Abstract
The ZMR® porous stem is a modular cylindrical porous-coated femoral stem for revision THA. The objective of this study was to evaluate the clinical and radiographic outcomes of this stem at midterm followup. We prospectively reviewed 69 patients (72 femoral revisions) treated with the stem. The indication for revision was aseptic loosening in 61 (85%), periprosthetic fractures in five (7%), infection in three (4%), dislocation in two (3%), and fractured stem in one (1%). Minimum followup was 60 months (mean, 85 months; range, 60–114 months). The survival rate with revision for any reason as an end point was 93.8%. Mean preoperative Harris hip score was 39 points, and mean Harris hip score at last followup was 72 points. Four (5.5%) stems required rerevision, two (2.8%) for loosening, one (1.4%) for fracture at the modular junction, and one (1.4%) for infection. Subsidence occurred in eight (11%) patients, in the range of 5 to 25 mm. Two (2.89%) of the stems that subsided were symptomatic and progressive. The ZMR® porous stem is a versatile system that offers a reliable fixation and an off-the-shelf solution for a multitude of femoral reconstruction challenges.
Level of Evidence: Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
In performing revision THA, the main challenges presented to the surgeon are obtaining stable and durable component fixation and restoring joint kinematics in the face of varying amounts of bone loss and deformity. Femoral revisions in which bone loss is minimal can be dealt with using conventional or revision nonmodular stems [27]. However, in many situations, a deficient proximal femur will not reliably support such a component. Bone loss, secondary to osteolysis, infection, fracture, or the need to sacrifice bone stock while extracting a well-fixed stem has been managed by various techniques and implants. Long uncemented stems designed to bypass the proximal femur, relying on distal fixation of at least 4 to 7 cm for stability [3, 8, 15, 19, 28, 29], have had consistently low failure rates, with survival greater than 95% at 5 to 10 years, and good functional outcomes [3, 7, 8, 14–16, 24, 25]. Distal fixation stems may be modular or monoblock, with tapered, cylindrical, or fluted designs [8, 13].
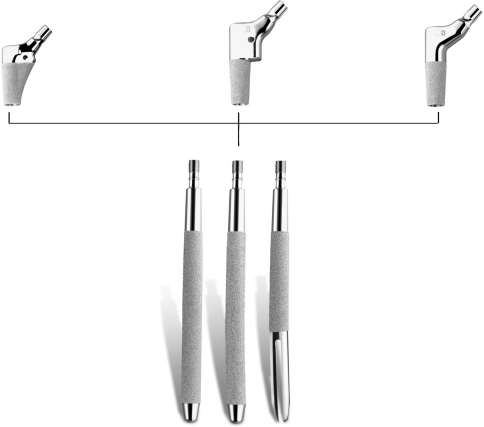
The two senior authors (AEG, DB) have been using a modular revision system (ZMR®; Zimmer, Inc, Warsaw IN) for the last 10 years. The stem is cylindrical with a circumferential coating of a porous, plasma-sprayed titanium alloy, which allows distal or extensive (proximal and distal) fixation. Three distinct porous-coated modular body configurations allow the surgeon flexibility with proximal fill and with restoration of the hip’s kinematics (Fig. 1). Previous reports presented encouraging results using this system [9, 13, 29].
Fig. 1.
A photograph shows the ZMR® porous stem (lower) and bodies (upper): the spout body (upper left), the calcar body (upper middle), and the cone body (upper right). (Photograph courtesy of and reprinted with permission of Zimmer, Inc, Warsaw, IN.)
The purposes of our study were (1) to assess the survival rate of the ZMR® porous stems at midterm followup, (2) to evaluate functional outcome (using the Harris hip score [HHS]) and complications, and (3) to assess the incidence, risk factors, and clinical significance of subsidence.
Materials and Methods
We performed femoral revision surgery in 95 patients (99 femoral revisions) between November 1999 and June 2004. We prospectively followed 78 of these patients (81 femoral revisions) in whom the ZMR® porous stem was used. The other 18 femoral revisions were performed using proximal femoral allografts. One patient died and eight were lost to followup before 5 years of followup were completed. Thus, 69 patients (72 femoral revisions) were available for evaluation. The mean age of the patients at the time of surgery was 70 years (range, 36–89 years). Included were 38 (55%) women and 31 (45%) men. The indication for 61 revisions (85%) was aseptic loosening. Five (7%) revisions were performed for periprosthetic fractures, three (4%) for infection (two-stage revision), two (3%) for instability, and one (1%) for a fractured stem. The study operation was a first THA revision for 38 (53%) patients, a second revision for 23 (32%), and a third to fifth revision for 11 (15%). The mean preoperative HHS was 39 points (range, 9–84 points). Bone deficiency in the femora was classified according to the classification described by Saleh et al. [27]: Type I femoral revision involves no significant bone loss; Type II represents contained cavitary bone loss with thinning of cortices; in Type III deficiency bone loss is segmental, involving the lesser trochanter and extending no more than 5 cm distal to it; Type IV segmental defects extend greater than 5 cm into the diaphysis and may not always allow distal fixation; and Type V defects represent a periprosthetic fracture with circumferential loss of bone stock proximal to the fracture. There were no Type I defects, 50 (69%) Type II, 14 (19%) Type III, three (4%) Type IV, and five (7%) Type V.
For surgical exposure, we performed an extended trochanteric osteotomy (ETO) in 50 (69%) cases and a modified trochanteric sliding osteotomy in 22 (31%). The old femoral component extracted during surgery was a cemented stem in 34 (47%) cases, a cementless stem in 35 (49%), and a cement spacer in three (4%). The spout body was used in 56 (78%) cases, the cone body in 13 (18%), and the calcar body in three (4%). We used 220-mm bowed stems in 22 (31%) cases, 170-mm bowed stems in 40 (56%), 170-mm straight stems in three (4%), and 115-mm straight stems in seven (10%). Strut allografts were used in 48 (67%) cases. The cup also was revised in 37 (51%) cases. The minimum followup was 60 months (mean, 85 months; range, 60–114 months). All patients were enrolled and provided consent to participate in the study before the operation.
Our surgical preoperative planning included radiographic assessment of femoral bone loss and old stem fixation. For distal fixation, at least 5 cm of diaphyseal tube was required. When such fixation was impossible, we used a proximal femoral allograft and prosthesis construct (PFA) [26]. In situ stem type and fixation dictated surgical exposure. For cemented stems and well-fixed cementless stems with extensive coating, we performed an ETO to aid in exposure and implant removal. The end of the osteotomy was extended to the level of the cement plug or the distal end of the porous coating. If that length of osteotomy precluded distal fixation with at least 5 cm of diaphyseal bone, we made it shorter and drilled through the more distal cement to extract it. For cementless stems that were loose or only proximally coated, a modified trochanteric slide osteotomy usually was chosen. Templating of the modular body was performed first. Three types of bodies are available. The spout body has a medial curve to provide fill to the proximal femur and is appropriate when proximal bone stock is only moderately compromised (Fig. 2). The cone body is conical and allows flexibility for version adjustments. The calcar body has a medial buildup to help resist subsidence and to physiologically load the proximal medial femur. Body type, size, height, and offset were determined and the location of the junction was marked on the radiograph. Different body heights allowed adjustment of leg length, and different body sizes allowed optimization of proximal fill. The stem was templated next. The stems are available in several lengths. The shortest stem that will allow at least 5 cm of distal fixation was chosen. Appropriate stem diameter was estimated. Erythrocyte sedimentation rate and C-reactive protein levels were obtained for all patients, and if suggestive of infection, we performed a preoperative hip aspiration
Fig. 2A–B.
(A) This 83-year-old man had a loose cemented stem with a Type II femoral defect. (B) Six years after revision with a 170-mm porous stem and a spout body, the stem is well fixed and the ETO has healed (arrow). A 5-cm diaphyseal tube distal to the ETO was available for distal stem fixation.
All patients were in the lateral decubitus position during the operation. We routinely used a modified trochanteric slide to improve surgical exposure in complex hip revisions, and if necessary, the slide was extended distally (ETO) to remove the femoral stem. Sequential flexible reamers for bowed stems and rigid reamers for straight stems were used to prepare the femoral canal. Proximal reaming to fit the body also was performed. We performed intraoperative radiographs with a trial component in place in all cases to rule out fractures and perforations and to confirm appropriate distal fixation. The modular stems were assembled on a back table and inserted in the correct version and depth as marked with the trial component. Assembly of the stem in situ after trialing the body with the stem already in place is also an option, but we did not do so. Cortical struts were used in situations of uncontained noncircumferential bone defects, for periprosthetic fractures, and for repair of ETOs.
Followups occurred at 6 weeks, 12 weeks, 6 months, and 1 year after the procedure and then annually. Clinical evaluation of each patient, as performed by the surgeon, included the HHS [11] preoperatively, at 6 weeks, 6 months postsurgery, and at annual followups. The HHSs were calculated by a research assistant (MM). We obtained routine standard hip radiographs (anteroposterior [AP] view of the pelvis and AP and lateral views of the affected hip) performed preoperatively, immediate postoperatively, at 6 weeks, 6 months, and annually thereafter. The immediate postoperative series of radiographs served as the baseline with which all subsequent radiographs were compared. When early subsidence was suspected, serial radiographs, 6 weeks apart, were performed until the stem stabilized or a decision was made to revise the stem. All radiographs were reviewed by one observer (DL) not involved in patient care. Subsidence was determined by measuring the distance between a fixed point on the stem (usually the body-stem junction) and a fixed point on the femur (the lesser trochanter if available). A difference of 5 mm or more in the measured distance between the immediate postoperative radiograph and the radiograph taken at last followup was considered as subsidence [4, 13].
We performed Kaplan-Meier survival analysis (MedCalc®, Version 9.2.0.1; MedCalc Software, Mariakerke, Belgium) to June 2009 with revision for any reason as end point. The 95% confidence interval (95% CI) was calculated. Continuous variables were compared using the t test for independent samples. Discrete variables were analyzed with the chi square test. Differences with p values less than 0.05 were considered significant.
Results
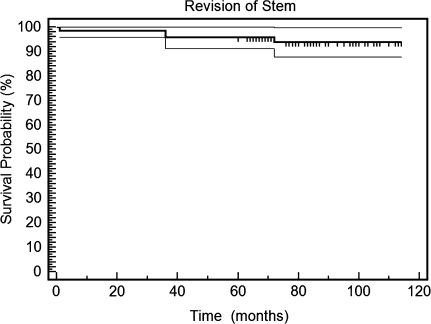
The Kaplan-Meier survival with femoral revision for any reason as an end point was 93.8% (95% CI, 90.8%–96.8%) (Fig. 3). Four stems (5.5%) were revised. Two cases (2.8%) needed revision for loosening. One of them had early failure at 1 month, clearly related to a very wide femoral canal, for which the 19.5-mm diameter stem used was too narrow. One other patient had progressive, asymptomatic slow subsidence of a 15-mm stem and had revision surgery 3 years postoperatively after pain and increasing leg length discrepancy developed. Both loose stems were revised to a PFA. One patient had fracture of the stem at the modular junction 6 years after the operation. The fractured stem was revised to a PFA. One stem was revised owing to infection. Other reoperations included five cup revisions, one washout for infection, and open reduction and internal fixation with plates and strut grafts for two periprosthetic fractures.
Fig. 3.
A Kaplan-Meier survival analysis is shown. The thin lines represent the 95% CI for the survival rate. The survival rate at 10 years was 93.8% (95% CI, 90.8%–96.8%).
The mean HHS for the entire group improved from 39 points (range, 9–84 points) before the operation to 72 points (range, 32–93 points) at last followup. Three patients (4.2%) had dislocations: two (2.8%) were reduced closed and never dislocated again, but one patient (1.4%) required cup revision. Two patients (2.8%) had deep infections: one (1.4%) was treated successfully with a washout and one (1.4%) required a two-stage revision, in which another ZMR® stem was used. One patient (1.4%) had an intraoperative perforation of the anterior cortex and one patient (1.4%) had intraoperative fracture starting at the tip of the ETO. Both were diagnosed intraoperatively; treatment consisted of conversion to a longer stem and application of a strut graft. One stem (1.4%) was fractured in the body-stem junction 6 years postoperatively and was revised.
Subsidence occurred in eight (11%) patients, in the range of 5 to 25 mm. The overall subsidence (mean ± standard deviation) for the study series was 1.6 ± 5.0 mm. Two patients were symptomatic and had revision surgery. The six other patients who had radiographic evidence of subsidence were followed and stabilized sometime during the first postoperative year. Only two of them complained of pain, which resolved with stabilization of the stem.
Discussion
Femoral reconstruction in revision THA may present the surgeon with various challenges, including obtaining primary and durable fixation of the implant. The ZMR® porous stem is a versatile modular system that allows distal or extensive (proximal and distal) fixation and versatile proximal reconstruction. The objective of this study was to evaluate its clinical and radiographic outcomes at midterm followup.
Our study has certain limitations. We prospectively collected all data, but the study was not randomized and we had no control group for which we used a different component or different surgical technique to compare and contrast outcomes.
Results of cemented femoral components in revision THA have been suboptimal, with failure rates of 17% to 60% at 2 to 8 years of followup [12, 21, 23]. Alternate solutions for revision of the bone-deficient femur, including impaction grafting, megaprosthesis, and PFA, are technically demanding and have had high complication rates [17, 18, 26]. Cementless revision stems thus have become an appealing option. Several different concepts of cementless revision stems have been introduced and used successfully during the last 2.5 decades (Table 1). Modular primary fixation stems, such as the S-ROM® system (Depuy Orthopaedics, Inc, Warsaw IN), rely on proximal support by a modular porous-coated sleeve, whereas the distal part of the stem is uncoated. It provides distal stability but not distal fixation [5, 20]. These stems are less suitable when proximal bone loss is severe. In addition, they compromise the use of ETO. Distal fixation stems have several advantages. They are versatile and can be used in different clinical situations, including various severities of bone loss and periprosthetic fractures. They are also compatible with ETO. Common distal fixation stem designs include porous-coated cylindrical stems and tapered stems. Tapered stems are designed according to the principles of the Wagner SL stem (Sulzer Orthopedics Ltd, Baar, Switzerland), with conical geometry for distal axial stability and three-point fixation and longitudinal splines for rotational stability [10, 30]. The principle of the use of cylindrical, extensively porous-coated stems is to bypass the bone deficiency and rely on distal bone for fixation [19], but when used with porous proximal bodies, they can provide extensive fixation capabilities. Potential problems related to distal fixation stems are thigh pain and stress shielding [8]. Modularity offers the potential advantage of adjustment and restoration of leg length, offset, version, and proximal fill, although these advantages have not been clearly shown in comparative studies [1, 6]. Disadvantages of stem modularity include the risk of stem fractures, fretting, and higher cost [1, 6, 22]. Survival of various distal fixation stems at 5 to 10 years is consistently approximately 95%, with no clear superiority of any specific design (Table 1). Earlier experience with the ZMR® system was encouraging. Sporer and Paprosky [29] reported the short-term outcome of 11 ZMR® taper stems used for severe segmental bone defects, with only one failure related to infection. Kang et al. [13] reported 2 to 5 years’ followup of 39 ZMR® stems, mostly porous, with only one revision related to subsidence and instability. Our series had a 93.8% survival rate of the ZMR® porous stem at 10 years. Mechanical failures were related to stem undersizing. We had one case of stem fracture at the modular junction. Prevention of this is achieved by getting proximal fixation or the use of the more recently introduced extra large stems. We now routinely use these extra large junction stems for high-demand patients and larger patients or when only distal fixation is possible.
Table 1.
Results from published series of cementless femoral revision
| Study | Year | Stem* | Number of revisions | Followup (years)† | Survival | Functional outcome score‡ |
|---|---|---|---|---|---|---|
| Böhm and Bischel [3] | 2004 | Wagner SL tapered, nonmodular | 129 | 8.1 (5.1–14.1) | 95.2% | Merle d’Aubigné 7.7 → 14.4 |
| Cameron [5] | 2002 | S-ROM modular, proximal ingrowth | 211 | 6.5 (2–12) | 1.4% revision | |
| Engh et al. [8] | 2004 | Cylindrical porous coated, distal fixation | 777 | 5 years: 97.7% | ||
| 10 years: 93.8% | ||||||
| 15 years: 92.7% | ||||||
| Kang et al. [13] | 2008 | ZMR (mostly porous) | 39 | (2–5) | HHS 47 → 72 | |
| Krishnamurthy et al. [15] | 1997 | AML extensive porous coated, distal fixation, nonmodular | 297 | 8.3 (5–13) | 2.4% mechanical failure rate | Merle d’Aubigné 4.8 → 10.2 |
| Kwong et al. [16] | 2003 | Link MP modular, tapered-fluted, distal fixation | 143 | 3.5 (2–6) | 97.2% | HHS → 92 |
| Moreland and Moreno [21] | 2001 | Extensively porous coated, nonmodular | 137 | 9.3 (5–16) | 7% revision for any reason | Merle d’Aubigné 5.8 → 9.4 |
| Paprosky et al. [24] | 1999 | AML extensively porous coated, nonmodular | 170 | 13.2 (10–16) | 95% | Merle d’Aubigné 5.4 → 10.8 |
| Current study | 2009 | ZMR porous | 72 | 7 (5–10) | 93.1% | HHS 39 → 72 |
* Stems include Wagner SL (Sulzer Orthopedics Ltd, Baar, Switzerland), S-ROM® (Depuy Orthopaedics, Inc, Warsaw IN), ZMR® (Zimmer, Inc, Warsaw IN), AML® (Depuy), LINK® MP™ (Wright Medical Technology, Inc, Arlington, TN); †values expressed as means, with ranges in parentheses; ‡functional outcome score expressed as preoperative score → followup score; HHS = Harris hip score.
Subsidence of distal fixation stems is a well-recognized phenomenon, with less than certain clinical significance. Cylindrical porous-coated stem subsidence was correlated to low stem-canal ratio [13, 24]. Paprosky et al. [24] reported 16% subsidence of nonmodular porous-coated implants, with stabilization of most during the first 2 postoperative years. Unstable subsided stems were revised to larger-diameter stems. Wagner tapered nonmodular stems were reported to subside more than 5 mm in as many as 48% to 54% of patients, with most stems stabilizing after 3 to 13 months [2, 10]. Subsidence was correlated to stem undersizing, osteoporosis, deficient metaphyseal support, and the use of the transfemoral approach. As in these reports, most subsided stems in our series were asymptomatic and stabilized within the first year. Our results and those of others [10, 13, 24] suggest inappropriate selection of stem diameter and undersizing may be responsible for many cases of progressive subsidence. The thickest-diameter ZMR® porous stems available are 25.5 mm. In patients with very wide femoral canals, other techniques should be considered. Our practice is to be prepared for a proximal femoral allograft in these cases [26]. Another option is the use of impaction grafting [17]. As with other aspects of arthroplasty, careful preoperative planning is crucial here. We also recommend routine intraoperative radiographs.
The ZMR® porous stem is a versatile system that offers an off-the-shelf solution for various femoral problems, including aseptic loosening, infections, periprosthetic fractures, and instability, in a simple, uniform, and reproducible technique, as long as a 5-cm diaphyseal tubular segmental support can be provided. When such support cannot be anticipated owing to very distal bone deficiency, usually in the setting of the multiply revised hip, or when the femoral canal is exceptionally wide, a proximal femoral allograft should be available.
Acknowledgments
We thank Matthew MacDonald for help in data collection and calculation of hip scores and David Razao for help in data collection.
Footnotes
One of the authors (AEG) serves as a consultant for Zimmer, Inc, Warsaw, IN.
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Barrack RL. Orthopaedic crossfire: stem modularity is unnecessary in revision total hip arthroplasty: in the affirmative. J Arthroplasty. 2003;18(3 suppl 1):98–100. doi: 10.1054/arth.2003.50075. [DOI] [PubMed] [Google Scholar]
- 2.Böhm P, Bischel O. Femoral revision with the Wagner SL revision stem: evaluation of one hundred and twenty-nine revisions followed for a mean of 4.8 years. J Bone Joint Surg Am. 2001;83:1023–1031. doi: 10.1302/0301-620X.83B7.11413. [DOI] [PubMed] [Google Scholar]
- 3.Böhm P, Bischel O. The use of tapered stems for femoral revision surgery. Clin Orthop Relat Res. 2004;420:148–159. doi: 10.1097/00003086-200403000-00021. [DOI] [PubMed] [Google Scholar]
- 4.Callaghan JJ, Salvati EA, Pellicci PM, Wilson PD, Jr, Ranawat CS. Results of revision for mechanical failure after cemented total hip replacement, 1979 to 1982: a two to five-year follow-up. J Bone Joint Surg Am. 1985;67:1074–1085. [PubMed] [Google Scholar]
- 5.Cameron HU. The long-term success of modular proximal fixation stems in revision total hip arthroplasty. J Arthroplasty. 2002;17(4 suppl 1):138–141. doi: 10.1054/arth.2002.32462. [DOI] [PubMed] [Google Scholar]
- 6.Cameron HU. Orthopaedic crossfire: stem modularity is unnecessary in revision total hip arthroplasty: in opposition. J Arthroplasty. 2003;18(3 suppl 1):101–103. doi: 10.1054/arth.2003.50076. [DOI] [PubMed] [Google Scholar]
- 7.Dalury DF, Gonzales RA, Adams MJ. Minimum 5-year results in 96 consecutive hips treated with a tapered titanium stem system. J Arthroplasty. 2008 Dec 3. [Epub ahead of print]. [DOI] [PubMed]
- 8.Engh CA, Jr, Hopper RH, Jr, Engh CA., Sr Distal ingrowth components. Clin Orthop Relat Res. 2004;420:135–141. doi: 10.1097/00003086-200403000-00019. [DOI] [PubMed] [Google Scholar]
- 9.Garbuz DS, Toms A, Masri BA, Duncan CP. Improved outcome in femoral revision arthroplasty with tapered fluted modular titanium stems. Clin Orthop Relat Res. 2006;453:199–202. doi: 10.1097/01.blo.0000238875.86519.cf. [DOI] [PubMed] [Google Scholar]
- 10.Grünig R, Morscher E, Ochsner PE. Three- to 7-year results with the uncemented SL femoral revision prosthesis. Arch Orthop Trauma Surg. 1997;116:187–197. doi: 10.1007/BF00393708. [DOI] [PubMed] [Google Scholar]
- 11.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–755. [PubMed] [Google Scholar]
- 12.Hungerford DS, Jones LC. The rationale of cementless revision of cemented arthroplasty failures. Clin Orthop Relat Res. 1988;235:12–24. [PubMed] [Google Scholar]
- 13.Kang MN, Huddleston JI, Hwang K, Imrie S, Goodman SB. Early outcome of a modular femoral component in revision total hip arthroplasty. J Arthroplasty. 2008;23:220–225. doi: 10.1016/j.arth.2007.03.006. [DOI] [PubMed] [Google Scholar]
- 14.Köster G, Walde TA, Willert HG. Five- to 10-year results using a noncemented modular revision stem without bone grafting. J Arthroplasty. 2008;23:964–970. doi: 10.1016/j.arth.2007.08.024. [DOI] [PubMed] [Google Scholar]
- 15.Krishnamurthy AB, MacDonald SJ, Paprosky WG. 5- to 13-year follow-up study on cementless femoral components in revision surgery. J Arthroplasty. 1997;12:839–847. doi: 10.1016/S0883-5403(97)90152-2. [DOI] [PubMed] [Google Scholar]
- 16.Kwong LM, Miller AJ, Lubinus P. A modular distal fixation option for proximal bone loss in revision total hip arthroplasty: a 2- to 6-year follow-up study. J Arthroplasty. 2003;18(3 suppl 1):94–97. doi: 10.1054/arth.2003.50083. [DOI] [PubMed] [Google Scholar]
- 17.Leopold SS, Rosenberg AG. Current status of impaction allografting for revision of a femoral component. Instr Course Lect. 2000;49:111–118. [PubMed] [Google Scholar]
- 18.Malkani AL, Settecerri JJ, Sim FH, Chao EY, Wallrichs SL. Long-term results of proximal femoral replacement for non-neoplastic disorders. J Bone Joint Surg Br. 1995;77:351–356. [PubMed] [Google Scholar]
- 19.McAuley JP, Engh CA., Jr Femoral fixation in the face of considerable bone loss: cylindrical and extensively coated femoral components. Clin Orthop Relat Res. 2004;429:215–221. doi: 10.1097/01.blo.0000150274.21573.f4. [DOI] [PubMed] [Google Scholar]
- 20.McCarthy JC, Lee JA. Complex revision total hip arthroplasty with modular stems at a mean of 14 years. Clin Orthop Relat Res. 2007;465:166–169. doi: 10.1097/BLO.0b013e318159cb97. [DOI] [PubMed] [Google Scholar]
- 21.Moreland JR, Moreno MA. Cementless femoral revision arthroplasty of the hip: minimum 5 years followup. Clin Orthop Relat Res. 2001;393:194–201. doi: 10.1097/00003086-200112000-00022. [DOI] [PubMed] [Google Scholar]
- 22.Mroczkowski ML, Hertzler JS, Humphrey SM, Johnson T, Blanchard CR. Effect of impact assembly on the fretting corrosion of modular hip tapers. J Orthop Res. 2006;24:271–279. doi: 10.1002/jor.20048. [DOI] [PubMed] [Google Scholar]
- 23.Mulroy WF, Harris WH. Revision total hip arthroplasty with use of so-called second-generation cementing techniques for aseptic loosening of the femoral component: a fifteen-year-average follow-up study. J Bone Joint Surg Am. 1996;78:325–330. doi: 10.2106/00004623-199603000-00002. [DOI] [PubMed] [Google Scholar]
- 24.Paprosky WG, Greidanus NV, Antoniou J. Minimum 10-year-results of extensively porous-coated stems in revision hip arthroplasty. Clin Orthop Relat Res. 1999;369:230–242. doi: 10.1097/00003086-199912000-00024. [DOI] [PubMed] [Google Scholar]
- 25.Rodriguez JA, Fada R, Murphy SB, Rasquinha VJ, Ranawat CS. Two-year to five-year follow-up of femoral defects in femoral revision treated with the Link MP modular stem. J Arthroplasty. 2008 Oct 31. [Epub ahead of print]. [DOI] [PubMed]
- 26.Safir O, Kellett CF, Flint M, Backstein D, Gross AE. Revision of the deficient proximal femur with a proximal femoral allograft. Clin Orthop Relat Res. 2009;467:206–212. doi: 10.1007/s11999-008-0573-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Saleh KJ, Holtzman J, Gafni A, Saleh L, Davis A, Resig S, Gross AE. Reliability and intraoperative validity of preoperative assessment of standardized plain radiographs in predicting bone loss at revision hip surgery. J Bone Joint Surg Am. 2001;83:1040–1046. doi: 10.2106/00004623-200107000-00009. [DOI] [PubMed] [Google Scholar]
- 28.Sporer SM, Paprosky WG. Revision total hip arthroplasty: the limits of fully coated stems. Clin Orthop Relat Res. 2003;417:203–209. doi: 10.1097/01.blo.0000096803.78689.0c. [DOI] [PubMed] [Google Scholar]
- 29.Sporer SM, Paprosky WG. Femoral fixation in the face of considerable bone loss: the use of modular stems. Clin Orthop Relat Res. 2004;429:227–231. doi: 10.1097/01.blo.0000150120.80409.0d. [DOI] [PubMed] [Google Scholar]
- 30.Wagner H, Wagner M. Cone prosthesis for the hip joint. Arch Orthop Trauma Surg. 2000;120:88–95. doi: 10.1007/pl00021223. [DOI] [PubMed] [Google Scholar]