Abstract
Objectives:
To examine the validity of body composition estimates obtained using foot-to-foot bio-electrical impedance analysis (BIA) in overweight and obese children by comparison to a reference four-compartment model (4-CM).
Subjects/Methods:
38 males: age (mean ± sd) 13.6 ± 1.3 years, body mass index 30.3 ± 6.0 kg.m−2 and 14 females: age 14.7 ± 2.2 years, body mass index 32.4 ± 5.7 kg.m−2 participated in the study. Estimates of fat-free mass (FFM), fat mass (FM) and percentage body fat (PBF) obtained using a Tanita model TBF-310 and a 4-CM (derived from body mass, body volume, total body water and total body bone mineral measurements) were compared using bias and 95% limits of agreement (Tanita minus 4-CM estimates).
Results:
Body composition estimates obtained with the Tanita TBF-310 were not significantly different from 4-CM assessments: for all subjects combined the bias was −0.7kg for FM, 0.7kg for FFM and −1.3% for PBF. However, the 95% limits of agreement were substantial for individual children: males, up to ±9.3kg for FFM and FM and ±11.0% for PBF; females, up to ±5.5kg for FFM and FM and ±6.5% for PBF.
Conclusions:
The Tanita TBF-310 foot-to-foot BIA body composition analyser with the manufacturer's prediction equations is not recommended for application to individual children who are overweight and obese although it may be of use for obtaining group mean values.
Keywords: bio-electrical impedance analysis, four-compartment model, body composition, children
Introduction
A number of studies have compared body composition estimates obtained in children from foot-to-foot (leg-to-leg) bio-electrical impedance analysis (BIA) against measurements from established laboratory techniques with mixed findings; such techniques include the two-compartment models (2-CM) of body composition, densitometry [1, 2] and dual-energy Xray absorptiometry (DXA) [3-6]. Discrepancies between techniques may be partly due to the inappropriate use of assumed constant proportions of the gross components of fat-free mass (water, protein and mineral) in 2-CMs for children of particular age groups, as these proportions are known to alter systematically with increasing age [7]. The reference four-compartment model (4-CM) essentially overcomes such potential discrepancies by incorporating independent measurements of total body water (TBW), total body bone mineral (TBBM), body weight (BWt) and body volume (BV) and is considered the most accurate of the safe and acceptable methods of body composition analysis. Furthermore, studies examining the validity of densitometry [8-11] and DXA [9-13] against reference 4-CMs have demonstrated substantial biases and 95% limits of agreement between methods, essentially obviating the use of 2-CMs for the validation of other techniques. Only one study in boys has examined the accuracy of foot-to-foot BIA body composition estimates against an appropriate 3-CM (BV, BWt and TBW) [8].
In the current climate of increasing amounts of childhood obesity and health sequelae into adulthood, accurate body composition information is essential for clinical practice and research purposes. Therefore, the aim of the present study was to determine the accuracy of body composition estimates using foot-to-foot BIA in overweight and obese children.
Methods
Subjects
Fifty-two overweight and obese children (38 male and 14 female) participated in the study. Subjects consist of two cohorts of children recruited from the local community by advertisement in newspapers and doctors surgeries or were residents on the Carnegie International Weight Loss Camp, Leeds, UK [14]. BWt was measured using scales integral to the Tanita BIA device, height (m) was measured using a floor-standing stadiometer and body mass index (BMI; kg.m−2) was calculated for each subject. BMI standard deviation scores (BMI SDSs) were calculated for each subject using UK National centile charts [15]. Children were included in the study if their BMI SDSs were above 1.04 (85th centile) representing the overweight category, and included 33 males and 12 females with BMI SDSs above 1.64 (95th centile) representing the obese. Characteristics of the sample are shown in Table 1. The study protocol was approved by Leeds (West) Teaching Hospital Research Ethics Committee, and both participant written informed assent and parental/guardian written informed consent were obtained prior to testing.
Table 1.
Subject characteristics and body composition estimates.
| Characteristic | Males (n=38) | Females (n=14) | ||
|---|---|---|---|---|
| mean ± sd | range | mean ± sd | range | |
| Age (y) | 13.6 ± 1.3 | 10.9 – 15.6 | 14.7 ± 2.2 | 11.1 – 17.6 |
| Body mass (kg) | 82.8 ± 18.9 | 46.0 – 118.2 | 87.5 ± 20.5 | 54.4 – 118.8 |
| Height (m) | 1.65 ± 0.11 | 1.46 – 1.86 | 1.64 ± 0.07 | 1.49 – 1.75 |
| BMI (kg.m−2) | 30.3 ± 6.0 | 21.1 – 42.4 | 32.4 ± 5.7 | 22.7 – 40.2 |
| BMI sds | 2.70 ± 0.76 | 1.14 – 3.85 | 2.78 ± 0.74 | 1.36 – 3.63 |
| FFM (kg; 4-CM) | 51.0 ± 12.3 | 31.4 – 75.5 | 49.2 ± 6.9 | 36.0 – 61.6 |
| FM (kg; 4-CM) | 31.8 ± 14.4 | 2.7 – 62.3 | 38.3 ± 14.3 | 17.0 – 58.0 |
| PBF (%; 4-CM) | 37.5 ± 12.0 | 3.5 – 58.1 | 42.3 ± 7.2 | 28.2 – 52.2 |
Bio-electrical impedance analysis
Body composition estimates were obtained using a Tanita TBF-310 (Tanita Corp., Tokyo, Japan) BIA device following manufacturer's recommended protocol and using prediction equations provided by the manufacturer and integral to the system. All measurements were undertaken after an overnight fast using the standard prediction equation mode with participants wearing swimsuits, also required as part of the preparation for other measurements.
Four-compartment model
Dual-energy X-ray absorptiometry
DXA measurements of bone mineral content ash (BMCash; kg) were made using a Prodigy fan-beam densitometer (GE/Lunar, Madison, WI, USA) and following the manufacturer's recommendations. Scan modes, standard or thick, were software selected (version 5.0) based upon an estimation of patient thickness.
Air displacement plethysmography
Body volume was measured using the BOD POD© whole body air displacement plethysmograph (Life Measurement Inc., Concord, CA), software version 1.69, in accordance with the manufacturer's operating instructions. Details of the measurement procedures have been described previously [16, 17]. Thoracic gas volume was measured in 23 subjects and estimated in the remaining 29 (22 male, 7 female) using child-specific equations [18].
Total body water
Two different methods for TBW calculation (plateau and interpolation) were used in the different cohorts of children, although the basic principle of determining the maximum 2H enrichment in the body water pool after administration of the dose was adhered to. Both methods have been shown to be both comparable and valid for accurate determination of TBW [19]. After obtaining a sample of saliva, plateau method (n=17), or urine, interpolation method (n=35), to determine background enrichments, an oral dose of approximately 0.35 mole 2H2O in 100 ml water was administered. The exact amount of dose given was determined by weighing the dosing bottle before and after administration. A sample of the dosing solution was kept frozen for later analysis with the samples. Further saliva samples were then collected at 4, 5 and 6 hours post dose and further urine samples were collected on the same evening subjects received the 2H2O and for the following three consecutive evenings. 2H enrichment was measured using isotope ratio mass spectrometry as previously described [20], and TBW was calculated using the following equation:
where D (g) is the amount of oral dosing solution administered to the subject, T (g) is the amount of deionised tap water used to dilute a sample of the dosing solution d (g). All expressed as delta values (%o), Ed is enrichment of the diluted dose d in T and Et is the enrichment of the tap water diluent. For plateau method Es is the mean enrichment of saliva samples at 4, 5 and 6 hours with Ep, the enrichment of the pre dose sample. For the interpolation method, where pre-dose values are subtracted from all post dose samples before plotting time vs logged enrichment graphs, (Es-Ep) is replaced instead by the enrichment determined by back extrapolation to T=0 of the disappearance curves of 2H over 3 days.
Finally, 2H2O dilution is corrected by 4% to account for the exchange of deuterium with non-aqueous hydrogen and converted to kg by dividing by 1000.
4-compartment model
Based on the actual measurements as provided by each technique, BWt (kg), BV (litres), BMCash (kg) and TBW (litres) were integrated into a reference 4-CM for estimation of FM [21]:
Statistical analyses
Agreement between Tanita and 4-CM body composition estimates was assessed using bias (mean difference) and 95% limits of agreement (±2SD), as described by Bland and Altman [22]. Paired t-test was applied to determine if any differences between techniques reached significance (P<0.05). Correlation matrices and stepwise multiple linear regression analyses were used to establish whether or not variability in particular subject characteristics may contribute to discrepancies between techniques. Additionally, bias introduced by the different total body water collection methods was examined using independent t-tests and by inclusion as a dummy variable (urine = 1, saliva = 2) in the stepwise regression.
Results
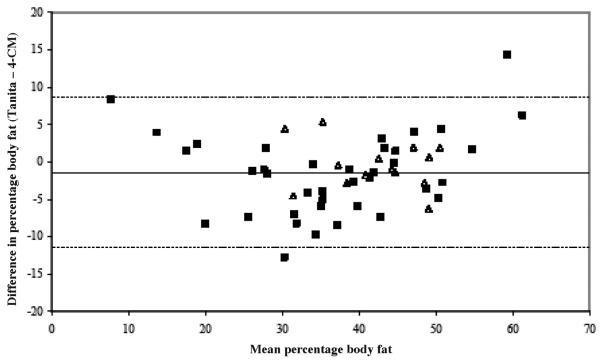
Body composition estimates, obtained using the 4-CM, are summarized in Table 1. Biases between the 4-CM and Tanita BIA methods for FFM and fat (FM and PBF) were relatively small in all cases (Table 2). These mean differences were not significant because of the substantial variability of individual differences between methods, represented by the large 95% limits of agreement (Table 2; Figure 1) and which were considerably greater for the males than females. Examination of the different total body water collection methods revealed no significant mean differences in 4-CM, Tanita BIA and delta body composition estimates. There was apparently no influence of the size of measurement on the differences between methods (i.e. the differences were not apparently related to the means of methods). However, application of the correlation matrix and subsequent stepwise multiple linear regression analysis indicated a significant influence of FFM on discrepancies in body composition assessments between methods (FM/FFM: R2 = 0.12; P<0.05, PBF: R2 = 0.21; P<0.01), but no effect of FM, PBF or total body water collection method. The apparent effect of FFM was reflected in BWt and Ht, probably because of the strong positive inter-relationships between FFM, BWt and Ht (all: r ≥ 0.58; P<0.001), which were effectively eliminated when BWt and Ht were factored into the model along with FFM.
Table 2.
Mean difference (Tanita – 4-CM estimate) ± 95% limits of agreement between methods.
| Method | All (n = 52) |
Males (n = 38) |
Females (n = 14) |
|---|---|---|---|
| FFM (kg) | 0.7 ± 8.4 | 0.8 ± 9.3 | 0.5 ± 5.5 |
| FM (kg) | −0.7 ± 8.4 | −0.8 ± 9.3 | −0.5 ± 5.5 |
| PBF (%) | −1.3 ± 9.9 | −1.6 ± 11.0 | −0.4 ± 6.5 |
NB – in no case was there a significant influence of the size of the measurement (average of the two techniques) on the difference between the techniques.
Figure 1.
Bland and Altman plots comparing percentage body fat estimated by Tanita BIA with 4-CM measurements: ■ boys; ▲ girls.
Discussion
The main findings from this study indicate that Tanita foot-to-foot BIA does not apparently provide accurate measurements of body composition for a considerable proportion of individual overweight or obese children, even though on a group basis the lack of a significant difference may at first sight indicate that the technique is accurate. In fact, 40% of children in the present study obtained a Tanita BIA PBF estimate greater than ±4% of the reference 4-CM value. Therefore, this technique does not appear to be applicable in clinical practice or research in which individual estimates may be required, supporting the findings in 42 males, aged 10.1-14.5 years, by Parker et al. [8] who reported 95% limits of agreement of ±7.8kg FM and ±14.1% PBF when comparing foot-to-foot BIA, using a Tanita TBF-521, to a criterion 3-CM. In contrast to the present study, however, Parker et al. [8] reported a mean BIA overestimation of 2.3 kg FM which resulted in a 4.1% overestimation in PBF. Possible factors impacting on this difference include the use of different Tanita body fat analysers and variations in age and the proportion fat in the subjects of each sample.
In both the Parker et al. [8] and current study the manufacturer's undisclosed equations were used for body composition estimation. When considering the individual error in BIA estimates it would appear that applicability of these prediction equations is confounded by a number of intra- and inter-individual differences that result in invalid body composition estimates in a large number of children, especially in the overweight and obese. Previous studies have demonstrated that standard hand-to-foot BIA impedance measurements are heavily influenced by disproportionate body segmental contribution, with the distal regions of the arms and legs accounting for the largest proportion of total body impedance and the trunk accounting for the lowest [23, 24]. Fuller and Elia [23] demonstrated that the forearm and lower leg, while only proportionally representing 1.3% and 3.7% of body mass, accounted for 25.0% and 31.5% of the total body impedance measurement. In contrast, the trunk, proportionally representing 46.2% of body mass, only produced a 10.0% contribution to total body impedance. The findings of Fuller and Elia [23] and Lukaski [24] are of particular concern for foot-to-foot BIA where, because impedance is only measured across the lower limbs, the greatest relative contribution to total impedance values will be from the lower leg. Furthermore, it was shown previously that the relative influence of the limbs on bioelectrical properties of the whole body is significantly related to the difference between methods [25]. The multiple regression analysis applied in the present study indicated that FFM per se was a significant factor in the discrepancies observed between techniques, but did not indicate whether or not the amount of FFM was actually an aetiologic influence or if it was simply an empirical association. That FFM may make a contribution to erroneous estimates of body composition has been suggested previously [26], and may be a factor when applying foot-to-foot BIA to over-weight and obese children for at least two possible reasons. Firstly, the body distribution of FFM may be disproportionate in the overweight and obese compared to the subjects used to derive the prediction equations provided. Secondly, it is important to consider that regional distribution of body composition in overweight and obese children may differ to and have greater inter-individual variability than their lean peers. Jurimae et al [27], investigating the influence of anthropometric variables on whole-body resistance in 209 children aged 9 – 11 years, highlighted that a number of girth measurements were significantly related to whole-body resistance values, explaining between 30% and 50% of the variance. Thus, deviations from the assumed proportional contribution of leg impedance values will result in inaccurate prediction, and could partly explain the individual error in BIA body composition estimates found in the present study. However, additional studies are required to quantify the proportional contribution of the lower limb segments during foot-to-foot BIA measurement, from which correction factors may be applicable to potentially improve accuracy of foot-to-foot BIA, as suggested previously for hand-to-foot BIA [25].
When evaluating foot-to-foot BIA, consideration must be given to the theoretical underpinning of the technique. Standard hand-to-foot BIA commonly includes the impedance index (height (cm)2/Z (Ω)) as a statistical parameter within the body composition prediction equation. When performing a Tanita measurement, height is entered into the device, however, it is unknown if and how height is used in the prediction equation as these have not been disclosed by the manufacturer. Theoretically, the sum of leg length would provide a more accurate measurement of conductor length.
In addition to differences in regional body composition distribution individual variability in the intracellular water (ICW) to extracellular water (ECW) ratio may introduce errors into BIA body composition estimates. Due to differences in the type and amount of dissolved electrolytes in ICW and ECW [28], ICW has a higher specific resistivity than ECW [29]. Theoretically, variability in the ICW-to-ECW ratio will alter the relationship between body composition and impedance measurements [29]. In obese subjects, where a relative expansion of the ECW compartment has been reported in women [30] and children [31] this may have important implications for BIA prediction of body composition, especially if adipose tissue is accumulated disproportionately around the body. However, to the knowledge of the authors no studies have investigated variation in the ICW-to-ECW ratio with increasing fatness in children. Furthermore, as noted by Deurenberg et al. [29], ICW-to-ECW ratio is dependent on age, physical activity levels and the phase of menstruation in females.
In conclusion, this is the first study to demonstrate that, when compared to an appropriate criterion measure of body composition, Tanita TBF-310 foot-to-foot BIA was able to provide accurate estimates of group mean values but not of individual body composition assessments in either males or females, which showed considerable discrepancies in a high proportion of subjects. Assessment of body composition must be accurate on an individual basis and across all levels of body fat in order to: correctly identify the overweight and obese; aid development of overweight and obese definitions based on the association between health risks and body fat; further understanding of the relationship between body fat and other risk profile data, such as metabolic, fitness and fat distribution variables; and aid accurate interpretation when body composition measurements are used to standardise or index physiological variables, e.g. basal metabolic rate (BMR) adjustment for FFM. At this time therefore foot-to-foot BIA cannot be recommended for use by researchers, clinicians and practitioners, and even the general public to measure body composition on an individual basis.
References
- 1.Unick JL, Utter AC, Schumm S, et al. Evaluation of legto-leg BIA in assessing body composition in high-school-aged males and females. Res Sports Med. 2006;14:301–13. doi: 10.1080/15438620600992585. [DOI] [PubMed] [Google Scholar]
- 2.Azcona C, Koek N, Fruhbeck G. Fat mass by air-displacement plethysmography and impedance in obese/non-obese children and adolescents. Int J Pediatr Obes. 2006;1:176–82. doi: 10.1080/17477160600858740. [DOI] [PubMed] [Google Scholar]
- 3.Lazzer S, Boirie Y, Meyer M, et al. Evaluation of two foot-to-foot bioelectrical impedance analysers to assess body composition in overweight and obese adolescents. Br J Nutr. 2003;90:987–92. doi: 10.1079/bjn2003983. [DOI] [PubMed] [Google Scholar]
- 4.Tyrrell VJ, Richards G, Hofman P, et al. Foot-to-foot bioelectrical impedance analysis: a valuable tool for the measurement of body composition in children. Int J Obes. 2001;25:273–8. doi: 10.1038/sj.ijo.0801531. [DOI] [PubMed] [Google Scholar]
- 5.Goldfield GS, Cloutier P, Mallory R, et al. Validity of foot-to-foot bioelectrical impedance analysis in over-weight and obese children and parents. J Sports Med Phys Fitness. 2006;46:447–53. [PubMed] [Google Scholar]
- 6.Sung RYT, Lau P, Yu CW, et al. Measurement of body fat using leg to leg bioimpedance. Arch Dis Child. 2001;85:263–7. doi: 10.1136/adc.85.3.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lohman TG. Applicability of body composition techniques and constants for children and youths. In: Pandolf KB, editor. Exercise and Sport Sciences Reviews. Macmillan; New York: 1986. pp. 325–57. [PubMed] [Google Scholar]
- 8.Parker L, Reilly JJ, Slater C, et al. Validity of six field and laboratory methods for measurement of body composition in boys. Obes Res. 2003;11:852–8. doi: 10.1038/oby.2003.117. [DOI] [PubMed] [Google Scholar]
- 9.Gately PJ, Radley D, Cooke CB, et al. Comparison of body composition methods in overweight and obese children. J Appl Physiol. 2003;95:2039–46. doi: 10.1152/japplphysiol.00377.2003. [DOI] [PubMed] [Google Scholar]
- 10.Roemmich JN, Clark PA, Weltman A, et al. Alterations in growth and body composition during puberty. I. Comparing multicompartment body composition models. J Appl Physiol. 1997;83:927–35. doi: 10.1152/jappl.1997.83.3.927. [DOI] [PubMed] [Google Scholar]
- 11.Wells JCK, Fuller NJ, Dewit O, et al. Four-component model of body composition in children: density and hydration of fat-free mass and comparison with simpler models. Am J Clin Nutr. 1999;69:904–12. doi: 10.1093/ajcn/69.5.904. [DOI] [PubMed] [Google Scholar]
- 12.Sopher AB, Thorton JC, Wang J, et al. Measurement of percentage of body fat in 411 children and adolescents: a comparison of dual-energy x-ray absorptiometry with a four-compartment model. Pediatrics. 2004;113:1285–90. doi: 10.1542/peds.113.5.1285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wong WW, Hergenroeder AC, Stuff JE, et al. Evaluating body fat in girls and female adolescents: advantages and disadvantages of dual-energy X-ray absorptiometry. Am J Clin Nutr. 2002;76:384–9. doi: 10.1093/ajcn/76.2.384. [DOI] [PubMed] [Google Scholar]
- 14.Gately PJ, Cooke CB, Barth JH, et al. Children's residential weight-loss programs can work: a prospective cohort study of short-term outcomes for overweight and obese children. Pediatrics. 2005;116:73–7. doi: 10.1542/peds.2004-0397. [DOI] [PubMed] [Google Scholar]
- 15.Cole TJ, Freeman JV, Preece MA. Body mass index reference curves for the UK, 1990. Arch Dis Child. 1995;73:25–9. doi: 10.1136/adc.73.1.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dempster P, Aitkens S. A new air displacement method for the determination of human body composition. Med Sci Sports Exerc. 1995;27:1692–7. [PubMed] [Google Scholar]
- 17.McCrory MA, Gomez TD, Bernauer EM, et al. Evaluation of a new air displacement plethysmograph for measuring human body composition. Med Sci Sports Exerc. 1995;27:1686–91. [PubMed] [Google Scholar]
- 18.Fields DA, Hull HR, Cheline AJ, et al. Child-specific thoracic gas volume prediction equations for air-displacement plethysmography. Obes Res. 2004;12:1797–1804. doi: 10.1038/oby.2004.223. [DOI] [PubMed] [Google Scholar]
- 19.Coward WA. Calculation of pool sizes and flux rates. In: Prentice AM, editor. The doubly-labelled water method for measuring energy expenditure. Technical recommendations for use in humans. International Dietary Energy Consultancy Group, International Atomic Energy Agency; Vienna: 1990. pp. 48–68. [Google Scholar]
- 20.Hoffman DJ, Sawaya AL, Coward WA, et al. Energy expenditure of stunted and nonstunted boys and girls living in the shantytowns of Sao Paulo, Brazil. Am J Clin Nutr. 2000;72:1025–31. doi: 10.1093/ajcn/72.4.1025. [DOI] [PubMed] [Google Scholar]
- 21.Fuller NJ, Jebb SA, Laskey MA, et al. Four-component model for the assessment of body composition in humans: comparison with alternative methods, and evaluation of the density and hydration of fat-free mass. Clin Sci. 1992;82:687–93. doi: 10.1042/cs0820687. [DOI] [PubMed] [Google Scholar]
- 22.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–10. [PubMed] [Google Scholar]
- 23.Fuller NJ, Elia M. Potential use of bioelectrical impedance of the `whole body' and of body segments for the assessment of body composition: comparison with densitometry and anthropometry. Eur J Clin Nutr. 1989;43:779–91. [PubMed] [Google Scholar]
- 24.Lukaski HC. Biological indexes considered in the derivation of the bioelectrical impedance analysis. Am J Clin Nutr. 1996;64:S397–404. doi: 10.1093/ajcn/64.3.397S. [DOI] [PubMed] [Google Scholar]
- 25.Fuller NJ, Fewtrell MS, Dewit O, et al. Segmental bioelectrical impedance analysis in children aged 8 - 12 y: 1. The assessment of whole-body composition. Int J Obes. 2002;26:684–91. doi: 10.1038/sj.ijo.0801988. [DOI] [PubMed] [Google Scholar]
- 26.Lohman TG, Going SB, Hewitt MJ, et al. Correlation of residual error with fat-free body and percent fat using bioelectrical impedance equations. Med Sci Sports Exerc. 1990;22:S109. [Google Scholar]
- 27.Jurimae T, Leppik A, Jurimae J. Influence of anthropometric variables to the whole-body resistance in pre-adolescent children. In: Jurimae T, Hills AP, editors. Body composition assessment in children and adolescents. Med Sports Sci. Karger; Basel: 2001. pp. 61–70. [Google Scholar]
- 28.Forbes GB. Human body composition. Growth, Aging, Nutrition, and Activity. Springer-Verlag; New York: 1987. [Google Scholar]
- 29.Deurenberg P. The dependency of bioelectrical impedance on intra- and extra-cellular water distribution. In: Kral JG, Van Itallie TB, editors. Recent developments in body composition analysis: methods and applications. Smith-Gordon; Great Britain: 1993. pp. 43–8. [Google Scholar]
- 30.Waki M, Kral JG, Mazariegos M, et al. Relative expansion of extracellular fluid in obese vs. nonobese women. Am J Physiol. 1991;261:E199–203. doi: 10.1152/ajpendo.1991.261.2.E199. [DOI] [PubMed] [Google Scholar]
- 31.Battistini N, Virgili F, Severi S, et al. Relative expansion of extracellular water in obese vs. normal children. J Appl Physiol. 1995;79:94–6. doi: 10.1152/jappl.1995.79.1.94. [DOI] [PubMed] [Google Scholar]