Abstract
Objectives. We explored factors associated with perception of barriers to immunization among parents of Hmong origin in California, whose children experience persistent immunization inequities even with health insurance.
Methods. A partnership of academic researchers and members of the Hmong community conducted a community-based participatory research project. We collected data in naturalistic settings with a standardized instrument. We analyzed responses from 417 parents and caregivers and created a structural equation model to determine factors that contributed to perceived barriers.
Results. Of 3 potential contributing factors to perceived barriers—nativity, socioeconomic position, and use of traditional Hmong health care (i.e., consulting shamans and herbalists)—the latter 2 significantly predicted higher perceived barriers to immunization. Nativity, indicated by years in the United States, age of arrival in the United States, and English language fluency, did not predict perceived barriers.
Conclusions. Interventions aimed at reducing immunization inequities should consider distinct sociocultural factors that affect immunization rates among different refugee and immigrant groups.
Immunization is ranked the number 1 public health achievement in saving lives during the 20th century, as reported by the Centers for Disease Control and Prevention.1 However, despite recent success in reducing health inequities in immunization rates in young children,2 among some communities and ethnic groups, immunization rates remain below optimal levels.3,4
A core goal of Healthy People 2010 is eliminating disparities in immunization rates associated with race/ethnicity, income, geographic location, and other factors.5 Other Healthy People 2010 goals are to reduce health disparities in and deaths from cervical cancer and to decrease cases of chronic hepatitis B infection, which can lead to liver cancer.5 The incidence of both these cancers can be significantly lowered through immunization.6,7
Rates of liver and cervical cancer are 3 to 4 times as high among the Hmong in California as they are as among other Asians/Pacific Islanders in California.8 The Hmong are also much less likely than are other ethnic groups in California to have their cancers diagnosed at an early, treatable stage; prevention is key to reducing the cancer burden in this population.9 Up to 60% of liver cancer and 70% of cervical cancer can be prevented by adequate immunization,10 but the Hmong are the least likely among Asian/Pacific Islander groups to obtain these immunizations for their children.11 Our literature searches in MEDLINE and CINAHL revealed little research on specific barriers to immunization among the Hmong.
After the end of the Vietnam War in 1975, Hmong refugees from Laos were resettled in several nations, with the majority coming to the United States. By 2000, US residents of solely Hmong origin numbered 169 428, with the largest concentration (65 095 persons) in California.12 In 2004, California experienced another significant surge of Hmong refugees when the US government reclassified the Hmong held in the Wat Tham Krabok refugee camp in Thailand as refugees and permitted their entry to the United States.13 These 15 000 Hmong refugees present unique health needs arising from their long internment. Hmong refugees were reported to be underimmunized in the Wat Tham Krabok camp, and upon entrance to the United States they were provided with only the first dose of multiple-dose vaccinations.14 Adequate immunization coverage requires multiple doses given in specific sequences to be fully effective.15 Outreach and follow-up are needed—to protect individuals as well as the general public—for the Hmong community.
We used the social determinants of health framework to estimate the effects of sociocultural and economic factors on adequate immunization.16 Previous studies on barriers to immunization indicated that poverty, language usage, education, nativity, race/ethnicity, access to health care, and other factors may contribute to inadequate immunization.17–22 The linkages and relationships among these factors have not been fully explored.
To identify sociocultural factors that affect immunization rates among the Hmong, we used structural equation modeling, which allowed us to use manifest (or observed) variables to estimate the causal effects of latent (or unmeasured) variables. In structural equation modeling analysis, each latent variable represents a composite of manifest variables. Each model is tested to determine whether it is consistent with the empirical data.23,24 Structural equation modeling techniques permit a more parsimonious analysis and provide a framework for demonstrating relationships among theoretical constructs in addition to representing data.25 Structural equation modeling also considers differences among individual survey scores that may account for imperfect score validity and reliability.23 We hypothesized that nativity, type of health care provider, and socioeconomic position would predict perceptions of barriers to immunization.
METHODS
We conducted a community-based participatory research (CBPR) study.26 CBPR emphasizes working with rather than in communities and specifying social change as a desired outcome. CBPR is a socioecological approach to research with a concentration on the social, environmental, and behavioral determinants of health and how these factors influence health inequities.26 The CBPR partnership for our study included the principal investigator (D. L. B.) and members of the Hmong Women's Heritage Association, which serves the Hmong community in the Central Valley of California. The partners identified a critical need to understand the reasons for low immunization rates in the Hmong community and ultimately to create policy, advocacy, and service interventions to improve immunization rates.
Measurement
Our data collection instrument was the 23-item Search for Hardship and Obstacles to Shots (SHOTS) survey,27 which solicits responses on a Likert scale. Previous research found that parental perceptions of perceived barriers to immunization predicted immunization status.28 The SHOTS instrument was based on the Triandis adaption of the theory of reasoned action.29 This model is derived from health promotion theory but also considers the social determinants of health, such as the availability of health care and its influence on health choices.29,30
The SHOTS instrument has 3 subscales, each representing a type of perceived barrier: (1) access to immunization (e.g., “The clinic/facility wasn't open at the time I could go”), (2) concerns about vaccines (e.g., “I worry what is in the shots”), and (3) belief that immunization is not important (e.g., “I don't think kids shots are important”). A higher score registers greater perception of barriers to immunization. We used Jones et al.’s adaptation of the Brislin method for back-and-forth translation to translate the survey into Hmong.31 The translated instrument was reviewed by bilingual Hmong community members through cognitive interviewing to ensure content validity and then field tested.
Procedure
We recruited our cross-sectional convenience sample in 2008 through enrollment at natural settings in the Central Valley and San Joaquin Valley, with 95% of participants recruited during Hmong New Year events. These events attract a broad cross section of the Hmong community and are the largest and most heavily attended social events of the year.32 Additional participants were recruited during an event at a school with high Hmong student enrollment and at several sports events that were linked with the New Year celebrations.
Volunteers were eligible if they were of Hmong origin, were aged 18 years or older, had lived in the United States for at least 1 year, had at least 1 child in the home who was aged younger than 9 years, and reported being able to read and write in either Hmong or English. Our requirement that participants had lived in the United States for at least 1 year ensured that we did not have very recent refugees who might have received health services provided to refugees that were not generally available in the community. Participants with children aged younger than 9 years would have had more recent experiences with immunization and therefore better recall about them. We offered the questionnaires in both Hmong and English versions, and the majority of participants (64%) chose to complete the English version. Bilingual Hmong interpreters were available for participants who needed minimal assistance with completing the questionnaires. Participants received a $5 gratuity for their time.
We compared our sample with the data for the Hmong from the 2000 Census33 and found that it reflected the larger Hmong population well in median income (sample, $20 000–$30 000; census tract, $24 542), percentage who spoke English only (sample, 5.5; census tract, 4.6), and percentage with some high school education (sample, 47; census tract, 46).
We used G*Power3 software (available at: http://www.psycho.uni-duesseldorf.de/aap/projects/gpower) to determine that we required at least 220 participants to yield sufficient power for our statistical analyses (power = 0.9 level; large effect size = 0.5; α = 0.05).34 However, we collected as many surveys as possible within the constraints of the study's time line so that future social marketing regarding immunizations could draw on the most accurate information about the social demographics of Hmong in central California.
Data Analysis
We conducted a bivariate correlation to examine significant associations between sociodemographic variables and the total score from the SHOTS survey. Significant variables from the correlation were then included in a multiple regression analysis to predict the independent effects of the variables. The scores from each of the 3 subscales of the SHOTS survey served as the dependent variables in the multiple regression. The predictor variables included education, income, language used for reading or speaking, age of arrival in the United States, number of years living in the United States, and type of nonemergency health care. For participants who were born in the United States, we coded age of arrival as zero. We examined participants’ use of traditional Hmong health care practice to determine whether it had any significant effect on perceived barriers, because vaccines must be obtained through Western health care providers. We recoded type of health care services and predominant language used for reading or speaking as dummy variables.
We conducted data analyses with SPSS version 15.0.35 We set significance levels at .05 (2 tailed) and eliminated missing values with the listwise method. Tolerance and variance inflation factor values from the regression model met criteria for nonsignificant multicollinearity (minimum tolerance = 0.40; maximum tolerance = 0.99; variance inflation factor range = 1.01–2.52). The Durbin-Watson value was 1.31; therefore, the residuals in the model did not present heteroscedasticity.
Drawing on the social determinants of health framework and past research,17–21 we specified 2 latent factors for the structural equation modeling that were found to be associated with immunization status: nativity and socioeconomic position (SEP). The manifest variables of educational attainment and household income represented the latent factor of SEP. The manifest variables of language predominantly used for reading or speaking, number of years living in the United States, and age of arrival in the United States were entered in the model as the latent factor of nativity. A higher value for nativity indicated that participants were more native to the United States, regardless of birthplace. Because shamans and herbalists are an important source of health care for many Hmong,36 use of traditional Hmong health care practice was also entered as a predictor in the model. Traditional Hmong health care, defined as patronage of shamans and herbalists as health care providers, either alone or in combination with Western health care, was entered as a dichotomous variable, with 1 = use of traditional Hmong health care and 0 = no use of traditional Hmong health care.
To account for a possible variable that would explain the relationships of the predictors in the model, we allowed SEP, nativity, and traditional Hmong health care to correlate. For the latent variables nativity and SEP, the indicators for years of living in the United States and income served as reference variables, and their direct effects on the latent variables were specified at 1.00. We determined the degree of fit of the structural model to the data by a set of recommended goodness-of-fit indexes for structural equation modeling.24 We conducted the structural equation modeling analysis with LISREL version 8.80 structural equation modeling software and used a maximum likelihood estimation.37
RESULTS
We analyzed responses from 417 Hmong participants, most of whom were female (approximately 71%) and married (approximately 86%). Most participants (82%) were aged 40 years or younger (range = 18–59 years; mean = 32.7 years; interquartile range [IQR] = 12.0; 95% confidence interval [CI] = 31.8, 33.5). The vast majority of participants were born outside of the United States (approximately 58% in Laos and approximately 22% in Thailand; Table 1). When we included US-born participants in the calculation, the mean age of arrival in the United States was 14.5 years (IQR = 19; 95% CI = 13.4, 15.7); when we excluded persons born in this country, it was 18.1 years (IQR = 15; 95% CI = 17.0, 19.3). The average number of years lived in the United States was 18 (IQR = 18; 95% CI = 17.01, 18.9). Only 5% of participants reported not having any health insurance. The most common types of health insurance were Medicaid (52%) and private insurance (42%).
TABLE 1.
Sociodemographic Characteristics of Hmong Respondents (N = 417): California, 2008
| No. (%)a | |
| Women | 294 (70.5) |
| Men | 122 (29.3) |
| Age,b y | |
| 18–30 | 205 (49.3) |
| 31–40 | 136 (32.7) |
| 41–50 | 63 (15.1) |
| 51–59 | 12 (2.8) |
| Country of birth | |
| Laos | 240 (57.6) |
| Thailand | 92 (22.1) |
| United States | 80 (19.2) |
| Other | 4 (1.0) |
| Language used for reading or speaking | |
| Hmong only | 101 (24.2) |
| Mostly Hmong, some English | 149 (11.5) |
| Hmong and English equally | 135 (32.4) |
| Mostly English, some Hmong | 108 (25.9) |
| English only | 23 (5.5) |
| Marital status | |
| Married | 357 (85.6) |
| Separated, divorced, or widowed | 22 (5.3) |
| Single | 17 (4.1) |
| Living with partner | 16 (3.8) |
| Education | |
| No formal education | 72 (17.3) |
| Vocational or adult school | 60 (14.4) |
| ≤ Eighth grade | 28 (6.7) |
| Some high school | 34 (8.2) |
| High school graduate | 82 (19.7) |
| Some college | 76 (18.2) |
| ≥ College graduate | 50 (12.0) |
| Annual household income, $ | |
| 0–30 000 | 203 (49.8) |
| 30 001–60 000 | 155 (37.1) |
| > 60 000 | 50 (12.0) |
| Type of nonemergency health carec | |
| Western, private practice or HMO | 282 (67.6) |
| Western, community clinic | 55 (13.2) |
| Traditional only | 39 (9.4) |
| Western and traditional | 32 (7.7) |
| No health care provider | 5 (1.2) |
Note. HMO = health maintenance organizations.
Percentages do not equal 100 because of missing items.
Mean = 32.7; SD = 8.5.
Western indicates health care from conventional American providers; traditional indicates care from Hmong shamans and herbalists.
Bivariate and Multiple Regression Analyses
Mean score for the SHOTS complete scale was 24.97 (SD = 19.4; IQR = 30.0; 95% CI = 23.08, 26.87; range = 0.0–83.0). Our bivariate correlation found no significant association of age, gender, or country of birth with perceived barriers. We found significant negative correlations for education (r = −0.17; P = .001), income (r = −0.19; P < .001), years lived in the United States (r = −0.12; P = .015), and language (r = −0.28; P < .001). Age of arrival in the United States was positively correlated with perceived barriers (r = 0.14; P = .005).
The majority of respondents (approximately 68%) received nonemergency health care from providers in private practice and health maintenance organizations; we therefore chose this type of health care service as the reference group in the regression analysis. Factors that retained significant associations with perceived barriers to immunization in the multiple regression were income, language, any use of traditional Hmong health care, and no health care. The strongest associations, particularly for difficulties with access to immunization, were with speaking only or mostly Hmong and using traditional Hmong health care, either alone or in combination with Western health care providers (Table 2). Education, age of arrival, and use of community clinics were not significant predictors for any of the 3 subscales. We found a significant correlation with years lived in the United States only for the opinion that immunization was not important.
TABLE 2.
Multiple Regression Analysis of Sociodemographic Variables and Perceptions of Barriers to Immunization Among Hmong Respondents, by SHOTS Subscale: California, 2008
| Subscale 1—Accessa (n = 368) |
Subscale 2—Safetyb (n = 377) |
Subscale 3—Importancec (n = 378) |
|||||||
| b (SE) | B | P | b (SE) | B | P | b (SE) | B | P | |
| Income | −0.83 (0.28) | −0.15 | .003 | −0.29 (0.17) | −0.09 | .088 | −0.33 (0.13) | −0.13 | .015 |
| Education | −0.30 (0.22) | −0.07 | .184 | 0.02 (0.14) | 0.01 | .872 | −0.05 (0.11) | −0.03 | .650 |
| Age of arrival in United States, y | −0.03 (0.07) | −0.03 | .637 | 0.01 (0.04) | 0.02 | .778 | −0.04 (0.03) | −0.09 | .233 |
| Years lived in the United States | 0.02 (0.08) | 0.01 | .856 | 0.05 (0.05) | 0.07 | .334 | 0.08 (0.04) | 0.15 | .037 |
| Languaged | |||||||||
| Hmong or mostly Hmong | 7.40 (1.77) | 0.28 | .000 | 2.64 (1.11) | 0.17 | .018 | 1.86 (0.87) | 0.15 | .032 |
| Hmong and English equally | 5.50 (1.87) | 0.16 | .003 | 4.08 (1.15) | 0.20 | .000 | 3.28 (0.90) | 0.21 | .000 |
| Type of nonemergency health caree | |||||||||
| Western, community clinic | −2.27 (1.77) | −0.06 | .200 | −1.17 (1.06) | −0.06 | .272 | −1.40 (0.83) | −0.09 | .095 |
| Western and traditional | 7.14 (1.91) | 0.18 | .000 | 4.36 (1.19) | 0.18 | .000 | 3.02 (0.93) | 0.16 | .001 |
| Traditional only | 7.13 (1.86) | 0.18 | .000 | 3.57 (1.18) | 0.15 | .003 | 1.25 (0.90) | 0.07 | .167 |
| No health care provider | 12.87 (4.50) | 0.13 | .005 | 7.24 (3.13) | 0.11 | .021 | 1.71 (2.21) | 0.04 | .440 |
Note. SHOTS = Search for Hardship and Obstacles to Shots. Analysis was restricted to participants without missing values.
This subscale assessed barriers such as inconvenient clinic hours (R2 = 0.22; F10 367 = 10.15; P < .001).
This subscale assessed concerns about vaccine safety (R2 = 0.13; F10 376 = 5.51; P < .001).
This subscale assessed beliefs about the importance of immunization (R2 = 0.12; F10 377 = 4.90; P < .001).
Reference group for language was English and mostly English.
Western indicates health care from conventional American providers; traditional indicates care from Hmong shamans and herbalists. Reference group was Western health care providers in private practice and health maintenance organizations.
Structural Equation Modeling Analysis
Table 3 shows coefficients and t values from the structural equation modeling analysis. In our measurement model of the latent factors, all tested indicators showed significant associations. The goodness-of-fit indexes revealed a good fit of the model to the data (df = 16; χ2 = 43.55; P < .001; root mean square error for approximation = 0.071; comparative fit index = 0.977; Tucker–Lewis index = 0.948). We observed significant correlations in all 3 subscales (covariance range = 0.47–0.60; all, P < .001). Being native to the United States was positively correlated with SEP (r = 0.80; covariance = 0.30; P < .001); we found no correlation for SEP or nativity with use of traditional Hmong health care (r = 0.01 and 0.03, respectively).
TABLE 3.
Parameter Estimates for Correlations of Sociodemographic Variables With Survey Scores for Hmong Respondents in the Structural Equation Model: California, 2008
| b (SE) | B | t | |
| Subscale 1—accessa | |||
| Nativityb | 0.12 (0.25) | 0.10 | 0.49 |
| Socioeconomic position | −1.02 (0.47) | −0.49 | −2.16* |
| Traditional Hmong health care | 0.29 (0.05) | 0.29 | 5.31*** |
| Subscale 2—safetyc | |||
| Nativity | 0.12 (0.22) | 0.10 | 0.57 |
| Socioeconomic position | −0.62 (0.41) | −0.30 | −1.53 |
| Traditional Hmong health care | 0.26 (0.05) | 0.26 | 4.82*** |
| Subscale 3—importanced | |||
| Nativity | 0.47 (0.26) | 0.37 | 1.84 |
| Socioeconomic position | −0.97 (0.49) | −0.46 | −1.99* |
| Traditional Hmong health care | 0.21 (0.06) | 0.21 | 3.70*** |
| Nativity | |||
| Years lived in the United States | 1.00e | 0.79 | |
| Age of arrival in the United States, y | −1.05 (0.07) | −0.83 | −14.93*** |
| Languagef | 1.02 (0.07) | 0.80 | 14.55*** |
| Socioeconomic position | |||
| Income | 1.00e | 0.48 | |
| Education | 1.35 (0.20) | 0.65 | 6.61*** |
Note. Standardized estimates for measurement errors are proportions of unexplained variance. Analysis was restricted to participants without missing values (n = 340).
This subscale assessed barriers such as inconvenient clinic hours (R2 = 0.25).
Higher value on nativity means more native to the United States.
This subscale assessed concerns about vaccine safety (R2 = 0.12).
This subscale assessed beliefs about the importance of immunization (R2 = 0.13).
Factor loading fixed at 1.00 and not tested for statistical significance.
Higher value for language means more English is used for reading or speaking.
*P < .05; **P < .01; ***P < .001.
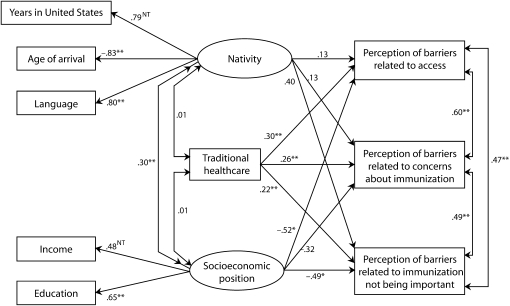
In our path analysis, in which nativity, SEP, and traditional Hmong health care predicted perception of barriers for each of the 3 subscales, correlations of nativity with perceived barriers did not reach statistical significance for any of the subscales, even though language was 1 of the indicators. The direct effect of SEP on perceived barriers was significant for 2 of the 3 subscales: access to immunization and belief that immunization was not important. The direct effect of traditional Hmong health care on perceived barriers was significant for all 3 subscales. Of the 3 predictors in the model, SEP had the strongest association: higher SEP significantly predicted lower perceived barriers to immunization (Figure 1).
FIGURE 1.
Structural equation model for barriers to immunization among parents of Hmong origin: California, 2008.
Note. NT = not tested (factor fixed at 1.00). The sample size was n = 340. Model fit: χ2 = 43.55; df = 16; root mean square error for approximation = 0.071; comparative fit index = 0.977; Tucker–Lewis index = 0.948. Values on 1-headed arrows are standardized coefficients. Values on 2-headed arrows are covariances.
*P < .05; **P < .01; ***P < .001.
DISCUSSION
To our knowledge, ours was the first study to explore barriers to immunization among Hmong living in the United States. We identified 3 main factors as potential contributors to perceived barriers to immunization: nativity, SEP, and use of traditional Hmong health care practices. Previous research found that patterns of vaccination varied among immigrant groups. One study found that children of foreign-born mothers who had resided in the United States for 5 years or less were less likely than were children whose mothers arrived earlier to have received all recommended vaccinations.17 However, a study in Germany found that less acculturation was positively associated with receiving vaccination but not with completion of the entire recommended schedule of vaccines.38 Vaccination status may also be influenced by attitudes toward vaccines prior to emigration.38
Our findings did not identify nativity in the United States as a significant predictor for perception of barriers to immunization. This implies that Hmong parents who are US born or have lived in this country longer may continue to face barriers similar to those of parents who are more recent immigrants. However, the strong correlation between nativity and SEP suggests that nativity may contribute indirectly to perception of barriers. Further, the different experiences of immigrant groups may give rise to different interactions with the health care system and to different perceptions about immunization and how to obtain it.
Participants who reported patronizing shamans or herbalists for health care were more likely to perceive barriers to immunization than were parents who sought health care solely from Western providers. A Hmong shaman we consulted for our study stated that shamans in general have no objection to immunization. “Shamans work on the spirit; we ask our clients to go to their doctor for preventions like shots” (T. S. Her, Hmong shaman, oral communication, March 2009).
In our discussions with Hmong community partners, we explored 2 possible explanations for the correlation we observed. First, it is possible that Hmong parents who seek services from shamans and herbalists have different perceptions about the efficacy and safety of interventions, such as immunization, in preventing disease. Qualitative research has demonstrated that Hmong in the United States blend and adapt traditional animism with Western medicine to interpret the role and possible failure of immunization in an outbreak.39 Hmong often use a multifaceted, hybrid pathway in seeking health care that incorporates Western medicine (for acute physical illness) and consultation with a shaman (for illnesses presumed to be spiritual or for which Western medicine has failed to provide an adequate cure or explanation).40,41 Despite shamans’ acceptance of immunization, Hmong parents who consult a shaman for health care may be blending ways of understanding health and may be distrustful of aspects of Western medicine, including immunizations.
Another explanation is that parents who seek services from shamans and herbalists may not seek (or may seek less often) routine medical care from Western health care providers. As a result, they may experience barriers arising from inconsistent health care or from the absence of a trusting relationship with a primary care provider. Studies have found that individuals who do not have regular care providers are more likely to be underimmunized or behind schedule in receiving immunization.42,43
Our Hmong respondents who patronized shamans and herbalists were a heterogeneous group. The use of shamans and herbalists was not associated with age, SEP, or nativity. Historically, the Hmong employed several types of traditional healers, and they continue to influence Hmong health practices.40 In Laos and later in the United States, Hmong customarily resorted to Western health care only as a last resort because shamans address balance within the body and soul, a traditional priority in this community.44,45 However, this trend may be changing: 42% of younger (aged 18–44 years) Hmong prefer to see a Western provider when a known illness is suspected.46 In addition, approximately 40% of Hmong have converted to a Western Christian religion and may consider use of a spiritual shaman a significant contradiction to their religious beliefs.47,48 Cultural attitudes, values, and behaviors influence when, where, why, and with whom a person of Hmong origin seeks health care services, including prevention services such as immunization.39,45,47
Our participants who had lower SEP were significantly more likely to perceive greater barriers to immunization, especially regarding access and perception of the importance of immunization. These results indicate that Hmong children, despite having health insurance, are at risk for underimmunization. Hmong Americans have the highest poverty and unemployment rates of all Asian/Pacific Islander groups in the United States.49 Health insurance alone is not sufficient to create access for marginalized groups that lack resources such as English language fluency and transportation.
Limitations
We conducted a structural equation modeling analysis of data from a Hmong population; replicating the model in other immigrant groups would help to establish its validity. Because we used a community-based survey, we may have missed barriers not captured in the instrument. We recruited a convenience sample of our target population at public events, where participants approached the data collection tables and no information could be collected on the characteristics of those who did not volunteer.
Our inclusion criteria required that parents have at least 1 young child in the home; our findings therefore may not apply to Hmong parents with adolescents. Because literacy in either Hmong or English was required to participate, the results may have underestimated perceived barriers to immunization in the overall Hmong community, particularly among people unable to read or write.
Conclusions
Our exploration of the reasons for Hmong children failing to receive adequate and timely immunization identified several sociocultural factors that directly or indirectly contribute to barriers to immunization. Interventions aimed at reducing immunization inequities need to consider the complex interplay of personal and environmental components that affect access to and utilization of health care, as well as the distinct worldviews and cultural beliefs among different immigrant and Asian/Pacific Islander groups. Further research is needed about the health-seeking behaviors of immigrants who have health insurance and about the most effective interventions to improve immunization rates.
The CBPR team, which includes Hmong shamans, plans to launch a social marketing campaign in the Hmong community and to advocate for adult educational programs, meaningful employment services, and culturally responsive health care systems. We also plan to advocate for disaggregation of Asian/Pacific Islander health data to allow for specific immunization rate tracking of subgroups such as the Hmong and inclusion of traditional healers as part of health care teams to enhance culturally responsive care.
Acknowledgments
We acknowledge with high regard and gratitude the support of Victoria Niederhauser, Janice Shoultz, the entire staff at Hmong Women's Heritage Association, and the research associates who assisted with this project. We also thank Kevin J. Grimm, Department of Psychology, University of California Davis, for his thoughtful review of the structural equation model.
Human Participant Protection
This study was approved by the institutional review board at University of Hawai‘i at Manoa.
References
- 1.Centers for Disease Control and Prevention Impact of vaccines universally recommended for children—United States, 1990–1998. MMWR Morb Mortal Wkly Rep 1999;48(12):238–243 [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention Eliminate disparities in adult and childhood immunization rates. Available at: http://www.cdc.gov/omhd/AMH/factsheets/immunization.htm. Updated June 5, 2007. Accessed August 22, 2007
- 3.Smith PJ, Stevenson J. Racial/ethnic disparities in vaccination coverage by 19 months of age. An evaluation of the impact of missing data result from record scattering. Stat Med 2008;27(20):4107–4118 [DOI] [PubMed] [Google Scholar]
- 4.Wooten KG, Luman ET, Barker LE. Socioeconomic factors and persistent racial disparities in childhood vaccination. Am J Health Behav 2007;31(4):434–445 [DOI] [PubMed] [Google Scholar]
- 5.Healthy People 2010. 2nd ed.Washington, DC: US Dept of Health and Human Services; 2000 [Google Scholar]
- 6.Bryan JT. Developing an HPV vaccine to prevent cervical cancer and genital warts. Vaccine 2007;25(16):3001–3006 [DOI] [PubMed] [Google Scholar]
- 7.Lavanchy D. Hepatitis B virus epidemiology, disease burden, treatment, and current and emerging prevention and control measures. J Viral Hepat 2004;11(2):97–107 [DOI] [PubMed] [Google Scholar]
- 8.Yang RC, Mills PK, Riordan DG. Cervical cancer among Hmong women in California, 1988 to 2000. Am J Prev Med 2004;27(2):132–138 [DOI] [PubMed] [Google Scholar]
- 9.Yang RC, Mills PK, Dodge JL. Cancer screening, reproductive history, socioeconomic status, and anticipated cancer-related behavior among Hmong adults. Asian Pac J Cancer Prev 2006;7(1):79–85 [PubMed] [Google Scholar]
- 10.Smith RA, Cokkinides V, Eyre HJ. American Cancer Society guidelines for the early detection of cancer, 2006. CA Cancer J Clin 2006;56(1):11–25 [DOI] [PubMed] [Google Scholar]
- 11.Butler LM, Mills PK, Yang RC, Chen MS. Hepatitis B knowledge and vaccination levels in California Hmong youth: implications for liver cancer prevention strategies. Asian Pac J Cancer Prev 2005;6(3):401–403 [PubMed] [Google Scholar]
- 12.American Fact Finder US Census 2000 Bureau. Available at: http://factfinder.census.gov/home/saff/main.html?_lang=en. Accessed June 20, 2009
- 13.Asian and Pacific Islander American Health Forum Health brief: Hmong in America. Revised August 2006. Available at: http://www.A&PIAhf.org/policy/index.htm. Accessed March 22, 2008
- 14.Asian and Pacific Islander American Health Forum California Hmong refugee resettlement: an informational hearing, California Commission on Asian and Pacific Islander American Affairs, November 16, 2004. Available at: http://www.A&PIAhf.org/policy/healthaccess/20041116testimony_hmong_resettlement.html. Accessed December 15, 2008
- 15.Omer SB, Salmon DA, Orenstein WA, deHart MP, Halsey N. Vaccine refusal, mandatory immunization, and the risks of vaccine-preventable diseases. N Engl J Med 2009;360(19):1981–1988 [DOI] [PubMed] [Google Scholar]
- 16.Baker EA, Metzler MM, Galea S. Addressing the social determinants of health inequities: learning from doing. Am J Public Health 2005;95(4):553–555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Buelow VH, Van Hook J. Timely immunization series completion among children of immigrants. J Immigr Minor Health 2008;10(1):37–44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Luman ET, Barker LE, Shaw KM, et al. Timeliness of childhood vaccination in the United States: days undervaccinated and number of vaccines delayed. JAMA 2005;293(10):1204–1211 [DOI] [PubMed] [Google Scholar]
- 19.Niederhauser VP, Stark M. Narrowing the gap in childhood immunization disparities. Pediatr Nurs 2005;31(5):380–386 [PubMed] [Google Scholar]
- 20.Stephan CL. Immunization registries: use of race and ethnicity, and socioeconomic status indicators to identify immunization disparities. AMIA Annu Symp Proc 2007(Oct 11):1124. [PubMed] [Google Scholar]
- 21.Klevens RM, Luman ET. US children living in and near poverty: risk of vaccine-preventable disease. Am J Prev Med 2001;20(suppl 4):41–46 [DOI] [PubMed] [Google Scholar]
- 22.Molinari NA, Koasa M, Messonnier ML, et al. Out-of-pocket costs of childhood immunizations: a comparison by type of insurance plan. Pediatrics 2007;120(5):e1148–e1156 [DOI] [PubMed] [Google Scholar]
- 23.Cohen J, Cohen P, West LS, et al. Applied Multiple Regression/Correlation Analysis for the Behavioral Sciences 3rd ed.Mahwah, NJ: Lawrence Erlbaum Associates; 2003 [Google Scholar]
- 24.Kline RB. Principles and Practice of Structural Equation Modeling 2nd ed.New York, NY: Guilford Press; 2005 [Google Scholar]
- 25.McArdle JJ. Current directions in structural factor analysis. Curr Dir Psychol Sci 1996;5(1):11–18 [Google Scholar]
- 26.Minkler M, Wallerstein N, Community-Based Participatory Research for Health: From Process to Outcomes 2nd ed San Francisco, CA: Jossey-Bass; 2008 [Google Scholar]
- 27.Niederhauser V. SHOTS survey Web site. 2009. Available at: http://www.shotsurvey.org. Accessed February 19, 2010
- 28.Prislin R, Dyer JA, Blakely CH, Johnson CD. Immunization status and sociodemographic characteristics: the mediating role of beliefs, attitudes, and perceived control. Am J Public Health 1998;88(12):1821–1826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Triandis HC. Cross-cultural psychology. Asian J Soc Psychol 1999;2(1):127–143 [Google Scholar]
- 30.Mejia GC, Kaufman JS, Corbie-Smith G, Rozier RG, Caplan DJ, Suchindran CM. A conceptual framework for Hispanic oral health care. J Public Health Dent 2008;68(1):1–6 [DOI] [PubMed] [Google Scholar]
- 31.Jones PS, Lee JW, Phillips LR, Zhang XE, Jaceldo KB. An adaptation of Brislin's translation model for cross-cultural research. Nurs Res 2001;50(5):300–304 [DOI] [PubMed] [Google Scholar]
- 32.Yang K. An assessment of Hmong American New Year and its implication for Hmong-American culture. Hmong Stud J 2008;8:1–32 Available at: http://www.hmongcc.org/HSJ8.html. Accessed October 1, 2008 [Google Scholar]
- 33.US Census Bureau American Fact Finder [fact sheet for a race, ethnic or ancestry group: Hmong]. Available at: http://factfinder.census.gov. Accessed September 20, 2006
- 34.Faul F, Erdfelder E, Lang AG, Buchner A. *Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 2007;39(2):175–191 [DOI] [PubMed] [Google Scholar]
- 35.SPSS [computer program]. Version 15.0. Chicago, IL: SPSS Inc; 2007 [Google Scholar]
- 36.Culhane-Pera K, Thao V. Hmong health beliefs and practices concerning children with high fevers. : Culhane-Pera KA, Vawter DE, Xiong P, Babbitt B, Solberg MM, Healing by the Heart: Clinical and Ethical Case Stories of Hmong Families and Western Providers Nashville, TN: Vanderbilt University Press; 2003:117–128 [Google Scholar]
- 37.Jöreskog KG, Sörbom D. LISREL 8.80 Student Edition [computer program]. Lincolnwood, IL: Scientific Software International; 2006 [Google Scholar]
- 38.Mikolajczyk RT, Akmatov MK, Stich H, et al. Association between acculturation and childhood vaccination coverage in migrant populations: a population based study from a rural region in Bavaria, Germany. Int J Public Health 2008;53(4):180–187 [DOI] [PubMed] [Google Scholar]
- 39.Henry RR. Measles, Hmong, and metaphor: culture change and illness management under conditions of immigration. Med Anthropol Q 1999;13(1):32–50 [DOI] [PubMed] [Google Scholar]
- 40.Cha D. Hmong American Concepts of Health, Healing, and Conventional Medicine New York, NY: Routledge; 2003 [Google Scholar]
- 41.Hickman JR. “Is it the spirit or the body?”: syncretism of health beliefs among Hmong immigrants to Alaska. NAPA Bull 2007;27(1):176–195 [Google Scholar]
- 42.Alessandrini EA, Shaw KN, Bilker WB, et al. Effects of Medicaid managed care on quality: childhood immunizations. Pediatrics 2001;107(6):1335–1342 [DOI] [PubMed] [Google Scholar]
- 43.Lieu TA, Black SB, Ray P, et al. Risk factors for delayed immunization among children in an HMO. Am J Public Health 1994;84(10):1621–1625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Johnson SK. Hmong health beliefs and experiences in the Western healthcare system. J Transcult Nurs 2002;13(2):126–132 [DOI] [PubMed] [Google Scholar]
- 45.Plotnikoff GA, Numrich C, Wu C, et al. Hmong shamanism. Animist spiritual healing in Minnesota. Minn Med 2002;85(6):29–34 [PubMed] [Google Scholar]
- 46.Pinzon-Perez H, Moua N, Perez MA. Understanding satisfaction with Shamanic practices among the Hmong in rural California. Int Electron J Health Educ 2005;8:18–23 [Google Scholar]
- 47.Detjen MG. Health and Acculturation of Hmong in the United States [dissertation] Madison: University of Wisconsin; 2008 [Google Scholar]
- 48.Hein J. Ethnic Origins: The Adaptation of Cambodian and Hmong Refugees in Four American cities New York, NY: Russell Sage Foundation; 2006 [Google Scholar]
- 49.Reeves TJ, Bennett CE. We the people: Asians in the United States. Census 2000 Special Reports. December 2004. Available at: http://www.census.gov/prod/2004pubs/censr-17.pdf. Accessed March 18, 2009