Abstract
Nociceptors are sensory neurons that detect harmful, or potentially harmful, stimuli, and can become sensitized following injury or repetitive stimulation. When sensitized, nociceptors often exhibit activity in the absence of apparent or additional stimulation, called ongoing (or spontaneous) activity (OA). In this report, we provide evidence that OA in nociceptors can be caused by the stimuli typically used to identify and characterize the neuron, which must by definition be noxious and therefore potentially sensitizing. Such OA caused by the experimental methodology can confound interpretation. In our nerve inflammation model, OA can potentially arise from multiple sites, including the lesion site and the receptive field. We provide evidence that the OA rate recorded during these experiments may be related to the site and cause of OA generation. We suggest that there are two types of OA, characterized by their rates. Very slow rates of ongoing activity (<0.2 Hz) are likely to arise from the receptive field and may indicate sensitization during the experiment. Faster rates are likely to arise from the nerve trunk, i.e. the neuritis, or the neuronal cell body. Without appropriate methodological consideration, interpretations of results from such studies of nociceptor function may be methodologically confounded.
Keywords: Ongoing activity, electrophysiology, methodology, neuritis, pain, nociception
1. Introduction
Understanding the function of nociceptors is an ongoing challenge. There are many ways of studying nociceptors, but arguably the most powerful method is to record from the neurons directly. The most common technique used is extracellular recording from the peripheral nerve trunk, although some researchers, including the present authors, also record from the dorsal roots. Identified neurons can be stimulated electrically, and mechanical, thermal, and chemical response properties can be tested at the receptive field or nerve trunk for individually characterized neurons. Changes in these parameters (e.g. changes in mechanical threshold or the development of ongoing activity) are interpreted as sensitization, and may impact sensory perception. Indeed, studies of sensitization are critical to understanding the actions of many drugs and other compounds.
A key feature of nociceptors is that they develop ongoing activity (OA) when they, or the structures they innervate, are injured or inflamed (Bessou and Perl, 1969; Perl, 1976; Perl, Kumazawa et al., 1976). Because noxious and potentially injurious stimulation must be used to activate or access nociceptor receptive terminals, OA can develop even in control/untreated animals. Thus, studies often report OA as a property of some normal nociceptors (Bove and Light, 1995; Bove, Ransil et al., 2003; Strassman and Levy, 2006; Dilley and Bove, 2008). Certainly, OA in a sensory element that could lead to pain is not desirable under normal circumstances. Since persistent nociceptor OA maybe the basis for some cases of acute and chronic pain, understanding the details of this characteristic is important to all studies of pain and nociception.
There is a methodological conundrum in the electrophysiological approaches to studying nociceptors, especially when studying non-cutaneous neurons. To characterize a deep neuron, one must identify its receptive field, which involves noxiously mechanically stimulating peripheral structures. Each search does not lead to identification, and thus it is normal in these experiments to deliver repeated noxious stimuli to the same structures over the course of hours. We hypothesized that the cumulative stimulation throughout such experiments leads to sensitization of the neuron's receptive field, which is reflected as OA. Such OA could be expected to mask the effects of various interventions, and thus lead to false negative results. The present report will demonstrate this masking effect in a model of localized peripheral nerve inflammation (the neuritis model).
2. Methods
2.1. Animals and surgery
All experiments adhered to the guidelines of the Committee for Research and Ethical Issues of the International Association for the Study of Pain and the Principles of laboratory animal care (NIH publication No. 86-23, revised 1996), and were approved by the Animal Care and Use Committees of Beth Israel Deaconess Medical Center and University of Southern Maine.
The data presented combine both published and unpublished observations from two different recording models, the methods of which have been recently detailed (Dilley and Bove, 2008; Bove, 2009). Data were gathered from adult, male Wistar and female Long Evans rats (there have been no reports of differences in peripheral neuronal sensitivities between these strains). In both models, recordings were made from normal nerves, and also from nerves that had been locally inflamed with complete Freund's adjuvant (the neuritis model). The nerve inflammation was accomplished by incising the skin over the posterior thigh, and exposing the sciatic nerve using blunt dissection. A small strip of surgical gelatin foam (5 × 5 × 10mm) was soaked in complete Freund's adjuvant and placed loosely around the nerve, and the animal allowed to recover until the desired post-operative day.
2.2. Dorsal root recordings
Recordings were made from untreated (n=6) and neuritis animals, 1 (n=18), 4 (n=17) and 8 (n=14) weeks following surgery (details in Dilley and Bove, 2008). A lumbar laminectomy was performed from L2 to L5 to expose the contents of the spinal canal. The surrounding skin was used to form a pool that was filled with mineral oil. The dura mater was opened and the left L5 dorsal root was cut close to the dorsal root entry zone. The cut end of the root was positioned on a small black glass platform (10 mm × 6 mm) for recording. Bipolar stimulating electrodes were placed under the dorsal root, distal to the platform.
Recordings were made from fine filaments that were teased from the cut end of the dorsal root, using finely sharpened forceps. Filaments were split until single action potentials could be evoked using electrical stimulation of the dorsal root (square wave pulses: 0.5–0.9 ms duration and 30–40 V amplitude). Only filaments with clearly identifiable waveforms were studied.
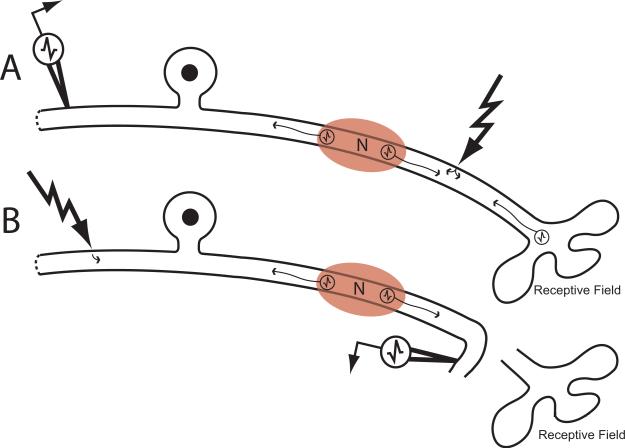
During dorsal root recordings, receptive fields (RF) for electrically isolated neurons with slowly conducting axons (<1.5m/s) within the sciatic nerve were searched for below the knee using intense mechanical stimuli (Fig. 1A). Neurons were only included for further study if they had mechanically sensitive RFs in the lower limb located distal to the exposed part of the sciatic nerve, i.e. the axons pass through the neuritis.
Figure 1.
Recording methods. A. Recordings were made from dorsal rootlets, with conduction velocities determined from electrical stimulation of the dorsal root and sciatic nerve (jagged arrow). In these experiments, noxious stimuli were applied to the innervated structures to locate the receptive fields (RF). Ongoing activity (OA) sources include the RF, the neuritis lesion (N), and the cell body. B. Recordings were made from filaments of the sural nerve, and confirmed as sensory units by electrical stimuli of the dorsal roots. The RFs in these experiments could not contribute to OA.
Critical for the present report, the time was recorded at which noxious stimulation of the periphery commenced, i.e. the time that the first neuron's receptive field was identified. Thereafter, the time that each subsequent neuron was recorded was also noted.
2.3. Peripheral nerve recordings
Recordings were made from untreated (n = 13) and neuritis animals 3–8 days following surgery (n = 12; details in Bove, 2009). The sciatic and sural nerves were carefully dissected from the ankle to the sciatic notch. The surrounding skin was used to form a pool that was filled with mineral oil. Recordings were made from fine filaments that were teased from the sural nerve. Following a lumbar laminectomy, another oil pool was formed over the lumbar spinal cord. The L4–L6 dorsal roots were cut close to the spinal cord and placed over bipolar stimulating electrodes.
During peripheral nerve recordings, sensory neurons with slowly conducting axons within the sciatic nerve were identified by electrically stimulating the dorsal roots while recording from the distal end of the cutaneous sural nerve (Fig. 1B). Therefore, axons were stimulated in an antidromic (opposite) direction. In these recordings, no RF could be determined, because they had been disconnected from the nerve. Consequently, there could be no sensitization due to RF stimuli.
2.4. Outcome measurements
In all experiments, ongoing activity was recorded for at least 2 minutes for each neuron. In the dorsal root model, there were three possible sources of OA: the receptive field, the neuritis lesion, and the neuronal cell body. In the peripheral nerve recording model, there were two potential sources of OA: the neuritis lesion and the neuronal cell body. Data were collected in raw form at 20 KHz for offline analysis using Spike 2 software (Cambridge Electronic Designs, UK).
2.5. Statistical analysis
All comparisons between frequency data were made using multiple Chi-Square tests or, when expected frequencies were less than 5, Fisher's exact tests. Paired comparisons were against the control group unless stated. When multiple comparisons were made, Bonferroni's correction was applied in assessing the significance (e.g. between control and neuritis groups, the level of significance was p = 0.017). Since the rates of ongoing activity were negatively skewed, a Kruskal-Wallis test was used to compare between all groups. Correlation coefficients were calculated between the time from first recording and the percentage of neurons exhibiting OA and also the time from first recording and the rate of OA.
3. Results
3.1. Changes in Leg Appearance
In the dorsal root recordings, the lower limb was repeatedly noxiously stimulated while searching for RFs. In these experiments, it took the experimenter between 11 and 15 minutes to locate the first mechanically sensitive RF, and 15–30 minutes to characterize the neuron and subsequently identify another neuron and its RF. This process resulted in visible swelling of the lower limb and foot, which increased over time.
3.2. Ongoing activity
3.2.1. Percentage of OA
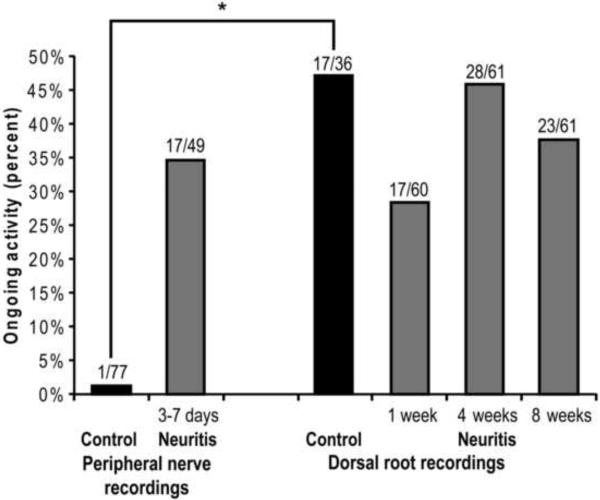
In both experimental setups (dorsal root and peripheral nerve recordings), OA was present in a number of neurons in each group (Fig. 2). In control peripheral nerve experiments the neurons were primarily silent, with only one of 77 neurons showing any OA. However, during neuritis, the percentage of neurons with OA increased significantly to 35% at 3–8 days (17/49; p = 0.001, Fisher Exact Test). In experiments recorded from the dorsal roots, there were no significant differences between control and neuritis groups at 1, 4, and 8 weeks (p = 0.16, Chi-Square 4 × 2 contingency table). However, 47% (17/36) of the neurons recorded from the dorsal root during control conditions exhibited OA, a significant difference compared to the OA incidence of the control peripheral nerve recordings (p<0.0001, Chi-Square).
Figure 2.
Percentage of neurons exhibiting OA under different recording conditions. There was negligible OA in control neurons when recorded without the contribution of the RF (peripheral nerve recordings), but 35% exhibited OA during neuritis (p<0.0001, Chi-square; all cutaneous neurons with intact RFs, black bars). There were no significant differences in the percentage of neurons with OA when recorded at the dorsal root, between any groups (gray bars).
3.2.2. Rates of OA
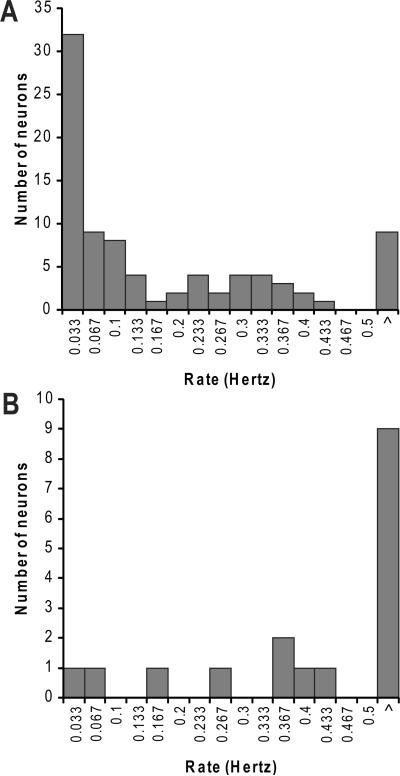
When the OA rates from the dorsal root recordings were compared, there were no significant differences between groups (untreated, 1, 4 and 8 weeks; p = 0.58, Kruskal-Wallis). There was also no change in the rates over time when all OA rates were pooled (r2 = 0.003; p = 0.6). Figure 3A shows the rates for all neurons recorded from the dorsal root. There appears to be a bimodality in the rates, with one population having very slow OA, apparently peaking at under 1 action potential per minute (0.033 Hz), and another population with a faster peak OA rate (~0.3 Hz). These two populations overlapped near 0.2 Hz. Only 11% of neurons with OA had rates >0.5 Hz.
Figure 3.
Ongoing activity rates of neurons recorded from the dorsal roots (A) and peripheral nerve (B).
In the peripheral nerve recordings (i.e. without the receptive field attached; Fig. 3B), rates of OA tended to be faster. Fifty three percent of neurons fired at rates >0.5 Hz. There were negligible neurons firing at 1 action potential per minute (0.033 Hz).
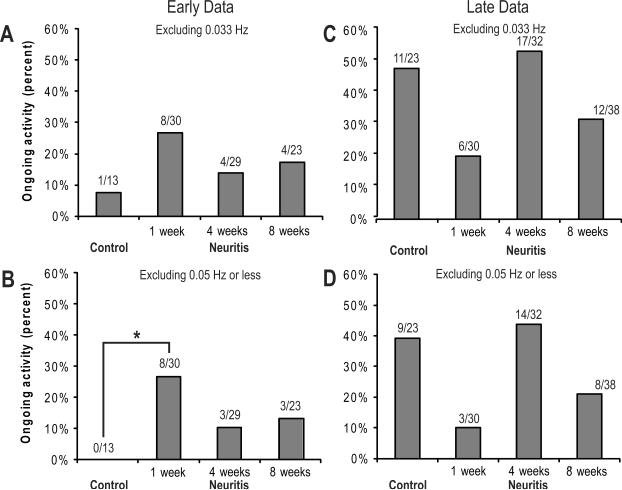
It is clear from the peripheral nerve recordings that the neuritis caused a significant increase in OA incidence from control recordings (Fig. 2). However, this effect was absent from the dorsal root recordings (Fig. 2). Because of this discrepancy, and the apparent bimodality in the rates from the dorsal root data (Fig. 3A), we hypothesized that the high proportion of neurons with very slow OA (which were absent from the peripheral nerve recordings) may be masking the true effect of the neuritis. We hypothesized that the very slow OA rates observed in the dorsal root recordings may have come from the RFs. When we separated the neurons based on whether they were recorded in the first hour (early; see 3.2.3, below), and thus had less inflammation due to RF stimulation, an effect of the neuritis became more clear (Fig. 4A and B), in that it is more consistent with the pattern of OA observed in the peripheral nerve recordings. In 4A, OA with rates of 0.033 Hz have been removed, and in 4B, OA with <0.05 Hz have been removed. In contrast, there is no clear effect seen when this analysis is performed on recordings performed one hour or longer into the recording session (late) in the experiment (Fig. 4C and D).
Figure 4.
The effect of neuritis on OA incidence over time, comparing neurons recorded within the first hour (early) to those recorded later in the experiment (late) neurons (see text) When neurons with the slower OA rates (A and C: <0.033 Hz; B and D:<0.5 Hz) are removed, a clear pattern develops for the early-recorded neurons (A, B), revealing that neuritis most likely causes ongoing activity peaking at 1 week and becoming less at 4 and 8 weeks. The data from the later-recorded units (C, D) do not fit any pattern, regardless of whether the very slowly discharging neurons are included. * p = 0.04, One-way Fisher exact test comparing control with one week neuritis.
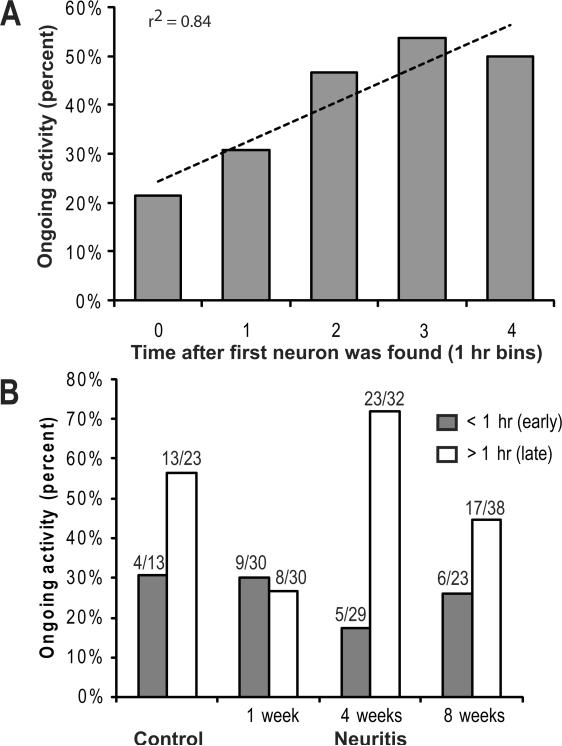
3.2.3. Time trends
To evaluate the possibility that OA incidence and/or rate were due to repeated RF searches, ongoing activity data for all dorsal root recordings (control and neuritis) were pooled and grouped by hour following the first recording. There was found to be a significant positive correlation between time after first recording and OA incidence (r2 = 0.84, p = 0.03; Fig. 5A). Because of this observation, we separated the data into neurons recorded within the first hour (early) and those recorded in later hours (late), and found the OA incidences to be significantly different (p = 0.0003, Chi-square). With the exception of the 1 week time point, there were more neurons with OA recorded late in each group (Fig. 5B).
Figure 5.
A. The percentage of neurons exhibiting OA increased with time after the localization of the first unit. These data are all from dorsal root recordings, from all time points, including control and 1, 4, and 8 weeks following the induction of sciatic neuritis. B. Percentage of neurons with OA, recorded at the dorsal root, separated by time during the experiment. More neurons exhibited OA later in the experiment.
4. Discussion
During inflammation, OA develops in skin, joint, and muscle nociceptors (Perl, Kumazawa, Lynn, and Kenins, 1976; Grigg, Schaible et al., 1986; Schaible, Schmidt et al., 1987; Berberich, Hoheisel et al., 1988; Cohen and Perl, 1988), and is an indicator of sensitization (Perl, Kumazawa et al., 1976). The present data demonstrate a methodological confound of characterizing nociceptors by their RF properties, especially when studying OA. To locate RFs, especially in deep tissues, the structures must be stimulated noxiously. Thus, when a slowly conducting neuron is isolated, the peripheral structures from the distal thigh to the toes are stimulated noxiously using fingers or forceps. However, if a mechanical receptive field is not found, another neuron is isolated, and the search repeated. This typically takes dozens of searches over the course of the recording sessions, which in these experiments were 4–7 hours long. In our experiments it was clear that the noxious mechanical stimulus necessary to identify the RFs was in itself sufficient to cause inflammation. Because there was no RF present in the peripheral nerve recordings, such inflammation was not present. Consistently, there was no OA during the control recordings. We conclude that the OA in the dorsal root recordings was at least in part due to sensitization from repeated noxious stimuli. The differences in OA rates and incidence from our previous publications describing effect of neuritis on axons (Bove, Ransil, Lin, and Leem, 2003; Dilley, Lynn et al., 2005; Dilley and Bove, 2008) are likely due to methodological artifacts.
The presence of OA in normal nociceptor neurons, especially from deep structures such as muscle has been contentious for a long time. In two of our (GB) earlier papers, where we studied putatively normal nociceptors from deep paraspinal structures and from cranial dura mater (Bove and Light, 1995; Bove and Moskowitz, 1997), OA was present in the majority of nociceptors, and in the latter paper, the OA rates were higher later in the experiment. In both papers, it was suggested that the OA was likely due to methodological factors. The incidence of OA in muscle nociceptors was also reported to be higher in later recordings (from 66% to 90%). These reports consistently demonstrate that the recording methods induce cause OA, and thus sensitization.
Our data from dorsal root recordings reveal two possible types of OA, very slow (peak rate ~0.33 Hz) and slow (peak rate 0.3 Hz). This was suggested both by the bimodality of the rates and because the removal of the very slow OA neurons showed a temporal relationship with inflammation-induced axonal mechanical sensitivity (Dilley and Bove, 2008). Although there were higher rates of OA in these recordings (>0.5 Hz), these only accounted for 11% of neurons with OA. Importantly, in our peripheral nerve recordings where the RF could not contribute to the OA, no neurons exhibited very slow OA. Collectively, these observations support that the very slow OA may come from the receptive field, while the faster rates of OA may come from the lesion.
There are few reports that include such slow OA rates. When recording from uninjured nociceptors following injury to neighboring axons (afferent or efferent) in the same nerve, very slow rates of OA have been reported. In one of the studies, the median discharge rate from uninjured nociceptors was 0.04 Hz following injury to neighboring afferent axons (Wu, Ringkamp et al., 2001). In another report, OA rates in uninjured nociceptors were 0.001 – 0.01 Hz following injury to neighboring efferent axons, and these rates were not different from sham-operated animals (Wu, Ringkamp et al., 2002). In another study, the median rate of OA in uninjured nociceptors was not given, but only 3% of neurons had rates ≥0.07 Hz, with the vast majority of these exhibiting OA ≤0.02 Hz (Ali, Ringkamp et al., 1999). In each of these studies, sensitizing stimulation to the RF was avoided. When neighboring afferent axons were injured, the median OA rate was <0.02 Hz, but when the axons were also locally inflamed, the median rate increased to 1.8 Hz (Djouhri, Koutsikou et al., 2006). In this study, potentially sensitizing stimuli of the RF were applied throughout the experiments. We also reported OA rates following an L4 lesion while recording from uninjured L5 nociceptors (Dilley and Bove, 2008). The median rate was 0.2 Hz, with 4 neurons below this rate and 10 above this rate. These data are all consistent with our hypothesis that OA may arise from the RF. However, the data are inconsistent with our hypothesis that the very slow OA is due to cumulative noxious stimuli to the RF, since three of the studies avoided mechanical stimulation of the RF.
An alternate and attractive hypothesis that would explain these disparate findings is that very slow OA may be due to cumulative antidromic discharge into the RF, resulting in neurogenic inflammation (NI). In all the experiments cited and reported presently, the nerves were repeatedly electrically stimulated at levels suprathreshold to evoke action potentials (see arrows, Fig. 1). This releases neuropeptides into the RF, leading to NI (Jancso, Janscó-Gábor et al., 1967; Kenins, 1981; Kenins, Hurley et al., 1984). It could be that NI is responsible for the very slow OA of nociceptors. Clinical studies have shown OA present in nociceptors during neuropathic pain (Campero, Serra et al., 1998), and have implicated NI as a probable mechanism of spontaneous pain at least in chronic regional pain syndromes (Birklein and Schmelz, 2008).
Ongoing activity in sensory elements could be expected to impact the sensory modality of that element. Thus, OA in nociceptors could be expected to lead to the sensation of pain. However, the discharge rate that is necessary to reach perception remains unclear, and definitive studies have not been performed. Using microneurography in humans, which is similar to the methods reported here, Konietzny et al., reported that electrically evoked nociceptor discharge rates as low at 0.5 Hz could evoke pain (Konietzny, Perl et al., 1981). Another human study reported that while nociceptor discharge under 0.2 Hz usually did not evoke pain, 0.4 Hz usually did (Van Hees and Gybels, 1981), consistent with a similar report (Van Hees and Gybels, 1972). These findings are in general consistent with our findings (Fig. 3). Although it thus remains unknown whether very slow levels of OA are significant for pain, any low rate will release neurotransmitters at their synapses in the spinal cord, which may be extensive due to the high degree of branching of primary afferent neurons to spinal cord neurons. Thus, very slow rate discharge from multiple neurons, even with RFs spatially remote from each other, could potentially lead to facilitation of the sensory system. Further inquiry is thus justified before dismissing the very slow rate OA as experimental artifact in studies of primary afferent nociceptors. Moreover, there are numerous potential sites on a sensory neuron where ongoing activity could develop. Determining the site responsible for the OA will inform interpretation, and may direct treatment. It is suggested that future experiments consider these factors in their analyses until we understand more about the nature of OA in nociceptors.
Acknowledgments
Financial support was provided by a grant to GMB by the Samueli Institute, and by National Institutes of Health Grant 5R01AR048925 (GMB) through the National Institute of Arthritis and Musculoskeletal and Skin Diseases and the National Center for Complementary and Alternative Medicine.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Reference List
- Ali Z, Ringkamp M, Hartke TV, Chien HF, Flavahan NA, Campbell JN, Meyer RA. Uninjured C-fiber nociceptors develop spontaneous activity and alpha- adrenergic sensitivity following L-6 spinal nerve ligation in monkey. J Neurophysiol. 1999;81:455–466. doi: 10.1152/jn.1999.81.2.455. [DOI] [PubMed] [Google Scholar]
- Berberich P, Hoheisel U, Mense S. Effects of a carrageenan-induced myositis on the discharge properties of group III and IV muscle receptors in the cat. J.Neurophysiol. 1988;59:1395–1409. doi: 10.1152/jn.1988.59.5.1395. [DOI] [PubMed] [Google Scholar]
- Bessou P, Perl ER. Response of cutaneous sensory units with unmyelinated fibers to noxious stimuli. J.Neurophysiol. 1969;32:1025–1043. doi: 10.1152/jn.1969.32.6.1025. [DOI] [PubMed] [Google Scholar]
- Birklein F, Schmelz M. Neuropeptides, neurogenic inflammation and complex regional pain syndrome (CRPS) Neurosci.Lett. 2008;437:199–202. doi: 10.1016/j.neulet.2008.03.081. [DOI] [PubMed] [Google Scholar]
- Bove GM. Focal nerve inflammation induces neuronal signs consistent with symptoms of early complex regional pain syndromes. Exp.Neurol. 2009;219:223–227. doi: 10.1016/j.expneurol.2009.05.024. [DOI] [PubMed] [Google Scholar]
- Bove GM, Light AR. Unmyelinated nociceptors of rat paraspinal tissues. J.Neurophysiol. 1995;73:1752–1762. doi: 10.1152/jn.1995.73.5.1752. [DOI] [PubMed] [Google Scholar]
- Bove GM, Moskowitz MA. Primary afferent neurons innervating guinea pig dura. J.Neurophysiol. 1997;77:299–308. doi: 10.1152/jn.1997.77.1.299. [DOI] [PubMed] [Google Scholar]
- Bove GM, Ransil BJ, Lin H-C, Leem JG. Inflammation induces ectopic mechanical sensitivity in axons of nociceptors innervating deep tissues. J.Neurophysiol. 2003;90:1949–1955. doi: 10.1152/jn.00175.2003. [DOI] [PubMed] [Google Scholar]
- Campero M, Serra J, Marchettini P, Ochoa JL. Muscle Nerve. 1998;21:1661–1667. doi: 10.1002/(sici)1097-4598(199812)21:12<1661::aid-mus6>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- Cohen RH, Perl ER. Chemical factors in the sensitization of cutaneous nociceptors. Prog.Brain Res. 1988;74:201–206. doi: 10.1016/s0079-6123(08)63014-9. [DOI] [PubMed] [Google Scholar]
- Dilley A, Bove GM. Resolution of inflammation induced axonal mechanical sensitivity and conduction slowing in C-fiber nociceptors. J.Pain. 2008;9:185–192. doi: 10.1016/j.jpain.2007.10.012. [DOI] [PubMed] [Google Scholar]
- Dilley A, Lynn B, Pang SJ. Pressure and stretch mechanosensitivity of peripheral nerve fibres following local inflammation of the nerve trunk. Pain. 2005;117:462–472. doi: 10.1016/j.pain.2005.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Djouhri L, Koutsikou S, Fang X, McMullan S, Lawson SN. Spontaneous pain, both neuropathic and inflammatory, is related to frequency of spontaneous firing in intact C-fiber nociceptors. J.Neurosci. 2006;26:1281–1292. doi: 10.1523/JNEUROSCI.3388-05.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eliav E, Benoliel R, Herzberg U, Kalladka M, Tal M. The Role of IL-6 and IL-1beta in Painful Perineural Inflammatory Neuritis. Brain Behav.Immun. 2009;24:474–484. doi: 10.1016/j.bbi.2009.01.012. [DOI] [PubMed] [Google Scholar]
- Grigg P, Schaible HG, Schmidt RF. Mechanical sensitivity of group III and IV afferents from posterior articular nerve in normal and inflamed cat knee. J.Neurophysiol. 1986;55:635–643. doi: 10.1152/jn.1986.55.4.635. [DOI] [PubMed] [Google Scholar]
- Jancso N, Janscó-Gábor A, Szolcsányi J. Direct evidence for neurogenic inflammation and its prevention by denervation and by pretreatment with capsaicin. Br.J.Pharmacol.Chemother. 1967;31:138–151. doi: 10.1111/j.1476-5381.1967.tb01984.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenins P. Identification of the unmyelinated sensory nerves which evoke plasma extravasation in response to antidromic stimulation. Neurosci.Lett. 1981;25:137–141. doi: 10.1016/0304-3940(81)90321-9. [DOI] [PubMed] [Google Scholar]
- Kenins P, Hurley JV, Bell C. The role of substance P in the axon reflex in the rat. Br.J.Derm. 1984;111:551–559. doi: 10.1111/j.1365-2133.1984.tb06624.x. [DOI] [PubMed] [Google Scholar]
- Konietzny F, Perl ER, Trevino D, Light A, Hensel H. Sensory experiences in man evoked by intraneural electrical stimulation of intact cutaneous afferent fibers. Exp.Brain Res. 1981;42:219–222. doi: 10.1007/BF00236910. [DOI] [PubMed] [Google Scholar]
- Perl ER. Sensitization of nociceptors and its relation to sensation. In: Bonica JJ, Albe-Fessard D, editors. Advances in Pain Research and Therapy. Vol. 1. Raven Press; New York: 1976. pp. 17–28. [Google Scholar]
- Perl ER, Kumazawa T, Lynn B, Kenins P. Sensitization of high threshold receptors with unmyelinated (C) afferent fibers. Prog.Brain Res. 1976;43:263–277. doi: 10.1016/S0079-6123(08)64359-9. [DOI] [PubMed] [Google Scholar]
- Schaible HG, Schmidt RF, Willis WD. Convergent inputs from articular, cutaneous and muscle receptors onto ascending tract cells in the cat spinal cord. Exp.Brain Res. 1987;66:479–488. doi: 10.1007/BF00270680. [DOI] [PubMed] [Google Scholar]
- Strassman AM, Levy D. Response properties of dural nociceptors in relation to headache. J Neurophysiol. 2006;95:1298–1306. doi: 10.1152/jn.01293.2005. [DOI] [PubMed] [Google Scholar]
- Van Hees J, Gybels J. C nociceptor activity in human nerve following painful and non painful skin stimulation. J.Neurol.Neurosurg.Psychiat. 1981;44:600–607. doi: 10.1136/jnnp.44.7.600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Hees J, Gybels JM. Pain related to single afferent c fibers from human skin. Brain Research. 1972;48:397–400. doi: 10.1016/0006-8993(72)90198-9. [DOI] [PubMed] [Google Scholar]
- Wu G, Ringkamp M, Hartke TV, Murinson BB, Campbell JN, Griffin JW, Meyer RA. Early onset of spontaneous activity in uninjured C-fiber nociceptors after injury to neighboring nerve fibers. J.Neurosci. 2001;21:RC140. doi: 10.1523/JNEUROSCI.21-08-j0002.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu G, Ringkamp M, Murinson BB, Pogatzki EM, Hartke TV, Weerahandi HM, Campbell JN, Griffin JW, Meyer RA. Degeneration of myelinated efferent fibers induces spontaneous activity in uninjured C-fiber afferents. J.Neurosci. 2002;22:7746–7753. doi: 10.1523/JNEUROSCI.22-17-07746.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]