Abstract
Background
Rotating-hinge total knee prostheses may be used for the treatment of global instability about the knee. The designs of previous generations were associated with suboptimal outcomes.
Questions/purposes
We evaluated the clinical and radiographic outcomes of salvage knee reconstructions using modern-generation, modular, kinematic rotating-hinge total knee prostheses.
Methods
We retrospectively reviewed 26 rotating-hinge arthroplasty devices to examine whether acceptable results were obtainable using a single arthroplasty design. The average age of the patients was 77 years (SD, 9 years); the minimum followup was 24 months (mean, 46 months; range, 24–107 months). The indication was revision surgery in 21 patients and complex primary surgery in five. Patients were evaluated clinically (Knee Society score) and radiographically (positions of components, signs of loosening, bone loss).
Results
Knee Society pain scores improved from 40 preoperatively to 77 postoperatively, and function scores improved from 36 to 51. ROM improved from –15º to –10º. None of the patients’ knee pain or function worsened. No loosening of implants was observed. Nonprogressive radiolucent lines were identified around the femoral and tibial components in three knees. Three patients required reoperations: one showed a supracondylar periprosthetic fracture treated by open reduction and internal fixation, whereas the other two had periprosthetic infections.
Conclusions
Reconstruction with rotating-hinge total knee prostheses can provide substantial improvement in function and a reduction in pain in extreme circumstances, such as gross instability. We believe this salvage procedure should be reserved for severe ligamentous deficiencies in elderly and sedentary patients or whenever revision surgery techniques fail.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
A ligamentous deficiency in the knee can be related to a previous trauma, associated with severe varus-valgus deformities, or due to revision surgery associated with severe bone losses. This happens in the segmental type [9], combined epiphyseal and cavitary patterns, and types of bone destruction in which large portions of distal femur or proximal tibia are missing, which may include collateral ligament attachment.
Competent and functional collateral ligaments are a prerequisite when performing a conventional TKA [16]. In cases of primary surgery for knees with severe deformities or in revision surgery in knees with substantial bone loss, standard condylar implants do not allow for proper stabilization of the joint, even when using models with constraint. Under these circumstances, condylar TKA designs will fail within a short period of time [22].
Although attempts have been made to reconstruct the ligaments with grafts and reinsertion techniques, the results are poor and the failures caused by these techniques are difficult to solve [1–4, 13–15]. Rotating-hinge total knee prostheses may be used for the treatment of global instability or severe bone loss around the knee. Hinged prostheses were first designed and used for knee reconstruction after the resection of neoplasms. Fixed-hinge TKAs implanted in the middle of the last century led to a high percentage of failures [12]. However, these models have been improved with modular designs and a wider availability of sizes and different rotational systems, thus reducing the risk of aseptic loosening. Older generations of rotating-hinge designs were associated with suboptimal outcomes [11, 18, 19], but there have been improvements in the design of these prostheses in recent years, the most important of which are the ability of the implant to rotate and the introduction of metal wedge augmentation and modular fluted stems with variable offset, which improve the alignment and allow press-fit fixation [5–8, 20, 21, 23]. Complete systems using these designs are now available for primary complex surgery or for revision surgery. These designs provide a more congruent articulation, leading to a decrease in wear and transmitted stress at the bone-implant interface. The rotating-hinge arthroplasty offers enough stability, allowing for an intrinsic rotation that simulates the biomechanical reply of a normal knee and diminishes the stress produced by an elevated constriction. In much of the literature on these models, this indication is described together with others already in place (Table 1).
Table 1.
Indications for rotating-hinge arthroplasty
| Surgery | Indications |
|---|---|
| Primary | Large deformities |
| Comminuted distal femoral fractures in elderly patients | |
| Pseudoarthrosis or distal femoral fractures | |
| Absence or deficit of muscular control | |
| Tumoral surgery (bone block resection with ligamentous insertions needed) | |
| Congenital dislocation of knee | |
| Ankylosis with severe instability after surgical exposition | |
| Revision | Bone losses that cannot be reconstructed with allografts or metal augmentations |
| Losses that include collateral ligamentous insertions | |
| Revision of previous hinges | |
| Extensor mechanism injury in need of reconstruction in unstable knees | |
| Large flexion gap that impedes adequate stability with conventional TKAs | |
| Differences between flexion and extension gaps not recoverable with conventional TKAs | |
| Last resort when the only viable alternative is a complex arthrodesis |
Previous reports of patient series treated by modern rotating-hinge prostheses are difficult to compare because several different types of prostheses were often used and followups were fairly short. In this report, we aimed to provide a more meaningful clinical and radiographic evaluation of 26 rotating-hinge arthroplasties performed in our institution using a single type of prosthesis for patients with instability or severe bone loss. We evaluated the functional outcome of the knees, the radiographic results, and the potential medical and orthopaedic complications.
Patients and Methods
In this retrospective case series, we selected the records of 26 patients (five men, 21 women), when the key reason for selection of the rotating-hinge prosthesis was collateral ligament deficiency. In all patients, the TKA implanted was the Stryker Rotating Hinge Prosthesis (Stryker Orthopaedics, Mahwah, NJ). Minimum followup was 24 months (mean, 46 months; range, 24–107 months). No patients were lost to followup.
From these records, we extracted data concerning the patients and the procedures, including demographics, previous deformities, bone loss, diagnosis, and duration of followup after TKA. The mean body mass index was 31 (range, 18–52). The average age of the patients was 77 years (SD, 9 years). The indication was revision surgery in 21 patients and complex primary surgery in five. In revision surgery, large portions of distal femur or proximal tibia are missing, including ligamentous deficiency (segmental bone loss type according to Huff and Sculco’s simplified classification [9]). Three patients showed medial ligamentous deficiency, another five presented lateral ligamentous deficiency, and both ligaments were missing in the rest. These five knees had used the same arthroplastic model with independent polyethylenes (Interax® prosthesis; Stryker), which failed due to dislocation and early wear (Fig. 1). Of the five complex primary surgeries, two exhibited bone femoral loss (one medial and another lateral coupled with ligamentous deficiency). The other three knees featured a severe tibial deformity with lateral bone loss, medial ligamentous deficiency, and instability (Fig. 2). In these five knees, the deformity ranged between 20° varus and 30° valgus.
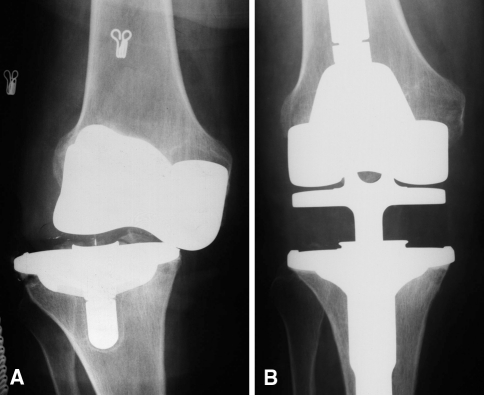
Fig. 1A–B.
(A) An AP radiograph shows polyethylene dislocation with severe lateral instability in an Interax® prosthesis. (B) An AP radiograph shows the knee 3 years after rotating-hinge arthroplasty.
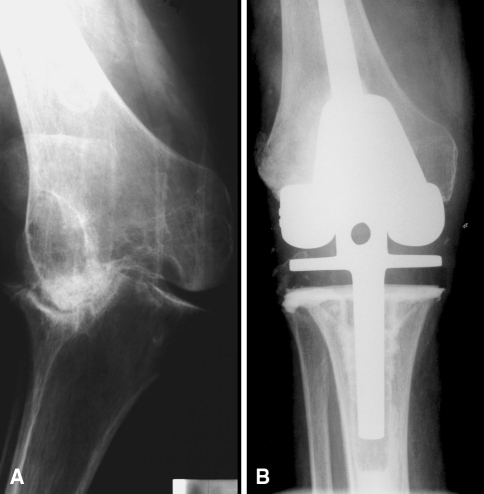
Fig. 2A–B.
(A) A radiograph shows severe deformity with medial instability. (B) A radiograph shows the knee 8 years after rotating-hinge arthroplasty.
All procedures were performed through a medial parapatellar arthrotomy and under tourniquet control. We used tibial cementation in all knees and femoral cementation in 14 patients; in the rest, a noncemented femoral stem of differing diameter was used, allowing each femur to be press-fit, optimizing fixation. Antibiotic-impregnated cement containing gentamicin was used in all knees. Polyethylene inserts longer than 10 mm in height were used to resolve four cases, and structural bone allografts were used to resolve another two. Most of the bone defects (< 1 cm) were resolved with cement, especially in older patients. In seven knees, metal tibial augments were used, and in six knees, metal femoral augments were used. Morselized bone allografts were not used. In three knees, it was necessary to reinforce the insertion of the extensor mechanism by placing two staples in the tibial insertion of the patellar tendon. These patients were casted in extension for 30 days after surgery. The postoperative management was similar for all patients and weightbearing with two crutches was allowed at 48 hours. Physical therapy was started after the seventh postoperative day whenever a 90° flexion was not achieved.
We assessed the clinical outcome using the Knee Society score (KSS), which was calculated before surgery and at the time of latest followup. Serial AP and lateral radiographs of the knee were reviewed in detail at the latest followup. The positions of the components were assessed by an orthopaedic surgeon (MASG) and were considered optimal if the tibiofemoral angle was within 3° of neutral alignment. Postoperative radiographs were also evaluated for signs of loosening and bone loss. The femur and tibia were divided into standard zones.
Changes in the KSS and ROM were evaluated via Student’s t test, and the level of significance was set at p < 0.05.
Results
Overall, the rotating-hinge arthroplasty resulted in improved knee functioning in this series of patients. Twenty-three patients were walking with one crutch and another three with two crutches at the last followup. The KSS improved (p < 0.001) from a preoperative mean of 40 points (SD, 17.6 points) to a postoperative mean of 77 points (SD, 14.8 points); the functional score improved (p = 0.09) from 36 points (SD, 29.7 points) to 51 points (SD, 33.2 points). ROM improved (p = 0.03) from –15° (SD, 8.78°) before TKA to –10° (SD, 7.37°) after TKA. None of the patients’ knee pain or function worsened.
In the radiographic analysis, nonprogressive radiolucent lines (> 2 mm) were identified around the femoral and tibial platforms or stems in three knees. In the femoral stem, they were located in Zone 4 in two knees and in Zone 6 in one knee. In the tibial stem, they appeared in Zone 3 in two knees and in Zone 2 in one knee. These lines remained stable throughout the study period. No loosening or subsidence was observed. The positions of the components were considered optimal in all knees except one (5º varus) and the tibiofemoral angle was considered optimal in 22 knees. The mean limb alignment was 4.5° valgus (range, −5° to 7° valgus).
Medical complications included postoperative confusion (one patient), pulmonary embolus (one patient), urinary tract infection (two patients), and exacerbation of chronic renal failure (one patient).
Due to orthopaedic complications, three patients required revision surgery. One showed a supracondylar periprosthetic fracture treated by open reduction and internal fixation. The other two had periprosthetic infections treated with a two-stage resection arthroplasty and reimplantation in one patient and via incision and drainage in the other. Five patients showed complications related to the patella and extensor mechanism. In two patients, the patella showed a subluxation in full flexion of the knee, which was well tolerated by the patients. As for the other three, it was necessary to reinforce the patellar tendon in surgery.
Discussion
Rotating-hinge total knee prostheses may be used for the treatment of global instability about the knee. The designs of previous generations were associated with suboptimal outcomes. We evaluated the clinical and radiographic outcomes of salvage knee reconstructions performed using modern-generation, modular, kinematic rotating-hinge total knee prostheses.
Our study has some limitations. First, it is retrospective and noncontrolled. The relatively short duration of followup and the relatively small patient population sample are also limitations. The study combined two groups of patients, primary and revision surgery, and the radiographic evaluation was carried out by only one surgeon.
Our study has demonstrated rotating-hinge prostheses are a correct alternative for ligamentous deficiencies both in primary surgery and in severe types of bone loss in revision surgery. We obtained an improvement in function, pain, and ROM of the knee. No patient got worse compared with preoperative status, but the use of crutches was required in all cases. For three patients, walking was difficult and required two crutches.
Postoperative radiographs showed nonprogressive radiolucent lines in only three knees. No loosening or subsidence of prostheses was observed at followup. The positions of the components were considered optimal in all knees except one. The mean limb alignment was 4.5° valgus, which is an acceptable result in this type of arthroplasty.
In spite of the high mean age of the patients (near 80 years old), medical complications were not common. As for orthopaedic complications, we observed one supracondylar periprosthetic fracture and two infections. Another two patients showed a patellar subluxation in maximum flexion, which was well tolerated.
The clinical outcome of the rotating-hinge TKA has been evaluated in several studies, and the results and the frequency of complications have been heterogeneous (Table 2). Comparisons among rotating-hinge series are difficult because several different types of prostheses are involved and followups are still relatively short. The earliest generation of rotating-hinge devices achieved slightly better results than the original fixed-hinge implants, but long-term results were still disappointing.
Table 2.
Comparison of studies of rotating-hinge prostheses
| Study | Year | Number of arthroplasties | Followup (months)* | Number of knees requiring revision surgery† |
|---|---|---|---|---|
| Westrich et al. [23] | 2000 | 24 | 33 (21–62) | 1 |
| Barrack [2] | 2001 | 23 | 58 (24–102) | 1 |
| Springer et al. [20] | 2001 | 69 | 72.5 (24–199) | 18 |
| Pour et al. [16] | 2007 | 44 | 50.4 (24–96) | 6 |
| Deehan et al. [7] | 2008 | 68 | 120 (36–216) | 4 |
| Joshi and Navarro-Quilis [10] | 2008 | 78 | 94 (56–130) | 8 |
| Hernández-Vaquero and Sandoval-Garcia | 2009 | 26 | 46 (24–107) | 2 |
* Values are expressed as medians, with ranges in parentheses; †nonperiprosthetic fractures.
Böhm and Holy [6] evaluated 422 consecutive primary TKAs using one specific design of hinged total knee prosthesis at a mean 6 years. The cumulative rates of survival at 20 years were from 86.8% to 96.0% depending on the end points, but because they were primary surgeries, their results cannot be compared with our series. Barrack [2] reported satisfying clinical results in a study of 23 modern-generation hinged TKAs evaluated at 2- to 9-year followup. The clinical results, ROM, and satisfaction were comparable to those of a standard condylar revision knee arthroplasty, despite the fact that the cases were more complex. Joshi and Navarro-Quilis [10] reviewed the results of 78 revision TKAs using a rotating-hinge device in patients requiring revision arthroplasty due to aseptic loosening. Fifty-seven patients showed excellent results, with a ROM of 104° in flexion and complete extension, better than our results. The seriousness of our cases can explain these differences in ROM.
Pradhan et al. [17] conducted a retrospective study of 51 rotating-hinge prostheses in revision surgery with a maximum followup of 6 years. Reasons for revision were infection and aseptic loosening in 46 cases. There was a notable improvement in the pain, stability, ROM, and mobility of the patients. Postoperatively, 33 presented excellent or good results (better results in patients with aseptic loosening). Pour et al. [16] included in their study 44 knee arthroplasties using modern-generation kinematic rotating-hinge prostheses with a mean followup of 4.2 years. The prostheses provided substantial improvement in function and reduction in pain, but a relatively large number of complications and failures (periprosthetic infection in three knees, aseptic loosening in four, and a periprosthetic fracture in one) were encountered. The rate of prosthetic survival was 68.2% at 5 years with revision or reoperation as the end point. Our results at the same followup are similar, but we did not find any cases of aseptic loosening.
A few reports have highlighted the major complications that can arise when using these fully constrained prostheses. Springer et al. [21] recently reported on the early results of distal femoral arthroplasty for nonneoplastic limb salvage in a study of 26 knees and highlighted some of the major associated complications. In that report, the periprosthetic infection (five knees) was the main cause of failure. This complication is present in all series and it also appears in ours. Kester et al. [11] studied one type of device, which was removed because of implant loosening with pain, while two prostheses also produced a late infection. Radiographically, all the devices showed signs of progressive radiolucencies. A marked varus drift was observed in eight (67%) of the retrieved prostheses. Seventy-three percent of the polyethylene tibial stems exhibited extensive wear on the anterior and medial aspects of the articulating surface. That study pinpoints serious design flaws in one type of rotating-hinge prosthesis, but these results cannot be used to make comparisons with other designs, such as those in our series. Wang and Wang [22] describe two rotating-hinge prostheses that dislocated as a result of mechanical failure of the prosthetic component within 5 months of initial implantation. This is a complication of a specific model, like that of the previous work. Clinicians should be aware of this potential complication when selecting rotating-hinge prostheses for certain patients.
A rotating-hinge knee prosthesis should be considered a salvage device and should be used primarily for elderly and sedentary patients with complex knee problems. Our experience with only one model at medium-length followup allows us to recommend this solution for certain patients who lack any other surgical options. Not knowing longer-term results, we believe this salvage procedure should be reserved primarily for cases in which other models could not be implanted or whenever revision surgery techniques fail. Reconstruction with a rotating-hinge total knee prosthesis can provide substantial improvement in function and a reduction in pain in knees with ligamentous deficiency. This procedure can be considered the reconstruction of last resort in the presence of a ligamentous instability (primary, traumatic, in revision surgery, or because of a tumor) which is unlikely to be controlled with other methods.
Acknowledgments
We thank J.M. Fernandez-Carreira, MD, for the statistical analysis.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at Hospital St Agustín and Department of Orthopaedic Surgery, School of Medicine, University of Oviedo.
References
- 1.Anderson JA, Baldini A, MacDonald JH, Pellicci PM, Sculco TP. Primary constrained condylar knee arthroplasty without stems extensions for the valgus knee. Clin Orthop Relat Res. 2006;442:199–203. doi: 10.1097/01.blo.0000185675.99696.29. [DOI] [PubMed] [Google Scholar]
- 2.Barrack RL. Evolution of the rotating hinge for complex total knee arthroplasty. Clin Orthop Relat Res. 2001;392:292–299. doi: 10.1097/00003086-200111000-00038. [DOI] [PubMed] [Google Scholar]
- 3.Barrack RL. Rise of the rotating hinge in revision total knee arthroplasty. Orthopedics. 2002;25:1020, 1058. [DOI] [PubMed]
- 4.Barrack RL, Lyons TR, Ingraham RQ, Johnson JC. The use of a modular rotating hinge component in salvage revision total knee arthroplasty. J Arthroplasty. 2000;15:858–866. doi: 10.1054/arth.2000.9056. [DOI] [PubMed] [Google Scholar]
- 5.Berend KR, Lombardi AV., Jr Distal femoral replacement in nontumor cases with severe bone loss and instability. Clin Orthop Relat Res. 2009;467:485–492. doi: 10.1007/s11999-008-0329-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Böhm P, Holy T. Is there a future for hinged prostheses in primary total knee arthroplasty? J Bone Joint Surg Br. 1998;80:302–309. doi: 10.1302/0301-620X.80B2.7905. [DOI] [PubMed] [Google Scholar]
- 7.Deehan DJ, Murray J, Birdsall PD, Holland JP, Pinder IM. The role of the rotating hinge prosthesis in the salvage arthroplasty setting. J Arthroplasty. 2008;23:683–688. doi: 10.1016/j.arth.2007.05.055. [DOI] [PubMed] [Google Scholar]
- 8.Hartford JM, Goodman SB, Schurman DJ, Knoblick G. Complex primary and revision total knee arthroplasty using the condylar constrained prosthesis: an average 5-year follow-up. J Arthroplasty. 1998;13:380–387. doi: 10.1016/S0883-5403(98)90002-X. [DOI] [PubMed] [Google Scholar]
- 9.Huff TW, Sculco TP. Management of bone loss in revision total knee arthroplasty. J Arthroplasty. 2007;22(7 Suppl 3):32–36. doi: 10.1016/j.arth.2007.05.022. [DOI] [PubMed] [Google Scholar]
- 10.Joshi N, Navarro-Quilis A. Is there a place for rotating-hinge arthroplasty in knee revision surgery for aseptic loosening? J Arthroplasty. 2008;23:1204–1211. doi: 10.1016/j.arth.2007.10.016. [DOI] [PubMed] [Google Scholar]
- 11.Kester MA, Cook SD, Harding AF, Rodriguez RP, Pipkin CS. An evaluation of the mechanical failure modalities of a rotating hinge knee prosthesis. Clin Orthop Relat Res. 1988;228:156–163. [PubMed] [Google Scholar]
- 12.McAuley JP, Engh GA. Constraint in total knee arthroplasty: when and what? J Arthroplasty. 2003;18:51–54. doi: 10.1054/arth.2003.50103. [DOI] [PubMed] [Google Scholar]
- 13.Nelson CL, Lonner JH, Rand JA, Lotke PA. Strategies of stems fixation and the role of supplemental bone graft in revision total knee arthroplasty. J Bone Joint Surg Am. 2003;85(Suppl 1):S52–S57. doi: 10.2106/00004623-200300001-00010. [DOI] [PubMed] [Google Scholar]
- 14.Parsley BS, Sugano N, Bertolusso R, Conditt MA. Mechanical alignment of tibial stems in revision total knee arthroplasty. J Arthroplasty. 2003;18(7 Suppl 1):33–36. doi: 10.1016/S0883-5403(03)00302-4. [DOI] [PubMed] [Google Scholar]
- 15.Petrou G, Petrou H, Tilkeridis C, Stavrakis T, Kapetsis T, Kremmidas N, Gavras M. Medium-term results with a primary cemented rotating-hinge total knee replacement: a 7- to 15-year follow-up. J Bone Joint Surg Br. 2004;86:813–817. doi: 10.1302/0301-620X.86B6.14708. [DOI] [PubMed] [Google Scholar]
- 16.Pour AE, Parvizi J, Slenker N, Purtill JJ, Sharkey PF. Rotating hinged total knee replacement: use with caution. J Bone Joint Surg Am. 2007;89:1735–1741. doi: 10.2106/JBJS.F.00893. [DOI] [PubMed] [Google Scholar]
- 17.Pradhan NR, Bale L, Kay P. Porter ML Salvage revision total knee replacement using the Endo-Model rotating hinge prosthesis. Knee. 2004;11:469–473. doi: 10.1016/j.knee.2004.03.001. [DOI] [PubMed] [Google Scholar]
- 18.Rand JA, Chao EY, Stauffer RN. Kinematic rotating-hinge total knee arthroplasty. J Bone Joint Surg Am. 1987;69:489–497. [PubMed] [Google Scholar]
- 19.Sharkey PF, Hozack WJ, Rothman RH, Shastri S, Jacoby SM. Why are total knee arthroplasties failing today? Clin Orthop Relat Res. 2002;404:7–13. doi: 10.1097/00003086-200211000-00003. [DOI] [PubMed] [Google Scholar]
- 20.Springer BD, Hanssen AD, Sim FH, Lewallen DG. The kinematic rotating hinge prosthesis for complex knee arthroplasty. Clin Orthop Relat Res. 2001;392:283–291. doi: 10.1097/00003086-200111000-00037. [DOI] [PubMed] [Google Scholar]
- 21.Springer BD, Sim FH, Hanssen AD, Lewallen DG. The modular segmental kinematic rotating hinge for nonneoplastic limb salvage. Clin Orthop Relat Res. 2004;421:181–187. doi: 10.1097/01.blo.0000126306.87452.59. [DOI] [PubMed] [Google Scholar]
- 22.Wang CJ, Wang HE. Early catastrophic failure of rotating hinge total knee prosthesis. J Arthroplasty. 2000;15:387–391. doi: 10.1016/S0883-5403(00)90877-5. [DOI] [PubMed] [Google Scholar]
- 23.Westrich GH, Molano AV, Sculco TP, Buly RL, Laskin RS, Windsor R. Rotating hinge total knee arthroplasty affected knees. Clin Orthop Relat Res. 2000;379:195–208. doi: 10.1097/00003086-200010000-00023. [DOI] [PubMed] [Google Scholar]