Abstract
Purpose
Intra-articular screw penetration is one complication of volar plate fixation of distal radius fractures. This study was designed to determine the most utilized imaging techniques and views during volar plating of distal radius fractures and to evaluate surgeons’ ability to detect intra-articular screw placement on static fluoroscopic images and rotational fluoroscopy.
Methods
Active members of The American Society for Surgery of the Hand were polled regarding preferred imaging techniques (fluoroscopic versus cassette radiographs) and views (rotational fluoroscopy, static orthogonal/anatomic tilt/semi-pronated imaging) during volar plating of distal radius fractures. Following the survey, volar locking plates were applied to 30 cadaveric distal radii. A single screw intentionally penetrated the radiocarpal joint in half of the specimens (15 arms) and intentionally did not penetrate the radiocarpal joint in the other half. Imaging (standard posterior-anterior (PA) and lateral views, 11° tilt PA and 22° tilt lateral views, and two 360° fluoroscopy movies) was performed utilizing a custom jig. Five blinded surgeons reviewed randomized image sets evaluating for intra-articular screw placement. Receiver operating characteristic curves were constructed to compare the reliability of each fluoroscopic projection/movie.
Results
Among 696 survey respondents, 88% exclusively utilized fluoroscopic imaging (without cassette radiographs) and nearly 66% preferred either tilt images or rotational fluoroscopy to detect intra-articular screw penetration. In our cadaveric model, rotational fluoroscopy provided the highest sensitivity (93%) and specificity (96%) for the detection of intra-articular screw penetration. Rotational fluoroscopy was significantly more reliable (p<0.01) than most images (standard lateral, 11° PA, 22° lateral, paired PA/lateral) and trended strongly toward better reliability for all remaining images (standard PA [p=0.07], paired 11° PA/22° lateral [p=0.08], 22° tilt fluoroscopy movie [p=0.11]).
Conclusions
Rotational fluoroscopy improves the surgeon’s ability to detect intra-articular screw penetration during volar plating of the distal radius. No combination of imaging allowed detection of all intra-articular screws. A high level of suspicion for intra-articular screw penetration should be maintained during volar plating of distal radial fractures.
Level of evidence
Unable to be determined according to guidelines
Keywords: complication, distal radius, fracture, fluoroscopy, volar plate
Introduction
Volar locked plating systems are now widely utilized in the treatment of distal radius fractures. Advocates of volar plating cite decreased extensor tendon irritation compared with dorsal plating, ease of fracture reduction, and sufficient stability to afford early postoperative mobilization. Unlike dorsal plating, a radiocarpal arthrotomy is not performed during volar fixation and screw placement is commonly assessed radiographically. This risks an increasing incidence of screw penetration into the radiocarpal joint. Unrecognized intra-articular hardware may lead to early arthrosis and compromise clinical outcomes.
The geometry of the distal radius prevents any single radiographic view from profiling the entire articular surface.1 The articular surface is biconcave, with scaphoid and lunate facets. The average radial inclination is 22° and the average palmar tilt is 11°.2, 3 This obliquity makes it difficult to evaluate the articular surface on standard posterior-anterior (PA) and lateral radiographic projections. While those orthogonal views are perpendicular to the long axis of the radius, they are typically oblique projections of the radiocarpal articular surface.
“Anatomic tilt” radiographic projections (11° PA, 22° lateral) are intended to better profile the articular surface in order to judge fracture reduction or intra-articular penetration by hardware. Boyer et al reported superior ability to detect intra-articular screw penetration following dorsal plating of the distal radius using these projections.4 A 45° pronated oblique view is also described for assessing proper screw placement in the subchondral bone.5 Several authors have demonstrated the utility of anatomic tilt x-rays in assessing reduction of the distal radius articular surface.6, 7
To our knowledge, only one investigator has evaluated the accuracy of tilt images for detecting intra-articular screw penetration during volar plating of the distal radius.1 Soong et al determined that multiple tilted radiographic projections were necessary to accurately judge all of the screws placed through a volar plate.1
Our study objectives were two-fold. First, we sought to identify which fluoroscopic projections members of the American Society for Surgery of the Hand (ASSH) rely upon during volar distal radius plating and what those surgeons perceived as the incidence of intra-articular hardware. Second, we attempted to quantify surgeons’ ability to detect intra-articular screws following volar distal radius plating using both static fluoroscopic imaging (standard and tilt views) and rotational fluoroscopy. Our hypothesis was that rotational fluoroscopy would provide superior visualization of hardware within the radiocarpal joint.
Materials and Methods
Survey
All active members of The American Society for Surgery of the Hand (ASSH) were polled to determine their preferences regarding radiographic views (question 1 below) and imaging technique (question 2 below) during volar plating of distal radius fractures. Using SurveyMonkey (SurveyMonkey, Menlo Park, CA), a three question Internet-based survey was sent to 1493 surgeons. The three questions were as follows:
Following volar plating of a distal radius fracture, what is your preferred method of intraoperative imaging to assess for intra-articular screw penetration?
For your “final films” do you typically use standard cassette x-rays, fluoroscopy only, both?
What percent of the time do you believe that screws/pegs are left intra-articularly after distal radius plating (overall, not personal incidence)? An open comment section was provided following these questions.
Cadaveric Study
Thirty, fresh-frozen cadaveric arms were used for this study. Each specimen was thawed to room temperature overnight before experimentation. A volar distal radius locking plate (Acumed Acu-Loc, Hillsboro, OR) was placed on each specimen via a standard volar approach. The plate was positioned where its contour best fit the distal radius. Although clinical practice is to combine contour fit with fluoroscopic evaluation of placement, the use of intact radii resulted in only a single position (proximal to distal) where the plate’s contour matched that of the radius. The two distal rows of screw holes on each plate were filled with locking screws or pegs. Half (15) of the specimens had a single screw or peg intenstionally placed from the distal row penetrating into the radiocarpal joint. A dorsal arthrotomy was made in each specimen to record the presence and location (scaphoid/lunate facet) of intra-articular screws. Joint penetration from the screws ranged from 1 to 3 millimeters.
A custom jig was constructed consisting of a cross-slide rotary table with specimens secured within radiolucent PVC pipe (Figure 1). The jig allowed precise positioning of the specimen (to the nearest degree) as well as the ability to rotate the specimen 360°. Six fluoroscopic projections were then recorded for each specimen with the use of a mini-C arm (Hologic Insight, Bedford, MA): standard PA, standard lateral, 11° tilt PA, 22° tilt lateral, and rotational fluoroscopy movies at 0° and 22° of inclination in relation to the long axis of the radius (Figure 2,3). The 22° inclination movie was included to test fluoroscopy performed at an inclination believed to provide an optimal joint profile as it rotated through the lateral projection. Each movie recorded one complete 360° rotation such that the wrist began imaged in a posterior-anterior position and then was rotated clockwise keeping the fluoroscopic unit stationary until returning to the PA position. A total of 180 images/movies were collected, downloaded, and compiled as a digital slide show.
Figure 1.
Custom cross-slide rotary table used to position specimens.
Figure 2.
Standard PA and lateral fluoroscopic projections.
Figure 3.
Anatomic tilt (11° volar, 22° lateral) fluoroscopic projections.
Five blinded surgeons were shown the individual images in random order. The surgeons included one hand fellowship-trained orthopaedic surgeon, three orthopaedic hand fellows, and one orthopaedic chief resident. The observers were asked to record: a) whether or not any screw was intra-articular at the radiocarpal joint, and b) the location of any intra-articular screw (scaphoid or lunate facet). In the initial viewing, each image/movie was presented and rated in isolation (i.e. the PA view and lateral views of each specimen were separated). The images were then reshuffled in random order and presented to the observers two weeks after the first viewing. In the second viewing, the images were presented as pairs, with either PA/lateral or 11° PA/22° lateral tilt projections of each specimen appearing simultaneously. The rotational fluoroscopy movies were presented independently.
Statistical Methods
Power analysis was performed to determine the number of observations needed to detect a difference in accuracy of at least 8% between fluoroscopic projections. Alpha was set to 0.05 and beta was set to 0.20. We calculated that at least 138 observations were needed to detect such a difference. Using 5 surgeons and 30 specimens we obtained 150 observations for each fluoroscopic projection.
The ability of each fluoroscopic image/movie to demonstrate intra-articular screws was assessed in several ways. Sensitivity (probability that the surgeon would respond positively when a screw was placed in the joint), specificity (probability that the surgeon would respond negatively when there is no screw placed in the joint), and kappa values were calculated for each projection/movie using the visual assessment of intra-articular hardware by arthrotomy as the gold standard. For these determinations, data across all observers were treated as independent observations.
Area under receiver operating characteristic (ROC) curves constructed from the sensitivity and specificity of each fluoroscopic projection was analyzed using chi-square testing. This determined if there were significant differences between the various projections.
For specimens with intra-articular hardware, chi square and Fisher’s exact test were used to determine if the location (i.e. scaphoid or lunate facet) or depth of joint penetration of the intra-articular screw impacted the proportion of correct observations that identified the articular penetration.
Post-hoc analysis confirmed data adequacy. Kappa values were determined for surgeon agreement with the gold standard for each observing surgeon on each fluoroscopic projection. This revealed minimal differences between the individual observing surgeons both in viewing the entire set of images and in viewing each individual image type. Ninety-five percent confidence intervals were also examined for the sensitivity of rotational fluoroscopy and paired image viewings as sensitivity was judged to be the most important image property (to prevent unrecognized intra-articular hardware) and paired image viewing most closely replicated the viewing of fluoroscopic data in the clinical setting. Confidence intervals for those images’ sensitivity were 14% or less which confirmed sample size adequate for reasonably precise results.
Source of Funding
Funding for this study was provided by a grant from the University Orthopaedic Research and Education Foundation (UOREF). No outside sources of funding were utilized.
Results
Survey Results
Six hundred and ninety six ASSH members (47%) responded to our survey. Responses indicated that the majority of surgeons relied upon both anatomic tilt views and rotational fluoroscopy to determine if hardware was placed intra-articularly (Table 1). Less than 13% of surgeons ordered final cassette radiographs following fixation (Table 2). Finally, 70% of surgeons estimated the incidence of unrecognized intra-articular hardware between 1% and 5%(Table 3). In the “open comments” section of the survey, the majority of surgeons reported having identified intra-articular screws but few noted having placed intra-articular screws themselves.
Table 1.
Responses to survey question: Following volar plating of a distal radius fracture, what is your preferred method of intraoperative imaging to assess for intra-articular screw penetration? (choose all that apply)
| Imaging Technique | Response percent | Response count |
|---|---|---|
| Live, rotational fluoroscopic views | 67% | 466 |
| Anatomic tilt (11° PA and 22° lateral) views | 65% | 451 |
| Standard PA and lateral views | 23% | 161 |
| 45° pronated view | 11% | 77 |
Table 2.
Responses to survey question: For your final films, do you typically use:
| Imaging Technique | Response percent | Response count |
|---|---|---|
| Fluoroscopy only | 87.6% | 606 |
| Standard cassette x-rays | 3.6% | 25 |
| Both | 8.8% | 61 |
Table 3.
Responses to survey question: What percentage of time do you believe that screws/pegs are left intra-articularly after distal radius plating? (overall, not personal, incidence)
| Incidence of intra-articular hardware |
Response percent | Response count |
|---|---|---|
| 0% | 12.3% | 87 |
| 0-2% | 34.9% | 246 |
| 2-5% | 36.7% | 259 |
| 5-10% | 13.0% | 92 |
| >10% | 3.0% | 21 |
Cadaveric Results
The surgeons evaluating images in this study performed similarly. Viewing static images, the overall rate of correct responses for the 5 surgeons ranged from 77% to 84%. Viewing fluoroscopy movies and paired images, the overall rate of correct responses ranged from 88% to 93%. Kappa values for each surgeon’s accuracy on each of the fluoroscopic projections revealed consistency between the surgeons (Table 4). There was no correlation with level of training.
Table 4.
Kappa values for surgeon agreement with the gold standard by image type.
| View | Kappa Range |
|---|---|
| PA | 0.73-0.87 |
| 11° PA | 0.53-0.80 |
| Lateral | 0.07-0.13 |
| 22° Lateral | 0.40-0.67 |
| Neutral Fluoroscopy Movie | 0.87-0.93 |
| 22° Tilt Fluoroscopy Movie | 0.73-0.93 |
| PA/Lateral paired | 0.53-0.80 |
| 11° PA/ 22° Lateral paired | 0.73-0.87 |
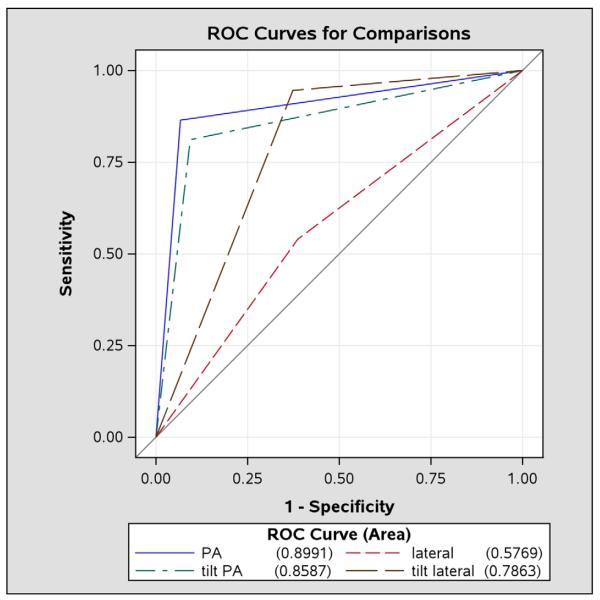
Table 5 summarizes the observers’ ability to accurately determine whether or not screws were intra-articular on each fluoroscopic view. When each static image was observed without a paired orthogonal view, the PA and 11° PA performed similarly (p=0.13). The standard PA image proved superior to both the lateral and 22° lateral projections (p<0.05) (Figure 4).
Table 5.
Reliability of each image type used to detect intra-articular hardware.
| View | Gold Standard |
Raters | Kappa (95% CI) | AUC (95% CI) | Sn (95% CI) Sp (95% CI) |
||
|---|---|---|---|---|---|---|---|
| absent | present | total | |||||
| PA | absent | 64 | 10 | 74 | 0.80 (0.70, 0.90) | 90% (85%, 95%) | Sn=93% (85%, 98%) Sp=86% (77%, 93%) |
| present | 5 | 70 | 75 | ||||
| total | 69 | 80 | 149 | ||||
| Lateral | absent | 40 | 35 | 75 | 0.15 (−0.01, 0.30) | 58% (50%, 66%) | Sn=61% (49%, 72%) Sp=53% (41%, 65%) |
| present | 29 | 46 | 75 | ||||
| total | 69 | 81 | 150 | ||||
| 11° PA | absent | 60 | 15 | 75 | 0.71 (0.59, 0.82) | 86% (80%, 91%) | Sn=91% (82%, 96%) Sp=80% (69%, 88%) |
| present | 7 | 68 | 75 | ||||
| total | 67 | 83 | 150 | ||||
| 22° Lateral |
absent | 71 | 4 | 75 | 0.57 (0.45, 0.70) | 79% (73%, 85%) | Sn=63% (51%, 74%) Sp=95% (87%, 99%) |
| present | 28 | 47 | 75 | ||||
| total | 99 | 51 | 150 | ||||
| Neutral Movie |
absent | 72 | 3 | 75 | 0.89 (0.82, 0.97) | 95% (91%, 98%) | Sn=93% (85%, 98%) Sp=96% (89%, 99%) |
| present | 5 | 70 | 75 | ||||
| total | 77 | 73 | 150 | ||||
| 22° Tilt Movie |
absent | 68 | 7 | 75 | 0.81 (0.72, 0.91) | 91% (86%, 95%) | Sn=91% (82%, 96%) Sp=91% (82%, 96%) |
| present | 7 | 68 | 75 | ||||
| total | 75 | 75 | 150 | ||||
| PA/Lat | absent | 57 | 18 | 75 | 0.69 (0.58, 0.81) | 85% (79%, 90%) | Sn=93% (85%, 98%) Sp=76% (65%, 85%) |
| present | 5 | 70 | 75 | ||||
| total | 62 | 88 | 150 | ||||
| 11° PA / 22° Lat |
absent | 67 | 8 | 75 | 0.81 (0.72, 0.91) | 91% (86%, 95%) | Sn=92% (83%, 97%) Sp=89% (80%, 95%) |
| present | 6 | 69 | 75 | ||||
| total | 73 | 77 | 150 | ||||
Sn = sensitivity, Sp=specificity, AUC=area under ROC curve, 95%CI=confidence interval
Figure 4.
ROC curves for static images, each viewed in isolation.
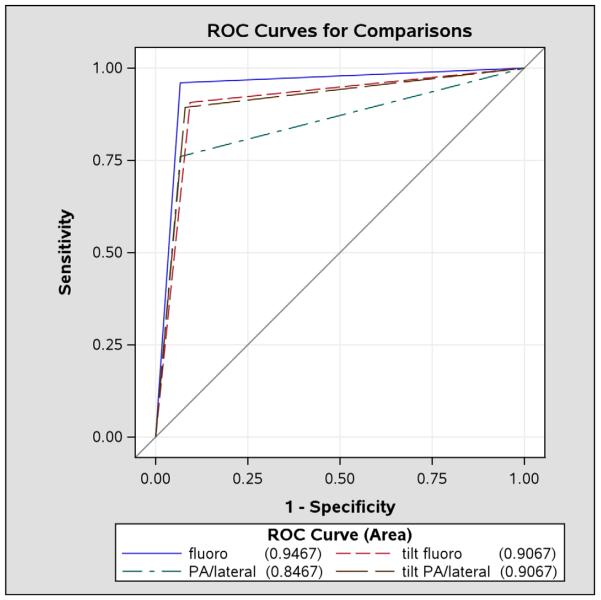
Figure 5 presents the ROC curves for the fluoroscopy movies and static images viewed as orthogonal pairs. The neutral fluoroscopy movie significantly outperformed the paired PA/lateral views (p<0.01) and trended toward superiority over the 22° fluoroscopy movie (p=0.11) and the paired 11° PA/22° lateral images (p=0.08).
Figure 5.
ROC curves for the images viewed in pairs and rotational fluoroscopy (fluoro = fluoroscopy).
Surgeons were more likely to detect screw intra-articular screw penetration as the depth of the penetration increased (p<0.01). When viewing each image in isolation, 54 of 180 observations (30%) missed screws that protruded into the joint by 1mm while only 39 of 270 observations (14%) failed to identify screws that protruded 2-3mm into the joint. When viewing paired orthogonal images, 9 of 60 observations (15%) did not identify screws entering the joint 1mm while 2 of 90 observations (2%) failed to identify screws with 2-3mm of joint penetration.
The sensitivity of each image type to detect 1mm of joint penetration was assessed in 6 cadaver specimens. Sensitivity remained the highest for rotational fluoroscopy (87%), the PA view (83%), and the 11°PA view (80%). All other individual views performed poorly (57-67%).
When viewing each fluoroscopic projection independently, observers were equally accurate in determining intra-articular screw presence in the scaphoid and lunate facets. Observers were generally less likely to miss intra-articular screws entering the lunate facet when viewing fluoroscopy movies or paired PA/lateral or 11° PA/22° lateral images (Table 6).
Table 6.
Comparison of surgeon ability to detect intra-articular hardware by screw location.
| View | Rater determination of screw presence |
Location, gold standard |
p-value* | |
|---|---|---|---|---|
| Location 1 |
Location 2 | |||
| PA | Incorrect | 3 (10%) | 2 (5%) | 0.64† |
| Correct | 27 (90%) | 38 (95%) | ||
| Lateral | Incorrect | 11 (37%) | 17 (42%) | 0.62 |
| Correct | 19 (63%) | 23 (58%) | ||
| 11° PA | Incorrect | 4 (13%) | 3 (8%) | 0.45† |
| Correct | 26 (87%) | 37 (92%) | ||
| 22° Lateral |
Incorrect | 10 (33%) | 17 (42%) | 0.44 |
| Correct | 20 (67%) | 23 (58%) | ||
| Neutral Movie |
Incorrect | 3 (10%) | 1 (2%) | 0.31† |
| Correct | 27 (90%) | 39 (98%) | ||
| 22° Tilt Movie |
Incorrect | 6 (20%) | 0 | 0.004† |
| Correct | 24 (80%) | 40 (100%) | ||
| PA/Lat | Incorrect | 4 (13%) | 0 | 0.03† |
| Correct | 26 (87%) | 40 (100%) | ||
| 11°PA/ 22°Lat |
Incorrect | 5 (17%) | 1 (2%) | 0.08† |
| Correct | 25 (83%) | 39 (98%) | ||
P-value compares proportion correct across locations by chi-square test, unless otherwise indicated.
P-value by Fisher’s exact test.
Even when presented with either paired orthogonal fluoroscopic projections or rotational movies, surgeons failed to recognize intra-articular screws. On each set of paired static images or movie, a total of 75 observations were made in which a screw penetrated in the radiocarpal joint (15 specimens with intra-articular screws, 5 observers). On static images, 5 (7%) observations missed such hardware on standard orthogonal images while 6 (8%) observations failed to identify the joint penetration on 11° PA/22° lateral projections. Similarly, 5 (7%) observations of neutral fluoroscopy missed intra-articular hardware and 7 (9%) observations of 22° movies missed such hardware. Of the 11 observations in which intra-articular screws were missed on a pair of static images, 6 were correctly recognized on fluoroscopy of that same specimen by the respective surgeon. Similarly, 7 of the 12 observations that missed screws within the radiocarpal joint that on fluoroscopy were correctly identified by the respective surgeon on paired static images of that specimen.
Discussion
The results of our survey to ASSH members provided a clinical basis for our cadaveric study. As 88% of responding surgeons indicated a sole reliance on fluoroscopic imaging for volar fixation of the distal radius, we were assured that a study without cassette radiographs would most closely approximate current practice. The large proportion of surgeons utilizing live rotational fluoroscopy in addition to tilt images demonstrated a need to attempt to quantify the contribution of fluoroscopy to volar distal radius fixation.
Boyer et al critically evaluated the benefit of anatomic tilt radiographs for dorsal plating of the distal radius.4 Our findings that the PA and 11° PA views were highly sensitive for intra-articular hardware and that 22° lateral views were more reliable than standard lateral images agree with their findings. The overall sensitivities among image types in our study were less than the previous study. Differences in methodology that may account for the discrepancy include the use of volar versus dorsal plates, fluoroscopic images versus cassette radiographs, and the individual surgeons who evaluated the images. Additionally, the study by Boyer et al did not specify the depth of joint penetration which may have been greater than the 1-3mm in this study thereby allowing greater ease in identification of intra-articular hardware.
Using a single cadaveric distal radius fixed with a volar locked plate, Soong et al evaluated multiple radiographic projections in an attempt to visualize intra-articular screw placement.1 They concluded that only an 11° PA view correctly showed all screws to be extra-articular. Our study had similar sensitivity for the standard and 11° PA images. This could be due to the specific volar locking plate applied in our study. Of the many volar plates commercially available, the Acumed (Acu-Loc, Hillsboro, OR) plate has a distal row of screws that are placed largely perpendicular to the plate with minimal distal angulation. Therefore, even the standard PA view produced an effective profile of these screws. When screws are directed more distal-dorsal it is expected that the 11° PA image would be of greater benefit as the dorsal screw ends otherwise superimpose on the mid-portion of the concave distal radius articular surface. Soong et al also noted an inability to achieve a single tilt lateral view that profiled the entire joint surface and suggested rotational fluoroscopy as a solution.1 To this end, the fact that we standardized our tilt lateral image to be 22° as opposed to a variable degree based on each specimen likely results in less optimal accuracy and sensitivity for this view in our study.
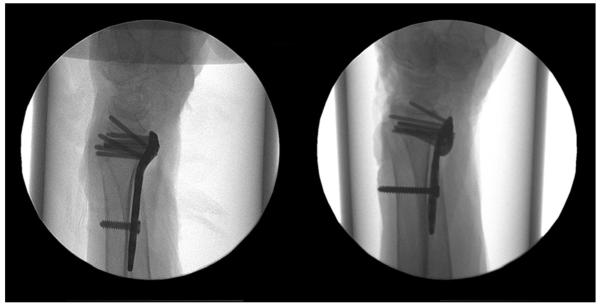
The low sensitivity (63%), or ability to detect screws that were penetrating the radiocarpal joint, on the 22° lateral view was unexpected. This view is felt to be well suited to detect such intra-articular hardware and has been a cornerstone of the authors’ radiographic evaluation during distal radius fracture fixation. We believe that this result is in part due to differences in how images were presented to blinded surgeons versus how that fluoroscopic projection is used clinically. Each surgeon was presented the image first in isolation without an orthogonal image and, perhaps more importantly, without any labeling of the image projection. Unblinded review of our images confirmed that each 22° lateral view profiled the radiocarpal joint surface and appeared well suited to accurately identify intra-articular hardware by the authors. However, without recognizing that the image was a 22° lateral projection, intra-articular hardware may appear similar to radial styloid screws on a standard lateral projection (Figure 6). Therefore, we believe that having labeled the images as tilt views would have improved the sensitivity of the 22° lateral view and that our data should not discourage surgeons from utilizing this projection in clinical practice.
Figure 6.
Comparison of lateral projection of extra-articular screws with a distally directed styloid screw (left) and 22° lateral projection with an intra-articular screw (right).
There are several limitations to this study. Only intact cadaveric distal radii were utilized. Fractures of the distal radius are often associated with decreased radial inclination, dorsal tilt, and intra-articular comminution which may render imaging of the articular surface less predictable. Second, only one of over 30 distal radius plates in production was studied.8 Each plate has a unique contour and configuration of distal screws. In addition, newly designed plates now feature variable-angle locking screws. While performing testing on every plate is beyond the scope of this study, we feel that the plate used in the study is representative of commonly used volar locking plates. Third, the tilt angles used in the study (11° PA and 22° lateral) are population averages which do not account for individual anatomic variability. Finally, our survey response rate was 47% which prohibit us from commenting on the clinical practice of the remaining 53% of the ASSH membership.
It should be noted that rotational fluoroscopy does expose the patient to greater radiation than static imaging. Thus, the risks and benefits of rotational imaging must be weighed even when considering the limited radiation delivered from current mini-C arm’s. In the authors’ experience, brief rotation of the wrist will often allow efficient imaging and identification of problematic hardware as, at times, multiple attempts at static imaging will fail to accurately profile the point of interest. We believe that the small amount of additional radiation is justified when it may prevent intra-articular screw placement.
Rather than indicating the superiority of a single fluoroscopic projection or movie, we believe our data supports the incorporation of several static images with fluoroscopy to minimize intra-articular screw placement during volar plate fixation. Our results indicate that even with a comprehensive radiographic evaluation, the ability to detect intra-articular hardware is imperfect. This likely explains the broad experience of survey responders indicating that they had encountered screws penetrating the radiocarpal joint. This data provides caution and encourages diligence on the part of surgeon performing volar plating in examining for intra-articular hardware. We should note that the high percentage of specimens with intra-articular screws, far exceeding that expected in clinical practice, limits our results to determining the sensitivity/specificity of each image’s interpretation as any positive or negative predictive values of image interpretation are affected by the increased prevalence of the complication.
Volar locked plating of distal radius fractures performed with fluoroscopic guidance continues to grow in popularity. This study demonstrates the difficulty of detecting intra-articular screw penetration radiographically. Clinically, several techniques beyond diligent review of radiographic images may serve to prevent against this complication. Some surgeons augment volar plating with an arthroscopic assessment of the joint surface.5, 9 Such an evaluation would be expected to reveal intra-articular screw placement although this requires addition time, expertise, and equipment. Additionally, screws can be placed slightly more proximal allowing for an increased degree of safety. More proximal hardware placement also represents a compromise as volar locked plates are designed to provide subchondral support which requires hardware to buttress the subchondral bone.8 The alternative utilized by one of the authors has been to drill and place distal screws unicortically which should prevent articular penetration and prominent dorsal hardware. The technique of unicortical hardware remains imperfect in the face of intra-articular fracture lines and dorsal comminution and likely has biomechanical effects that have yet to be defined. Finally, the simple clinical evaluation of ranging the operative wrist and rotating the forearm to assess for crepitus or catching that would suggest radiocarpal or radio-ulnar hardware penetration is employed by the authors.
Acknowledgement
The authors acknowledge the assistance of the Washington University School of Medicine Institute of Clinical and Translational Sciences for the statistical analysis performed. This analysis was made possible by the grant below.
“This publication was made possible by Grant Number UL1 RR024992 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH) and NIH Roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NCRR or NIH.“
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Matthew L. Tweet, Department of Orthopaedic Surgery University of Cincinnati College of Medicine 538 Oak Street Cincinnati, OH 45219.
Peter J. Stern, Department of Orthopaedic Surgery University of Cincinnati College of Medicine 538 Oak Street Cincinnati, OH 45219.
References
- 1.Soong M, Got C, Katarincic J, et al. Fluoroscopic evaluation of intra-articular screw placement during locked volar plating of the distal radius: a cadaveric study. J Hand Surg Am. 2008;33:1720–1723. doi: 10.1016/j.jhsa.2008.07.021. [DOI] [PubMed] [Google Scholar]
- 2.Schuind FA, Linscheid RL, An KN, et al. A normal data base of posteroanterior roentgenographic measurements of the wrist. J Bone Joint Surg Am. 1992;74:1418–1429. [PubMed] [Google Scholar]
- 3.Mann FA, Kang SW, Gilula LA. Normal palmar tilt: is dorsal tilting really normal? J Hand Surg Br. 1992;17:315–317. doi: 10.1016/0266-7681(92)90120-q. [DOI] [PubMed] [Google Scholar]
- 4.Boyer MI, Korcek KJ, Gelberman RH, et al. Anatomic tilt x-rays of the distal radius: an ex vivo analysis of surgical fixation. J Hand Surg Am. 2004;29:116–122. doi: 10.1016/j.jhsa.2003.09.004. [DOI] [PubMed] [Google Scholar]
- 5.Smith DW, Henry MH. The 45 degrees pronated oblique view for volar fixed-angle plating of distal radius fractures. J Hand Surg Am. 2004;29:703–706. doi: 10.1016/j.jhsa.2004.04.006. [DOI] [PubMed] [Google Scholar]
- 6.Lundy DW, Quisling SG, Lourie GM, et al. Tilted lateral radiographs in the evaluation of intra-articular distal radius fractures. J Hand Surg Am. 1999;24:249–256. doi: 10.1053/jhsu.1999.0249. [DOI] [PubMed] [Google Scholar]
- 7.Kumar D, Breakwell L, Deshmukh SC, et al. Tangential views of the articular surface of the distal radius-aid to open reduction and internal fixation of fractures. Injury. 2001;32:783–786. doi: 10.1016/s0020-1383(01)00155-3. [DOI] [PubMed] [Google Scholar]
- 8.Drobetz H, Bryant AL, Pokorny T, et al. Volar fixed-angle plating of distal radius extension fractures: influence of plate position on secondary loss of reduction--a biomechanic study in a cadaveric model. J Hand Surg Am. 2006;31:615–622. doi: 10.1016/j.jhsa.2006.01.011. [DOI] [PubMed] [Google Scholar]
- 9.Lutsky K, Boyer MI, Steffen JA, et al. Arthroscopic assessment of intra-articular distal radius fractures after open reduction and internal fixation from a volar approach. J Hand Surg Am. 2008;33:476–484. doi: 10.1016/j.jhsa.2007.12.009. [DOI] [PubMed] [Google Scholar]