Abstract
Background
Sexual behaviours among HIV-positive male patients in Cambodia have not been fully evaluated.
Objectives
The patterns of sexual behaviours and social factors were compared between married and single men.
Methods
A retrospective cross-sectional survey of 174 male HIV patients was undertaken during March 1999–June 2000 in Phnom Penh.
Results
Many participants (61%) reported that they were unaware that their sexual behaviours may have put them at risk of HIV infection. Sexual behaviours included having sex with a sex worker (90%), multiple sexual partners (41%), and both of these behaviours (37%). Two-thirds (69%) reported using a condom when having sex with a sex worker. Condom use with multiple sexual partners was low (24%). A history of condom use with a sex worker was less likely to be reported among married men than single men (P = 0.008). Always using condoms with a sex worker did not differ between married men and single men. Social factors that influenced visiting a sex worker included invitation by a friend (88%), alcohol consumption (74%), and having extra spending money (72%). Multivariate analysis suggests that alcohol consumption (P = 0.008) and having extra spending money (P = 0.02) were strongly associated with visiting a sex worker.
Conclusions
In Cambodia, HIV-infected men frequently reported a history of using sex workers. Having multiple sex partners or using a sex worker and multiple sexual partners were not rare. Interventions should target men in settings where alcohol is consumed and to encourage married men to use condoms.
Keywords: HIV, men, social factors
Introduction
A civil war lasting for over 30 years, and the genocide of the Khmer Rouge in Cambodia (1975–1979) ruined the country's social structure and healthcare system, resulting in increased poverty. This created an environment for the easy spread of HIV. After the first case of HIV infection was diagnosed in 1991 among blood donors, HIV in Cambodia spread rapidly to the general population.1 Cambodia experienced the peak of HIV prevalence at 3% in 1997, and the prevalence among adults aged 15–49 years old remains the highest in Asia.2,3
HIV in Cambodia is primarily transmitted through heterosexual contact.4,5 Clients of sex workers have been a major bridge for HIV transmission and spread.6 The patterns of infection suggest that the HIV epidemic has now diffused from commercial sex workers through their clients to all segments of Cambodian society.
Socioeconomic and demographic factors and sexual behaviour patterns prevalent among the male clients of Cambodian sex workers before becoming HIV-infected have not been fully evaluated. The present study was designed to compare differences between married and single male patients before their diagnosis of HIV infection in a Cambodian hospital. The results of this survey were intended to lead to the development, implementation, and monitoring of culturally-appropriate and effective HIV prevention strategies and educational materials for Cambodian men.
Methods
Study design
One hundred and ninety-one HIV-infected male patients were interviewed face-to-face, between March 1999 and June 2000, in Khmer by a specially trained study physician at the Sihanouk Hospital Center of HOPE (SHCH). Seventeen (9%) male patients were identified as being either divorced (n = 11) or widowed (n = 6), and were excluded from the analysis because the primary comparisons were of married and unmarried men. Of the remaining 174 (91%) men, two-thirds reported being married, and the remainder were single. This primary interview dataset was analysed between August and December 2004 using a record abstraction form.
Participants were instructed to report sexual behaviours between the year 1991 and being diagnosed with HIV. The questionnaire was developed, including sociodemographic data and patterns of sexual behaviour variables such as age of first sex, condom use during sexual activity, and other social factor variables. The type of sexual partners such as spouse, sex workers, and multiple sexual partners was included in the questionnaire as well. Participants were also questioned regarding the number of visits per month with sex workers, multiple sexual partners, or both. Social factors that were investigated as being associated with sex worker visits included invitation by a friend, alcohol consumption, extra spending money, active solicitation by a sex worker and watching a pornographic film. History of sexually transmissible infections (STIs) and knowledge of HIV infection were also part of the interview. Being diagnosed with STIs was based on a patient self-report. Common STI syndromes reported included the diagnosis and treatment of genital ulcers, urethral discharge, genital warts, or inguinal lymphadenitis.
Participants were diagnosed as HIV-infected when both the HIV 1/2 particle agglutination assay and the microparticle enzyme immunoassay were positive.7 Retrospective analysis of the survey data was reviewed and approved by the institutional review boards of Brown University and the SHCH.
The SHCH is an adult non-profit hospital, established in late 1996 in Phnom Penh, Cambodia. Between 1999 and 2003, approximately 5000 patients from across the country received free care at SHCH every month. By 2000, an estimated 800 HIV-infected patients were registered in the HIV clinic and the majority of them were diagnosed in advanced stages of the disease.
Survey definitions
In the survey, a ‘sex worker’ meant a woman who sold sex either in a brothel or non-brothel based setting. ‘Multiple sexual partners’ was defined a participant having had sex with more than one female partner that did not involve payment for sex. A ‘spouse’ was defined as a woman partner who lived with a man, and the man self-identified as being her husband. Sexual behaviours were defined as sexual intercourse with each type of partner before testing HIV-seropositive and were dichotomised by ‘yes’ or ‘no’ answers. The number of encounters with sex workers or multiple sexual partners and was categorised as either ‘one to two times’ or ‘three times or more’ per month.
Analyses
Contingency tables were generated by comparing the responses by marital status. Bivariate analyses were performed to evaluate the relationship between demographics, sexual behaviours, social factors, and history of sex worker visits.
Multiple logistic regression analyses were used to determine the adjusted odds ratio (OR) of each factor. All significant results at levels lower or equal to 0.15 in bivariate analyses were entered into models. ORs were used to interpret the strength of associations. A P-value < 0.05 of χ2 was considered statistically significant. Data analysis was performed at Brown University Community Health Department using SAS for windows 8.
Results
Demographics and HIV knowledge
Participant demographics and HIV knowledge are summarised in Table 1. In this survey, 109 (63%) HIV-infected men reported being soldiers, labourers, police officers, or farmers. Married patients were equally as likely as single patients to self-report being soldiers or police officers. Farmers (n = 14) or labourers (n = 32) were more likely to be married rather than single (31% v. 17%, P = 0.05). All were heterosexual and only three reported drug use. One hundred and six men (61%) were unaware that their sexual behaviours may have put them at risk of HIV infection. Married men were as likely as single men to report risk-taking behaviours. One hundred and fifteen men (76%) reported at least one episode of genital ulcer disease. Married men were equally as likely as single men to report an episode of genital ulcer disease.
Table 1.
Demographics and HIV knowledge
| Total n = 174 | Married n = 116 | Single n = 58 | P-value | ||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Mean (s.d.) age | 33 (7) | 35 (7) | 29 (4) | <0.0001 | |||
| Residence | |||||||
| Phnom Penh | 89 | 51 | 57 | 49 | 32 | 55 | 0.45 |
| Provinces | 85 | 49 | 59 | 51 | 26 | 45 | |
| Occupation | |||||||
| Solider | 46 | 26 | 25 | 22 | 21 | 36 | 0.037 |
| Police | 17 | 10 | 12 | 10 | 5 | 9 | |
| Labourer | 32 | 18 | 24 | 21 | 8 | 14 | |
| Farmer | 14 | 8 | 12 | 10 | 2 | 3 | |
| Unemployed | 15 | 9 | 7 | 6 | 8 | 14 | |
| OtherA | 50 | 29 | 36 | 31 | 14 | 24 | |
| Education level | |||||||
| ≥ Middle school | 90 | 52 | 54 | 47 | 36 | 62 | 0.37 |
| Primary school | 64 | 37 | 48 | 41 | 16 | 28 | |
| No school | 15 | 8 | 10 | 9 | 5 | 9 | |
| Not known | 5 | 3 | 0 | 0 | |||
| History of sexually transmissible infection | |||||||
| Yes | 115 | 76 | 74 | 77 | 41 | 76 | 0.52 |
| No | 36 | 24 | 23 | 24 | 13 | 24 | |
| Awareness of the risk of HIV infection | |||||||
| Yes | 50 | 29 | 34 | 29 | 16 | 28 | 0.38 |
| No | 41 | 24 | 27 | 23 | 14 | 24 | |
| Unsure | 65 | 37 | 40 | 34 | 25 | 43 | |
| Not known | 18 | 10 | 0 | 0 | |||
| Age of sexual debut | |||||||
| <20 | 77 | 44 | 54 | 47 | 23 | 40 | 0.55 |
| ≥20 | 85 | 49 | 56 | 48 | 29 | 50 | |
| Not known | 12 | 7 | 0 | 0 | |||
Including students, n = 2; governmental staff, n = 11, and minor self-businesses, n = 37 (such as barber, motor vehicle driver, street/market vendor, waiter, and occasional worker, etc.)
Patters of sexual behaviours
In the whole sample, the majority (n = 157) reported having sexual intercourse with a sex worker and 71 (41%) had multiple sexual partners. Sixty-five men (37%) reported intercourse with both sex workers and multiple sexual partners.
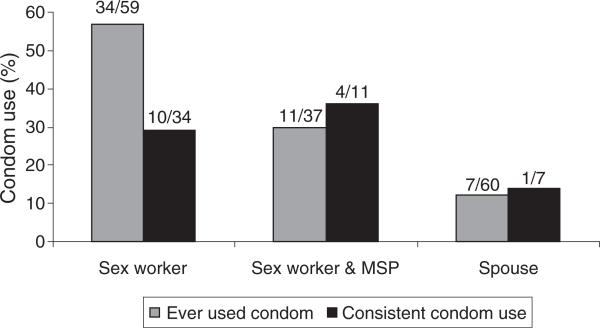
As presented in Table 2, married men were almost as likely as single men to report a history of sex with a sex worker (88% v. 95%). Overall, condom use was reported among 109 men (69%) when having sex with a sex worker. Only 17 men (24%) reported using a condom when having sex with their multiple sexual partners and 16 men (25%) said they wore a condom with sex workers and multiple sexual partners. The married men were less likely to report condom use with sex workers compared with single men (OR = 0.3; P = 0.008). Always using a condom with sex workers did not differ between married men and single men. The patterns of condom use by married patients with different types of partners are shown in Fig. 1.
Table 2.
Patterns of sexual behaviours stratified by marital status
| Characteristics | Total n = 174 | Married n = 116 | Single n = 58 | P-value | |||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| With a sex worker | |||||||
| Yes | 157 | 90 | 102 | 88 | 55 | 95 | 0.15 |
| No | 17 | 10 | 14 | 12 | 3 | 5 | |
| Number of visits (month) | |||||||
| 1 to 2 times | 116 | 74 | 78 | 79 | 38 | 72 | 0.33 |
| ≥3 times | 36 | 23 | 21 | 21 | 15 | 28 | |
| Not known | 5 | 3 | 0 | 0 | 0 | 0 | |
| History of condom use | |||||||
| Yes | 109 | 70 | 64 | 65 | 45 | 85 | 0.008 |
| No | 43 | 27 | 35 | 35 | 8 | 15 | |
| Not known | 5 | 3 | 0 | 0 | 0 | 0 | |
| Patterns of condom use | |||||||
| Always | 23 | 21 | 13 | 20 | 10 | 22 | 0.81 |
| Sometimes | 86 | 79 | 51 | 80 | 35 | 78 | |
| With multiple sexual partners | |||||||
| Yes | 71 | 41 | 46 | 40 | 25 | 43 | 0.66 |
| No | 103 | 59 | 70 | 60 | 33 | 57 | |
| Number of visits (month) | |||||||
| 1 to 2 times | 39 | 55 | 24 | 55 | 15 | 60 | 0.19 |
| ≥3 times | 30 | 42 | 20 | 45 | 10 | 40 | |
| Not known | 2 | 3 | 0 | 0 | 0 | 0 | |
| History of condom use | |||||||
| Yes | 17 | 24 | 12 | 30 | 5 | 20 | 0.22 |
| No | 48 | 67 | 28 | 70 | 20 | 80 | |
| Not known | 6 | 9 | 0 | 0 | 0 | 0 | |
| Patterns of condom use | |||||||
| Always | 6 | 35 | 5 | 42 | 1 | 20 | 0.41 |
| Sometimes | 11 | 65 | 7 | 58 | 4 | 80 | |
| With both | |||||||
| Yes | 65 | 37 | 41 | 35 | 24 | 41 | 0.43 |
| No | 109 | 63 | 75 | 65 | 34 | 59 | |
| Number of visits (month) | |||||||
| 1 to 2 times | 36 | 55 | 22 | 54 | 14 | 58 | 0.71 |
| ≥3 times | 29 | 45 | 19 | 46 | 10 | 42 | |
| History of condom use | |||||||
| Yes | 16 | 25 | 11 | 30 | 5 | 21 | 0.44 |
| No | 45 | 69 | 26 | 70 | 19 | 79 | |
| Not known | 4 | 6 | 0 | 0 | 0 | 0 | |
| Patterns of condom use | |||||||
| Always | 5 | 35 | 4 | 42 | 1 | 20 | 0.41 |
| Sometimes | 11 | 65 | 7 | 58 | 4 | 80 | |
Fig. 1.
Patterns of condom use by married men with each type of sex partner. MSP, multiple sexual partners.
Social factors associated with using a sex worker
The majority (n = 81) of male patients reported that they had sex when their friends invited them. Many (n = 68) reported that they had visited sex workers when they were consuming alcohol with friends. Men also said that they would seek sex with sex workers when they had extra spending money (n = 66). Thirty-four participants (37%) indicated that they engaged in intercourse with sex workers when they were solicited by women in brothels or night clubs, or by street girls (Table 3).
Table 3.
Social factors associated with visiting a sex worker
| Total n = 92 | Married n = 61 | Single n = 31 | P-value | ||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Invitation by friends | 81 | 88 | 51 | 84 | 30 | 97 | 0.07 |
| Alcohol consumption | 68 | 74 | 42 | 69 | 26 | 84 | 0.1 |
| Having extra spending money | 66 | 72 | 39 | 64 | 27 | 87 | 0.02 |
| Solicitation by a sex worker | 34 | 37 | 21 | 34 | 13 | 42 | 0.5 |
| Watching a pornographic film | 23 | 25 | 14 | 23 | 9 | 29 | 0.5 |
| Having a party | 21 | 23 | 12 | 20 | 9 | 29 | 0.3 |
| Feeling alienated | 16 | 17 | 8 | 13 | 8 | 26 | 0.1 |
| Lack of employment | 15 | 16 | 10 | 16 | 5 | 16 | 0.97 |
| Living far away from spouse | 15 | 15 | 15 | 25 | 0 | 0 | Not applicable |
| Getting along with spouse | 13 | 14 | 13 | 21 | 0 | 0 | Not applicable |
Factors associated with visiting a sex worker
In this survey, alcohol consumption (OR = 18.4; P = 0.008) and having extra spending money (OR = 14.5; P = 0.02) were strongly associated with visiting a sex worker for married men and single men before their diagnosis of HIV infection (Table 4). The number of visits to a sex worker (one to two times per month) of HIV-infected men, as well as visits to a sex worker, stratified by marital status, was also performed in multivariate analysis. However, these models were not found to be significant.
Table 4.
Factors associated with visiting a sex worker
| OR (95% confidence interval) Unadjusted | OR (95% confidence interval) AdjustedA | |
|---|---|---|
| Alcohol consumption | 45 (5.7–360)**** | 18.4 (2.1–159)** |
| Solicitation by a sex worker | 9.3 (1.2–73.8)** | |
| Having a party | 4.7 (0.6–37.8)* | |
| Having extra spending money | 40.6 (5.1–322)**** | 14.5 (1.7–127)** |
| Age <30 | 2.2 (0.8–6.4)* | |
| Age of sexual debut <20 | 2.7 (0.7–10.5)* |
Adjusting for solitciation by a sex worker, having a party, age <30 years, and first sex age <20 years. Invitation by friend, watching a pornographic film, feeling alienated, lack of employment, urban residence, soldiers, police, military (soldiers or police), low education (primary school or lower), ever used condom, and unknown risk for HIV infection were not statistically significant.
χ2 test:
P < 0.15
P < 0.05
***P < 0.01
P < 0.001
Discussion
The context of sexual behaviours is complex in human society. Many factors such as demographics, lifestyle, and cultural norms influence sexual activity and behaviour among youth and adults.8–11 The present study is the first survey from Cambodia to describe sexual behaviours among HIV-infected males before being diagnosed with HIV.
In a previous Cambodian study, farmers and labourers were rarely identified as a high-risk group for HIV infection.12 The present study showed that 63% of the HIV-infected men identified themselves as soldiers, labourers, police officers or farmers (Table 1). These findings indicate that farmers and labourers may also be acting as sexual bridges between sex workers and their low-risk spouses. This would be consistent with the observed dissemination of HIV, even to rural farming areas in Cambodia. HIV preventive programs of governmental institutions and non-governmental organisations in Cambodia should consider these populations in order to effectively prevent the future spread of new HIV infections in the country.
None of the survey participants reported anal intercourse. This is because these populations might find it uncomfortable to answer this question. Yet, because all men in the present study were self-identified as heterosexual; anal intercourse may rarely occur among them. Anal intercourse was reported by 81% (n = 206) of men who reported to have sex with men in Phnom Penh.13
Also, in the present study, only three men had used drugs. The relative risk of illicit drug use among them might have been low at that time. In 2004, the estimation of the prevalence of illicit drug use among adults in Cambodia was varied. For example, amphetamine use was 0.29%, heroin was 0.036%, and injecting drug use was 0.026%, according to the UNAIDS.14
Most (61%, Table 1) HIV-infected male patients were unaware of their risk for HIV infection through their sexual behaviours. Yet, two-thirds of this population reported a history of STIs. This finding highlights the potential role of STIs to increased risk for HIV acquisition.15,16 In a Thailand study, 43% of young men reported a history of STIs, which was strongly associated with HIV infection.17 The inability of HIV-infected Cambodian males to recognise the association between their sexual behaviours and HIV infection suggests that public awareness campaigns have not reached this group.
Our survey results showed that the vast majority (90%) of HIV-infected men reported a variety of sexual behaviours. A study in Thailand reported that 97% of HIV-infected men identified themselves as frequent sex worker visitors.18 The preference for buying sex in Cambodia may be one of the factors contributing to the country having the highest HIV prevalence in Asia.2,3 In the present survey, HIV-infected men reported that they used sex workers more frequently than multiple sexual partners (90% v. 41%, respectively). Further research studies are needed to understand why Cambodian men frequently use sex workers.
Condom use with sex workers by married men was lower than single men (P = 0.008), and condom use was similarly infrequent with their spouses (Fig. 1). Cambodian's Behavioral Surveillance Survey indicated that consistent condom use with a sex worker was 70% (for soldiers) and 81% (for police),19 an increase from earlier surveys, and is much higher than we observed in the present cohort (10/34, or 29%, Fig. 1). Of concern in these data is that the group of men with the highest risk for HIV infection also failed to use condoms with their spouses, effectively contributing to the generalisation of the epidemic. Perhaps this behaviour is not surprising, because only one-third of the survey populations felt that their behaviours were risky (Table 1).
Although the present survey showed that men were more likely to use sex workers than multiple sexual partners, as well as both, our survey failed to identify the different social factors associated with sex workers between married men and single men. As discussed earlier, further efforts should take this consideration.
The multivariate analysis in this study indicated alcohol consumption and having extra spending money were strongly associated with visiting a sex worker. Alcohol is one of the more powerful predictors of buying sex, which has also been described in studies in Thailand and Vietnam.8,9 One Ethiopian study also pointed out alcohol drinking was strongly and linearly associated with initiation of sexual activity, and alcohol intake had a significant and linear association with unprotected sex.11
This survey highlights that HIV-infected married patients had a high risk of sexual behaviours with sex workers, and a low prevalence of condom use. The risk patterns of this group should therefore be a focus of highest priority for prevention efforts to decrease new HIV infection. Intervention should also be targeted in settings where alcoholic beverages are consumed by Cambodian men in order to avoid a resurgence of the significant epidemic in this developing country that is slowly recovering from its recent genocide.
Acknowledgements
The authors thank the SHCH in Phnom Penh, Cambodia, for allowing the use of data. This investigation was supported by the Miriam Hospital, Brown University and the NIH Fogarty International Center AIDS International Training and Research Program Grant #TW00237 and Lifespan-Tufts-Brown CFAR #P30 AI42853.
Footnotes
Conflicts of interest
None declared.
References
- 1.Phalla T, Leng HB, Mills S, Bennett A, Wienrawee P, Gorbach P, et al. HIV and STD epidemiology, risk behaviors, and prevention and care response in Cambodia. AIDS. 1997;12:11–8. [PubMed] [Google Scholar]
- 2.UNAIDS/WHO [22 August 2007];AIDS Epidemic Update: December 2005. Available online at: http://www.unaids.org/epi/2005/doc/report_pdf.asp.
- 3.National Center for HIV/AIDS, Dermatology and STDs (NCHADS) [29 June 2007];Report on HIV Sentinel Surveillance (HSS) 2003. Available online at: http://www.nchads.org/Publication/HSS/HSS_2003_Report.pdf.
- 4.Abraham S. HIV in Southeast Asia. Harv AIDS Rev. 1998:2–6. Fall. [PubMed] [Google Scholar]
- 5.Prybylski D, Alto WA. Knowledge, attitudes and practices concerning HIV/AIDS among sex workers in Phnom Penh, Cambodia. AIDS Care. 1999;11:459–72. doi: 10.1080/09540129947857. 10.1080/09540129947857. [DOI] [PubMed] [Google Scholar]
- 6.Hor LB, Detels R, Heng S, Mun P. The role of sex worker clients in transmission of HIV in Cambodia. Int J STD AIDS. 2005;16:170–4. doi: 10.1258/0956462053057567. 10.1258/0956462053057567. [DOI] [PubMed] [Google Scholar]
- 7.UNAIDS-WHO Revised recommendations for the selection and use of HIV antibody tests. Wkly Epidemiol Rec. 1997;72:81–8. [PubMed] [Google Scholar]
- 8.Celentano DD, Nelson KE, Suprasert S, Eiumtrakul S, Kuntolbutra S, Beyrer C, et al. Behavioral and sociodemographic risks for frequent visits to commercial sex workers among northern Thai men. AIDS. 1993;7:1647–52. doi: 10.1097/00002030-199312000-00016. [DOI] [PubMed] [Google Scholar]
- 9.Thuy NT, Lindan CP, Phong TH, Van Dat, Nhung VT, Barclay J, et al. Predictors of visits to commercial sex workers by male attendees at sexually transmitted disease clinics in southern Vietnam. AIDS. 1999;13:719–25. doi: 10.1097/00002030-199904160-00013. [DOI] [PubMed] [Google Scholar]
- 10.Varga CA. South African young people's sexual dynamics: implications for behavioral responses to HIV/AIDS. Health Transition Center, Australian National University; Canberra: pp. 13–34. [Google Scholar]
- 11.Kebede D, Alem A, Mitike G, Enquselassie F, Berhane F, Abebe Y, et al. Khat and alcohol use and risky sex behaviors among in-school and out-of-school youth in Ethiopia. BMC Public Health. 2005;5:109–17. doi: 10.1186/1471-2458-5-109. 10.1186/1471-2458-5-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gorbach PM, National Center for HIV/AIDS, Dermatology and STDs (NCHADS) [29 June 2007];The Cambodian behavior surveillance survey, first round: 1997. University of Washington. Available online at: http://www.nchads.org/Publication/BSS/BSS1997.pdf.
- 13.Girault P, Saidel T, Song N, Wijngaarden VJ, Dallabetta G, Stuer F, et al. Family Health International (FHI) [13 March 2008];Sexual behavior, STIs and HIV among men who have sex with men in Phnom Penh, Cambodia. doi: 10.1521/aeap.16.1.31.27727. Available online at: http://www.fhi.org/en/HIVAIDS/pub/survreports/MSMCambodia/index.htm. [DOI] [PubMed]
- 14.UNAIDS [4 March 2008];Consensus estimates of the number of problem drug users in Cambodia, 2004. Available online at: http://www.un.org.kh/unaids/docs/CambodiadrugprevalenceestimatesJune2005.pdf.
- 15.Kassler WJ, Zenilman JM, Erickson B, Fox R, Peterman TA, Hook EW., 3rd Seroconversion in patients attending sexually transmitted disease clinics. AIDS. 1994;8:351–6. doi: 10.1097/00002030-199403000-00009. 10.1097/00002030-199403000-00009. [DOI] [PubMed] [Google Scholar]
- 16.Grosskurth H, Mosha F, Todd J, Mwijarubi E, Klokke A, Senkoro K, et al. Impact of improved treatment of sexually transmitted diseases on HIV infection in rural Tanzania: randomized controlled trial. Lancet. 1995;26:530–6. doi: 10.1016/s0140-6736(95)91380-7. 10.1016/S0140-6736(95)91380-7. [DOI] [PubMed] [Google Scholar]
- 17.Nopkesorn T, Mastro TD, Sangkharomya S, Sweat M, Singharaj P, Limpakarnjanarat K, et al. HIV-1 infection in young men in northern Thailand. AIDS. 1993;7:1233–40. doi: 10.1097/00002030-199309000-00013. 10.1097/00002030-199309000-00013. [DOI] [PubMed] [Google Scholar]
- 18.Nelson KE, Celentano DD, Suprasert S, Wright N, Eiumtrakul S, Tulvatana S, et al. JAMA. 1993;270:955–60. 10.1001/ jama.270.8.955. Risk factors for HIV infection among young adult men in northern Thailand.
- 19.Family Health International . The Cambodian behavioral surveillance survey 1997–1999. Family Health International; Phnom Penh: 1999. [2 July 2007]. Available online at: http://www.fhi.org/en/HIVAIDS/pub/survreports/Cambodia_BSS.htm. [Google Scholar]