Abstract
Objectives. We examined whether cocaine-dependent homeless persons had stable housing and were employed 6, 12, and 18 months after they entered a randomized controlled trial comparing 2 treatments.
Methods. One group (n = 103) received abstinence-contingent housing, vocational training, and work; another group (n = 103) received the same intervention plus cognitive behavioral day treatment. We examined baseline and early treatment variables for association with long-term housing and employment.
Results. Although the enhanced-treatment group achieved better abstinence rates, the groups did not differ in long-term housing and employment stability. However, consecutive weeks of abstinence during treatment (and to a lesser extent, older age and male gender) predicted long-term housing and employment stability after adjustment for baseline differences in employment, housing, and treatment.
Conclusions. Our data showed a relationship of abstinence with housing stability. Contrasting these results with the increasingly popular Housing First interventions reveals important gaps in our knowledge to be addressed in future research.
Homelessness remains a major problem despite considerable public awareness and publicly funded interventions.1–3 Prevalence of US homelessness per day in 2007 was estimated to be 671 788.4 Although the estimated prevalence of alcohol and substance use disorders among homeless persons varies depending on where and how data are collected, national cross-sectional surveys suggest that 38% have past-year alcohol problems and 46% have past-year drug problems, and both co-occur with mental illness.5 The health, mortality, and criminal justice implications of homelessness have been well-studied and reflect increased societal costs when homelessness and its correlates are poorly addressed.6–8
We developed and evaluated an effective intervention for homeless cocaine-dependent persons in several randomized controlled trials conducted in Birmingham, Alabama.9–11 The most recent trial, Homeless 4,12 treated 2 groups with abstinence-contingent housing and work therapy (for 6 months), which had been found in earlier trials to be more effective than either not providing housing or providing housing without an abstinence contingency. One Homeless 4 group (treatment) received 6 months of abstinence-contingent housing and work training alone; the other group (enhanced treatment) received the same contingency management plus daily cognitive behavioral day treatment.
We used rigorous methods to diagnose mental illness and measure abstinence (defined as zero use of alcohol and common illicit drugs), housing, and employment stability throughout treatment and in follow-ups at 6, 12, and 18 months. We examined whether superior long-term housing and employment stability were related to the superiority in long-term abstinence achieved by the enhanced-treatment group. We addressed 3 research questions: (1) What is the effect of treatment group on housing and employment stability over time? (2) Does sustained abstinence achieved during treatment and aftercare contribute to long-term housing and employment stability? (3) What other factors predict housing and employment outcomes?
Investigating housing and employment outcomes in this context is relevant to the literature on Housing First,13 which places no preconditions on the receipt of housing, and more traditional treatment-oriented, linear approaches to housing, which connect it to treatment. Many communities rely on addiction treatment as a point of entry to treatment for a major subset of the homeless population, it is therefore important to determine whether long-term housing and employment are achieved by persons who pursue effective addiction treatments.
METHODS
Applicants for Homeless 4 were recruited from Birmingham Health Care, the largest agency serving homeless persons in Alabama, between November 2001 and June 2004. Of 339 persons screened, 206 met study criteria, which comprised McKinney Act criteria for homelessness14: a diagnosis of cocaine dependence by the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition,15 measured by reported cocaine use within the past 2 weeks; psychological distress, indicated by a score of at least 70 (2 standard deviations above the mean) on 1 or more Brief Symptom Inventory subscales16,17; willingness to participate; and no plans to move from Birmingham for 18 months.
Exclusion criteria were cognitive impairment that compromised informed consent and conditions that required immediate inpatient treatment. Treatment groups were randomly assigned, with 103 participants in each. Participant demographic and treatment data are reported in Table 1. Our research methods are described in more detail elsewhere.12
TABLE 1.
Participant Baseline Demographic and Treatment Characteristics: Homeless 4 Trial, Birmingham, AL, 2001–2005
| Treatment Group | Enhanced-Treatment Group | P | |
| Gender, no. (%) | |||
| Men | 77 (74.8) | 72 (69.9) | .53 |
| Women | 26 (25.2) | 31 (30.1) | |
| Age, y, mean (SD) | 39.5 (7.2) | 40.6 (7.2) | .29 |
| Race | |||
| African American | 96 (93.2) | 99 (96.1) | .54 |
| White | 7 (6.8) | 4 (3.9) | |
| Drug abused, y, mean (SD) | |||
| Alcohol | 17.7 (10.4) | 18.5 (10.2) | .59 |
| Cannabis | 11.0 (9.4) | 10.2 (9.7) | .59 |
| Cocaine | 12.4 (7.0) | 11.4 (6.0) | .29 |
| Education, y, mean (SD) | 11.7 (1.7) | 12.2 (1.5) | .04 |
| Disabled, no. (%) | 13 (12.9) | 3 (2.9) | .01 |
| Homelessness, mo, mean (SD) | 30.9 (43.7) | 27.7 (46.8) | .61 |
| Previous period of homelessness, mo, no. (%) | .02 | ||
| 0–6 | 36 (36.7) | 50 (50) | |
| 7–12 | 8 (8.2) | 13 (13) | |
| > 12 | 54 (55.1) | 37 (37) | |
| Missing information, no. | 5 | 3 | |
| Consecutive weeks abstinent, mean (SD) | 14.1 (12.6) | 19.2 (16.0) | .048 |
| Cumulative treatment days, mean (SD) | 18.1 (8.5) | 19.6 (9.4) | .051 |
| Work therapy hours, mean (SD) | 115 (68) | 127 (73) | .15 |
| Fraction of time in program-provided housing, mean (SD) | 0.597 (0.47) | 0.636 (0.47) | .2 |
Note. The sample size for each group was n = 103.
Assessment
Substance use was assessed by testing urine specimens collected under observation. At baseline and follow-ups, urine was tested for cocaine, marijuana, alcohol, benzodiazepines, opiates, and amphetamine. During phase 1 of treatment (weeks 1–8) and aftercare (weeks 9–24), urine was tested for cocaine, marijuana, and alcohol on Monday, Wednesday, and Friday. In weeks 25 to 52, urine was tested randomly once a week, and participants were paid $10 per specimen. In weeks 53 to 78, urine was tested randomly once every 2 months and participants were paid $50 per specimen.
At baseline and follow-ups, interviewers who did not know participants' treatment assignment used the Retrospective Housing, Employment and Substance Abuse Treatment Overview to determine housing and employment outcomes.18 This instrument applies a timeline follow-back procedure to identify salient dates of remembered housing and employment episodes and then fills in gaps to render a complete record of housing and employment episodes across a maximum of 6 months.19 We measured exposure to each treatment modality, including work training, with a daily activities log in which staff recorded hours spent in each scheduled activity.
Design
The Homeless 4 study was a 2-group, randomized controlled trial, comparing treatment (abstinence-contingent housing, vocational training, and work therapy) with enhanced treatment, which included the same interventions plus extensive cognitive behavioral day treatment that used many procedures of the community reinforcement approach of Higgins et al.20–22 Participants received an hourly wage for their time in training and work assignments.
The abstinence contingency included consequences for both the housing and employment–training interventions. Participants who provided a drug- or alcohol-positive urine specimen, failed to provide a specimen, or did not comply with work guidelines, were, within 6 hours of the test or occurrence, transported to a shelter or other housing; the work or training stipend rate was reset to $1.25 per hour, with subsequent opportunity to increase by $1.00 per hour for each day they met the abstinence contingency and work compliance guidelines up to a maximum of $5.25 per hour. Return to provided housing was contingent on 3 consecutive negative urine tests.
Outcomes
To facilitate analyses, housing and employment at each assessment point (baseline and months 6, 12, and 18) were measured as days housed and days employed in the past 60 days. Evaluation of the distributions of these measures indicated that the vast majority of participants (between 80% and 90%) had either 0 or 60 days housed or employed. Consequently, these interval measures were converted to binary outcomes of housed and employed (considered positive if a participant had ≥ 40 days housed or employed in the past 60, and not housed or not employed otherwise). For participants with missing data at any time point, these binary measures were coded as not housed and not employed.
The largest number of consecutive weeks abstinent over the first 52 weeks of study participation provided a measure of each person's sustained abstinence. Missing drug tests were coded as unexcused and assumed positive for drugs, excused (for example, when patients were hospitalized or attended a family funeral out of town), or administratively missing. Administratively missing was coded when tests were scheduled but not conducted because of computer or scheduling problems or when tests were scheduled for clinic holidays. Both excused and administratively missing specimens were assumed to be randomly missing and were not counted as disruptive to a series of consecutive drug-free specimens.
Statistical Analyses
We used intention-to-treat analyses for all outcomes. Primary analyses focused on effects of treatment group on long-term housing and employment and effects of sustained abstinence on housing and employment at 12 and 18 months. Additional analyses examined other factors predictive of long-term housing and employment.
We assessed the effect of treatment group on housing and employment outcomes through contingency tables with χ2 statistics to detect the relationship between treatment group and the binary housing and employment measure (where the outcome of ≥ 40 days housed or employed at the assessment point was considered a positive outcome) at each time point. We used a generalized estimating equation extension of generalized linear models on these binary measures of housing and employment during each phase to assess differences between treatment groups on housing and employment as a function of treatment group, study phase, and their interaction. We used models to generate unadjusted estimates of the temporal effects of treatment and to assess the effects after adjustment for baseline housing and employment status in the respective models.
We evaluated the effect of sustained abstinence on housing and employment at 12 and 18 months through both descriptive and model-based approaches. For the unadjusted descriptive analyses, we converted the continuous measure of consecutive weeks abstinent during the first year of treatment into an ordinal measure with 4 levels (0–4, 5–16, 17–28, and > 28 consecutive weeks abstinent) after examining the distribution. We used contingency tables with associated Mantel–Haenszel χ2 tests and graphical summaries to examine the relationship between abstinence and the probability of being housed or employed at 12 and 18 months.
We also used logistic regression analyses to assess the effect of sustained abstinence on housing and employment. These regression models included a term for treatment group to evaluate whether sustained abstinence was an important independent predictor of better housing and employment outcomes or simply a marker of those outcomes and potentially a mediator of treatment.
We used logistic regression models to identify other factors that might predict housing and employment and to examine whether the effect of early sustained abstinence and treatment group assignment on housing and employment was confounded by several other factors. These comprised baseline homelessness (days homeless over the past 60 days), baseline employment (days employed over the past 60 days), age, gender, education, previous years of cocaine use at baseline, dose of treatment during the first 8 weeks of treatment, and exposure to program housing and employment training during the 6 months of treatment. For analyses of employment, participants who were defined as disabled or retired at baseline (16 total participants) were excluded.
To address the possibility that the effect of consecutive weeks abstinent on long-term housing and employment was mediated by the exposure to housing and employment during treatment that was contingent on maintaining abstinence, we controlled for those factors in a series of logistic regression models. For housing, we used models that included 2 alternative housing variables that reflected abstinence-contingent housing: (1) total fraction of days during the 60 days prior to the 2- and 6-month assessments that were spent in either stable housing or program-provided housing and (2) total fraction of days spent in program-provided housing. For employment, we used models that included total hours of work therapy, access to which was contingent on abstinence.
RESULTS
Table 1 shows demographic variables, which were comparable between treatment groups, except that the enhanced-treatment group had 0.5 years more of education, and the treatment group had more individuals who were disabled or retired (treatment group, 12.9%; enhanced-treatment group, 2.9%; P = .02) and more chronically homeless participants (homeless for more than 1 year prior to entry into the program). In subsequent analyses, factors that differed across treatment groups were examined as potential confounders of the effect of treatment and the effect of sustained abstinence on housing and employment.
Housing and Employment Outcomes
Participants living in program-provided housing were not categorized as housed. The percentage of participants who were housed for more than 40 of the past 60 days in the treatment and enhanced-treatment groups, respectively, were at baseline, 9.9 versus 8.7; at 6 months, 8.9 versus 10.7; at 12 months, 36.6 versus 44.7; and at 18 months, 35.6 versus 44.7. These between-treatment group differences were not statistically significant (P > .19).
The percentage of participants who were employed for more than 40 of the past 60 days in the treatment and enhanced-treatment groups, respectively, were at baseline, 8.0 versus 6.0; at 6 months, 22.7 versus 22.0; at 12 months, 26.1 versus 39.0; and at 18 months, 21.6 versus 28.0. The between-group differences at 12 and 18 months were not statistically significant (P > .06 at all time points).
The generalized estimating equation model analyses of housing and employment as a function of treatment group, study phase, and their interaction showed that the probability of being stably employed improved in both groups between baseline and 6 months (P < .001) and 12 and 18 months (P < .001), and the probability of being housed also improved in both groups between baseline and 12 and 18 months (P < .001). The model provided no evidence of differences after baseline between treatment groups for either housing (P = .61) or employment (P = .36).
We constructed additional models to evaluate whether the absence of a treatment group effect or temporal effects might be confounded by baseline differences in previous homelessness, employment, or education or by temporal differences in local unemployment levels. The results were consistent with the primary models (data not shown). Thus, the answer to our first empirical question was that treatment group did not have a significant effect on long-term housing and employment.
Relationship of Sustained Abstinence to Housing and Employment
Complete abstinence results are reported in Milby et al.12 Analysis of variance procedures compared treatment groups for the most consecutive weeks of abstinence. During 6 months of treatment and aftercare through 12 months, the enhanced-treatment group achieved significantly more consecutive weeks of abstinence than did the treatment group (Table 1).
A second critical question was whether sustained abstinence affects long-term housing and employment. Because these treatment regimens affected sustained abstinence, analyses also examined relationships among treatment group, sustained abstinence, and long-term housing and employment.
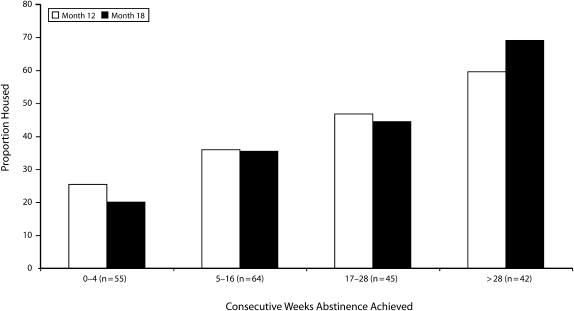
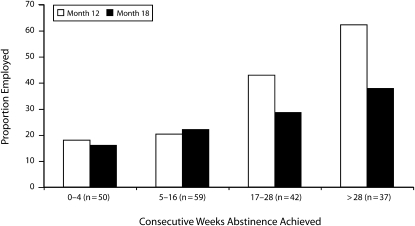
Figures 1 and 2 show the strong monotonic relationships between sustained abstinence over the first 52 weeks and housing at 12 months (Mantel–Haenszel χ21 = 12.7; P < .001) and 18 months (Mantel–Haenszel χ21 = 23.7; P < .001) and between sustained abstinence and employment at 12 months (Mantel–Haenszel χ21 = 21.0; P < .001) and 18 months (Mantel–Haenszel χ21 = 24.3; P < .001). These unadjusted results, with missing housing and employment data classified as not housed and not employed, did not change substantively in stratified analyses with control for treatment group or after excluding missing housing and employment records, assuming those missing data to be missing at random (data not shown). Results from these contingency table analyses were consistent with those from our logistic regression models.
FIGURE 1.
Proportion of participants housed by weeks of sustained abstinence at 12- and 18-month follow-up after treatment: Homeless 4 Trial, Birmingham, AL, 2001–2005.
FIGURE 2.
Proportion of participants employed by weeks of sustained abstinence at 12- and 18-month follow-up after treatment: Homeless 4 Trial, Birmingham, AL, 2001–2005.
The unadjusted results from the Mantel–Haenszel tests of the data in Figures 1 and 2 were consistent with both unadjusted and adjusted results from logistic regression models with the continuous measure of consecutive weeks abstinent as a predictor. For the outcome of stable housing, the logistic regression model showed a strong relationship at month 12 (odds ratio [OR] = 1.04 per additional week abstinent; 95% confidence interval [CI] = 1.019, 1.0610; P < .001). The OR associated with each additional 8 weeks of consecutive abstinence was 1.37 (95% CI = 1.16, 1.61). Analogously, at month 18, consecutive weeks abstinent predicted stable housing (OR = 1.058 per additional week abstinent; 95% CI = 1.035, 1.082; P < .001). For each additional 8 consecutive weeks of abstinence, the OR was 1.57 (95% CI = 1.32, 1.87). For employment, the model similarly showed a strong relationship at month 12 (OR = 1.059 per additional week abstinent; 95% CI = 1.035, 1.084; P < .001); for each additional 8 consecutive weeks of abstinence, the OR was 1.58 (95% CI = 1.32, 1.90). At month 18, the OR was 1.029 per additional week abstinent (95% CI = 1.007, 1.052; (P = .01); for each additional 8 consecutive weeks of abstinence, the OR was 1.26 (95% CI = 1.06, 1.50).
Predictors of Stable Housing and Employment
We included treatment group in a series of stepwise logistic models (as a design aspect of the study) and found that it was not a significant predictor of either stable housing or employment. However, consecutive weeks of abstinence remained a significant housing predictor at 12 months (OR = 1.36 for 8-week difference; 95% CI = 1.15, 1.60; P < .001). At 18 months, greater age predicted stable housing (OR = 1.83 for 10-year difference; 95% CI = 1.08, 2.64; P = .016) and consecutive weeks of abstinence (OR = 1.49 for 8-week difference; 95% CI = 1.25, 1.79; P < .001).
For 12- and 18-month employment, male gender and consecutive weeks of abstinence (8-week increments) were significant predictors (at 12 months, for male gender, OR = 2.66; 95% CI = 1.17, 6.06; P = .02; for abstinence, OR = 1.60; 95% CI = 1.32, 1.96; P < .001; at 18 months, for male gender, OR = 2.78; 95% CI = 1.22, 6.33; P = .015; for abstinence, OR = 1.63; 95% CI = 1.34, 1.99; P < .001).
Controls for Treatment Housing and Employment
Control for program-provided housing during treatment had minimal effect on the association of consecutive weeks of abstinence with long-term housing. Abstinence continued to be a strong predictor in models that controlled for these factors. Consecutive weeks of abstinence (in 8-week increments) was strongly related to long-term housing at 12 months (OR = 1.32; 95% CI = 1.08, 1.59; P < .001) and 18 months (OR = 1.58; 95% CI = 1.25, 1.91; P < .001) after control for exposure to program-provided housing. We had comparable results when we controlled for the combination of stable and program-provided housing (data not shown).
The employment analyses suggested that the effects of abstinence were mediated to some degree through the abstinence-contingent work therapy at 18 months but not at 12 months. At 12 months, consecutive weeks of abstinence (in 8-week increments) was still strongly related to employment after control for hours of work therapy (OR = 1.55; 95% CI = 1.18, 2.01; P < .001), but a similar result was not seen at 18 months (OR = 1.17; 95% CI = 0.89, 1.52; P = .25).
DISCUSSION
Although the enhanced-treatment group achieved superior sustained abstinence at 12 and 18 months, we found no treatment group differences in housing and employment stability at these follow-up points. Nevertheless, analyses revealed a strong positive relation between consecutive weeks of abstinence and 12- and 18-month housing and 12-month employment, even when treatment exposure to housing and employment were controlled. Taken together, these results inform understanding of the relationships between an effective treatment of serious substance use disorder, abstinence, housing, and employment stability for substance-dependent homeless persons. In previous randomized trials of our effective enhanced-treatment intervention, homeless substance abusers with serious mental illness had improved abstinence, fewer symptoms of mental illness, fewer diagnoses, and less functional impairment.23–25
If abstinence-contingent housing and work training are the most important aspects of this treatment approach, as recent analyses suggest,26 it may be difficult to detect any additional marginal effect of behavioral day treatment on housing and employment. The earlier study of this controlled trial, which focused on abstinence outcomes, found greater abstinence only at 12 and 18 months and not during or immediately after treatment.12 Although the treatment groups differed in mean consecutive weeks of abstinence, the distributions of abstinent weeks overlapped substantially. Within each treatment group, individuals who established early and lengthy stretches of abstinence were most likely to be stably housed and employed at 12 and 18 months.
Among the limitations of this and earlier studies was that local availability and conditions for subsidized housing entry varied over time. Because the study was powered to detect differences in abstinence between trial groups, it was underpowered to detect differences in housing and employment. We speculate that unstable local housing availability during the study may have affected measured housing outcomes. The agency controlling the federally subsidized Shelter Plus Care housing imposed an abstinence requirement of 4 consecutive months after completing treatment. Any participant on its waiting list who tested positive for drugs was placed at the end of the list. Our intensive protocol for drug use measurement showed that few met the criterion set by Shelter Plus Care authorities. Thus, inability to meet publicly subsidized program criteria may have masked any relative abstinence advantage of enhanced-treatment participants.
Our housing outcomes were consistent with those of Orwin et al.27 In a large sample of homeless persons in Chicago who received substance abuse treatment, they found a 43% reduction in homelessness at their 3-year follow-up. One of 2 predictors of continued homelessness was continued cocaine use. Participants in our study were dependent on crack cocaine, and consecutive weeks of abstinence incrementally increased their odds for being stably housed at 12 and 18 months.
Our current and previous research,10,11 along with the study by Orwin et al.,27 represents a contrast to a newer housing approach, Housing First.13, 28–30 Housing First offers permanent housing without treatment-related preconditions, other than provision of payment and agreement for a case manager to visit. In a randomized controlled trial that compared Housing First to a more traditional treatment-oriented approach (Continuum of Care) in New York,13 the Continuum of Care group received housing on the basis of treatment participation. The Housing First trial group achieved better long-term housing stability, even though abstinence outcomes were not different from those of the Continuum of Care group, implying that abstinence may not be relevant to long-term housing success.
By contrast, our data showed that abstinence was strongly related to subsequent housing stability. However, the studies are not perfectly comparable. Persons with psychoses were not included in our trial but were participants in the Housing First trial. Moreover, we do not know whether persons with severe cocaine dependence were recruited in the Housing First trial. Finally, our study intervention involved time-limited housing interventions, not permanent housing.
Serious gaps in the homeless research literature leave us with important unanswered policy questions. Should communities invest in evidence-based addiction treatment and reduce barriers to housing entry after such treatment? Our research suggests the effectiveness of such approaches for those with drug dependence and nonpsychotic mental disorders. Should communities consider Housing First for persons without severe cocaine or other drug dependence but with psychotic and other serious mental disorders? Housing First approaches may well be more effective for this group. More controlled studies comparing these alternatives are urgently needed.
Acknowledgments
This research was supported by the National Institute on Drug Abuse (grant 1RO1 DA11789).
Human Participant Protection
This study was approved by the University of Alabama at Birmingham's institutional review board.
References
- 1.Office of Community Planning and Development. The Annual Homeless Assessment Report to Congress Washington, DC: US Department of Housing and Urban Development; 2007 [Google Scholar]
- 2.Singer J. Taking it to the streets: homelessness, health, and health care in the United States. J Gen Intern Med 2003;18(11):964–965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tompsett CJ, Toro PA, Guzicki M, Schlienz N, Blume M, Lombardo S. Homelessness in the US and Germany: A cross-national analysis. J Community Appl Soc Psychol 2003;13(3):240–257 [Google Scholar]
- 4.Office of Community Planning and Development. The Third Annual Homeless Assessment Report to Congress Washington, DC: US Department of Housing and Urban Development; July2008 [Google Scholar]
- 5.Burt M, Aron L. America's Homeless II: populations and services. Presented at: Urban Institute; February 1, 2000; Washington, DC: Available at: http://www.urban.org/publications/90344.html. Accessed January 1, 2000 [prepresentation draft] [Google Scholar]
- 6.Culhane DP, Metraux S, Hadley T. Public service reductions associated with placement of homeless persons with severe mental illness in supportive housing. Hous Policy Debate 2002;13(1):107–162 [Google Scholar]
- 7.Kertesz SG, Larson MJ, Horton NJ, Winter M, Saitz R, Samet JH. Homeless chronicity and health-related quality of life trajectories among adults with addictions. Med Care 2005;43(6):574–585 [DOI] [PubMed] [Google Scholar]
- 8.Salit SA, Kuhn EM, Hartz AJ, Vu JM, Mosso AL. Hospitalization costs associated with homelessness in New York City. N Engl J Med 1998;338(24):1734–1740 [DOI] [PubMed] [Google Scholar]
- 9.Milby JB, Schumacher JE, Raczynski JM, et al. Sufficient conditions for effective treatment of substance abusing homeless persons. Drug Alcohol Depend 1996;43(1-2):39–47 [DOI] [PubMed] [Google Scholar]
- 10.Milby JB, Schumacher JE, McNamara C, et al. Initiating abstinence in cocaine abusing dually diagnosed homeless persons. Drug Alcohol Depend 2000;60(1):55–67 [DOI] [PubMed] [Google Scholar]
- 11.Milby JB, Schumacher JE, Wallace D, Freedman MJ, Vuchinich RE. To house or not to house: the effects of providing housing to homeless substance abusers in treatment. Am J Public Health 2005;95(7):1259–1265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Milby JB, Schumacher JE, Vuchinich RE, Freedman MJ, Kertesz S, Wallace D. Toward cost-effective initial care for substance-abusing homeless. J Subst Abuse Treat 2008;34(2):180–191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tsemberis S, Gulcur L, Nakae M. Housing First, consumer choice, and harm reduction for homeless individuals with a dual diagnosis. Am J Public Health 2004;94(4):651–656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stewart B. McKinney Homelessness Assistance Act (1987), Public Law 100-177. [Google Scholar]
- 15.Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition Washington, DC; American Psychiatric Association; 1994 [Google Scholar]
- 16.Derogatis LR. The SC-R-90 Manual I: Scoring, Administration and Procedures for the SCL-90 Baltimore, MD: Clinical Psychometric Research; 1977 [Google Scholar]
- 17.Derogatis LR, Cleary PA. Confirmation of the dimensional structure of the scl-90-R: a study in construct validation. J Clin Psychol 1977;33:981–989 [Google Scholar]
- 18.Barrow SM, Hellman F, Lovell AM, Plapinger JD, Robinson CR, Struening EI. Personal History Form. Community Support Systems Evaluation Program Epidemiology of Mental Disorders Research New York, NY: Research Department, New York State Psychiatric Institute; 1985 [Google Scholar]
- 19.Sobell MB, Maisto SA, Sobell LC, Cooper AM, Cooper TC, Sander B. Developing a prototype for evaluating alcohol treatment effectiveness. Sobell LC, Sobell MB, Ward E, Evaluating Alcohol and Drug Abuse Treatment Effectiveness: Recent Advances New York, NY: Pergamon Press; 1980:129–150 [Google Scholar]
- 20.Higgins ST, Delaney DD, Budney AJ, et al. A behavioral approach to achieving initial cocaine abstinence. Am J Psychiatry 1991;148(9):1218–1224 [DOI] [PubMed] [Google Scholar]
- 21.Higgins ST, Sigmon SC, Wong CJ, et al. Community reinforcement therapy for cocaine-dependent outpatients. Arch Gen Psychiatry 2003;60:1043–1052 [DOI] [PubMed] [Google Scholar]
- 22.Higgins ST, Wong CJ, Badger GJ, Ogden DE, Dantona RT. Contingent reinforcement increases cocaine abstinence during outpatient treatment and 1 year of follow-up. J Consult Clin Psychol 2000;68:64–72 [DOI] [PubMed] [Google Scholar]
- 23.McNamara C, Schumacher JE, Milby JB, Wallace D, Usdan S. Prevalence of nonpsychotic mental disorders does not affect treatment outcome in a homeless cocaine-dependent sample. Am J Drug Alcohol Abuse 2001;27(1):91–106 [DOI] [PubMed] [Google Scholar]
- 24.Schumacher JE, Milby JB, McNamara C, et al. Effectiveness of abstinent contingent drug addiction treatment measured by DSM-III-R Substance Use Disorder diagnoses: Homeless 2. Drug Alcohol Depend 2001;63(Suppl 1):S141 [Google Scholar]
- 25.Schumacher JE, Milby JB, Wallace D, et al. Diagnostic compared with abstinence outcomes of day treatment and contingency management among cocaine-dependent homeless persons. Exp Clin Psychopharmacol 2003;11(2):146–157 [DOI] [PubMed] [Google Scholar]
- 26.Schumacher JE, Milby JB, Wallace D, et al. Meta-analysis of day treatment and contingency-management dismantling research: Birmingham Homeless Cocaine Studies (1990–2006). J Consult Clin Psychol 2007;75(5):823–828 [DOI] [PubMed] [Google Scholar]
- 27.Orwin RG, Scott CK, Arieira C. Transitions through homelessness and factors that predict them: three-year treatment outcomes. J Subst Abuse Treat 2005;28(Suppl 1):S23–S39 [DOI] [PubMed] [Google Scholar]
- 28.Ending chronic homelessness [editorial]. New York Times March 13, 2002:A24 [Google Scholar]
- 29.Up and off the streets [editorial] New York Times June 9, 2003:A30 [Google Scholar]
- 30.Ekholm E. New campaign shows progress for homeless. New York Times June 7, 2006: A18 [Google Scholar]