Abstract
This case report describes the combined surgical, orthodontic and prosthodontic rehabilitation of an adult female patient with a previous history of follicular ameloblastoma, which was treated through partial mandibulectomy and an immediate replacement of missing bone with an autologous calvarial bone graft. Orthodontic treatment was undertaken in order to restore occlusal disturbances and obtain sufficient space for two dental implants and an optimum prosthodontic rehabilitation.
Keywords: Follicular ameloblastoma, Bone graft, Mandibulectomy, Orthodontic treatment
INTRODUCTION
Ameloblastoma is a benign but locally aggressive neoplasm of the odontogenic epithelium.1 Accounting for 11% of all odontogenic tumors, ameloblastoma is the most common odontogenic neoplasm affecting the jaws, yet it only accounts for 1% of all tumors of the maxilla and mandible.2–4 The average age of patients presenting with ameloblastoma is 36 years, with men and women being equally affected.5 Ameloblastomas are classified as solid/multicystic, intraosseous, or unicystic, with peripheral subtypes.6,7 The radiographic appearance of ameloblastoma, dentigerous cysts, and odontogenic keratocysts is similar and for this reason a biopsy is recommended to obtain a precise diagnosis of ameloblastoma.8 Although a benign tumor, ameloblastoma is aggressive because of the myeline nature of its growth and because its conservative treatment is associated with a high rate of recurrence (50%–90%). Primary resection of this benign tumor is, therefore, considered the only predictable curative form of therapy.7–11 Unfortunately, this treatment leaves the patient with a defect in the affected region of the jaw. A multi-disciplinary approach is needed for the patient’s complete rehabilitation, including bone grafting, the planned placement of implant, and the prosthetic work. Sometimes the orthodontist’s role in this multidisciplinary approach is to create an optimum occlusal relationship and sufficient space to allow for successful reconstruction of the affected region of the jaw.
CASE REPORT
Diagnosis and etiology
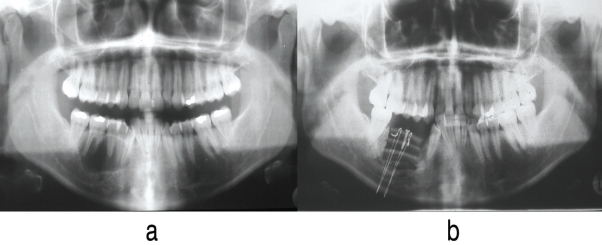
A 31-year-old Caucasian female was referred to the Graduate Orthodontic Clinic of Aristotle University of Thessaloniki following mandibulectomy and immediate replacement of removed bone with autologous calvarial bone graft for the purposes of evaluation and treatment of occlusal disturbances. The patient’s medical/dental history referred to a tumor, which was histologically classified as follicular ameloblastoma. According to the history, the tumor was located in the posterior right mandibular region encompassing three teeth, specifically the first and second premolars and the first molar. The first author performed a partial mandibular resection and an immediate reconstruction utilizing bone graft taken from the patient’s calvaria. All three teeth were removed along with the tumor (Figure 1).
Figure 1.
Panoramic radiographs: a. initial radiograph showing the tumor in the right lower region; b. following partial mandibular resection and immediate reconstruction using calvarial bone graft.
Extraoral examination revealed an orthognathic profile without facial asymmetry and with the lips competent at rest (Figure 2). Intraoral examination revealed amalgam restorations in all maxillary and mandibular second molars, in the left first maxillary premolar, and the left mandibular first molar. Clinical examination indicated satisfactory dental hygiene and periodontal condition, with absence of bleeding on probing and no significant pocket depths. An analysis of dental casts revealed a Class I malocclusion characterized by a 3 mm overjet, 3 mm of overbite, moderate crowding in the anterior region of both dental arches (3 mm crowding in the maxillary dental arch and 6 mm in the mandibular one, respectively), a labially positioned mandibular right canine, a 2 mm deviation of the lower dental arch midline to the right, moderate Bolton tooth size discrepancy (mandibular anterior relatively larger than maxillary ones), and an edentulous space due to the aforementioned surgical procedure (Figure 2).
Figure 2.
Pre-treatment extraoral and intraoral photographs.
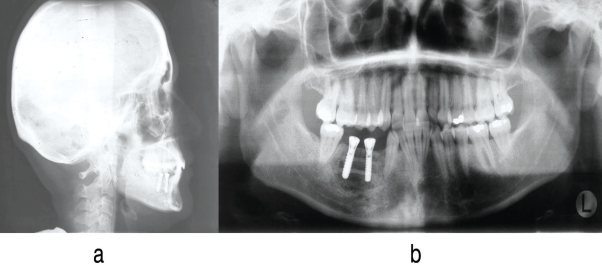
Panoramic radiograph showed no pathology. Analysis of the cephalometric radiograph indicated harmonious sagittal and vertical skeletal relationships (SNA: 83°, SNB: 80°, facial angle: 90°, ANB: 3°, individual ANB: 3.5°) (Figure 3).
Figure 3.
Pre-treatment X-rays, after implant placement: a. cephalometric radiograph; b. panoramic radiograph.
Treatment objectives and alternatives
The problem list for this patient included the presence of a Class I malocclusion characterized by a condition of moderate crowding in the anterior region of both dental arches, a labially positioned mandibular right canine, a mild deviation of the mandibular dental arch midline to the right, a moderate tooth size discrepancy, and an edentulous space in the right posterior area of the mandible due to the extractions of the right premolars and first molar. The patient’s chief complaint referred to the need for optimum prosthetic rehabilitation and a desire for improvement of dental esthetics.
A comprehensive orthodontic treatment aiming to correct the above-mentioned occlusal problems was proposed and accepted by the patient.
Treatment progress
The placement of the two dental implants took place by the first author prior to the orthodontic treatment and according to the orthodontic treatment plan. A setup of the patient’s dental casts was made to facilitate accurate determination of the exact positions of the two implants. Following their placement, a lingual arch was banded on the lower dental arch for anchorage and space preservation. Fixed appliances (.018″ X .022″, Roth) were bonded on the maxillary teeth in order to level and align the dental arch. Following the placement of a bracket, the mandibular right canine was uprighted and brought into the dental arch by means of a T-loop. Then, fixed appliances were bonded to the remaining mandibular teeth and reproximation took place on the lower incisors. The fixed appliances were removed after alignment and leveling of both dental arches, crowding alleviation, and correction of dental arch midlines. Essix ® maxillary and mandibular splints were used for retention until the placement of prostheses (Figure 4). New Essix ® mandibular retainer was delivered following the end of prosthetic work. Due to the patient’s advanced stage of pregnancy (9th month) and the relevant inconvenience, at this stage it was not possible to place a bonded lingual retainer in the lower anterior teeth, as was originally planned.
Figure 4.
Post-orthodontic treatment photographs and X-rays.
Treatment results
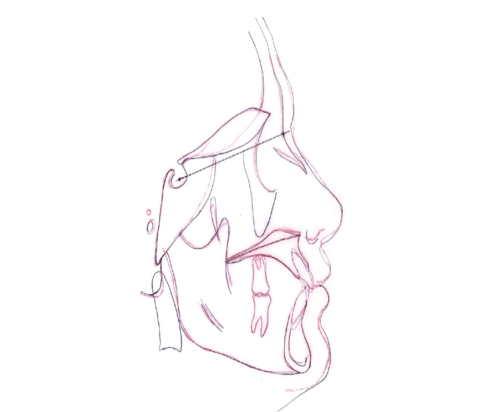
The active orthodontic treatment utilizing fixed appliances in both dental arches lasted 11 months. Superimposition of the initial and final tracings of the lateral cephalometric X-rays indicated that slight labial proclination of the upper and lower incisors occurred post-treatment (Figure 5). Prosthodontic rehabilitation of the partially edentulous right mandibular dental arch region was achieved through the placement of two implants and two crowns, respectively (Figure 6).
Figure 5.
Overall superimposition of initial and final lateral cephalometric tracings.
Figure 6.
Post-treatment photographs.
DISCUSSION
Ameloblastoma is a benign odontogenic tumor arising from the residual epithelial components of tooth development. It is a slow growing, locally aggressive tumor capable of causing facial deformity, with a high recurrence rate due its capacity to infiltrate trabecular bone. The treatment of ameloblastoma varies from curettage to en block resection. Bone grafts replace the surgically removed bone, with autologous bone grafting being the most desirable. It is typically harvested from intraoral sources (e.g., chin) or extraoral sources (e.g., iliac crest, fibula, calvarial bone).
The most commonly used graft material for alveolar ridge reconstruction is free autogenous iliac bone.12 In this case, however, autologous calvarial bone grafts were used to reconstruct the missing mandibular bone following the surgical resection of the tumor and the removal of three teeth in the region. The advantages of calvarial bone grafting include good integration, absence of pain from the donor site, and no visible scar. These advantages, however, are not applicable in the case of thin calvaria bone with a thickness of less than 5 mm.12 Recent reports on the use of calvarial bone grafting for the reconstruction and subsequent placement of dental implants have presented good clinical outcomes, with low rates of graft resorption and high implant survival rates.13–16 The results of these studies have showed that calvarial bone grafting appears to be less prone to resorption than iliac grafts are.
In this case, complete functional rehabilitation of the patient included the replacement of the lost three teeth. This goal could have been achieved by the placement of two implants and a bridge, replacing all three teeth. However, this treatment plan would not have addressed the patient’s chief complaint, nor would it result in optimum functionality and esthetics. Accordingly, the placement of the two implants was decided in relation to the orthodontic treatment plan, aiming for an optimum result. The two implants were placed in the posterior region of the edentulous area, hence replacing only two of the missing teeth, with the extra space being used to correct crowding and to improve dental occlusion.
The outcome of this interdisciplinary approach was the satisfactory restoration of both occlusal function and esthetics.
CONCLUSIONS
A multidisciplinary approach, including oral surgery, orthodontics, and prosthodontics was able to provide a patient diagnosed with follicular ameloblastoma in the right mandibular region with a satisfactory occlusion following partial mandibular resection and removal of adjacent teeth in the affected site.
REFERENCES
- 1.Junquera L, Ascani G, Vicente JC, Garcia-Consuegra L, Roig P. Ameloblastoma revisited. Ann Otol Rhinol Laryngol. 2003;112:1034–1039. doi: 10.1177/000348940311201207. [DOI] [PubMed] [Google Scholar]
- 2.Gorlin RJ, Chaudhry AP, Pindborg JJ. Odontogenic tumors: Classification, histopathology clinical behaviour in man and domesticated animals. Cancer. 1961;14:73–101. doi: 10.1002/1097-0142(196101/02)14:1<73::aid-cncr2820140111>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 3.Adekeye EO. Ameloblastoma of jaws: A survey of 109 Nigerian patients. J Oral Surg. 1980;38:36–41. [PubMed] [Google Scholar]
- 4.Adekeye EO, Lavery KM. Recurrent ameloblastoma of the maxillofacial region. Clinical features and treatment. J Maxillofac Surg. 1986;14:153–157. doi: 10.1016/s0301-0503(86)80282-x. [DOI] [PubMed] [Google Scholar]
- 5.Reichart PA, Philipsen HP, Sonner S. Ameloblastoma: biological profile of 3677 cases. Eur J Cancer B Oral Oncol. 1995;31:86–99. doi: 10.1016/0964-1955(94)00037-5. [DOI] [PubMed] [Google Scholar]
- 6.Ghandhi D, Ayoub AF, Pogrel MA, MacDonald G, Brocklebank LM, Moos KF. Ameloblastoma: a surgeon’s dilemma. J Oral Maxillofac Surg. 2006;64:1010–1014. doi: 10.1016/j.joms.2006.03.022. [DOI] [PubMed] [Google Scholar]
- 7.Carlson ER, Marx RE. The ameloblastoma: primary, curative surgical management. J Oral Maxillofac Surg. 2006;64:484–494. doi: 10.1016/j.joms.2005.11.032. [DOI] [PubMed] [Google Scholar]
- 8.Peterson LJ, Ellis E, Hupp J, Tucker MR. Contemporary oral and maxillofacial surgery. St. Louis: Elsevier Health Sciences; 2002. pp. 345–357. [Google Scholar]
- 9.Shatkin S, Hoffmeister FS. Ameloblastoma: a rational approach to therapy. Oral Surg Oral Med Oral Pathol. 1965;20:421–435. doi: 10.1016/0030-4220(65)90231-8. [DOI] [PubMed] [Google Scholar]
- 10.Sehdev MK, Huvos AG, Strong EW, Gerold FP, Willis GW. Ameloblastoma of maxilla and mandible. Cancer. 1974;33:324–333. doi: 10.1002/1097-0142(197402)33:2<324::aid-cncr2820330205>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 11.Müller H, Slootweg PJ. The ameloblastoma, the controversial approach to therapy. J Maxillofac Surg. 1985;13:79–84. doi: 10.1016/s0301-0503(85)80021-7. [DOI] [PubMed] [Google Scholar]
- 12.Gleizal AM, Beziat JL. Maxillary and mandibular reconstruction using bicortical calvarial bone grafts: a retrospective study of 122 reconstructions in 73 patients. Plast Reconstr Surg. 2007;119:542–548. doi: 10.1097/01.prs.0000246377.67189.c6. [DOI] [PubMed] [Google Scholar]
- 13.Iizuka T, Smolka W, Hallermann W, Mericske-Stern R. Extensive augmentation of the alveolar ridge using autogenous calvarial split bone grafts for dental rehabilitation. Clin Oral Implants Res. 2004;15:607–615. doi: 10.1111/j.1600-0501.2004.01043.x. [DOI] [PubMed] [Google Scholar]
- 14.Bianchi AE, Vinci R, Torti S, Sanfilippo F. Atrophic mandible reconstruction using calvarial bone grafts and implant-supported overdentures: radiographic assessment of autograft healing and adaptation. Int J Periodontics Restorative Dent. 2004;24:334–343. [PubMed] [Google Scholar]
- 15.Smolka W, Bosshardt DD, Mericske-Stern R, Iizuka T. Reconstruction of the severely atrophic mandible using calvarial split bone grafts for implant-supported oral rehabilitation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:35–42. doi: 10.1016/j.tripleo.2005.03.022. [DOI] [PubMed] [Google Scholar]
- 16.Gratz KW, Sailer HF, Haers PE, Oechslin CK. Mandibular reconstruction with full thickness calvarial bone and temporal muscle flap. Br J Oral Maxillofacial Surg. 1996;34:379–385. doi: 10.1016/s0266-4356(96)90091-1. [DOI] [PubMed] [Google Scholar]