Abstract
Background
There is limited information regarding revision total knee arthroplasty (TKA) with respect to etiology, outcome, and long-term survival comparing different implant types.
Questions/purposes
We compared patient outcomes, survivorship and modes of failure and the most common etiologic factors for rerevision between different revision implant types.
Methods
We retrospectively reviewed 349 cases of revision TKA in 343 patients whose mean age was 67.8 years. Three implant types were used: posterior stabilized, condylar constrained knee, and rotating hinge. The etiologies included infection (32.7%), aseptic loosening (14.9%), and polyethylene wear (12.3%). The minimum followup was 12 months (mean, 57.7 months; range, 12–120 months).
Results
The mean Knee Society scores were 89 (range, 48–94), 88.9 (range, 45–95), and 84 (range, 56–94) and the mean ranges of motion were 110.0° (range, 70°–125°), 106.1° (range, 70°–120°), and 111.7° (range, 85°–125°) for the posterior stabilized, condylar constrained knee, and rotating hinge types, respectively. The rotating hinge group had the highest satisfaction rates (88%). Overall 10-year survivorship was 90.6% with highest survivorship seen in the rotating hinge group. The most common causes for rerevision were infection (2.9% of our cohort), instability (1.7%), and aseptic loosening (1.4%). The mean overall time to rerevision was 69.9 months (range, 11–119 months).
Conclusions
In our experience periprosthetic infection is the most common cause of failure of both primary and revision TKA. Functional outcome and range of motion improve irrespective of revision implant type. The rotating hinge prosthesis provides patient satisfaction and survivorship similar to that of other implant types.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
As a result of the success of TKA [3, 5, 16, 19], its indications have widened to include younger and more active patients, increasing the demand for the procedure. The number of revision TKAs is therefore also rising with a projected increase of 601% from 2005 to 2030 [22]. Furthermore, greater than 50% of these revision procedures are expected to occur in the younger age groups by 2011 [23].
Revision TKA must address soft tissue integrity and bone stock, which are often compromised. The surgical decision of implant choice must be based on these factors. Contemporary designs of revision TKA prostheses have evolved to provide systems with increasing levels of constraint. The modular posterior stabilized implant design requires a functional soft tissue envelope with varus-valgus and anteroposterior stability. They have been successfully used in revision, particularly in conversion of UKA to TKA [17, 24]. Constrained implants include the nonlinked condylar constrained and the linked rotating hinge designs. They are used in cases of valgus-varus instability and/or increased flexion gap laxity. The rotating hinge variety is generally reserved for the more severe cases or elderly patients with low functional demand and is perceived as providing poorer patient outcomes. Controversy remains with regard to the relative indications for different revision implant types with little published information on outcomes comparing the different designs [26, 28]. Although causes of failure and survivorship are well-documented for primary TKA, similar data on revision procedures are lacking [9]. Furthermore, the largest studies have been reported from the United States, which supposes a specific patient population.
The objective of this study was to review our experience of a large cohort of revision TKA cases from a single tertiary referral center. Our primary aim was to compare the clinical outcome of the different revision implant types using the American Knee Society Score (AKSS) and ROM. We also wished to analyze survivorship and modes of failure of these revision TKAs and, finally, to assess the most common etiologic factors leading to rerevision.
Patients and Methods
We carried out a retrospective review of prospectively collected data entered in our database of revision TKAs. All operations were performed between January 1999 and February 2008 at our institution. Our exclusion criteria included patients with simple débridement and washout, simple liner exchange, fracture fixation, or an isolated patellar resurfacing. The minimum followup postoperatively was 1 year (mean, 57.7 months; range, 12–120 months). After exclusion, we were left with 349 revision TKAs in 343 patients who were eligible and included in the study. Six patients underwent staged bilateral revision procedures. Two hundred ninety-two cases were referred from an outside institution. The average age was 67.8 years (range, 32–94 years). The average body mass index (BMI) was 25.14 kg/m2 (range, 18.9–46.6 kg/m2). There were 204 (59.5%) males and 139 (40.5%) females. The average interval from the primary TKA to the revision procedure was 84.3 months (range, 1–167 months). The cause of failure requiring revision surgery was determined by a full history, clinical examination, radiologic investigations, and intraoperative findings including examination under anesthesia, inspection of the explanted components, and results of tissue and fluid cultures. Isolated wear was differentiated from aseptic loosening intraoperatively in which there was absence of concomitant osteolysis and migration. One hundred twelve (32.1%) patients underwent revision TKA within 2 years of the primary procedure, whereas 237 (67.9%) patients underwent revision TKA more than 2 years after their primary procedure. There were 18 recorded deaths at final review.
Surgery was carried out using a standard technique with an incision usually through the previous scar; the most lateral scar was used where multiple scars were present. An extended medial parapatellar arthrotomy was used in the majority of cases but a patellar turn-down (15 patients), rectus snip (104 patients), or tibial tubercle osteotomy (24 patients) was also used in cases of difficult exposure.
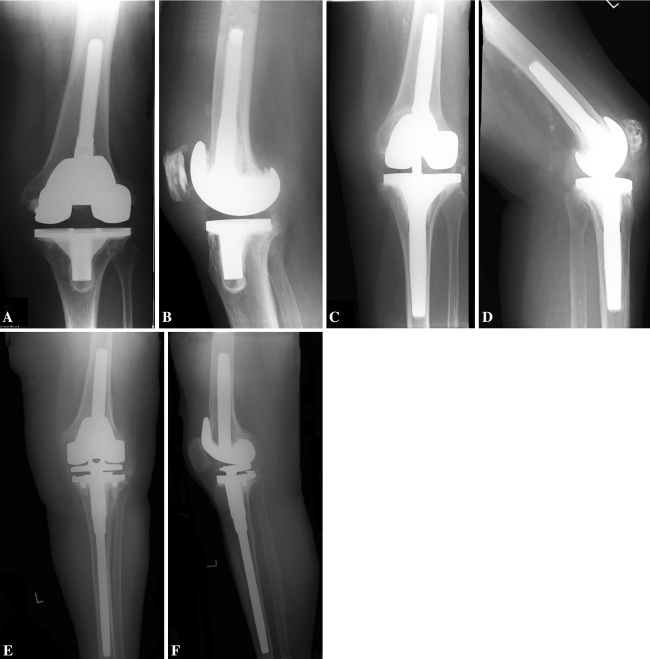
The choice of implant design was based on thorough preoperative and intraoperative evaluation. Implant choice was dictated by the extent of integrity of surrounding soft tissue structures providing stability to the knee and the extent of periarticular, metaphyseal, and even diaphyseal bone defects. We have been using the posterior stabilized (PS), condylar constrained knee (CCK) implant, and rotating hinge (RH) revision TKA implants concurrently at our institution. In cases in which collateral ligaments were intact and functional, providing valgus-varus stability, a PS implant would be used. The most common etiology in which a PS implant was used was conversion of a UKA to a TKA resulting from disease progression followed by malalignment and aseptic loosening. Our implant of choice was the PFC Sigma Cruciate Substituting (DePuy, Warsaw, IN) prosthesis. Small cavitatory periarticular defects would undergo augmentation with either cement or bone graft. In cases of partially intact or functioning collateral ligaments, cases with valgus-varus deformities of greater than 15° or with flexion-extension gap mismatches that may predispose to cam dissociation of a standard modular PS design, a CCK implant was considered. We used Total Condylar III (DePuy, Johnson & Johnson, Warsaw, IN) as our CCK prosthesis of choice. Larger periarticular and metaphyseal defects would be restored to achieve a normal joint line using modular metal augment options. We would use a RH prosthesis in cases in which there is complete absence of collateral ligament support or in cases of very severe valgus-varus deformity and flexion contracture, which would necessitate the complete release of the collateral ligaments. Cases of severe flexion gap laxity, which may predispose to cam dissociation and dislocation even in an unlinked constrained CCK prosthesis or with bone defects that may not be amenable to joint line restoration with metal augments, would be revised using the RH design. We used the customized SMILES prosthesis (Stanmore Implants, Elstree, UK) on a patient-by-patient basis based on bilateral long-leg measurement radiographs. The MRH system (Stryker, Kalamazoo, MI) and the S-ROM Noiles (DePuy), which has fixed embedded valgus angles of 6° and 7°, respectively, were also used. In cases of poor metaphyseal bone stock, judged to require diaphyseal fixation for stability, stemmed femoral or tibial components were used. Most CCK and all RH implant were stemmed. Cemented stem fixation would be reserved for the elderly population or those with osteoporotic bone except in cases of the RH implant in which we favor cemented stem fixation. This is the result of our experience of patients returning pain at the tip of uncemented stems. A modular PS implant was used in 126 (36.1%) cases; 72 cases had stemless fixation, 39 uncemented stems, and 15 cemented stems. A CCK implant was used in 149 cases; 40 cases had stemless fixation, 62 uncemented stems, and 47 cemented stems. A RH implant was used in 74 cases; 20 cases had uncemented stem fixation and 54 cemented stem fixation (Fig. 1). Two hundred four patients underwent patellar resurfacing. Of the remainder, 79 had their previously resurfaced patella retained and 66 were deemed unreconstructable. All cases in the CCK and RH groups had revision of all components of the index procedure with 16 cases in the PS group undergoing a single component revision on either the tibial or femoral side. A two-stage technique was used in all cases in which infection was established preoperatively or on evidence of infected tissue intraoperatively. A single-stage technique was used in all other cases. All patients underwent chemical and mechanical thromboprophylaxis unless contraindicated. Physiotherapy was started in the hospital and continued after discharge. Parenteral antibiotic therapy was administered for 5 days in all cases with extended protocols for infected cases dependent on sensitivity. The most common organisms identified were coagulase-negative staphylococcus (35.1%) and Staphylococcus aureus (21.1%). Routine clinical and radiographic followup was undertaken at 6 weeks, 6 months, and yearly thereafter for all patients, including those referred from an outside institution.
Fig. 1A–F.
Radiographic images of a modular posterior stabilized implant are shown from (A) the anteroposterior view and (B) the lateral view. Radiographic images of a condylar constrained knee implant are shown from (C) the anterioposterior view and (D) the lateral view. Radiographic images of a rotating hinge implant are shown from (E) the anteroposterior view and (F) the lateral view.
Clinical evaluation was performed using the AKSS and ROM on all patients preoperatively and annually until latest followup. Clinical evaluation and ROM were measured passively by a single observer (JT) using a goniometer with the patient in the supine position. We compared the mean AKSS scores and ROM at latest followup with the preoperative values. Three hundred six of 343 patients had recorded entries for AKSS preoperatively and at latest followup. Two of the authors (FH, SP) contacted all available patients by telephone and asked if they were satisfied after their revision TKA.
We calculated descriptive statistics (means, SD, and range) for continuous study variables. Outcome variables were compared using the analysis of covariance (ANCOVA) and analysis of variance tests for parametric data. The ANCOVA included covariate analysis of the potential confounding factors of age and BMI. Post hoc Tukey (honestly significant difference) test was used to compare the different implant groups. We used the chi square test to compare the dichotomous response satisfaction rates between the different implant groups and to determine the association between etiology of revision and demographic variables of age and BMI. Patients were categorized according to their age into either younger than 65 years or older than 65 years. BMI was categorized into underweight (less than 18.5 kg/m2), normal weight (18.5–24.9 kg/m2), overweight (25–29.9 kg/m2), obese (30–34.9 kg/m2), and very obese (greater than 35 kg/m2). We used Kaplan-Meier analysis to study survivorship of each implant; the end point was failure with rerevision for any reason. All statistical analyses were performed using XLSTAT (Version 7.0; Addinsoft, New York, NY).
Results
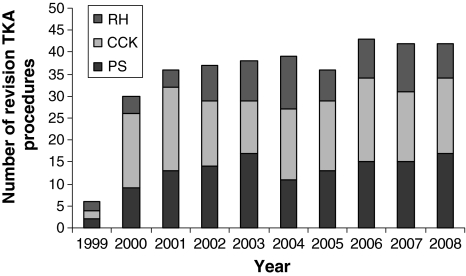
There was an overall rise in the number of cases per year for each implant type (Fig. 2). The most common reason for revision TKA amongst all patients was infection (114 patients [32.7%]). This accounted for 35.7% of patients revised at less than 2 years from the primary procedure and 31.2% of patients revised at greater than 2 years. Aseptic loosening (52 patients [14.9%]), polyethylene wear (43 patients [12.3%]), and conversion of UKA resulting from disease progression (29 patients [8.3%]) were other common modes of failure requiring revision TKA (Table 1). With regard to age, polyethylene wear (p = 0.005) and conversion of UKA (p < 0.001) were associated with patients younger than 65 years of age. Infection (p = 0.001) and periprosthetic fractures (p < 0.001) were associated with patients older than 65 years of age. Aseptic loosening (p = 0.003) and conversion of UKA (p = 0.041) were the only indications for revision TKA associated with an increasing BMI.
Fig. 2.
A graph shows trends in the incidence of revision TKA at our institution using rotating hinge (RH), condylar constrained knee (CCK), and posterior stabilized (PS) implants.
Table 1.
Indications for revision TKA in our cohort
| Cause for revision | Time from index to revision | |
|---|---|---|
| Less than 2 years (%) | Greater than 2 years (%) | |
| Aseptic loosening | 10 (2.9) | 42 (12.0) |
| Wear | 3 (0.9) | 40 (11.5) |
| Instability | 15 (4.3) | 12 (3.4) |
| Infection | 40 (11.5) | 74 (21.2) |
| Fracture | 6 (1.7) | 23 (6.6) |
| Patella | 10 (2.9) | 5 (1.4) |
| Conversion of unicompartmental replacement | 4 (1.1) | 25 (7.1) |
| Malalignment | 13 (3.7) | 10 (2.9) |
| Component failure | 1 (0.3) | 2 (0.6) |
| Extensor mechanism failure | 2 (0.6) | 3 (0.9) |
| Stiffness | 8 (2.3) | 1 (0.2) |
| Total | 112 | 237 |
A significant difference was noted between pre- and postrevision surgery ROM and AKSS scores for all three implant groups. There was a mean improvement in ROM from 101.9° to 108.7° (p < 0.0001), whereas mean AKSS improved from 33.8 to 87.9 (p < 0.0001) (Table 2).
Table 2.
Pre- and postoperative outcome variables in our cohort of revision TKAs
| Implant | Preoperative ROM (SD, range) | Postoperative ROM (SD, range) | p value |
|---|---|---|---|
| All | 101.9° (17.1, 40–130) | 108.7° (10.5, 70–125) | < 0.0001 |
| PS | 103.0° (19.6, 45–125) | 110.0° (9.1, 70–125) | < 0.0001 |
| CCK | 102.0° (15.5, 60–130) | 106.1° (11.9, 70–120) | < 0.0001 |
| RH | 100.1° (15.5, 40–115) | 111.7° (8.5, 85–125) | < 0.0001 |
| Implant | Preoperative AKSS (SD, range) | Postoperative AKSS (SD, range) | p value |
|---|---|---|---|
| All | 33.8 (9.6, 21–71) | 87.9 (6.5, 45–95) | < 0.0001 |
| PS | 35.2 (9.8, 25–71) | 89.0 (5.9, 48–94) | < 0.0001 |
| CCK | 34.1 (9.2, 25–71) | 88.9 (4.3, 45–95) | < 0.0001 |
| RH | 31.0 (9.5, 21–68) | 84.0 (9.0, 56–94) | < 0.0001 |
PS = posterior stabilized; CCK = condylar constrained knee; RH = rotating hinge; AKSS = American Knee Society Clinical Score.
The choice of implant design best predicted the ROM (p < 0.0001) and AKSS (p < 0.0001) after revision TKA once age and BMI had been accounted for as covariates. For ROM and AKSS, the largest contributions toward significance were age (p < 0.0001, p < 0.0001) and type of implant (p = 0.005, p < 0.0001), whereas BMI did not contribute (p = 0.73, p = 0.55). There was a difference in ROM (p = 0.0001) among the three different implant types. Post hoc analysis demonstrated lower AKSS in the RH group compared with either the PS (p < 0.0001) or CCK (p < 0.0001) groups, although no difference was seen between these latter groups (p = 0.88). Similar analysis demonstrated ROM was lower in the CCK group (PS: p = 0.0001, RH: p < 0.0001); no difference was found for ROM between the PS and RH groups (p = 0.22). One hundred seven (85%) patients in the PS group, 122 (82%) patients in the CCK group, and 65 (88%) patients in the RH group were satisfied with their revision TKA. There was no difference between the groups in that regard (p = 0.50).
The overall survivorship for revision TKA is 90.6% (95% confidence interval [CI], 87.3%–93.9%). Survivorship at 10 years was 90.3% (95% CI, 84.9%–95.8%) for the PS group, 89.3% (95% CI, 84.7%–95.0%) for the CCK group, and 92.5% (95% CI, 85.6%–99.3%) for the RH group.
The most common causes for rerevision were infection (2.9%), instability (1.7%), and aseptic loosening (1.4%) (Table 3). The mean overall time to rerevision was 69.9 months (SD, 26.8; range, 11–119 months).
Table 3.
Causes of failure of revision TKA with mean times to rerevision surgery
| Cause for rerevision | Type of implant | |||||
|---|---|---|---|---|---|---|
| PS | CCK | RH | ||||
| Number of cases | Mean time to rerevision (months) | Number of cases | Mean time to rerevision (months) | Number of cases | Mean time to rerevision (months) | |
| Aseptic loosening | 2 | 96.5 | 1 | 72 | 2 | 65.5 |
| Instability | 3 | 58 | 3 | 87.3 | ||
| Infection | 2 | 77 | 6 | 66.8 | 2 | 71.5 |
| Fracture | 2 | 65.5 | 1 | 72 | ||
| Patella | 3 | 87.3 | ||||
| Extensor mechanism failure | 2 | 59.5 | ||||
| Stiffness | 3 | 40.7 | ||||
PS = posterior stabilized; CCK = condylar constrained knee; RH = rotating hinge.
Discussion
The aim of our study was to present the longest followup of the largest series of revision TKA cases from a tertiary referral centre in a UK setting. We examined the etiology of revision TKA and compared its association with demographic variables, including age and BMI, showing periprosthetic infection and aseptic loosening as the most common reasons for revision TKA. We compared AKSS, patient satisfaction, ROM, and survivorship among the three different revision implant types. Although AKSS and ROM were lowest in the RH group, patient satisfaction and survivorship were better compared with other implant types.
Our study is limited by its retrospective design. Patient satisfaction was assessed with a dichotomous “yes/no” response as opposed to a scaled response, which may have provided a more precise assessment. More than two-thirds of our patients were referred from a different institution. There is variability in the final followup interval at which patient-reported outcomes were recorded. Nonetheless, our study represents a very large cohort of revision TKA cases in which data have been collected in a blinded manner.
The most common etiology leading to the need for revision was periprosthetic infection, which accounted for over 30% of cases. This is in agreement with other single-center studies [10, 36] as well as that of Bozic et al. [6] who reported infection to be the most frequent indication for revision TKA from a stratified US sample of 60,355 cases. Theirs remains the largest such study undertaken to date. Other studies meanwhile report aseptic loosening and polyethylene wear as the most common reasons for revision TKA [32, 33]. Data from the national joint registry of England and Wales have also shown aseptic loosening to be the most common etiologic factor for revision TKA accounting for 38% of cases nationwide. This was followed by periprosthetic infections accounting for 24% of the cases [9]. A similar trend in etiology has also been seen in the Swedish and Australian Arthroplasty registry reports [2, 24]. Our institution is a regional tertiary referral center for infected arthroplasty cases, which explains why our data are in agreement with the former rather than the latter studies. Revision from a UKA to a TKA resulting from disease progression is also a common indication in our series, which we found to be strongly associated with young patients and increasing BMI. The Swedish knee arthroplasty register, although identifying aseptic loosening as the dominant cause for failure of primary UKA, has also shown progression of disease as a significant etiology accounting for over 20% of the revisions of UKA cases nationwide [24].
Our data show an association between polyethylene wear and age less than 65 years as an indication for revision TKA. It is believed that although primary TKA restores activity in younger patients, this precipitates increased wear, thus promoting early failure [27]. Periprosthetic fractures were common in patients older than 65 years of age in our series, which is likely to be multifactorial. Reasons include an increased predisposition to falls and poor bone quality [15]. Foran et al. [11] suggest there is a trend for obesity to influence aseptic loosening after primary TKA, although this could not be statistically proven in their sample of 60 cases. In our cohort, however, with a larger number of patients, this association reached statistical significance. The association between other complications, including infection, is less clear. Although there is evidence to suggest a link between obesity and deep infection [8, 29], our data did not demonstrate this. Our data are similar to a previous report of 320 TKAs, which showed no difference in terms of infection rates between gender-specific groups of generally obese and nonobese patients [1]. Furthermore, recent studies relating obesity as a risk factor for periprosthetic infection implicate morbid obesity with a BMI of greater than 40 or 50 kg/m2 [25, 30]. In our cohort of patients, there were only three patients matching this criterion.
The indications for revision implant systems such as the RH are constantly evolving [26, 28]. Our threshold for using this implant is decreasing and this is reflected by its increasing use in our cohort after 2001 with a resultant decrease in CCK use (Fig. 1). Arthroplasty registries primarily communicate outcomes in terms of implant survivorship, which may not necessarily reflect patient functional outcomes or satisfaction [31]. There are few reports comparing outcomes between the different implant types in revision TKA [28]. We demonstrated a major improvement in patient outcome and ROM after revision TKA irrespective of implant type. This was not affected by BMI and is in agreement with other studies [1, 14]. The scale of improvement after revision TKA is similar among the three implant groups. Furthermore, satisfaction rates were similar in the three implant groups. Post hoc testing in our study demonstrated poorer AKSS in the RH group compared with the CCK and PS groups. Although this is in keeping with a previous study, which demonstrated better outcomes with a CCK implant type as compared with an older-generation RH prosthesis [13], our AKSS scores within the RH group at final followup are comparable to those of more recent accounts of contemporary RH designs [3, 18, 37]. Patients within the RH group in our study had a higher mean age than in the PS and CCK groups, which may be a causative factor for the comparatively lower AKSS; they also invariably were the group with the greatest bone and soft tissue loss, hence the choice of an RH implant. Although not significant, the group also had higher satisfaction rates as compared with the PS and CCK groups. This may be attributable to lower expectations among these patients as a result of their low preoperative function as illustrated by their lowest preoperative AKSS. There is evidence to suggest age as a demographic variable has a negative correlation with knee outcome scores [7]. In addition, a previous meta-analysis review has failed to show a difference in patient outcomes among different revision implant types [33]. ROM is similar between the RH and PS groups, which agrees with previous work comparing the RH design with a condylar design in revision TKA [4]. Kinematic studies of the native knee have demonstrated axial rotation during flexion and extension [12, 21]. The lack of rotational freedom in a CCK implant may result in reduced ROM. Nonetheless, our patient outcome results within the CCK group are comparable to that of other centers that successfully use the implant [20].
Overall survivorship in our cohort after revision TKA at 10 years is 90.6%. Using rerevision as the end point, data from the Finnish arthroplasty registry demonstrated a 10-year survival rate of 79% [34]. Our results also compare favorably to a recent review of 640 revision TKAs with a 9-year survival rate of 85% [35]. This study also identifies infection (46% of cases), instability, and aseptic loosening as the predominant reasons for rerevision. Our cohort of revision TKAs showed a similar trend in which periprosthetic infection, aseptic loosening, and instability accounted for the majority of rerevisions.
Our data suggest periprosthetic infection is the most common etiology for revision and rerevision TKA, especially in the elderly. Younger age group and an increasing BMI play a role in aseptic loosening as a cause for revision TKA. All three revision implant designs demonstrate clear improvements in function and ROM. The RH implant design provides equivalent patient satisfaction and survivorship in comparison to the other constrained and semiconstrained implant types.
Acknowledgments
We thank Jenni Tahmasebbi (JT) for her assistance in patient evaluation and assessment of patient outcome.
Footnotes
One of the authors (FSH) receives research funding from Smith and Nephew, Stryker, and Finsbury Orthopaedics.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at University College Hospital, London, UK.
References
- 1.Amin AK, Patton JT, Cook RE, Brenkel IJ. Does obesity influence the clinical outcome at five years following total knee replacement for osteoarthritis? J Bone Joint Surg Br. 2006;88:335–340. doi: 10.1302/0301-620X.88B3.16488. [DOI] [PubMed] [Google Scholar]
- 2.Australian Orthopaedic Association National Joint Registry Annual Report. Adelaide, Australia: AOA; 2009.
- 3.Barrack RL. Evolution of the rotating hinge for complex total knee arthroplasty. Clin Orthop Relat Res. 2001;392:292–299. doi: 10.1097/00003086-200111000-00038. [DOI] [PubMed] [Google Scholar]
- 4.Barrack RL, Lyons TR, Ingraham RQ, Johnson JC. The use of a modular rotating hinge component in salvage revision total knee arthroplasty. J Arthroplasty. 2000;15:858–866. doi: 10.1054/arth.2000.9056. [DOI] [PubMed] [Google Scholar]
- 5.Berger RA, Rosenberg AG, Barden RM, Sheinkop MB, Jacobs JJ, Galante JO. Long-term followup of the Miller-Galante total knee replacement. Clin Orthop Relat Res. 2001;388:58–67. doi: 10.1097/00003086-200107000-00010. [DOI] [PubMed] [Google Scholar]
- 6.Bozic KJ, Kurtz SM, Lau E, Ong K, Chiu V, Vail TP, Rubash HE, Berry DJ. The epidemiology of revision total knee arthroplasty in the United States. Clin Orthop Relat Res. 2009 Jun 25 [Epub ahead of print]. [DOI] [PMC free article] [PubMed]
- 7.Bremner-Smith AT, Ewings P, Weale AE. Knee scores in a ‘normal’ elderly population. Knee. 2004;11:279–282. doi: 10.1016/j.knee.2003.06.001. [DOI] [PubMed] [Google Scholar]
- 8.Dowsey MM, Choong PF. Obese diabetic patients are at substantial risk for deep infection after primary TKA. Clin Orthop Relat Res. 2009;467:1577–1581. doi: 10.1007/s11999-008-0551-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Emsley D, Martin J, Newell C, Pickford M, Royall M, Swanson M. The National Joint Registry 5thAnnual Report. Hemel Hempstead, UK: National Joint Registry; 2008.
- 10.Fehring TK, Odum S, Griffin WL, Mason JB, Nadaud M. Early failures in total knee arthroplasty. Clin Orthop Relat Res. 2001;392:315–318. doi: 10.1097/00003086-200111000-00041. [DOI] [PubMed] [Google Scholar]
- 11.Foran JR, Mont MA, Rajadhyaksha AD, Jones LC, Etienne G, Hungerford DS. Total knee arthroplasty in obese patients: a comparison with a matched control group. J Arthroplasty. 2004;19:817–824. doi: 10.1016/j.arth.2004.03.017. [DOI] [PubMed] [Google Scholar]
- 12.Freeman MA, Pinskerova V. The movement of the normal tibio-femoral joint. J Biomech. 2005;38:197–208. doi: 10.1016/j.jbiomech.2004.02.006. [DOI] [PubMed] [Google Scholar]
- 13.Goldberg VM, Figgie MP, Figgie HE, III, Sobel M. The results of revision total knee arthroplasty. Clin Orthop Relat Res. 1988;226:86–92. [PubMed] [Google Scholar]
- 14.Hamoui N, Kantor S, Vince K, Crookes PF. Long-term outcome of total knee replacement: does obesity matter? Obes Surg. 2006;16:35–38. doi: 10.1381/096089206775222140. [DOI] [PubMed] [Google Scholar]
- 15.Hernigou P, Mathieu G, Filippini P, Demoura A. Intra- and postoperative fractures of the femur in total knee arthroplasty: risk factors in 32 cases [in French] Rev Chir Orthop Reparatrice Appar Mot. 2006;92:140–147. doi: 10.1016/s0035-1040(06)75699-9. [DOI] [PubMed] [Google Scholar]
- 16.Indelli PF, Aglietti P, Buzzi R, Baldini A. The Insall-Burstein II prosthesis: a 5- to 9-year follow-up study in osteoarthritic knees. J Arthroplasty. 2002;17:544–549. doi: 10.1054/arth.2002.32186. [DOI] [PubMed] [Google Scholar]
- 17.Johnson S, Jones P, Newman JH. The survivorship and results of total knee replacements converted from unicompartmental knee replacements. Knee. 2007;14:154–157. doi: 10.1016/j.knee.2006.11.012. [DOI] [PubMed] [Google Scholar]
- 18.Joshi N, Navarro-Quilis A. Is there a place for rotating-hinge arthroplasty in knee revision surgery for aseptic loosening? J Arthroplasty. 2008;23:1204–1211. doi: 10.1016/j.arth.2007.10.016. [DOI] [PubMed] [Google Scholar]
- 19.Keating EM, Meding JB, Faris PM, Ritter MA. Long-term followup of nonmodular total knee replacements. Clin Orthop Relat Res. 2002;404:34–39. doi: 10.1097/00003086-200211000-00007. [DOI] [PubMed] [Google Scholar]
- 20.Kim YH, Kim JS. Revision total knee arthroplasty with use of a constrained condylar knee prosthesis. J Bone Joint Surg Am. 2009;91:1440–1447. doi: 10.2106/JBJS.H.00425. [DOI] [PubMed] [Google Scholar]
- 21.Koo S, Andriacchi TP. The knee joint center of rotation is predominantly on the lateral side during normal walking. J Biomech. 2008;41:1269–1273. doi: 10.1016/j.jbiomech.2008.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 23.Kurtz SM, Lau E, Ong K, Zhao K, Kelly M, Bozic KJ. Future young patient demand for primary and revision joint replacement: national projections from 2010 to 2030. Clin Orthop Relat Res. 2009;467:2606–2612. doi: 10.1007/s11999-009-0834-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lidgren L, Robertsson O, Dahl A. The Swedish Arthroplasty Register—Annual Report 2009. Lund, Sweden: Wallin & Dalholm AB; 2009:48.
- 25.Malinzak RA, Ritter MA, Berend ME, Meding JB, Olberding EM, Davis KE. Morbidly obese, diabetic, younger, and unilateral joint arthroplasty patients have elevated total joint arthroplasty infection rates. J Arthroplasty. 2009;24(Suppl):84–88. doi: 10.1016/j.arth.2009.05.016. [DOI] [PubMed] [Google Scholar]
- 26.McAuley JP, Engh GA. Constraint in total knee arthroplasty: when and what? J Arthroplasty. 2003;18:51–54. doi: 10.1054/arth.2003.50103. [DOI] [PubMed] [Google Scholar]
- 27.Naudie DD, Ammeen DJ, Engh GA, Rorabeck CH. Wear and osteolysis around total knee arthroplasty. J Am Acad Orthop Surg. 2007;15:53–64. doi: 10.5435/00124635-200701000-00006. [DOI] [PubMed] [Google Scholar]
- 28.Nelson CL, Gioe TJ, Cheng EY, Thompson RC., Jr Implant selection in revision total knee arthroplasty. J Bone Joint Surg Am. 2003;85(Suppl 1):S43–S51. doi: 10.2106/00004623-200300001-00009. [DOI] [PubMed] [Google Scholar]
- 29.Patel VP, Walsh M, Sehgal B, Preston C, DeWal H, Di Cesare PE. Factors associated with prolonged wound drainage after primary total hip and knee arthroplasty. J Bone Joint Surg Am. 2007;89:33–38. doi: 10.2106/JBJS.F.00163. [DOI] [PubMed] [Google Scholar]
- 30.Pulido L, Ghanem E, Joshi A, Purtill JJ, Parvizi J. Periprosthetic joint infection: the incidence, timing, and predisposing factors. Clin Orthop Relat Res. 2008;466:1710–1715. doi: 10.1007/s11999-008-0209-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Serra-Sutton V, Allepuz A, Espallargues M, Labek G, Pons JM. Arthroplasty registers: a review of international experiences. Int J Technol Assess Health Care. 2009;25:63–72. doi: 10.1017/S0266462309090096. [DOI] [PubMed] [Google Scholar]
- 32.Sharkey PF, Hozack WJ, Rothman RH, Shastri S, Jacoby SM. Insall Award paper. Why are total knee arthroplasties failing today? Clin Orthop Relat Res. 2002;404:7–13. doi: 10.1097/00003086-200211000-00003. [DOI] [PubMed] [Google Scholar]
- 33.Sheng P, Lehto M, Kataja M, Halonen P, Moilanen T, Pajamaki J. Patient outcome following revision total knee arthroplasty: a meta-analysis. Int Orthop. 2004;28:78–81. doi: 10.1007/s00264-003-0526-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sheng PY, Konttinen L, Lehto M, Ogino D, Jamsen E, Nevalainen J, Pajamaki J, Halonen P, Konttinen YT. Revision total knee arthroplasty: 1990 through 2002. A review of the Finnish arthroplasty registry. J Bone Joint Surg Am. 2006;88:1425–1430. doi: 10.2106/JBJS.E.00737. [DOI] [PubMed] [Google Scholar]
- 35.Suarez J, Griffin W, Springer B, Fehring T, Mason JB, Odum S. Why do revision knee arthroplasties fail? J Arthroplasty. 2008;23:99–103. doi: 10.1016/j.arth.2008.04.020. [DOI] [PubMed] [Google Scholar]
- 36.Vessely MB, Whaley AL, Harmsen WS, Schleck CD, Berry DJ. The Chitranjan Ranawat Award: Long-term survivorship and failure modes of 1000 cemented condylar total knee arthroplasties. Clin Orthop Relat Res. 2006;452:28–34. doi: 10.1097/01.blo.0000229356.81749.11. [DOI] [PubMed] [Google Scholar]
- 37.Westrich GH, Mollano AV, Sculco TP, Buly RL, Laskin RS, Windsor R. Rotating hinge total knee arthroplasty in severely affected knees. Clin Orthop Relat Res. 2000;379:195–208. doi: 10.1097/00003086-200010000-00023. [DOI] [PubMed] [Google Scholar]