Abstract
Background
Most quality metrics focus on underuse of services, leaving unclear the factors associated with potential overuse.
Objective
To assess associations between physician and patient characteristics, and the rapidity and modality of imaging for uncomplicated low back pain (LBP)
Setting
Fee-for-service Medicare
Population
35,039 beneficiaries with acute LBP and treated by one of 4,567 primary care physicians (PCPs) responding to the 2000-2001 or 2004-2005 Community Tracking Study Physician Surveys.
Methods
We analyzed Medicare claims from 2000-2002 and 2004-2006. We modified a measure of inappropriate imaging developed by the National Committee on Quality Assurance. Without assessing appropriateness of imaging for specific cases, we characterized the rapidity (within 28 days, within 29-180 days, none within 180 days) and modality of imaging (CT/MRI, only radiograph, no imaging). We used ordered logit models to assess relationships between imaging and patient demographics, and physician/practice characteristics including exposure to financial incentives based on patient satisfaction, clinical quality, cost profiling, or productivity.
Results
28.8% of 35,039 beneficiaries with LBP were imaged within 28 days, and an additional 4.6% between 28-180 days. Among imaged patients, 88.2% had a radiograph, while 11.8% had CT/MRI as their initial study. White patients received higher levels of imaging than black patients or those of other races [29.7%, 24.8%, 18.9% (p<0.001) for imaging within 28 days and 10.8%, 9.1%, 7.2% (p<0.05) for CT/MRI, respectively]. Medicaid patients received less rapid or advanced imaging than other patients. Patients had more rapid imaging and advanced imaging if their PCP worked in large practices. Compared to no incentives, clinical quality-based incentives were associated with less advanced imaging (10.5% vs. 1.4% for within 28 days, respectively, p<0.001), while incentive combinations including satisfaction measures were associated with more rapid and advanced imaging. Results persisted in multivariate analyses, and when the outcome was redefined as the number of imaging studies performed.
Conclusions
Rapidity and modality of imaging for low back pain is associated with patient and physician characteristics but the directionality of associations with desirable care processes is opposite of associations for measures targeting underuse. Metrics that encompass overuse may suggest new areas of focus for quality improvement.
Keywords: financial incentives, performance measurement, imaging, low back pain
BACKGROUND
Insurers press for standardized measurement of physicians’ performance to broaden programs that link performance to financial incentives. Existing metrics focus on patient experience, relative costs for comparable conditions, and clinical quality. Yet the vast majority of currently available measures on clinical quality focus on the underuse of services.1 Few focus on overuse of services that might induce harm through complications from unnecessary follow-up testing or treatment,2 and/or that raise health care costs with little improvement in outcomes. Moreover, if patients tend to prefer more rather than fewer services, programs that only measure underuse but omit overuse may induce even more overuse of services.
Policymakers call for the development of overuse measures and their inclusion in performance measurement and incentive programs,3 yet little is known about the patterns of care that these measures would reveal. To help anticipate the effects of applying overuse measures, we investigate associations between characteristics of patients and their primary care physicians (PCPs), and the rapidity and modality of imaging those patients receive for uncomplicated acute low back pain (LBP). We focus on LBP as a prevalent condition4 for which imaging – particularly with advanced modalities – is rarely indicated, even for elderly patients.5,6,7
METHODS
Data Sources
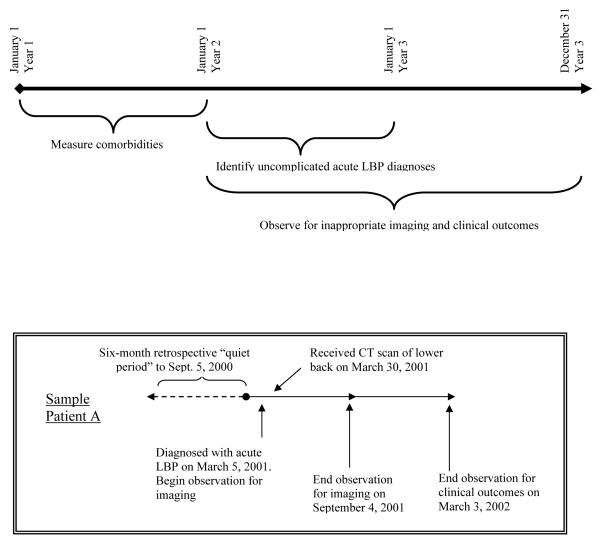
We analyzed claims data for Medicare fee-for-service beneficiaries treated by respondents to the 2000-2001 or 2004-2005 Community Tracking Study (CTS) Physician Surveys. Samples for these nationally representative surveys are clustered in 60 metropolitan statistical areas. Responses from 2000-2001 were linked to claims for years 2000-2002 while responses from 2004-2005 were linked to claims for years 2004-2006. Details on the survey and its linkage to Medicare claims are described elsewhere.8.9 Our analysis focuses on CTS primary care physicians (specialties of general internal medicine, general practice, family practice, internal medicine/pediatrics, geriatrics). The pooled dataset included information on 4,567 unique PCPs, and three years of claims for each beneficiary. (Figure 1)
Figure 1.
Study Design
Study Design
We used the first year of observation in each 3-year period to identify exclusion criteria and adjust for co-morbidities. Using the second year of observation, we identified beneficiaries as having an episode of acute low back pain if they had relevant diagnostic codes from an ambulatory or emergency department visit but lacked similar diagnostic codes within the six previous months. To assess imaging, we examined Medicare claims from inpatient, outpatient, and professional services files to detect radiologic studies of the lower back within 6 months of the incident LBP diagnosis. We derived diagnostic codes used to identify LBP, and procedure codes used to identify imaging procedures, from the measure of inappropriate imaging for LBP developed by the National Committee on Quality Assurance (NCQA).10
Responsible Physicians and Their Practices
Starting with the earlier round of the CTS survey, we used the Unique Physician Identification Number (UPIN) to identify the physician who billed for the greatest number of evaluation and management (E&M) visits during the entire observation period (January 1, 2000 thru June 30, 2002) for a given beneficiary. We similarly identified eligible PCPs from the later round of the survey using claims for years 2004-2006. We focused on beneficiaries whose “Plurality” physician was a CTS PCP. To assess the robustness of our results to methods of attribution, we conducted two separate analyses attributing beneficiaries who 1) had any evaluation and management visits with the CTS PCP during the observation period; and 2) had their initial LBP diagnosis coded by the CTS PCP. To identify whether the imaging study was conducted in the same organization in which the CTS PCP worked, we used the Tax Identification Number (TAXID) associated with each physician’s UPIN on claims.
Patient Population
Eligible patients were enrolled in Medicare for at least 6 months after the incident diagnosis of LBP. Thus, identified episodes of LBP occurred between January 1, 2001 and June 30, 2002 for the first cohort. For years 2000-2002, we included beneficiaries 65 years and older as of January 1, 2000 who were continuously enrolled in fee-for-service Medicare through the subsequent 18 months (until June 30, 2002), and did not enter hospice or nursing homes. We excluded those with end-stage renal disease or who received care in more than one state during 2000. This procedure was repeated for the next CTS round linked to 2004-2006 Medicare claims. We excluded beneficiaries whose initial LBP diagnosis was coded by a radiologist because this may reflect patient self-referrals.
To focus on cases of uncomplicated LBP, we used the NCQA definition10 to identify these episodes in claims. We applied additional, more stringent criteria to exclude patients who might have had a legitimate indication for imaging. Thus, patients whose claims indicated neurologic deficit, trauma, low impact injuries, cancer, infection, non-specific anemias, or constitutional symptoms suggestive of increased cancer risk were excluded. Detailed criteria for identifying patients with uncomplicated LBP are shown in Appendix A.
Outcome Measures
In primary analyses, we examined the rapidity and modality of imaging. We defined rapidity of imaging as an ordinal variable based on timing of the first imaging study – no imaging (none within 180 days of diagnosis), delayed (within 29-180 days), or rapid (within 28 days). Modality of imaging was defined as a separate ordinal variable – no imaging, radiograph only, or computed tomography/magnetic resonance imaging (CT/MRI). The “CT/MRI” category included patients who received radiographs and CT/MRI concurrently or serially. In secondary analyses, we considered the number of imaging studies performed within 180 days (none, one, more than one).
Patient Characteristics
We included patient sex; race (white, black, other – because data on other racial categories in Medicare data are not as reliable); and Medicaid eligibility, while adjusting for comorbidities.11,12 Drawing on data from the Area Resources File, we also adjusted for median household income in the beneficiary’s zip code; and the percent of adults 25 years and older in the county with 12 or more years of education, as aggregate measures of sociodemographic status.
Physicians’ Financial Incentives
We assessed the rapidity and modality of imaging relative to PCPs’ self-reported financial incentives including: 1) practice ownership (employed, part owner, full owner); 2) the overall effect of incentives, derived from responses to the question: “How would you describe your overall personal financial incentives in your practice? On balance, do these incentives favor reducing services to individual patients, favor expanding services to individual patients, or favor neither?” and 3) a composite 9-category variable constructed from a set of questions identifying factors on which physicians’ compensation was based (only his/her own productivity, only clinical quality measures, only patient satisfaction surveys, productivity and quality, productivity and satisfaction, quality and satisfaction, all three, none, and solo practice physicians who were not asked questions on incentives). We did not include in this composite responses about physicians’ exposure to incentives based on cost profiling because this variable was not associated with rapidity or modality of imaging in bivariate or multivariate analyses.
Other Physician/Practice Characteristics, and Area Factors
We considered the individual physician’s: specialty (family/general practice vs. general internal medicine); number of years in practice; board certification; and medical school site (U.S./Canada vs. elsewhere). Practice characteristics included: type (solo/2-person, small group of 3-10, medium group of 11-50, large groups of greater than 50, medical school, group/staff HMO, all other types); and the percent of practice revenues derived from Medicare, Medicaid, and capitation (each categorized as terciles). We adjusted for radiologist supply (number of patient-care radiologists per capita in the metropolitan statistical area), and urban vs. rural location.13 Finally, to control for unmeasured market factors, we included a dummy for each of the 60 metropolitan areas in the CTS sample.
Clinical Events
Using claims from the 6 month period subsequent to LBP diagnosis, we examined whether the rate of potential “cascade effects” of imaging and clinical conditions that might post hoc justify imaging that beneficiaries received as well as its rapidity. We considered: 1) hospitalization or surgery for LBP;14 2) complications or progression of LBP; and 3) new diagnoses of low back fractures or cancers with potential for bone metastases. (Appendix B).
Statistical Analyses
We performed ordered logit regressions with either the rapidity or modality of imaging as the dependent variable (referent = no imaging). To assess whether associations between the CTS PCP’s characteristics and imaging were influenced by care delivered by other physicians, we repeated analyses excluding beneficiaries who had visits with physicians other than the CTS PCP between the date of LBP diagnosis, and that of imaging (or within 6 months for beneficiaries who did not receive imaging). To account for secular trends, we also evaluated the interaction between each performance incentive variable, and the time period of the survey (2000-2002 or 2004-2006).
Analyses were conducted using SUDAAN, which accounts for clustering of patients within physicians and multiple observations of physicians responding to both survey rounds.15 We applied weights to reflect the probability of sampling and known differences between respondents and non-respondents. Weighted estimates are representative of non-federal PCPs providing patient care at least 20 hours per week in the continental U.S., and the Medicare beneficiaries that they treat.
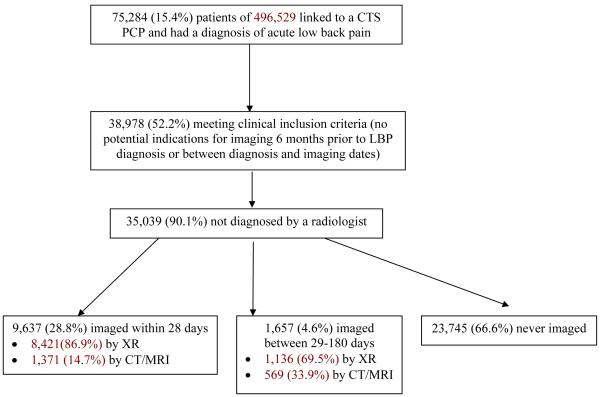
RESULT
Of 496,529 beneficiaries who met inclusion criteria and had a CTS PCP, 35,039 had a diagnosis of uncomplicated acute low back pain during the six-month assessment period. (Figure 2) Among these beneficiaries, 11,294 (32.2%) had at least one imaging study within 180 days of diagnosis. Twenty-nine percent (9,637) were imaged within 28 days of diagnosis, and 4.6% (1,657) between 28-180 days. Among these imaged patients, 88.2% had a plain radiograph, while 11.8% had CT or MRI as their initial study. The median number of days between diagnosis and imaging was zero (Inter-quartile range 0-7) for any modality, 11 (IQR 2-42) for CT, and 10 (IQR 3-30) for MRI.
Figure 2.
Study Populations
Care received from other physicians
For the 11,294 beneficiaries imaged within 180 days, 2,250 (19.9%) were treated by an orthopedic surgeon between the dates of diagnosis and imaging. The proportions who saw chiropractors, neurosurgeons, or rheumatologists were 1,619 (16.4%), 170 (1.5%), and 248 (2.0%), respectively. Among the 23,522 beneficiaries who did not receive imaging, 15.9% saw a chiropractor, 0.9% a neurosurgeon, and 2.7% a rheumatologist.
Site and rapidity of imaging
In a third of cases (29%) beneficiaries were imaged within their CTS PCP’s practice organization. In bivariate analyses, the site of imaging was not associated with the CTS PCP’s practice ownership status (data not shown). This held true irrespective of imaging modality. However, time between diagnosis and imaging was significantly shorter for beneficiaries imaged within their CTS PCP’s practice than for those imaged elsewhere (Mean of 9.5 days vs. 15.7 days, respectively).
Imaging and patients’ sociodemographic characteristics
Minority beneficiaries received less rapid and less advanced imaging than white beneficiaries [24.8%, 18.9%, 29.7% (p<0.001) for imaging within 28 days and 9.1%, 7.2%, 10.8% (p<0.05) for CT/MRI among black, patients of other races, and white patients, respectively]. Beneficiaries also covered by Medicaid received less rapid and less advanced imaging than other patients [22.7% vs. 29.7% (p<0.001) for imaging within 28 days and 7.3% 11.0% (p<0.001) for CT/MRI]. (Table 2) These results persisted in multivariate analyses. (Table 3)
Table 2.
Characteristics of Medicare beneficiaries with uncomplicated low back pain and their primary care physicians, and the rapidity and modality of imaging that they received
| Rapidity of imaging | Imaging modality | ||||||
|---|---|---|---|---|---|---|---|
| N (%) Total = 35,039 |
Within 28 days, Percent of beneficiaries (N = 9,637) |
Within 29-180 days Percent of beneficiaries (N =1,657) |
None within 180 days Percent of beneficiaries (N = 23,745) |
Any CT/MRI Percent of beneficiaries (N = 3,598) |
Radiograph only Percent of beneficiaries (N = 7,696) |
None within 180 days Percent of beneficiaries (N = 23,245) |
|
|
Characteristics of
beneficiaries |
|||||||
| Age | |||||||
| 65-74 | 19,856 (56.7) | 28.0 | 4.8 | 67.2 | 10.8 | 22.0 | 67.2 |
| 75-84 | 12,345 (35.2) | 29.6 | 4.7 | 65.7 | 10.3 | 24.0 | 65.7 |
| >84 | 2,838 (8.1) | 30.5a | 2.5c | 66.9 | 8.5a | 24.6 | 66.9 |
| Female | 24,281 (69.3) | 28.9 | 4.8 | 66.3 | 10.2 | 23.5 | 66.3 |
| Male | 10,758 (30.7) | 28.4 | 4.1 | 67.5 | 11.0 | 21.5a | 67.5 |
| Race | |||||||
| White | 30,746 (87.8) | 29.7 | 4.7 | 65.6 | 10.8 | 23.6 | 65.6 |
| Black | 2,626 (7.5) | 24.8c | 4.5 | 70.8c | 9.1a | 20.1b | 70.8c |
| Other | 1,667 (4.8) | 18.9c | 2.7c | 78.4c | 7.2a | 14.4c | 78.4c |
| Not Medicaid eligible | 30,664 (87.5) | 29.7 | 4.7 | 65.5 | 11.0 | 23.5 | 65.5 |
| Medicaid eligible | 4,375 (12.5) | 22.7c | 3.8a | 73.5c | 7.3c | 19.2b | 73.5c |
| Charlson index | |||||||
| No comorbidities | 31,684 (90.4) | 28.6 | 4.6 | 66.8 | 10.3 | 22.9 | 66.8 |
| 1 comorbidity | 1,711 (4.9) | 31.7 | 4.5 | 63.8 | 14.0b | 22.2 | 63.8 |
| ≥2 comorbidities | 1,644 (4.7) | 28.4 | 5.6 | 66.0 | 10.5 | 23.5 | 66.0 |
| Median household income in zip code |
|||||||
| Above county median | 17,693 (50.5) | 29.5 | 5.0 | 65.5 | 11.3 | 23.2 | 65.5 |
| Below county median | 16,599 (47.5) | 28.0a | 4.2 | 67.8c | 9.8b | 22.5 | 67.8c |
|
Characteristics of the
PCP and his or her practice |
|||||||
| Specialty | |||||||
| General internal medicine |
16,835 (48.0) | 31.1 | 4.5 | 64.4 | 11.2 | 24.4 | 64.4 |
| Family/general practice |
18,204 (52.0) | 26.5c | 4.8 | 68.8c | 9.8a | 21.4b | 68.8c |
| Years in practice | |||||||
| 0-10 | 9,452 (27.0) | 32.0 | 4.7 | 65.0 | 10.7 | 24.3 | 65.0 |
| 11-20 | 12,574 (35.9) | 29.0 | 4.7 | 66.3 | 10.1 | 23.6 | 66.3 |
| >20 | 13,013 (37.1) | 27.4 | 4.5 | 68.1a | 10.7 | 21.2b | 68.1a |
| Board certified | 30,640 (87.5) | 29.0 | 4.7 | 66.3 | 10.6 | 23.1 | 66.3 |
| Not board certified | 4,320 (12.3) | 26.5 | 4.0 | 69.5 | 9.5 | 21.0 | 69.5 |
| Medical school outside U.S./Canada |
5,958 (17.0) | 26.2 | 4.2 | 69.6 | 8.9 | 21.5 | 69.6 |
| U.S./Canadian medical school |
29,071 (83.0) | 29.3a | 4.7 | 66.0a | 10.9b | 23.2 | 66.0a |
| Practice type | |||||||
| Solo/2-person | 15,452 (44.1) | 25.3 | 4.5 | 70.2 | 10.0 | 19.7 | 70.3 |
| Small group, 3-10 | 7,104 (20.3) | 31.6c | 4.3 | 64.1c | 10.6 | 25.3c | 64.1c |
| Medium group, 11-50 | 2,877 (8.2) | 37.6c | 5.1 | 67.3c | 10.3 | 32.4c | 57.3c |
| Large group, >50 | 1,366 (3.9) | 33.9c | 4.9 | 61.1c | 11.2 | 27.7c | 61.1c |
| Medical school | 822 (2.4) | 25.0 | 4.3 | 70.7 | 9.3 | 20.0 | 70.7 |
| Hospital practice/Other |
6,889 (19.7) | 28.4c | 4.9 | 66.7c | 11.3 | 21.9a | 66.7c |
| Group/staff HMO | 529 (1.5) | 23.9 | 5.6 | 70.5 | 10.7 | 18.8 | 70.5 |
| Practice revenue derived from Medicaid |
|||||||
| 0-5% | 17,824 (50.9) | 30.7 | 4.5 | 64.8 | 11.2 | 24.0 | 64.8 |
| 6-15% | 10,908 (31.1) | 29.3 | 4.9 | 65.8 | 10.5 | 23.7 | 65.8 |
| >15% | 6,307 (18.0) | 23.8c | 34.5 | 71.7c | 8.9b | 19.4c | 71.7c |
| Practice revenue derived from capitation |
|||||||
| None | 16,659 (47.5) | 28.6 | 4.8 | 66.7 | 10.9 | 22.5 | 66.6 |
| 1-10% | 7,489 (21.4) | 31.1 | 4.4 | 64.5 | 11.1 | 24.5 | 64.5 |
| 11-25% | 4,330 (12.4) | 29.0 | 5.1 | 65.8 | 10.2 | 23.9 | 65.8 |
| >25% | 6,561 (18.7) | 26.4 | 3.9 | 69.7 | 8.8b | 21.5 | 69.7 |
| Practice ownership | |||||||
| Full owner | 14,830 (42.3) | 27.3 | 4.7 | 68.0 | 10.3 | 21.7 | 65.5 |
| Part-owner | 9,298 (26.5) | 30.1a | 4.3 | 65.6 | 10.0 | 24.4a | 65.6 |
| Employed | 10,911 (31.1) | 29.8a | 4.7 | 65.5 | 11.1 | 23.4 | 68.0 |
| Financial incentives | |||||||
| None of three types of incentives |
2,828 (8.1) | 31.0 | 4.9 | 64.1 | 10.5 | 25.4 | 64.1 |
| Only clinical quality incentives |
63 (0.2) | 26.1 | 3.0 | 70.9 | 1.4c | 27.8 | 70.9 |
| Only patient satisfaction incentives |
122 (0.4) | 58.0c | 5.9 | 36.1c | 17.1c | 46.9c | 36.1c |
| Only productivity incentives |
13,240 (37.8) | 30.0 | 4.6 | 65.4 | 10.6 | 24.1 | 65.4 |
| Clinical quality and patient satisfaction, but not productivity incentives |
144 (0.4) | 18.4b | 3.4 | 78.3b | 10.6 | 11.1b | 78.3b |
| Clinical quality and productivity, but not patient satisfaction incentives |
1,005 (2.9) | 29.9 | 4.7 | 65.4 | 11.6 | 22.9 | 65.4 |
| Patient satisfaction and productivity incentives, but not clinical quality incentives |
2,128 (6.1) | 33.6 | 3.7 | 62.7 | 11.1 | 26.2 | 62.7 |
| All three types of incentives |
3,200 (9.1) | 26.1 | 5.3 | 68.7 | 10.1 | 21.2 | 68.7 |
| Not asked questions on specific incentives |
11,902 (34.0) | 25.1a | 4.5 | 70.5b | 10.0 | 19.6 | 70.5b |
Unweighted counts and weighted percentages are based on analysis of claims in years 2000-2002 and 2004-2006 for 35,039 fee-for-service Medicare beneficiaries treated by one of 4,567 primary care physician respondents to the Community Tracking Study Physician Survey.
p-value<0.05
p-value<0.01
p-value<0.001 for comparisons to the first (referent) category for each patient, physician, or practice characteristic.
Table 3.
Rapidity and modality of imaging for Medicare patients with acute low back pain and the individual and practice characteristics of their primary care physiciansa
| Characteristics | N (%) Total = 35,039 |
Adjusted Odds Ratiob (95% CI) |
Adjusted Odds Ratiob (95% CI) |
|---|---|---|---|
| Characteristics of Patients | |||
| Age | |||
| 65-74 | 19,856 (56.7) | 1.00 | 1.00 |
| 75-84 | 12,345 (35.2) | 1.10 (1.02-1.18)a | 1.07 (1.01-1.14)a |
| >84 | 2,838 (8.1) | 1.02 (0.89-1.17) | 0.96 (0.85-1.09) |
| Male | 24,281 (69.3) | 1.00 | 1.00 |
| Female | 10,758 (30.7) | 1.04 (0.96-1.13) | 1.04 (0.96-1.13) |
| Race | |||
| White | 30,746 (87.8) | 1.00 | 1.00 |
| Black | 2,626 (7.5) | 0.84 (0.75-0.95)b | 0.88 (0.78-0.99)a |
| Other | 1,667 (4.8) | 0.70 (0.53-0.93)a | 0.72 (0.52-0.94)b |
| Not Medicaid eligible | 30,664 (87.5) | 1.00 | 1.00 |
| Medicaid eligible | 4,375 (12.5) | 0.80 (0.67-0.94)b | 0.79 (0.66-0.94)b |
| Klabunde score (mean) | 35,039 (100) | 1.09 (1.02-1.17)b | 1.09 (1.02-1.16)a |
| Charlson index | |||
| No comorbidities | 31,684 (90.4) | 1.00 | 1.00 |
| 1 comorbidity | 1,711 (4.9) | 1.16 (0.97-1.38) | 1.21 (1.03-1.42)a |
| ≥2 comorbidities | 1,644 (4.7) | 0.90 (0.73-1.11) | 0.92 (0.73-1.15) |
| Median household income in patient’s zip code |
|||
| Above county median | 17,693 (50.5) | 1.00 | 1.00 |
| Below county median | 16,599 (47.5) | 1.00 (0.92-1.10) | 0.93 (0.86-0.99)a |
|
|
|||
|
Characteristics of the PCP and his or
her practice |
|||
| Specialty | |||
| General internal medicine | 16,835 (48.0) | 1.00 | 1.00 |
| Family/general practice | 18,204 (52.0) | 0.92 (0.86-0.99)a | 0.93 (0.86-1.00)a |
| Years in practice | |||
| 0-10 | 9,452 (27.0) | 1.00 | 1.00 |
| 11-20 | 12,574 (35.9) | 0.99 (0.92-1.08) | 0.99 (0.92-1.07) |
| >20 | 13,013 (37.1) | 0.99 (0.90-1.09) | 1.00 (0.90-1.10) |
| Board certified | 30,640 (87.5) | 1.00 | 1.00 |
| Not board certified | 4,320 (12.3) | 0.99 (0.86-1.14) | 0.97 (0.84-1.12) |
| Medical school outside U.S./Canada | 5,958 (17.0) | 1.00 | 1.00 |
| U.S./Canadian medical school | 29,071 (83.0) | 1.03 (0.93-1.14) | 1.05 (0.96-1.15) |
| Practice type | |||
| Solo/2-person | 15,452 (44.1) | 1.00 | 1.00 |
| Small group, 3-10 | 7,104 (20.3) | 1.11 (0.97-1.26) | 1.07 (0.94-1.22) |
| Medium group, 11-50 | 2,877 (8.2) | 1.50 (1.28-1.77)c | 1.37 (1.19-1.58)c |
| Large group, >50 | 1,366 (3.9) | 1.24 (1.01-1.53)a | 1.21 (1.02-1.44)a |
| Medical school | 822 (2.4) | 0.93 (0.72-1.20) | 0.91 (0.72-1.16) |
| Hospital practice/Other | 6,889 (19.7) | 1.02 (0.89-1.17) | 1.02 (0.90-1.15) |
| Group/staff HMO | 529 (1.5) | 0.97 (0.73-1.29) | 1.01 (0.76-1.36) |
| Practice revenue derived from Medicaid | |||
| 0-5% | 17,824 (50.9) | 1.00 | 1.00 |
| 6-15% | 10,908 (31.1) | 0.92 (0.84-1.00)a | 0.92 (0.85-1.00)a |
| >15% | 6,307 (18.0) | 0.84 (0.76-0.93)c | 0.85 (0.77-0.94)c |
| Practice revenue derived from capitation | |||
| None | 16,659 (47.5) | 1.00 | 1.00 |
| 1-10% | 7,489 (21.4) | 1.00 (0.83-1.07) | 0.99 (0.93-1.06) |
| 11-25% | 4,330 (12.4) | 1.08 (0.95-1.23) | 1.07 (0.95-1.21) |
| >25% | 6,561 (18.7) | 0.93 (0.83-1.03) | 0.89 (0.81-0.98)a |
| Practice ownership | |||
| Full owner | 14,830 (42.3) | 1.00 | 1.00 |
| Part-owner | 9,298 (26.5) | 0.88 (0.90-0.97)b | 0.89 (0.90-0.98)a |
| Employed | 10,911 (31.1) | 0.80 (0.70-0.93)b | 0.82 (0.71-0.95)b |
| Financial incentives | |||
| None of three types of incentives | 2,828 (8.1) | 1.00 | 1.00 |
| Only clinical quality incentives | 63 (0.2) | 0.73 (0.43-1.25) | 0.62 (0.39-1.01) |
| Only patient satisfaction incentives | 122 (0.4) | 3.41 (2.70-4.30)c | 2.63 (2.12-3.26)c |
| Only productivity incentives | 13,240 (37.8) | 0.97 (0.87-1.09) | 0.97 (0.87-1.09) |
| Clinical quality and patient satisfaction, but not productivity incentives |
144 (0.4) | 0.70 (0.52-0.95)a | 0.75 (0.54-1.04) |
| Clinical quality and productivity, but not patient satisfaction incentives |
1,005 (2.9) | 1.01 (0.87-1.17) | 1.01 (0.87-1.16) |
| Productivity and patient satisfaction incentives, but not clinical quality incentives |
2,128 (6.1) | 0.99 (0.85-1.15) | 0.97 (0.83-1.14) |
| All three types of incentives | 3,200 (9.1) | 0.86 (0.73-1.02) | 0.89 (0.76-1.03) |
| Not asked questions on specific incentives |
11,902 (34.0) | 1.07 (0.90-1.28) | 1.05 (0.88-1.26) |
Unweighted counts, weighted percentages, and odds ratios are based on analysis of fee-for-service Medicare claims from 2000-2002 and 2004-2006 for 35,039 fee-for-service Medicare beneficiaries treated by one of 4,567 Community Tracking Study primary care physicians.
CI denotes confidence interval. Adjusted for beneficiary age, sex, Medicaid eligibility, race, and Klabunde and Charlson comorbidity scores; median household income in the beneficiary’s zip code and percentage of adults 25 years or older with at least 12 years of education; the CTS PCP’s specialty, number of years in practice, board certification status, site of medical school, practice ownership status, and exposure to financial incentives based on performance on quality, profiling, patient satisfaction, or productivity; type and size of the CTS PCP’s practice, as well as the percentage of its revenues derived from Medicare, Medicaid, and capitation; urban vs. rural location; radiologist supply per 1,000 capita in the CTS PCP’s county; the round of the survey (2000-2001 or 2004-2005), and the sampling cluster for the CTS survey (site dummy).
Imaging and primary care physicians’ exposure to financial incentives
Beneficiaries treated in practices more reliant on Medicaid revenues received less rapid and less advanced imaging than other beneficiaries [23.8% vs. 30.7% (p<0.001) for imaging within 28 days and 8.9% vs. 11.2% (p<0.01) for CT/MRI for highest vs. lowest terciles, respectively]. Similarly, patients whose CTS PCPs with greater than 25% of revenues derived from capitation or who were solo practitioners received both less rapid and advanced imaging than those treated in practices receiving no practice revenues from capitation or who were employed. (Table 2)
Beneficiaries treated by CTS PCPs with variable compensation based only on patient satisfaction received more rapid and advanced imaging than beneficiaries whose PCPs were exposed to other combinations of incentives. (Tables 2 and 3) In contrast, beneficiaries whose CTS PCP was exposed to incentives based on both clinical quality and satisfaction, but not productivity, received less rapid imaging. These associations with financial incentives persisted in multivariate analyses. Interactions between the round of the survey and each combination of incentives were non-significant.
Imaging and other characteristics PCPs and their practices
Beneficiaries treated by family/general practitioners consistently received less rapid and less advanced imaging than those cared for by general internists (Table 2).
Beneficiaries with CTS PCPs in practices of 10 or more physicians were more likely to receive imaging within 28 days than those seeing physicians in solo/2-person practices. In adjusted analyses, beneficiaries treated in larger group practices were also substantially more likely to receive advanced imaging. (Table 3)
Sensitivity analyses
Our core findings of associations between the level of imaging and patient and physician characteristics persisted across a range of sensitivity analyses. Results were similar when we attributed beneficiaries who had any visits with the CTS PCP to that PCP, and when we attributed to each CTC PCP only beneficiaries for whom they had coded the initial LBP diagnosis. Our results were also robust when we re-defined the level of imaging as the total number of low back imaging studies that a beneficiary received.
Clinical events after diagnosis of low back pain
Rates of new cancer diagnoses were similar regardless of the timing or modality of imaging (Table 4). Hospitalization for, and complications or progression of back pain were more common among beneficiaries receiving imaging than among those who did not.
Table 4.
Clinical events among Medicare beneficiaries within 180 days after diagnosis of acute low back pain, by the rapidity and modality of imaging they received
| Rapidity and Modality of Imaging |
Total (100%) |
New Diagnoses of Cancer N (%) |
Hospitalizations for Back Diagnoses N (%) |
Complications or Progression of Back Pain N (%) |
|---|---|---|---|---|
| No imaging | 22,745 | 1,511 (7.3) | 22 (0.1) | 28 (0.2) |
| Rapidity | ||||
| 29-180days | 1,657 | 64 (3.9)b | 69 (4.3)b | 29 (2.3)b |
| Within 28 days | 9,637 | 651 (5.8)a | 288 (2.5)b | 111 (1.0)b |
| Modality | ||||
| Radiograph only | 7,696 | 474 (5.3)a | 65 (0.7)b | 31 (0.3)a |
| CT/MRI | 3,598 | 241 (6.0)a | 292 (7.3)b | 109 (2.9) |
Unweighted counts and weighted percentages are based on analysis of claims in years 2000-2002 and 2004-2006 for 35,039 fee-for-service Medicare beneficiaries treated by one of 4,567 primary care physician respondents to the Community Tracking Study Physician Survey. P-values reflect comparisons to beneficiaries who did not receive imaging.
p<0.05
p<0.001
DISCUSSION
This study focused on the use of imaging for uncomplicated acute low back pain because it is prevalent and well established guidelines indicate that rapid or advanced imaging is not beneficial in the absence of specific complicating features or comorbid conditions.5,6,7
We found that rapidity and modality of imaging for back pain was associated with non-clinical characteristics of patients and the physicians and practices that treated them. Low-income and minority patients, and those treated in smaller practices or practices more reliant on Medicaid revenues received less rapid and advanced imaging than higher-income or white patients, and those in larger practices or settings less reliant on Medicaid. These results are consistent with previously reported patterns of care in terms of groups who tend to receive fewer services, although here, the patterns represent better quality care in contrast to when measuring quality in terms of underuse.19,20 Our findings were consistent across the timing or number of imaging studies, and for all modalities. Moreover, patients cared for by physicians exposed to incentives based on patient satisfaction received more rapid and advanced imaging, Conversely, those whose physicians were exposed to both clinical quality and productivity incentives received less rapid and advanced imaging.
The association between exposure to satisfaction incentives and the level of imaging is not unexpected. Patients may consider imaging reassuring, and those with higher socio-economic status may be more successful in obtaining testing in this context. But in contrast to generally underused services such as diabetic monitoring, more rapid or advanced imaging for LBP may not benefit patients, and may result in harm.22,23
Contrary to our hypothesis that incentives focused on underuse might result in greater potential overuse, we observed an inverse association between exposure to clinical quality incentives and the level of imaging. These results should be interpreted with caution as we had only a small number of observations for some combinations of incentives. Nevertheless, they suggest that quality-based incentives may improve appropriateness of care in some unmeasured arenas. This could reflect a broad ecologic effect, if physicians exposed to existing incentives become more generally aware of, and adherent to, clinical practice guidelines.24 Alternatively, physicians exposed to quality measurement may be less vulnerable to the effects of incentives that encourage imaging.
We also found that exposure to both clinical quality and satisfaction incentives among a small fraction of PCPs resulted in less rapid or advanced imaging than with either incentive alone or no incentives at all. Although some prior studies suggest that patient satisfaction tends to correlate with clinical quality,25,26 Landon et al. compared the experiences of Medicare beneficiaries in the fee-for-service vs. managed care programs, and found instead that the two systems had different strengths in quality versus satisfaction performance.27 Our findings are also consistent with those of Weyer et al., who reported that improvements in preventive services were associated with declines in patient satisfaction.28 Although our results require confirmation in larger populations of physicians facing this relatively rare combination of incentives, it is possible that physicians less pressured to maximize visit volume can better align their efforts to perform well on both clinical quality and patient satisfaction (e.g., by spending more time providing reassurance about deferred imaging). However, these benefits would accrue to relatively few patients, as far more physicians face productivity incentives than other types of incentives.29
We found that one-third of imaging studies were performed within the PCP’s practice organization, and that patients treated in large group practices were modestly more likely to receive rapid and advanced imaging than those treated in smaller practices. As large groups are more likely to have the resources to invest in imaging equipment,30 our results are consistent with other studies suggesting that practice-owned equipment results in supplier-induced demand and physician self-referral.31 These associations were independent of the higher likelihood that physicians in large practices were exposed to performance incentives. They contrast with studies showing that larger practices tend to outperform smaller ones in quality improvement efforts and on standardized measures emphasizing underuse.19,32,33
Finally, we found that many patients received imaging on the day of diagnosis. These care patterns are inconsistent with guidelines that recommend a trial of conservative therapy first, and suggest opportunities for quality improvement.
Our results should be interpreted within the context of our analytic approach. We could not determine appropriateness of imaging for a given patient. Ours is a comparative analysis of the level of imaging relative to patient, physician, and practice characteristics, and not an attempt to benchmark the behavior of individual physicians. The inability to identify particular cases of overuse with certainty does not invalidate our findings because all physicians are subject to such errors in coding and ascertainment. As an example, for our results to be biased, physicians would have to be more likely to code diagnoses of “red flag” conditions for minority patients than for white patients, at the same time that they are less likely to order imaging studies for minority patients. Although rates of back pain complications and hospitalizations was higher for patients receiving more rapid or advanced imaging, these differences may reflect, in part, events triggered by the initial imaging study itself and/or the relative aggressiveness of care delivered by physicians who are more likely to order imaging. Rates of cancer diagnoses were no higher for patients who had more rapid or advanced imaging.
We cannot be certain that each CTS PCP was truly responsible for imaging decisions for the patients studied, because claims-based attribution may not reflect actual care relationships.33 However, our conclusions were robust under both more liberal and more restrictive attribution approaches, and when we focused on patients whose initial LBP diagnosis was coded by the PCP, or those who saw only that physician between the dates of diagnosis and imaging. Thus regardless of the involvement of other providers, the level of imaging appears to be related to the characteristics of a patient’s PCP.
Our findings require confirmation with a broader set of overuse measures, but nevertheless have important implications. Development of more overuse metrics would balance out current measures that are heavily weighted toward underuse, perhaps by leveraging research on the comparative effectiveness of different treatment options.34 It is not surprising that physicians and practices with attributes associated with underuse of care are less likely to overuse imaging. However, our results may provide a rationale for tailoring packages of performance metrics to practice attributes. For example, a practice with high Medicaid revenue, many minority patients and minimal physician incentives for maximizing patient satisfaction may be more likely to benefit from measures emphasizing underuse. In contrast, practices with less Medicaid revenue, fewer minority patients and more satisfaction-based incentives may be more likely to benefit from performance measures that include overuse.
More balanced measurement of overuse and underuse might also allow insurers to design incentives to counter both. For example, insurers could offer higher co-payments for services that tend to be overused but lower or no co-payments for generally underused services. Similarly, bonuses could encourage physicians to avoid overused services or increase underused services. Mandatory delays in ordering overused services in the absence of clinical “red flags” is another alternative tool. Such interventions would need to avoid limiting necessary care particularly for low-income patients, but in the context of fee-for-service reimbursement, targeted and balanced incentives could better align the dual goals of quality improvement and cost containment.
Patterns of care revealed by the application of a single measure of potential overuse point to different foci for performance improvement than when measurement focuses on underuse. Given possible reversal in direction from the typical “quality advantage” for important subpopulations of patients and physicians, measuring overuse alongside underuse may be critical for improving the overall appropriateness of care.
Supplementary Material
Table 1.
Distribution of Medicare patients with uncomplicated acute low back pain, 2000-2002 and 2004-2006, by the characteristics of their primary care physicians
| Characteristic of primary care physicians and their practices |
Percentage of Beneficiaries N = 35,039 |
|---|---|
| Specialty | |
| General internal medicine | 49.1 |
| Family/general practice | 50.9 |
| Years in practice | |
| 0-10 | 26.4 |
| 11-20 | 36.3 |
| >20 | 37.3 |
| Board certified | 88.4 |
| Not board-certified | 11.6 |
| U.S./Canadian medical school | 81.5 |
| Medical school elsewhere | 18.5 |
| Practice type | |
| Solo/2-person | 42.3 |
| Small group, 3-10 | 21.4 |
| Medium group, 11-50 | 8.7 |
| Large group, >50 | 5.5 |
| Medical school | 1.8 |
| Hospital practice/Other | 19.0 |
| Group/staff HMO | 1.3 |
| Practice revenue derived from Medicaid | |
| 0-5% | 44.1 |
| 6-15% | 34.4 |
| >15% | 21.5 |
| Practice revenue derived from capitation | |
| None | 52.7 |
| 1-10% | 19.9 |
| 11-25% | 10.8 |
| >25% | 16.6 |
| Practice ownership | |
| Whole owner | 44.9 |
| Part-owner | 24.3 |
| Employed | 30.8 |
| Incentives based on quality measures | 13.1 |
| Incentives based on patient satisfaction | 17.8 |
| Incentives based on profiling | 7.5 |
| Incentives based on productivity | 54.7 |
Unweighted counts and weighted percentages are based on analysis of claims in years 2000-2002 and 2004-2006 for 35,039 fee-for-service Medicare beneficiaries treated by one of 4,567 primary care physician respondents to the Community Tracking Study Physician Survey
Acknowledgements
This study and the Community Tracking Study Physician Survey were supported by the Robert Wood Johnson Foundation. This analysis was also supported by grant R01 AG027312-02S1 from the National Institute on Aging (Dr. Landon). Funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; or preparation, review, or approval of the manuscript. None of the authors have any conflicts of interest. Dr. Pham had full access to the data and takes responsibility for the integrity of the data and accuracy of the analysis.
REFERENCES
- 1.National Quality Forum [accessed October 2, 2007];NQF-Endorsed Standards for Ambulatory Care. 2007 August 1; At: http://www.qualityforum.org/pdf/lsEndorsedStandardsALL08-14-07corrected.pdf.
- 2.Deyo RA. Cascade effects of medical technology. Annu Rev Pub Health. 2002;23:23–44. doi: 10.1146/annurev.publhealth.23.092101.134534. Epub 2001 Oct 25. [DOI] [PubMed] [Google Scholar]
- 3.Committee on Redesigning Health Insurance Performance Measures, Payment, and Performance Improvement Programs, Institute of Medicine . Performance Measurement: Accelerating Improvement. National Academies Press; Washington, DC: 2006. [Google Scholar]
- 4.Anderson GBJ. Epidemiologic features of chronic low-back pain. Lancet. 1999;354:581–5. doi: 10.1016/S0140-6736(99)01312-4. [DOI] [PubMed] [Google Scholar]
- 5.Bigos S, et al. Clinical practice guideline no.14. Agency for Heatlh Care Policy and Research; Rockville, MD: Dec, 1994. Acute low back problems in adults. (publication no. 95-0642) [Google Scholar]
- 6.Institute for Clinical Systems Improvement . Adult low back pain. ICSI; Bloomington, MN: Sep 63, 2004. [Google Scholar]
- 7.Chou R, et al. Diagnosis and treatment of low back pain: A joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Int Med. 2007;147:478–491. doi: 10.7326/0003-4819-147-7-200710020-00006. [DOI] [PubMed] [Google Scholar]
- 8.Bach PB, Pham HH, Schrag D, Tate RC, Hargraves JL. Primary care physicians who treat blacks and whites. N Engl J Med. 2004 Aug 5;351(6):575–84. doi: 10.1056/NEJMsa040609. [DOI] [PubMed] [Google Scholar]
- 9.Center for Studying Health System Change . Physician Survey Methodology Report, 2004-2005. Washington, D.C.: Technical Publication No. 70. [Google Scholar]
- 10.National Committee on Quality Assurance . HEDIS 2006 Technical Specifications. Washington, D.C.: [Google Scholar]
- 11.Klabunde CN, Potosky AL, Legler JM, Warren JL. Development of a comorbidity index using physician claims data. J Clin Epidemiol. 2000;53:1258–1267. doi: 10.1016/s0895-4356(00)00256-0. [DOI] [PubMed] [Google Scholar]
- 12.Romano PS. Adapting a clinical comorbidity index for use with ICD-9-CM administrative data: differing perspectives. J.Clin.Epidemiol. 1993;46:1075–1079. doi: 10.1016/0895-4356(93)90103-8. [DOI] [PubMed] [Google Scholar]
- 13.Area Resources File, 2005 release. Health Resources and Services Administration; Washington, D.C.: [Google Scholar]
- 14.Cherkin DC, Deyo RA, Volinn E, Loeser JD. Use of the International Classification of Diseases (ICD-9-CM) to identify hospitalizations for mechanical low back problems in administrative databases. Spine. 1992 Jul;17(7):817–25. doi: 10.1097/00007632-199207000-00015. [DOI] [PubMed] [Google Scholar]
- 15.SUDAAN analytic software. release 7.0. Research Triangle Institute International; Research Triangle Park, NC: software. [Google Scholar]
- 16.Welch WP, Miller ME, Welch HG, Fisher ES, Wennberg JE. Geographic variation in expenditures for physicians’ services in the United States. N Engl J Med. 1993 Mar 4;328(9):621–7. doi: 10.1056/NEJM199303043280906. [DOI] [PubMed] [Google Scholar]
- 17.Halm EA, Chassin MR, Turhim S, et al. Revisiting the appropriateness of carotid endarterectomy. 2003 Jun;34(6):1464–71. doi: 10.1161/01.STR.0000072514.79745.7D. Epub 2003 May 8. [DOI] [PubMed] [Google Scholar]
- 18.Leape LL, Park RE, Solomon DH, et al. Does inappropriate use explain small-area variations in the use of health care services? JAMA. 1990 Feb 2;263(5):669–72. [PubMed] [Google Scholar]
- 19.Pham HH, Schrag D, Hargraves JL, Bach PB. Delivery of preventive services to older adults by primary care physicians. JAMA. 2005 Jul 27;294(4):473–81. doi: 10.1001/jama.294.4.473. [DOI] [PubMed] [Google Scholar]
- 20.Landon BE, Normand SL, Meara E, et al. The relationship between medical practice characteristics and quality of care for cardiovascular disease. Med Care Res Rev. 2008 Apr;65(2):167–86. doi: 10.1177/1077558707310208. Epub 2007 Dec 20. [DOI] [PubMed] [Google Scholar]
- 21.Wilson IB, Dukes K, Greenfield S, Kaplan S, Hillman B. Patients’ role in the use of radiology testing for common office practice complaints. Arch Intern Med. 2001 Jan 22;161(2):256–63. doi: 10.1001/archinte.161.2.256. [DOI] [PubMed] [Google Scholar]
- 22.Deyo RA, Weinstein JN. Low Back Pain. N Engl J Med. 2001 Feb 1;344(5):363–370. doi: 10.1056/NEJM200102013440508. [DOI] [PubMed] [Google Scholar]
- 23.Modic MT, Obuchowski NA, Ross JS, et al. Acute low back pain and radiculopathy: MR imaging findings and their prognostic role and effect on outcome. Radiology. 2005 Nov;237(2):597–604. doi: 10.1148/radiol.2372041509. [DOI] [PubMed] [Google Scholar]
- 24.O’Malley AS, Pham HH, Reschovsky JD. Predictors of the growing influence of clinical practice guidelines. J Gen Intern Med. 2007 Jun;22(6):742–8. doi: 10.1007/s11606-007-0155-y. Epub 2007 Mar 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sequist TD, Schneider EC, Anastario M, et al. Quality Monitoring of Physicians: Linking Patients’ Experiences of Care to Clinical Quality and Outcomes. J Gen Intern Med. 2008 Aug 28; doi: 10.1007/s11606-008-0760-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schneider EC, Zaslavsky AM, Landon BE, Lied TR, Sheingold S, Cleary PD. National quality monitoring of Medicare health plans: the relationship between enrollees’ reports and the quality of clinical care. Med Care. 2001 Dec;39(12):1313–25. doi: 10.1097/00005650-200112000-00007. [DOI] [PubMed] [Google Scholar]
- 27.Landon BE, Zaslavsky AM, Bernard SL, Cioffi MJ, Cleary PD. Comparison of performance of traditional Medicare vs Medicare managed care. JAMA. 2004 Apr 14;291(14):1744–52. doi: 10.1001/jama.291.14.1744. [DOI] [PubMed] [Google Scholar]
- 28.Weyer SM, Bobiak S, Stange KC. Possible unintended consequences of a focus on performance: insights over time from the research association of practices network. Qual Manag Health Care. 2008 Jan-Mar;17(1):47–52. doi: 10.1097/01.QMH.0000308637.04850.ac. [DOI] [PubMed] [Google Scholar]
- 29.Reschovsky J, Hadley J. Physician financial incentives: use of quality incentives inches up, but productivity still dominates. Issue Brief Cent Stud Health Syst Change. 2007 Jan;108:1–4. [PubMed] [Google Scholar]
- 30.Casalino LP, Pham HH, Bazzoli G. Growth of single-specialty groups. Health Aff (Millwood) 2004 Mar-Apr;23(2):82–90. doi: 10.1377/hlthaff.23.2.82. [DOI] [PubMed] [Google Scholar]
- 31.Mitchell J. The prevalence of physician self-referral arrangements after Stark II: Evidence from advanced diagnostic imaging. Health Aff (Millwood) 2007 May/June;26(3):w415–w424. doi: 10.1377/hlthaff.26.3.w415. [DOI] [PubMed] [Google Scholar]
- 32.Audet AM, Doty MM, Shamasdin J, Schoenbaum SC. Measure, learn, and improve: physicians’ involvement in quality improvement. Health Aff (Millwood) 2005 May-Jun;24(3):843–53. doi: 10.1377/hlthaff.24.3.843. [DOI] [PubMed] [Google Scholar]
- 33.Pham HH, Schrag D, O’Malley AS, Wu B, Bach PB. Care patterns in Medicare and their implications for pay-for-performance. N Engl J Med. 2007 Mar 15;356(11):1130–9. doi: 10.1056/NEJMsa063979. [DOI] [PubMed] [Google Scholar]
- 34.Clancy CM. Getting to “smart” health care. Health Aff (Millwood) 2006 Nov-Dec;25(6):w589–92. doi: 10.1377/hlthaff.25.w589. Epub 2006 Nov 7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.