Abstract
Background
The accuracy of computer navigation applied to total knee arthroplasty (TKA) in knees with severe deformity has not been studied.
Questions/purposes
The purpose of this study was to compare the radiographic alignment achieved in total knee replacements performed with and without navigation and to search for differences in the final alignment of two groups of patients (with and without previous joint deformities) using the same system of surgical navigation.
Methods
The first series comprised 40 arthroplasties with minimal preoperative deformity. In 20 of them, surgical navigation was used, whereas the other 20 were performed with conventional jig-based technique. We compared the femoral angle, tibial angle, and femorotibial angle (FTA) by performing a post-TKA CT of the entire limb. In the second series, 40 additional TKAs were studied; in this case, however, they presented preoperative deformities greater than 10º in the frontal plane.
Results
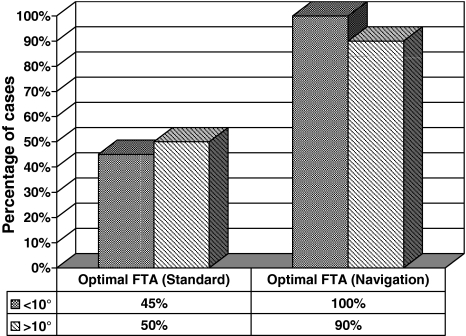
The positioning of the femoral and tibial component was more accurate in the group treated with surgical navigation and FTA improvement was statistically significant. When comparing the results of both series, FTA precision was always higher when using computer-assisted surgery. As for optimal FTA, data showed the use of surgical navigation improved the results both in the group with preoperative deformity greater than 10° in the frontal plane and in the group with minimal preoperative knee deformity.
Conclusions
Surgical navigation obtains better radiographic results in the positioning of the femoral and tibial components and in the final axis of the limb in arthroplasties performed on both deformed and more normally aligned knees.
Level of Evidence
Level II, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
The goals of TKA are to alleviate pain and correct deformity while increasing functionality. To accomplish that, it is considered necessary to stabilize the prosthetic joint both in flexion and extension, to restore the level of the articular line to its original site, to realign the axes, and to restore the ligamentous balance.
As many authors proved long ago [2], the factor that exerts the greatest influence on TKA survival and durability is prosthetic alignment, because interline obliquity and malalignment are frequently associated with earlier failure and poor functional results. Despite the use of new tools and equipment, the following facts have been observed: 10% of tibial cuts are performed with an error value over 4°, deviations in the final TKA alignment are commonplace, even when carried out by seasoned surgeons, and only in 75% of the cases is optimal femorotibial alignment achieved [12]. TKA performed in the standard manner is prone to errors [14], cannot be individually customized, is not based on the mechanical axis, and is not reproducible. In response, there has been a search for alternative techniques that may remedy these hindrances. Computer assistance to TKA is being explored as one such remedy.
A wide range of literature on the usefulness of surgical navigation for TKA already exists, and there are also numerous comparative studies on the radiographic results obtained with and without navigation. However, no publications report these results when surgical navigation is applied to knees featuring preoperative joint deformities. Preoperative deformity poses an additional challenge to the process of achieving exact alignment with TKA. Bone loss and ligamentous injuries make it difficult to achieve stability and proper ligamentous balance using conventional jigs and technique. The most frequent deformities appear in the frontal plane, known as genu varum or valgum deformities. They present the worst evolution and the lowest TKA survival rate in this group of patients [15].
The aims of the present work are to compare the coronal plane radiographic alignment achieved with and without navigation in patients with minimal preoperative joint deformities as well as to those achieved in patients with severe preoperative joint deformities. Finally, we asked if there are any differences of the alignment achieved between these two groups of patients when the same surgical navigation system is used.
Patients and Methods
In this prospective case series, two study groups were assessed. The first study population represents patients without preoperative deformity. The radiographic alignment after implanting a TKA with and without the help of surgical navigation was compared. This very same procedure was followed in the second study population, which represents patients with a preoperative joint deformity greater than 10° in the coronal plane (varus-valgus).
For the first series, 40 TKAs of the same model were implanted by the same surgical team. Patients were chosen from the surgery waiting lists and were randomly (closed envelope) assigned to one of two groups immediately preoperatively. In 20 knees, TKAs were implanted using the conventional procedure and standard equipment, whereas for the other 20, the implant was carried out with the help of a wireless nonimage-based navigation-assisted system (Stryker-Leibinger, Freiburg, Germany). Surgeons had experience with this type of technique (more than 50 cases at the start of the study), so the learning curve was considered to be over. Inclusion criteria for the first study included patients undergoing primary TKA for osteoarthritis rated as Ahlbäck’s Grade III or IV [1] with no varus or valgus deformities greater than 10º. Both groups were similar in terms of age, gender, and body mass index. Both the surgical technique (excluding the use of navigation) and the postoperative guidelines were similar. Patients were assigned to either group randomly, the surgeon not knowing which technique was to be assigned to each patient up to the very moment the operation started.
For the group who underwent the standard procedure, intramedullary femoral and extramedullary tibial alignment guiding rods were used. The attachment of the femoral component was systematically performed with 3º of external rotation, and all the femoral, tibial, and patellar cuts were performed following the technical recommendations provided by the implant designers.
The second study was carried out by the same team of surgeons. Patients included in this series showed deformities greater than 10º in the coronal plane. Another 40 TKAs were randomly assigned to both groups. In one of the 20 patient groups, surgical navigation was used following the system already described, whereas in the other group, the standard procedure using mechanical guiding rods was used. Case selection, surgical techniques, and inclusion criteria (except for the presence of deformity) were similar to those in the first study. In both the surgical mechanical group and the surgical navigation group, the bone cuts to achieve correct alignment and soft tissue release for the correction of the initial deformity were performed. CT scans were performed preoperatively and postoperatively in all the patients in both series. Images of the frontal plane of the entire limb, including the femoral head and the ankle, were obtained. A restraint system was used for the lower limb to keep it in neutral rotation. For each case, three angles were measured: femoral angle (FA), which is formed perpendicular between the femoral component axis and the mechanical axis of the femur; tibial angle (TA), formed perpendicular between the axis of the tibial platform and the tibial axis; and femorotibial angle (FTA), formed by the union of the mechanical axes of the femur and tibia. FA and TA reveal the quality of the component positioning, which, theoretically, should form a 90º angle with the mechanical axis of the bone segment. FTA is the final index for the placement of the arthroplasty and should be as close to 180º as possible. To facilitate the gathering and statistical analysis of the data, varus angulation was considered as negative and valgus angulation as positive (this way, angulation data appeared in the information provided by the navigation system).
Data were stored in an Access database and analyzed statistically with the SPSS software (SPSS Inc, Chicago, IL). A descriptive study of all the variables was carried out. The hypotheses put forward in the study were tested according to the distribution of variables through parametric tests. To compare the means of angulations among the studied groups, Student’s t test was used. To compare the percentage of optimal results among the examined groups, we used the chi square test.
Results
In the first series (without deformity), mean operation time for the standard technique group was 73 minutes (range, 62–89 minutes), whereas for the navigation group, it was 91 minutes (range, 83–101 minutes). There were no lost cases and no patient had any intraoperative complications. In the series of knees with major preoperative deformity, the 40 TKAs completed the study and there were also no lost cases or intraoperative complications. Mean operation time for the standard technique group was 77 minutes (range, 57–88 minutes), whereas for the navigation group, it was 83 minutes (range, 76–109 minutes). No technique-related complications were observed.
In the group of patients with minimal preoperative deformity the navigated patients had more ideally positioned implants than the nonnavigated as indicated by the FA (p = 0.001) and for the FTA (p < 0.001).Average postoperative FA for the knees with minimal preoperative deformity radiographic alignment was 91º (SD, 1.52) (Table 1). However, for the TA, the groups were similar and the navigated group did not have more ideal alignment. All cases included in the surgical navigation group showed a so-called “ideal” FTA (180° ± 3°), whereas only nine cases from the group that underwent conventional surgery presented such results (p < 0.0001).
Table 1.
Femoral angle (FA), tibial angle (TA), and femorotibial angle (FTA) in both groups
| Group | Technique | FA range (mean) | TA range (mean) | FTA range (mean) |
|---|---|---|---|---|
| No preoperative deformity | Standard | 90º–94º (91.7º) | 87º–95º (90.2º) | 172º–180º (175.9º) |
| Navigation | 87º–93º (90.2º) | 85º–93º (89.6º) | 177º–182º (179.2º) | |
| p value | 0.001 | NS | < 0.001 | |
| Preoperative deformity | Standard | 88–95º (91.9º) | 86–95º (90.4º) | 173–181º (177.1º) |
| Navigation | 87–93º (90.3º) | 85–93º (89.9º) | 177–183º (179.8º) | |
| p value | NS | NS | 0.005 |
NS = not significant.
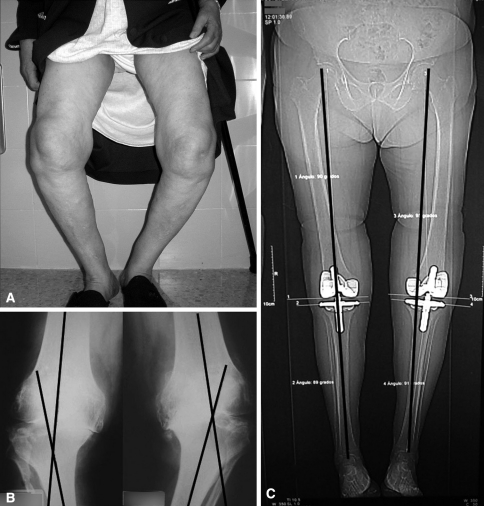
In the series with substantial preoperative deformity, the position of the femoral and tibial components was not more ideal in the group treated with surgical navigation (Table 1). However, the FTA was closer to the ideal in the navigated group (p = 0.005). In 90% of the cases in the surgical navigation group, the resulting FTA obtained after arthroplasty was within the recommended values (180° ± 3°), whereas such favorable results only were achieved in 50% of the patients who underwent conventional surgery (p = 0.007). Two patients exhibited bilateral deformities and received bilateral TKA; in one of the patients (Fig. 1), one arthroplasty was implanted with the help of surgical navigation, whereas the other was not. No differences were observed in clinical outcomes.
Fig. 1A–C.
(A) This photograph shows a patient with severe, bilateral genu varus deformity. (B) The preoperative radiographs for this patient are shown. (C) TKA was performed with navigation for the right knee and without it for the left knee.
When comparing the FA between two groups, we observed that only in the group without deformity was the adjustment to optimal values (90°) better when the navigation procedure was applied. Better results were achieved in FTA for both groups whenever surgical navigation was used. After studying the optimal FTA, we observed that the use of surgical navigation improved the results both in the group with previous deformities and in the group with no previous knee deformities (Fig. 2).
Fig. 2.
This graph depicts the number of cases with optimal results for femorotibial angle (FTA) in both standard and navigated techniques.
Discussion
The principal aim of this work was to study the advantages of the use of navigation in knees with articular deformities. Implanting a TKA to treat arthrosis coupled with deformity poses a challenge for the surgeon, because it is very complex to achieve exact alignment when performing surgery on highly altered structures.
Navigation may improve component placement in TKA and, more importantly, it can better reproduce the axis of the limb than when using the standard surgical approach. In our series, the optimal angulation of the femoral and tibial components in the frontal plane was achieved with more precision when using navigation, although results were more obvious in the case of the FTA, in which differences with the standard group were statistically significant. It may be possible that discrepancies of less than 1º in FA, TA, and FTA have little practical value, but the trends of our data suggest navigation in TKA results in higher precision. Other studies similar to ours have also demonstrated navigation allows for better alignment in TKA. Outliers are reduced both in number and severity with navigation, and the additional time required to navigate diminishes with experience [6, 7].
Our work has some limitations. Implant alignment is just one part of the surgical procedure, and the assessment of a TKA outcome should be based especially on the level of pain relief and knee functionality in the long term; such factors have not been studied in the present work. Other additional major limitations to this study would be that alignment measurements are obtained on limbs that are nonweightbearing, and the study only deals with deformities in the coronal plane without having considered the sagittal or transverse plane.
Despite the advantages surgical navigation has to offer to TKA in knee deformities, there are no published works such as ours on the outcomes achieved with this technique in an individualized set of knees exhibiting previous joint deformities. Studies do exist on its usefulness in extraarticular deformities [5, 11], but it is surprising how scarce these investigations are, especially when taking into account surgical navigation may be a reasonably helpful procedure to enhance arthroplasty placement in such complex scenarios.
Theoretically, it could be assumed that better control can be achieved in correction of deformity assisted by navigation, because the computer can demonstrate the results of the soft tissue releases in real time.
Complications in surgical navigation are related to technical mistakes or to problems with the anchoring of the trackers [8, 9]. Some authors mention the low reproducibility of the measurements obtained with navigation, especially on the transepicondylar axis [18], whereas others demonstrate a TKA performed with the help of computer-assisted surgical navigation did not result in more accurate implant positioning than that achieved in conventional TKA [10]. However, even those works admit the intraoperative feedback with regard to resection, implant, and limb alignment provided by computer-assisted surgery offers surgeons an opportunity to improve their judgment with regard to the accuracy with which they perform and evaluate each step of the TKA procedure [16] and that navigation can generate precise, accurate, and reproducible alignment measurements. This technology can function as an effective tool for assessing pre- and postoperative limb alignment and for relating intraoperative alignment measurements to clinical and functional outcomes [17]. Recent meta-analyses [3, 13] of alignment outcomes for navigation versus conventional TKA show major improvements in component orientation and mechanical axis when computer assistance is used. Unfortunately, to date, no studies have demonstrated that the improved alignment achieved with navigation results in better clinical outcomes [4]. This important question will hopefully be addressed by larger scale future studies.
Perhaps the best use for surgical navigation in TKA would be in complex knee scenarios when deformities are present or when mechanical alignment cannot be used. If we admit computer science has improved and will further improve countless fields within our scientific, social, and even domestic purview, it is difficult to remain blind to the advantages it could bring to surgical procedures.
Acknowledgments
We thank J. M. Fernandez-Carreira, MD, for statistical analysis.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This study belongs to a project promoted by the Health Research Institute (Carlos III Health Institute) of the Spanish National Healthcare System.
References
- 1.Ahlback S. Osteoarthrosis of the knee. A radiographic investigation. Acta Radiol Diagn. 1968;Suppl 277:7–72. [PubMed]
- 2.Bargren JH, Blaha JD, Freeman MA. Alignment in total knee arthroplasty. Correlated biomechanical and clinical observations. Clin Orthop Relat Res. 1983;173:178–183. [PubMed] [Google Scholar]
- 3.Bäthis H, Shafizadeh S, Paffrath T, Simanski C, Grifka J, Lüring C. Are computer assisted total knee replacements more accurately placed? A meta-analysis of comparative studies. Orthopäde. 2006;35:1056–1065. doi: 10.1007/s00132-006-1001-3. [DOI] [PubMed] [Google Scholar]
- 4.Bauwens K, Wich M, Ekkernkamp A, Stengel D, Matthes G, Gebhard F, Hanson B. Navigated total knee replacement. A meta-analysis. J Bone Joint Surg Am. 2007;89:261–269. doi: 10.2106/JBJS.F.00601. [DOI] [PubMed] [Google Scholar]
- 5.Bottros J, Klika AK, Lee HH, Polousky J, Barsoum WK. The use of navigation in total knee arthroplasty for patients with extra-articular deformity. J Arthroplasty. 2008;23:74–78. doi: 10.1016/j.arth.2007.01.021. [DOI] [PubMed] [Google Scholar]
- 6.Carter RE, III, Rush PF, Smid JA, Smith WL. Experience with computer-assisted navigation for total knee arthroplasty in a community setting. J Arthroplasty. 2008;23:707–713. doi: 10.1016/j.arth.2007.07.013. [DOI] [PubMed] [Google Scholar]
- 7.Haaker RG, Stockheim M, Kamp M, Breitenfelder J, Ottersbach A. computer-assisted navigation increases precision of component placement in total knee arthroplasty. Clin Orthop Relat Res. 2005;433:152–159. doi: 10.1097/01.blo.0000150564.31880.c4. [DOI] [PubMed] [Google Scholar]
- 8.Hernandez-Vaquero D, Suarez-Vazquez A. Complications of fixed infrared emitters in computer-assisted total knee arthroplasties. BMC Musculoskelet Disord. 2007;8:71–73. doi: 10.1186/1471-2474-8-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jung HJ, Jung YB, Song KS, Park SJ, Lee JS. Fractures associated with computer-navigated total knee arthroplasty. A report of two cases. J Bone Joint Surg Am. 2007;89:2280–2284. doi: 10.2106/JBJS.F.01166. [DOI] [PubMed] [Google Scholar]
- 10.Kim YH, Kim JS, Choi Y, Kwon OR. Computer-assisted surgical navigation does not improve the alignment and orientation of the components in total knee arthroplasty. J Bone Joint Surg Am. 2009;91:14–19. doi: 10.2106/JBJS.G.01700. [DOI] [PubMed] [Google Scholar]
- 11.Klein GR, Austin MS, Smith EB, Hozack WJ. Total knee arthroplasty using computer-assisted navigation in patients with deformities of the femur and tibia. J Arthroplasty. 2006;21:284–288. doi: 10.1016/j.arth.2005.07.013. [DOI] [PubMed] [Google Scholar]
- 12.Mahaluxmivala J, Bankes MJK, Nicolai P, Aldam CH, Allen W. The effect of surgeon experience on component positioning in 673 press fit condylar posterior cruciate-sacrificing total knee arthroplasties. J Arthroplasty. 2001;16:635–640. doi: 10.1054/arth.2001.23569. [DOI] [PubMed] [Google Scholar]
- 13.Mason JB, Fehring TK, Estok R, Banel D, Fahrbach K. Meta-analysis of alignment outcomes in computer-assisted total knee arthroplasty surgery. J Arthroplasty. 2007;22:1097–1106. doi: 10.1016/j.arth.2007.08.001. [DOI] [PubMed] [Google Scholar]
- 14.Mihalko WM, Boyle J, Clark LD, Krackow KA. The variability of intramedullary alignment of the femoral component during total knee arthroplasty. J Arthroplasty. 2005;20:25–28. doi: 10.1016/j.arth.2004.10.011. [DOI] [PubMed] [Google Scholar]
- 15.Ritter MA, Faris PM, Keating EM, Meding JB. Postoperative alignment of total knee replacement. Its effect on survival. Clin Orthop Relat Res. 1994;299:153–156. [PubMed] [Google Scholar]
- 16.Stulberg SD, Yaffe MA, Koo SS. Computer-assisted surgery versus manual total knee arthroplasty: a case-controlled study. J Bone Joint Surg Am. 2006;88:47–54. doi: 10.2106/JBJS.F.00698. [DOI] [PubMed] [Google Scholar]
- 17.Yaffe MA, Koo SS, Stulberg SD. Radiographic and navigation measurements of TKA limb alignment do not correlate. Clin Orthop Relat Res. 2008;466:2736–2744. doi: 10.1007/s11999-008-0427-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yau WP, Leung A, Chiu KY, Tang WM, Ng TP. Intraobserver errors in obtaining visually selected anatomic landmarks during registration process in nonimage-based navigation-assisted total knee arthroplasty. A cadaveric experiment. J Arthroplasty. 2005;20:591–596. doi: 10.1016/j.arth.2005.02.011. [DOI] [PubMed] [Google Scholar]