To the Editor
Impaired subjective sleep quality is a major clinical symptom of fibromyalgia (FM).1 Electroencephalographic (EEG) features such as the alpha-delta sleep pattern2 and cyclic alternating pattern (CAP) 3 have been proposed as markers of disturbed sleep in FM. A single-lead continuous electrocardiogram (ECG) 4 can be used to generate an automated “sleep spectrogram,” based on mathematical analysis of the coupling between heart rate variability and the respiratory modulation of QRS waveform on a beat-to-beat basis. The method permits assessment of high and low frequency cardiopulmonary coupling regimes. These do not correlate with standard NREM stages or delta power, but with non-CAP and CAP EEG, respectively.
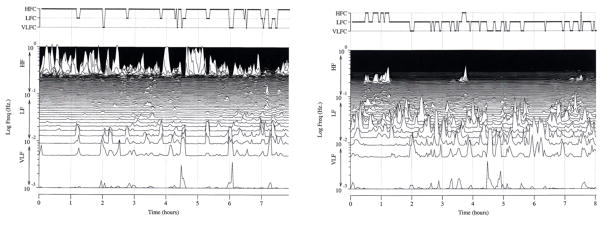
In a case-control design, we retrospectively analyzed continuous ECG recordings collected during polysomnography (PSG) from 14 patients with FM and 13 matched controls. As previously reported,5 these data sets did not reveal differences in conventional PSG measures. We report here (Table 1 and Figure 1) that elevated-low frequency coupling (the minimum low-frequency power be > 0.05 normalized units and that the low to high frequency ratio be >30), a distinct sleep spectrogram finding that correlates with manually scored apneas and hypopneas6, was significantly increased in fibromyalgia patients (Mann-Whitney test p=0.03). Using a minimum threshold of 50% high frequency coupling (selected based on a 48% mean among 2,747 Sleep Heart Health Study subjects with ≤ 5 apneas or hypopneas per hour of sleep), fibromyalgia patients were significantly less likely than controls to have stable sleep (Pearson Chi2 = 4.6; p=0.03). Two-week pain diary scores completed by the subjects correlated in expected directions with both high and elevated-low frequency coupling (Spearman rho=−0.35, p=0.03 and rho=0.44, p=0.01, respectively).
Table 1.
ECG-derived sleep spectrogram and fibromyalgia
| Spectrogram output | Fibromyalgia patients (Mean ± S.D.)1 | Control subjects (Mean ± S.D.)1 | P value (rank-sum test) |
|---|---|---|---|
| High frequency coupling | 30.8 ± 26.7 | 47.8 ± 21.5 | 0.08 |
| Low frequency coupling | 50 ± 24 | 34 ± 19 | 0.1 |
| elevated-low frequency coupling | 25.6 ± 18.5 | 12.4 ± 10.8 | 0.03 |
| Very low frequency coupling | 17.19 ± 8.7 | 17.18 ± 5.3 | 0.6 |
% of signal windows in the sleep period
Figure. Sleep spectrogram in a healthy (left) and a fibromyalgia (right) subject.
Note the dominance of high frequency coupling, which occurs periodically across the entire night in the healthy subject. This finding is distinct from slow wave sleep or delta power distributions, which are concentrated in the first half of the night. Note the paucity of time spent in high frequency coupling in the fibromyalgia patient. On the Y axis is plotted the log frequency representation of the coupling frequencies to allow differentiation of high frequency (HF), low frequency (LF) and very low frequency (VLF) bands; elevated-LFC is a subset of LFC. VLFC periods correlate with wake, REM or sleep-wake transitions.
Fine differences extractable from the EEG may not be possible from the ECG-based method, due in substantial part to the sampling/scoring windows, one-minute non-overlapping window for the EEG and 8.5-minute windows advancing by 2.1 minutes for the ECG-based spectrograms. This overlapping window procedure can be a limitation, by not allowing finer resolution, but a strength, by allowing estimates of mean state-related activity.
Wake-promoting influences may be excessively active during sleep in FM and could reflect increased traffic in nociceptive afferents or enhanced central nociceptive processing. The EEG-CAP approach, unlike the ECG-based approach, does not factor in respiratory influences on state. The fact that both ECG and EEG approaches yield consistent findings in this syndrome further solidifies the hypothesis of altered sleep stability in fibromyalgia.
Sleep spectrograms may provide low-cost, clinically useful insight into abnormal sleep in FM, and possibly into monitoring the effects of therapy.
Acknowledgments
Supported in part by grants from Pfizer, Inc., the Arthritis Foundation, Michigan Chapter, the Periodic Breathing Foundation, the G. Harold and Leila Y. Mathers Foundation, and the NIH-sponsored Research Resource for Complex Physiologic Signals (UO1EB008577). This work was performed at the University of Michigan, Ann Arbor, Michigan and the Beth Israel Deaconess Medical Center, Boston, Massachusetts.
Footnotes
Conflict of Interest
The following authors have a conflict of interest: Robert Joseph Thomas, M.D., Joseph E. Mietus, B.S., Chung-Kang Peng, Ph.D. and Ary L. Goldberger, M.D. They are all co-inventors of the sleep spectrogram technique, which is patented and licensed to Embla, Inc by the Beth Israel Deaconess Medical Center. All listed are covered by formal institutional royalty sharing properties. The payments in the past year have been less than $ 10,000. CKP is co-owner of DynaDx, Inc, a firm dedicated to the development of dynamic physiological assessments tools. ALG and JEM are consultants to DynaDx. None of the other authors have a relevant conflict of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Robert Joseph Thomas, Division of Pulmonary, Critical Care & Sleep, Department of Medicine, Beth Israel Deaconess Medical Center & Harvard Medical School, Boston, Massachusetts.
Joseph E. Mietus, Division of Interdisciplinary Medicine and Biotechnology, Beth Israel Deaconess Medical Center & Harvard Medical School and the Wyss Institute for Biologically Inspired Engineering at Harvard University Boston, Massachusetts
Chung-Kang Peng, Division of Interdisciplinary Medicine and Biotechnology, Beth Israel Deaconess Medical Center & Harvard Medical School and the Wyss Institute for Biologically Inspired Engineering at Harvard University Boston, Massachusetts
Ary L. Goldberger, Division of Interdisciplinary Medicine and Biotechnology, Beth Israel Deaconess Medical Center & Harvard Medical School and the Wyss Institute for Biologically Inspired Engineering at Harvard University Boston, Massachusetts
Leslie J. Crofford, Division of Rheumatology & Women’s Health, Department of Internal Medicine, University of Kentucky, Lexington, Kentucky
Ronald D. Chervin, Sleep Disorders Center, Department of Neurology
References
- 1.Bigatti SM, Hernandez AM, Cronan TA, Rand KL. Sleep disturbances in fibromyalgia syndrome: Relationship to pain and depression. Arthritis Rheum. 2008;59:961–7. doi: 10.1002/art.23828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Branco J, Atalaia A, Paiva T. Sleep cycles and alpha-delta sleep in fibromyalgia syndrome. J Rheumatol. 1994;21:1113–7. [PubMed] [Google Scholar]
- 3.Rizzi M, Sarzi-Puttini P, Atzeni F, et al. Cyclic alternating pattern: a new marker of sleep alteration in patients with fibromyalgia? J Rheumatol. 2004;31:1193–9. [PubMed] [Google Scholar]
- 4.Thomas RJ, Mietus JE, Peng CK, Goldberger AL. An electrocardiogram-based technique to assess cardiopulmonary coupling during sleep. Sleep. 2005;28:1151–61. doi: 10.1093/sleep/28.9.1151. [DOI] [PubMed] [Google Scholar]
- 5.Burns JW, Crofford LJ, Chervin RD. Sleep stage dynamics in fibromyalgia patients and controls. Sleep Med. 2008;9:689–96. doi: 10.1016/j.sleep.2007.10.022. [DOI] [PubMed] [Google Scholar]
- 6.Thomas RJ, Mietus JE, Peng CK, et al. Differentiating obstructive from central and complex sleep apnea using an automated electrocardiogram-based method. Sleep. 2007;30:1756–69. doi: 10.1093/sleep/30.12.1756. [DOI] [PMC free article] [PubMed] [Google Scholar]