Abstract
Background
Previous studies have suggested that azithromycin improves lung function in lung transplant recipients with bronchiolitis obliterans syndrome (BOS). However, these studies did not include a non-treated BOS control cohort or perform survival analysis. This study was undertaken to estimate the effect of azithromycin treatment on survival in lung transplant recipients with BOS.
Methods
We conducted a retrospective cohort study of consecutive lung transplant recipients who developed BOS between 1999 and 2007. An association between azithromycin treatment and death was assessed using univariate and multivariable time-dependent Cox regression analysis.
Results
Of the 178 recipients that developed BOS in our study, 78 developed BOS after 2003 and were treated with azithromycin. The azithromycin treated and untreated cohorts had similar baseline characteristics. Univariate analysis demonstrated that azithromycin treatment was associated with a survival advantage and this beneficial treatment effect was more pronounced when treatment was initiated during BOS stage 1. Multivariable analysis demonstrated azithromycin treatment during BOS stage 1 (adjusted hazard ratio=0.23, p=0.01) and absolute FEV1 value at the time of BOS stage 1 (adjusted hazard ratio=0.52, p=0.003) were both associated with a decreased risk for death.
Conclusion
In lung transplant recipients with BOS stage 1, azithromycin treatment initiated before BOS stage 2 was independently associated with a significant reduction in the risk of death. This finding supports the need for a randomized controlled trial to confirm the impact of azithromycin on survival in lung transplant recipients.
Introduction
Lung transplantation is an important therapeutic option for patients with end stage lung diseases. Despite the benefits of transplantation, mortality rates for lung transplantation are the highest of any solid organ transplant reaching 50% at 5 years.[1, 2] Long-term survival is limited by a form of chronic allograft dysfunction, called bronchiolitis obliterative syndrome (BOS). BOS affects 40% of lung transplant recipients at five years and is the leading cause of death beyond the first year of transplantation.[1, 2] Thus far, no therapy has clearly proven effective in decreasing mortality in BOS patients.
Azithromycin has been proposed as a potential treatment for BOS. Azithromycin is a macrolide antibiotic that has anti-inflammatory, antimicrobial, and gastrointestinal pro-motility properties. It can inhibit IL-8 associated inflammation, suppress infections, and prevent gastroesophageal reflux, which have all been thought to contribute to BOS.[3] Based on beneficial effects in pan-bronchiolitis and cystic fibrosis, azithromycin was proposed as a treatment for BOS in lung transplant recipients.[4–7] Previous studies of azithromycin for treatment of BOS have suggested improvement in lung function. These studies, however, were limited by relatively small numbers of subjects, lacked a comparison cohort of BOS recipients that did not receive azithromycin, followed patients for only a short length of time, and contained no survival data.[7–12] We hypothesized that in recipients with BOS stage 1, treatment with azithromycin would improve survival.
Accordingly, we designed a retrospective cohort study of 297 consecutive lung transplant recipients over a 6-year period at Washington University School of Medicine/Barnes-Jewish Hospital (WUSM/BJH) to determine the effect of azithromycin therapy for BOS on survival. Subjects were censored at death or January 1, 2008, which allowed for up to 9 years of follow up. Azithromycin treated recipients were analyzed collectively and then separated into cohorts according to whether azithromycin was initiated prior to or after BOS stage 2. For survival analysis, we employed univariate and multivariable time-dependent Cox regression analysis with death as the primary endpoint.
Methods
Study Design
Institutional Review Board approval for this study was obtained prior to data acquisition. A retrospective review of medical records was conducted on consecutive adult patients (age ≥ 18 years) at Washington University School of Medicine/Barnes-Jewish Hospital who underwent lung transplantation between August 1, 1998 and June 30, 2004. Follow up data was accrued on all eligible recipients until death or through January 1, 2008. Demographic and clinical characteristics were obtained from medical records and computerized databases. Recipients were excluded from the study if they did not develop BOS stage 1, could not be assessed for BOS stage 1 (due to death within 90 days of their transplant or had insufficient pulmonary function testing due to chronic tracheostomy) or if they were treated with azithromycin chronically for an indication other than BOS, such as mycobacterial disease.
Standard Care of Lung Transplant Subjects and Diagnostic Definitions
Pre-transplant evaluation, surgical procedures, post-operative care, surveillance bronchoscopy regimen, and triple-drug immunosuppressive regimens did not change substantially throughout the study period and have been described previously.[13–16] Patients were maintained on triple-drug immunosuppression with a corticosteroid, a purine synthesis antagonist, and a calcineurin inhibitor. Medication doses were adjusted according to trough levels, and immunosuppression was gradually lowered at six months post-operatively in the absence of recent allograft rejection. Treatment for BOS may have included azithromycin and antithymocyte globulin, and for continued decline in lung function, photopheresis and total lymphoid irradiation were considered. Azithromycin start date was defined as the first date that azithromycin was prescribed for BOS. The initiation of azithromycin treatment for BOS was based on a study published in 2003 and thus all patients treated with azithromycin were started subsequent to this first published report. All patients included in the azithromycin treated cohort were started on the medication specifically for treatment of BOS without additional changes in their maintenance immunosuppression regimen. Treatment was initiated with 5 continuous days of azithromycin at 250 mg/day followed by 250 mg/day three times a week for body weight < 70 kg and 500 mg/day three times a week for body weight > 70 kg. Subjects were typically started on azithromycin for ongoing lung function decline. Therefore, Azithromycin during BOS 1 was defined as azithromycin treatment that started after BOS stage 1 but before BOS stage 2. Azithromycin Post-BOS 2 was defined as azithromycin treatment started after the onset of BOS stage 2. Recipients in the No Azithromycin Cohort predominantly developed BOS prior to 2003 and if a recipient was given only a 5-day course of azithromycin for an upper respiratory infection they were also included in the No Azithromycin Cohort. Primary graft dysfunction, acute allograft rejection, and BOS were diagnosed and graded using standard criteria.[17–19] The highest rejection grade (0–4) of acute vascular (A score) and lymphocytic bronchitis (B score) from all biopsies prior to the development of BOS stage 1 were used as the highest A score and highest B score respectively. Bronchoalveolar lavage (BAL) with cell counts were not done routinely during this study period. Donor organ ischemic time, cytomegalovirus (CMV) pneumonitis, community acquired respiratory viral (CARV) infections were identified as previously defined, and Pseudomonas and Mycobacterial organisms were identified in respiratory specimens by standard culture techniques.[13–15]
Statistical Analysis
For two or three group comparisons, we used the two-tailed independent Student’s t-test or ANOVA respectively for continuous variables and the chi-square or Fisher’s exact test for categorical variables. To identify unique risk factors for death following BOS stage 1, we used univariate and multivariable Cox proportional hazards models. A variable was included in the multivariable model if there were statistically different frequencies between the groups at baseline, if the variable was associated with death in the univariate model (p < 0.10), or if the variable was associated with death in previous reports. To avoid risk inflation, no more than one variable was made time-dependent in the multivariate model. For all tests, p < 0.05 was considered significant. The data was tabulated in Excel 2002 (Microsoft Corp., Redmond, WA) and analyzed using SPSS 13.0 (SPSS Inc., Chicago, IL).
Results
Cohort assembly and baseline comparison
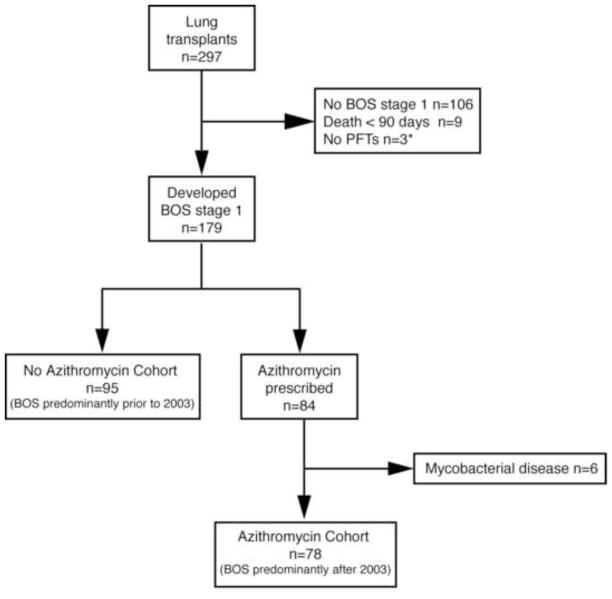
Of the 297 patients that received a lung transplant at WUSM/BJH between August 1, 1998 through June 30, 2004, 106 patients were excluded because they did not develop BOS stage 1 prior to January 1, 2008. During the follow-up period, 9 recipients were excluded due to death within 90 days of transplantation, and 3 were excluded because they did not have pulmonary function testing due to chronic tracheostomy. In our study population of 179 lung transplant recipients with BOS stage 1 or greater, 95 patients who predominantly developed BOS prior to 2003 were not prescribed azithromycin (No Azithromycin cohort) and 84 patients were prescribed azithromycin. Six of the 84 azithromycin treated patients were excluded because the indication for treatment was mycobacterial disease instead of BOS, leaving 78 patients who predominantly developed BOS after 2003 in the azithromycin treated group (Azithromycin cohort) (Figure 1).
Figure 1. Flowchart of lung transplant recipients with BOS treated with azithromycin.
Between August 1 1998 and June 30, 2004, 297 patients underwent lung transplantation. During our follow-up through January 1, 2008, BOS stage 1 developed in 179. Of these 179 recipients, 95 who predominately developed BOS prior to 2003 were not prescribed azithromycin for treatment of BOS (No Azithromycin Cohort) and 78 who predominantly developed BOS after 2003 received azithromycin for treatment of BOS (Azithromycin Cohort).
Comparison of the demographic and clinical characteristics between the No Azithromycin and Azithromycin Cohorts are shown on Table 1. No significant differences were present in terms of baseline demographic characteristics, ischemic time, date of transplant, type of transplant, primary graft dysfunction, lymphocytic bronchitis score, post transplant infections, time from transplant to BOS stage 1, FEV1 at BOS stage 1 or spirometry tests made between transplant and BOS stage 1, The Azithromycin cohort had higher grades of acute vascular rejection and received more antithymocyte globulin treatment for BOS stage 1than the No Azithromycin cohort. Collectively, these data suggest that the No Azithromycin and Azithromycin cohorts were very similar at the time of transplantation but the Azithromycin cohort may have had more severe acute vascular rejection.
Table 1.
Characteristics of lung transplant recipients with BOS in the No Azithromycin and Azithromycin Cohorts
| No Azithromycin n = 95 | Azithromycin n = 78 | p* | |
|---|---|---|---|
| Female, n (%) | 47 (50) | 42 (54) | 0.57 |
| Age at Transplant, mean years ± SD | 51.6 ± 12.7 | 49.0 ± 12.8 | 0.18 |
| Underlying Disease, n (%) | 0.44 | ||
| COPD | 58 (61) | 39 (50) | |
| α1-AT | 11 (12) | 10 (13) | |
| Cystic Fibrosis | 13 (14) | 14 (18) | |
| Pulmonary Fibrosis | 9 (10) | 7 (9) | |
| Other | 4 (4) | 8 (10) | |
| Ischemic Time, mean minutes ± SD | 313 ± 68 | 321 ± 61 | 0.41 |
| Ischemic Time > 330 min | 38 (40) | 29 (37) | 0.71 |
| Date of transplant, mean date ± SD in years | 2/5/01 ± 1.65 | 6/24/01 ± 1.77 | 0.15 |
| Type of Transplant, n (%) | 1.00 | ||
| Bilateral | 91 (96) | 74 (95) | |
| Single | 4 (4) | 4 (5) | |
| PGD at T0, n (%) | 0.47 | ||
| 0 | 14 (15) | 13 (17) | |
| 1 | 39 (41) | 28 (36) | |
| 2 | 26 (27) | 17 (22) | |
| 3 | 16 (17) | 20 (26) | |
| Highest A score, n (%) | 0.03 | ||
| 0 | 22 (23) | 14 (18) | |
| 1 | 25 (26) | 12 (15) | |
| 2 | 40 (42) | 34 (44) | |
| 3 | 8 (8) | 18 (23) | |
| Highest B score, n (%) | 0.16 | ||
| 0 | 30 (32) | 16 (21) | |
| 1 | 47 (50) | 37 (47) | |
| 2 | 16 (17) | 21 (27) | |
| 3 | 2 (2) | 4 (5) | |
| Pseudomonas culture positive, n (%) | 23 (24) | 27 (35) | 0.13 |
| CMV Pneumonitis, n (%) | 51 (54) | 31 (40) | 0.07 |
| CARV, n (%) | 13 (14) | 15 (19) | 0.32 |
| Time transplant to BOS stage 1, days ± SD | 813 ± 669 | 987 ± 705 | 0.10 |
| FEV1 at BOS stage 1, mean liters ± SD | 2.11 ± 0.79 | 2.22 ± 0.63 | 0.33 |
| Number of FEV1 measurements prior to BOS stage 1 | 25.11 ± 15.22 | 26.67 ± 13.31 | 0.51 |
| Antithymocyte globulin for BOS stage 1, n (%) † | 46 (52) | 61 (78) | <0.001 |
| Time BOS stage 1 to death/censoring, mean years ± SD | 2.29 ± 1.83 | 3.26 ± 1.94 | 0.001 |
Definition of abbreviations: α1-AT = alpha1 antitrypsin deficiency; BOS = bronchiolitis obliterans syndrome; CARV = community-acquired respiratory virus; CMV = cytomegalovirus; COPD = chronic obstructive pulmonary disease; FEV1 = forced expiratory volume in one second; Highest A score = highest acute vascular rejection score; Highest B score = highest lymphocytic bronchitis score; PGD = primary graft dysfunction; SD = standard deviation.
Chi-squared or Fisher’s exact test for categorical variables and independent groups t-test for continuous variables.
represents 89 recipients in No Azithro cohort.
Azithromycin treatment during BOS stage 1 is associated with decreased risk of death
The time between the diagnosis of BOS stage 1 and the initiation of azithromycin treatment for BOS varied from the day of BOS stage 1 diagnosis to after the onset of BOS stage 2. Therefore, we performed survival analysis using Cox regression with azithromycin treatment as a time dependent variable. Compared to the No Azithromycin Cohort, the Azithromycin cohort did not demonstrate a survival benefit, however, for those started on azithromycin after BOS stage 1 but prior to the development of BOS stage 2 (Azithromycin during BOS 1 cohort, N=31) there was a significant decrease in the risk of death (unadjusted hazard ratio [HR] = 0.29, 95% confidence interval [CI], 0.11 – 0.82, p = 0.02) (Table 2). In contrast, compared to the No Azithromycin cohort, there was no difference in the risk of death for those started on azithromycin after BOS stage 2 (Azithromycin Post-BOS 2, N=47) (unadjusted HR = 1.54, 95% CI, 0.91 – 2.61, p = 0.11)
Table 2.
Univariate Cox regression for progression of BOS stage 1 to death
| Variable | Death |
|
|---|---|---|
| Hazard Ratio (95% CI) | p | |
| Time Dependent | ||
| No Azithromycin | 1.00 | |
| Azithromycin (total group) | 1.08 (0.66–1.74) | 0.78 |
| Azithromycin during BOS 1 | 0.29 (0.11–0.82) | 0.02 |
| Azithromycin Post-BOS 2 | 1.54 (0.91–2.61) | 0.11 |
| Time Independent* | ||
| Female | 1.28 (0.79–2.10) | 0.32 |
| Age at transplant (per year) | 1.00 (0.98–1.02) | 0.65 |
| Underlying Disease | 0.51 | |
| COPD | 1.00 | |
| α1-AT | 1.65 (0.82–3.35) | |
| Cystic Fibrosis | 1.56 (0.77–3.14) | |
| Pulmonary Fibrosis | 1.11 (0.43–2.84) | |
| Other | 0.76 (0.18–3.15) | |
| Ischemic Time (per min) | 1.00 (1.00–1.01) | 0.26 |
| Ischemic Time > 330 min | 1.41 (0.86–2.30) | 0.17 |
| Date of transplant, (per day) | 1.00 (1.00-1.00) | 0.64 |
| Type of Transplant | 0.87 | |
| Bilateral | 1.00 | |
| Single | 1.09 (0.40–3.01) | |
| PGD at T0 | 0.052 | |
| 0 | 1.00 | |
| 1 | 1.74 (0.71–4.21) | |
| 2 | 1.95 (0.78–4.93) | |
| 3 | 3.57 (1.35–9.41) | |
| Highest A score | 0.74 | |
| 0 | 1.00 | |
| 1 | 1.48 (0.71–3.08) | |
| 2 | 1.14 (0.58–2.26) | |
| 3 | 1.23 (0.48–3.14) | |
| Highest B score | 0.99 | |
| 0 | 1.00 | |
| 1 | 1.03 (0.58–1.86) | |
| 2 | 1.09 (0.54–2.20) | |
| 3 | 1.17 (0.27–5.09) | |
| Pseudomonas culture positive | 1.74 (1.04–2.93) | 0.04 |
| CMV pneumonia | 1.03 (0.63–1.68) | 0.92 |
| CARV infection | 1.10 (0.60–2.03) | 0.76 |
| FEV1 at BOS stage 1 (per liter) | 0.47 (0.33–0.66) | <0.001 |
| Antithymocyte globulin for BOS stage 1 | 0.82 (0.49–1.38) | 0.46 |
Time independent analysis included No Azithro (n=95) and Early Azithro (n=31) cohorts
Definition of abbreviations: see Table 1
To determine if other demographic and clinical characteristics were risk factors for death in the No Azithromycin and Azithromycin during BOS 1 cohort, we performed additional univariate and multivariable Cox regression analysis. In the univariate models, the FEV1 at BOS stage 1 (HR = 0.47, 95% CI, 0.33 – 0.66, p = <0.001) and history of Pseudomonas cultured in respiratory specimens (HR = 1.74, 95% CI, 1.04 – 2.93, p = 0.04) were associated with a higher risk of death. Primary graft dysfunction demonstrated a trend toward an increased risk of death (p = 0.052), whereas all other demographic and clinical characteristics did not (p > 0.10) (Table 2).
To investigate if azithromycin treatment was associated with a significant decrease in risk of death independent of other variables, we performed multivariable Cox regression analysis. Variables were included in the multivariable model if there were statistically different frequencies between groups at baseline, if the variable was associated with death in the univariate model (p < 0.10), or if the variable associated with death in a previous report. To avoid risk inflation, no more than one variable was made time-dependent in the multivariate model. Azithromycin treatment, highest A score, CMV pneumonitis, CARV infection, antithymocyte globulin treatment, PGD score, Pseudomonas culture positive, FEV1 at BOS stage 1 and type of operation were entered into the model. Treatment with azithromycin (adjusted HR = 0.30, 95% CI 0.10 – 0.88, p = 0.03) and FEV1 at BOS stage 1 (adjusted HR = 0.53, 95% CI 0.35 – 0.81, p = 0.003) were associated with a significant decrease in the risk of death. Pseudomonas culture positive (adjusted HR = 1.96, 95% CI 1.06 – 3.60, p = 0.03) demonstrated a significant association with an increased risk of death (Table 3). All other variables failed to demonstrate a significant association with survival. Collectively, these data show that in lung transplant recipients with BOS stage 1, azithromycin treatment initiated prior to the onset of BOS stage 2 decreased the risk of death independent of other clinical characteristics.
Table 3.
Multivariable Cox regression for progression of BOS stage 1 to death*
| Variable | Death |
|
|---|---|---|
| Hazard Ratio (95% CI) | p | |
| Azithromycin treatment† | 0.30 (0.10–0.88) | 0.03 |
| FEV1 at BOS stage 1 | 0.53 (0.35–0.81) | 0.003 |
| Pseudomonas culture positive | 1.96 (1.06–3.60) | 0.03 |
variables tested in Cox proportional hazards model included: azithromycin treatment, highest A score, CMV pneumonitis, CARV infection, antithymocyte globulin treatment, PGD score, Pseudomonas culture positive, FEV1 at BOS stage 1, and type of operation.
time-dependent variable
Discussion
In this study, azithromycin treatment was associated with improved survival when analyzed as a time dependent variable. This mortality benefit remained present even after adjusting for type of transplant, acute rejection scores, CARV infections, a history of Pseudomonas in respiratory specimens, absolute FEV1 at BOS stage 1, and antithymocyte globulin treatment of BOS stage 1. Additionally, our data suggest that initiation of azithromycin for BOS should begin prior to the progression to BOS stage 2. Lastly, in the process of analyzing additional covariates, we demonstrated that FEV1 at the time of BOS stage 1 is strongly associated with the subsequent risk of death.
In the context of previous studies of azithromycin for lung transplant recipients with BOS, an improvement in lung function was identified in some but not all recipients.[7–12] The proportion of recipients with improved lung function ranged from 18 to 83%, and a recent study of 81 recipients with BOS stage 0p or greater demonstrated that 24 (30%) responded to azithromycin treatment with improved lung function and responders showed improved survival over non-responders.[11] In this study responders were defined as having a greater than 10% increase in FEV1 after 6 months after azithromycin. Using this definition, we had a similar number of azithromycin responders (36%), however we did not demonstrate a difference in survival between responders and non-responders. We did note that both our azithromycin responder and non-responder cohorts had a significantly higher survival compared to the No Azithromycin cohort. Accordingly, our work corroborates and extends the previous observations as we identified a survival advantage only in the recipients that were started on azithromycin during BOS stage 1 Since previous studies did not compare outcomes between recipients started on azithromycin to those never treated with azithromycin, it is difficult to make direct comparisons to the literature regarding the magnitude of our treatment effect.
In addition to identifying a beneficial association between azithromycin treatment for BOS during BOS stage 1 and survival, we also identified a decreased risk of death with FEV1 at BOS stage 1 and an increased risk of death with a history of being Pseudomonas culture positive. The association between FEV1 at time of BOS stage 1 and increased risk of death is not unexpected, however, the natural course of FEV1 progression after onset of BOS is believed to vary among patients and over time. Accordingly, results of future studies should account for this variable and analyzing factors that influence the relationship between FEV1 at BOS stage 1 and survival would be worthy of future analysis.[20, 21]
The mechanisms responsible for the benefit of azithromycin were not addressed in this study and remain unclear. Anti-inflammatory, antimicrobial, pharmacologic or gastrointestinal promotility mechanisms have all been suggested. Increased interleukin-8 (IL-8) and airway neutrophilia have been observed in the setting of BOS in some studies.[22–25] Macrolides have been reported to decrease IL-8 production in the nasal passageways of patients with polyps and in the sputum of patients with COPD, and in BOS recipients, responders to azithromycin treatment have been shown to have higher pre-treatment BAL neutrophilia and IL-8 expression.[9, 26, 27] Unfortunately, we did not have BAL data on these recipients to analyze neutrophilia or IL-8 expression. Chronic macrolide therapy has also been shown to suppress important pathogens such as Pseudomonas aeruginosa, which often colonizes the airways of patients with chronic airways disease.[28] Macrolides have been described to increased levels of certain immunosuppressive medications including cyclosporine, which may contribute to its beneficial effect on BOS.[29] Patients in our study on cyclosporine or tacrolimus did routinely have levels monitored to ensure they remained in normal range. We do not have data to directly address what the effect of azithromycin was on these drug levels in our cohorts, however, a previous study using azithromycin in lung transplant recipients did not show that azithromycin dramatically changed cyclosporine or tacrolimus levels.[7] Finally, gastroesophageal reflux and possibly chronic aspiration have been shown to be risk factors for developing BOS.[30–32] Macrolides may exert their beneficial effects through their known promotility properties by decreasing or preventing recurrent allograft injury due to chronic aspiration. Accurate data on reflux symptoms and treatment was not available. Additional studies will be required to further define the precise biochemical mechanisms responsible for the beneficial effects of azithromycin treatment.
As with any retrospective study, there are inherent limitations to the study design that may introduce bias. To avoid potential bias due to small sample size or limited follow-up time, we analyzed a large cohort of consecutive lung transplant recipients that developed BOS stage 1 over 6 years (n = 173) and censored all patients at death or at January 1, 2008 allowing for up to 9 years of follow up. We excluded patients that did not develop BOS stage 1 and 6 patients who received azithromycin treatment for mycobacterial disease so our results cannot be generalized to these recipients. Our results may be biased if there were improvements in survival throughout the study period that may have resulted in an era effect, however, transplant date was not associated with an improved survival in the univariate analysis. Recently adjunctive therapies for BOS beyond azithromycin have been used more frequently and include antithymocyte globulin, photopheresis and total lymphoid irradiation. Since photophoresis and total lymphoid irradiation are reserved for those recipients with progressive declines in lung function (i.e., as salvage treatments) we did not include them in our analysis. Antithymocyte globulin was included in our multivariable analysis and this adjunctive therapy did not negate the beneficial effect of azithromycin treatment. Finally, the small sample sizes could have over inflated the hazard ratio for risk of death. However, we made no more than one variable time dependent and our final multivariable model maintained an acceptable ratio of outcome events per independent variables. Although conducted in a retrospective fashion, we believe the results of this longitudinal study support a role for the use of azithromycin in the treatment of BOS.
In conclusion, our data suggest that azithromycin therapy may improve survival in lung transplant recipients who develop BOS. These data show an important potential advantage for the use of azithromycin when initiated after the onset of BOS stage 1 and prior to BOS stage 2 and support the need for a randomized controlled trial with long-term follow up to fully address the impact of azithromycin on survival in lung transplant recipients with BOS.
Acknowledgments
Funding: Funding by NIH/NHLBI T32 HL007317 and R01HL083894
The authors thank M. Gibson for help with data collection and J. Fassler, T. Francescon, C. Miller, W. Panus, L. Roldan, S. Rupp, and M. Scavuzzo for assistance in chart reviews.
Footnotes
Conflict of Interest Statement
No authors involved in the preparation of this manuscript have any financial relationships with industry or other agencies related to azithromycin or other macrolide antibiotics.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Trulock EP, Christie JD, Edwards LB, et al. Registry of the International Society for Heart and Lung Transplantation: twenty-fourth official adult lung and heart-lung transplantation report-2007. J Heart Lung Transplant. 2007;26:782–95. doi: 10.1016/j.healun.2007.06.003. [DOI] [PubMed] [Google Scholar]
- 2.Christie JD, Carby M, Bag R, et al. Registry of the International Society for Heart and Lung Transplantation: twenty-fifth official adult lung and heart/lung transplantation report--2008. J Heart Lung Transplant. 2008;27:957–69. doi: 10.1016/j.healun.2008.07.018. [DOI] [PubMed] [Google Scholar]
- 3.Williams TJ, Verleden GM. Azithromycin: a plea for multicenter randomized studies in lung transplantation. Am J Respir Crit Care Med. 2005;172:657–9. doi: 10.1164/rccm.2506011. [DOI] [PubMed] [Google Scholar]
- 4.Fujii T, Kadota J, Kawakami K, et al. Long term effect of erythromycin therapy in patients with chronic Pseudomonas aeruginosa infection. Thorax. 1995;50:1246–52. doi: 10.1136/thx.50.12.1246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kudoh S, Azuma A, Yamamoto M, et al. Improvement of survival in patients with diffuse panbronchiolitis treated with low-dose erythromycin. Am J Respir Crit Care Med. 1998;157:1829–32. doi: 10.1164/ajrccm.157.6.9710075. [DOI] [PubMed] [Google Scholar]
- 6.Jaffe A, Francis J, Rosenthal M, et al. Long-term azithromycin may improve lung function in children with cystic fibrosis. Lancet. 1998;351:420. doi: 10.1016/S0140-6736(05)78360-4. [DOI] [PubMed] [Google Scholar]
- 7.Gerhardt SG, McDyer JF, Girgis RE, et al. Maintenance azithromycin therapy for bronchiolitis obliterans syndrome: results of a pilot study. Am J Respir Crit Care Med. 2003;168:121–5. doi: 10.1164/rccm.200212-1424BC. [DOI] [PubMed] [Google Scholar]
- 8.Verleden GM, Dupont LJ. Azithromycin therapy for patients with bronchiolitis obliterans syndrome after lung transplantation. Transplantation. 2004;77:1465–7. doi: 10.1097/01.tp.0000122412.80864.43. [DOI] [PubMed] [Google Scholar]
- 9.Verleden GM, Vanaudenaerde BM, Dupont LJ, et al. Azithromycin reduces airway neutrophilia and interleukin-8 in patients with bronchiolitis obliterans syndrome. Am J Respir Crit Care Med. 2006;174:566–70. doi: 10.1164/rccm.200601-071OC. [DOI] [PubMed] [Google Scholar]
- 10.Yates B, Murphy DM, Forrest IA, et al. Azithromycin reverses airflow obstruction in established bronchiolitis obliterans syndrome. Am J Respir Crit Care Med. 2005;172:772–5. doi: 10.1164/rccm.200411-1537OC. [DOI] [PubMed] [Google Scholar]
- 11.Gottlieb J, Szangolies J, Koehnlein T, et al. Long-term azithromycin for bronchiolitis obliterans syndrome after lung transplantation. Transplantation. 2008;85:36–41. doi: 10.1097/01.tp.0000295981.84633.bc. [DOI] [PubMed] [Google Scholar]
- 12.Shitrit D, Bendayan D, Gidon S, et al. Long-term azithromycin use for treatment of bronchiolitis obliterans syndrome in lung transplant recipients. J Heart Lung Transplant. 2005;24:1440–3. doi: 10.1016/j.healun.2004.08.006. [DOI] [PubMed] [Google Scholar]
- 13.Khalifah AP, Hachem RR, Chakinala MM, et al. Respiratory viral infections are a distinct risk for bronchiolitis obliterans syndrome and death. Am J Respir Crit Care Med. 2004;170:181–7. doi: 10.1164/rccm.200310-1359OC. [DOI] [PubMed] [Google Scholar]
- 14.Khalifah AP, Hachem RR, Chakinala MM, et al. Minimal acute rejection after lung transplantation: a risk for bronchiolitis obliterans syndrome. Am J Transplant. 2005;5:2022–30. doi: 10.1111/j.1600-6143.2005.00953.x. [DOI] [PubMed] [Google Scholar]
- 15.Hachem RR, Khalifah AP, Chakinala MM, et al. The significance of a single episode of minimal acute rejection after lung transplantation. Transplantation. 2005;80:1406–13. doi: 10.1097/01.tp.0000181161.60638.fa. [DOI] [PubMed] [Google Scholar]
- 16.Mikols CL, Yan L, Norris JY, et al. IL-12 p80 is an innate epithelial cell effector that mediates chronic allograft dysfunction. Am J Respir Crit Care Med. 2006;174:461–70. doi: 10.1164/rccm.200512-1886OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yousem SA, Berry GJ, Cagle PT, et al. Revision of the 1990 working formulation for the classification of pulmonary allograft rejection: Lung Rejection Study Group. J Heart Lung Transplant. 1996;15:1–15. [PubMed] [Google Scholar]
- 18.Estenne M, Maurer JR, Boehler A, et al. Bronchiolitis obliterans syndrome 2001: an update of the diagnostic criteria. J Heart Lung Transplant. 2002;21:297–310. doi: 10.1016/s1053-2498(02)00398-4. [DOI] [PubMed] [Google Scholar]
- 19.Christie JD, Carby M, Bag R, et al. Report of the ISHLT Working Group on Primary Lung Graft Dysfunction part II: definition. A consensus statement of the International Society for Heart and Lung Transplantation. J Heart Lung Transplant. 2005;24:1454–9. doi: 10.1016/j.healun.2004.11.049. [DOI] [PubMed] [Google Scholar]
- 20.Nathan SD, Ross DJ, Belman MJ, et al. Bronchiolitis obliterans in single-lung transplant recipients. Chest. 1995;107:967–72. doi: 10.1378/chest.107.4.967. [DOI] [PubMed] [Google Scholar]
- 21.Lama VN, Murray S, Lonigro RJ, et al. Course of FEV(1) after onset of bronchiolitis obliterans syndrome in lung transplant recipients. Am J Respir Crit Care Med. 2007;175:1192–8. doi: 10.1164/rccm.200609-1344OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.DiGiovine B, Lynch JP, 3rd, Martinez FJ, 3rd, et al. Bronchoalveolar lavage neutrophilia is associated with obliterative bronchiolitis after lung transplantation: role of IL-8. J Immunol. 1996;157:4194–202. [PubMed] [Google Scholar]
- 23.Zheng L, Walters EH, Ward C, et al. Airway neutrophilia in stable and bronchiolitis obliterans syndrome patients following lung transplantation. Thorax. 2000;55:53–9. doi: 10.1136/thorax.55.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Riise GC, Andersson BA, Kjellstrom C, et al. Persistent high BAL fluid granulocyte activation marker levels as early indicators of bronchiolitis obliterans after lung transplant. Eur Respir J. 1999;14:1123–30. doi: 10.1183/09031936.99.14511239. [DOI] [PubMed] [Google Scholar]
- 25.Elssner A, Jaumann F, Dobmann S, et al. Elevated levels of interleukin-8 and transforming growth factor-beta in bronchoalveolar lavage fluid from patients with bronchiolitis obliterans syndrome: proinflammatory role of bronchial epithelial cells. Munich Lung Transplant Group. Transplantation. 2000;70:362–7. doi: 10.1097/00007890-200007270-00022. [DOI] [PubMed] [Google Scholar]
- 26.Yamada T, Fujieda S, Mori S, et al. Macrolide treatment decreased the size of nasal polyps and IL-8 levels in nasal lavage. Am J Rhinol. 2000;14:143–8. doi: 10.2500/105065800782102717. [DOI] [PubMed] [Google Scholar]
- 27.Basyigit I, Yildiz F, Ozkara SK, et al. The effect of clarithromycin on inflammatory markers in chronic obstructive pulmonary disease: preliminary data. Ann Pharmacother. 2004;38:1400–5. doi: 10.1345/aph.1D634. [DOI] [PubMed] [Google Scholar]
- 28.Tateda K, Ishii Y, Matsumoto T, et al. Direct evidence for antipseudomonal activity of macrolides: exposure-dependent bactericidal activity and inhibition of protein synthesis by erythromycin, clarithromycin, and azithromycin. Antimicrob Agents Chemother. 1996;40:2271–5. doi: 10.1128/aac.40.10.2271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Page RL, 2nd, Ruscin JM, Fish D, et al. Possible interaction between intravenous azithromycin and oral cyclosporine. Pharmacotherapy. 2001;21:1436–43. doi: 10.1592/phco.21.17.1436.34434. [DOI] [PubMed] [Google Scholar]
- 30.Palmer SM, Miralles AP, Howell DN, et al. Gastroesophageal reflux as a reversible cause of allograft dysfunction after lung transplantation. Chest. 2000;118:1214–7. doi: 10.1378/chest.118.4.1214. [DOI] [PubMed] [Google Scholar]
- 31.Cantu E, 3rd, Appel JZ, 3rd, Hartwig MG, et al. J. Maxwell Chamberlain Memorial Paper. Early fundoplication prevents chronic allograft dysfunction in patients with gastroesophageal reflux disease. Ann Thorac Surg. 2004;78:1142–51. doi: 10.1016/j.athoracsur.2004.04.044. [DOI] [PubMed] [Google Scholar]
- 32.Davis RD, Jr, Lau CL, Eubanks S, et al. Improved lung allograft function after fundoplication in patients with gastroesophageal reflux disease undergoing lung transplantation. J Thorac Cardiovasc Surg. 2003;125:533–42. doi: 10.1067/mtc.2003.166. [DOI] [PubMed] [Google Scholar]