colorectal cancer screening utilization among ethnic groups in California: are we closing the gap? Cancer Epidemiol Biomarkers Prev 2009;18(3):752–759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Newcomb PA, Norfleet RG, Storer BE, Surawica TS, Marcus PM. Screening sigmoidoscopy and colorectal cancer mortality. J Natl Cancer Inst 1992;84(20):1572–1575 [DOI] [PubMed] [Google Scholar]
- 5.Selby JV, Friedman GD, Quesenbery CP, Weiss NS. A case–control study of screening sigmoidoscopy and mortality from colorectal cancer. N Engl J Med 1992;326(10):653–657 [DOI] [PubMed] [Google Scholar]
- 6.Selby JV, Friedman GD, Quesenbery CP, Weiss NS. Effect of fecal occult blood testing on mortality from colorectal cancer: a case–control study. Ann Intern Med 1993;118(1):1–6 [DOI] [PubMed] [Google Scholar]
- 7.Mandel JS, Bond JH, Church TR, et al. Reducing mortality from colorectal cancer by screening for fecal occult blood. Minnesota Colon Cancer Control Study. N Engl J Med 1993;328(19):1365–1371 [DOI] [PubMed] [Google Scholar]
- 8.Hardcastle JD, Chamberlain JO, Robinson MHE, et al. Randomised controlled trial of faecal-occult-blood screening for colorectal cancer. Lancet 1996;348(9040):1472–1477 [DOI] [PubMed] [Google Scholar]
- 9.Kronborg O, Fenger C, Olsen J, Jorgensen OD, Sondergaard O. Randomised study of screening for colorectal cancer with faecal-occult-blood test. Lancet 1996;348(9040):1467–1471 [DOI] [PubMed] [Google Scholar]
- 10.US Preventive Services Task Force Screening for colorectal cancer: US Preventive Services Task Force recommendation statement. Ann Intern Med 2008;149(9):627–637 [DOI] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention Increased use of colorectal cancer tests—United States, 2002 and 2004. MMWR Morb Mortal Wkly Rep 2006;55(11):308–311 [PubMed] [Google Scholar]
- 12.Jenkins CN, McPhee SJ, Bird JA, Bonilla N-TH. Cancer risks and prevention practices among Vietnamese refugees. West J Med 1990;153(1):34–39 [PMC free article] [PubMed] [Google Scholar]
- 13.Walsh JME, Kaplan CP, Nguyen B, Gildengorin G, McPhee SJ, Perez-Stable EJ. Barriers to colorectal cancer screening in Latino and Vietnamese Americans compared with non-Latino White Americans. J Gen Intern Med 2004;19(2):156–166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wong ST, Gildengorin G, Nguyen T, Mock J. Disparities in colorectal cancer screening rates among Asian Americans and non-Latino Whites. Cancer 2005;104(suppl 12):2940–2947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.1990 Profiles of Asians and Pacific Islanders: Selected Characteristics Washington, DC: US Census Bureau; 1990 [Google Scholar]
- 16.Profiles of General Demographic Characteristics 2000: 2000 Census of Population and Housing, United States Washington, DC: US Census Bureau; 2001 [Google Scholar]
- 17.Nguyen BH, McPhee SJ, Stewart SL, Doan HT. Colorectal cancer screening in Vietnamese Americans. J Cancer Educ 2008;23(1):37–44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.US Census Bureau Census 2000 summary file 4, tables PCT38, PCT42, PCT130, and PCT142. Available at: http://factfinder.census.gov. Accessed March 19, 2009
- 19.Swallen KC, Glaser SL, Stewart SL, West DW, Jenkins C, McPhee S. Accuracy of racial classification of Vietnamese patients in a population-based cancer registry. Ethn Dis 1998;8(2):218–227 [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention Behavioral risk factor survey of Vietnamese—California, 1991. MMWR Morb Mortal Wkly Rep 1992;41(5):69–72 [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention Cigarette smoking among Chinese, Vietnamese, and Hispanics—California, 1989–1991. MMWR Morb Mortal Wkly Rep 1992;41(20):362–367 [PubMed] [Google Scholar]
- 22.Jenkins CNH, McPhee SJ, Le A, Pham GQ, Ha N-T, Stewart S. The effectiveness of a media-led intervention to reduce smoking among Vietnamese-American men. Am J Public Health 1997;87(6):1031–1034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jenkins CNH, McPhee SJ, Bird JA, et al. Effects of a media-led education campaign on breast and cervical cancer screening among Vietnamese-American women. Prev Med 1999;28(4):395–406 [DOI] [PubMed] [Google Scholar]
- 24.Jenkins CNH, McPhee SJ, Wong C, Nguyen T, Euler GL. Hepatitis B immunization coverage among Vietnamese-American children 3 to 18 years old. Pediatrics 2000;106(6):e78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hiatt R, Pasick RJ, Perez-Stable EJ, et al. Pathways to early cancer detection in the multiethnic population of the San Francisco Bay Area. Health Educ Q 1996;23(suppl):S10–S27 [Google Scholar]
- 26.Walsh JME, McPhee S. A systems model of clinical preventive care: an analysis of factors influencing patient and physician. Health Educ Q 1992;19(2):157–175 [DOI] [PubMed] [Google Scholar]
- 27.McPhee SJ, Bird JA, Ha N-T, Jenkins CNH, Fordham D, Le B. Pathways to early cancer detection for Vietnamese women: Suc Khoe La Vang! (Health Is Gold!). Health Educ Q 1996;23(suppl):S60–S75 [Google Scholar]
- 28.Bird JA, McPhee SJ, Ha N-T, Le B, Davis T, Jenkins CN. Opening pathways to cancer screening for Vietnamese-American women: lay health workers hold a key. Prev Med 1998;27(6):821–829 [DOI] [PubMed] [Google Scholar]
- 29.Nguyen BH, Vo PH, Doan HT, McPhee SJ. Using focus groups to develop colorectal cancer screening intervention among Vietnamese Americans. J Cancer Educ 2006;21(2):80–83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nguyen BH, Pham JT, Chew RA, McPhee SJ, Stewart SL, Doan HT. Effectiveness of continuing medical education in increasing colorectal cancer screening knowledge among Vietnamese American physicians. J Health Care Poor Underserved 2010;21(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nguyen TT, McPhee SJ, Nguyen T, Lam T, Mock J. Predictors of cervical Pap smear screening recognition, intention, and receipt among Vietnamese American women. Am J Prev Med 2002;23(3):207–214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nguyen T, Vo PH, McPhee SJ, Jenkins CN. Promoting early detection of breast cancer among Vietnamese American women: results of a controlled trial. Cancer 2001;91(suppl 1):267–273 [DOI] [PubMed] [Google Scholar]
- 33.Mock J, McPhee SJ, Nguyen T, et al. Effective lay health worker outreach and media-based education for promoting cervical cancer among Vietnamese American women. Am J Public Health 2007;97(9):1693–1700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McPhee SJ. Promoting breast and cervical cancer screening among Vietnamese American women: two interventions. Asian Am Pac Isl J Health 1998;6(2):344–350 [PubMed] [Google Scholar]
- 35.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol 1986;51(6):1173–1182 [DOI] [PubMed] [Google Scholar]
- 36.Agresti A. Categorical Data Analysis New York, NY: John Wiley & Sons; 1990 [Google Scholar]