Abstract
Episodic ataxia type 2 (EA-2) is an inherited disorder that is characterized by intermittent vertigo, ataxia, and interictal gaze-evoked nystagmus. Although abnormalities associated with this disorder have been found in the CACNA1A gene encoding the alpha1A (Cav2.1) subunit of the P/Q-type calcium channel, there are few reports of genetically confirmed EA-2 in Korea. In 1998, a Korean family with acetazolamide-responsive hereditary paroxysmal ataxia was reported, but the genetic background was not defined at that time. In the present study we performed direct sequencing of the entire exons and their flanking intronic sequences of the CACNA1A gene and found a deletion mutation (c.2042_2043delAG).
Keywords: Episodic ataxia type 2, CACNA1A, Korea
Several types of channelopathy, including spinocerebellar ataxia, familial hemiplegic migraine, and episodic ataxia (EA), may manifest with intermittent or progressive dizziness and ataxia. EA type 2 (EA-2) is an autosomal dominant disorder that is characterized by intermittent vertigo, ataxia, and interictal gaze-evoked nystagmus. Episodes may develop spontaneously or may be triggered by stress and exertion. The underlying cause of EA-2 is a genetic alteration of the voltage-dependent calcium channel (CACNA1A). Acetazolamide markedly reduces the number of attacks, possibly by stabilizing the ion channels through pH changes in brain tissue.1 Previously, one familial case with EA-2 and spinocerebellar ataxia type 6 (SCA6) was reported in association with CAG repeat expansion, and another sporadic case with EA-2 was found to have a balanced translocation in CACNA1A.2,3 However, isolated EA-2 due to a deletion in CACNA1A has not been documented in Korea. In 1998, our group reported on a Korean family with acetazolamide-responsive hereditary paroxysmal ataxia, but the genetic background was not defined at that time.4 In the present study we direct sequenced the entire exons and the flanking intronic sequences of the CACNA1A gene, and found a deletion mutation (c.2042_2043delAG). Here we report the first genetically proven Korean family with EA-2 over three generations that is attributable to a deletion in CACNA1A.
PATIENTS AND METHOD
Patients
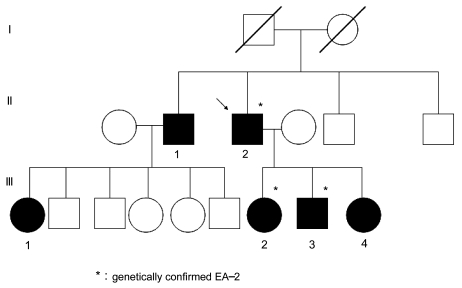
A 55-year-old man had experienced intermittent episodes of ataxia and dysarthria since the age of 15 years, which were precipitated mostly by emotional stress, exertion, exercise, consumption of hot food, and hot showers. He reported that the severity and number of attacks had increased with age. His past medical history was unremarkable. Five of his family members had similar symptoms (Fig. 1). Between the attacks, physical, neurological, and laboratory findings were normal except for subtle gaze-evoked nystagmus. During the episodes, he showed aggravated gaze-evoked nystagmus, dysarthria, and ataxia involving both arms and legs. The episodes lasted 30 min to 1 hour. Acetazolamide at 750 mg per day markedly decreased the severity and frequency of the episodes. The detailed clinical features of this patient and his family members have been reported previously.4
Figure 1.
Pedigree of a family with episodic ataxia type 2.
Genetic Analyses
After obtaining their informed consent to participate, direct sequencing analysis was applied to three family members to detect CACNA1A gene mutations. Genomic DNA was extracted from peripheral blood leukocytes using the Wizard Genomic DNA Purification Kit following the manufacturer's instructions (Promega, Madison, WI, USA). All five coding exons of the CACNA1A gene and their flanking intronic regions were amplified using primer sets designed by the authors (available on request). The polymerase chain reaction15 was performed with a thermal cycler (model 9700, Applied Biosystems, Foster City, CA, USA) as follows: initial incubation at 94℃ for 5 min, followed by 32 cycles of denaturation at 94℃ for 30's, annealing at 60℃ for 30's, and extension at 72℃ for 30's. The amplicon (5µL) was treated with 10 U of shrimp alkaline phosphatase and 2 U of exonuclease I (USB, Cleveland, OH, USA) at 37℃ for 15 min, and was incubated at 80℃ for 15 min for enzyme inactivation. Cycle sequencing was performed on an ABI Prism 3100 Genetic Analyzer with the BigDye Terminator Cycle Sequencing Ready Reaction kit (Applied Biosystems).
RESULTS
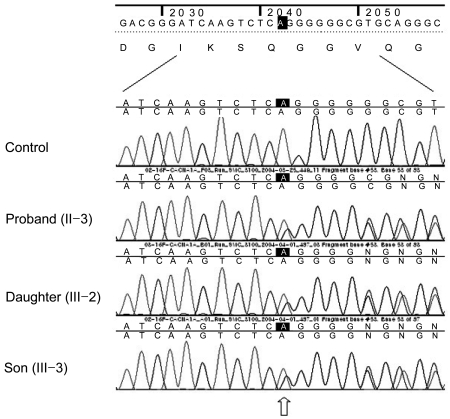
Direct sequencing of the entire exons and the flanking intronic sequences of the CACNA1A gene in the proband (II-2; Fig. 2) revealed a heterozygous deletion mutation in exon 16 (c.2042_2043delAG base on the reference mRNA sequence, NM_000068; Fig. 2), resulting in a frameshift in the protein level (p.Gln681ArgfsX16). This variation was also found in the patient's affected son and one of his two affected daughters. The other family members declined the genetic analysis.
Figure 2.
Mutation analysis of the CACNA1A gene. Direct sequencing of exon 16 shows overlapped peaks (arrow) from nucleotide position 2042 due to a heterozygous 2-base-pair deletion (c.2042_2043delAG; p.Gln681ArgfsX16). The proband's son and one of his two daughters also had the same mutation.
DISCUSSION
Hereditary EA shows autosomal dominant inheritance. In EA type 1 (EA-1), the patient shows paroxysmal ataxia with myokymia or myotonia lasting several seconds to minutes.5 Genetic abnormalities include point mutations in a potassium channel gene, KCNA1, on chromosome 12p.6 Attacks of EA-2 last longer than those of EA-1. EA-2 is associated with mutations in a voltage-dependent calcium channel gene, CACNA1A, which is located on chromosome 19p and codes for the main transmembrane component of a neuronal calcium channel.7 This gene is expressed throughout the nervous system, but is especially common in the cerebellum and at the neuromuscular junction.8 Other genetic diseases involving CACNA1A include SCA6 and familial hemiplegic migraine.9 The type of mutation is known to be only weakly associated with the clinical manifestation or severity in EA-2,10 but CAG repeat expansion is found more commonly in SCA6. So far, two genetically proven cases of EA-2 have been reported in Korea. The first report described a family with EA-2 and SCA6 due to CAG repeat expansion in the CACNA1A calcium-channel gene.2 That family comprised both EA-2 and SCA6 patients with the same mutation, suggesting that SCA6 and EA-2 are allelic disorders. The second report was of a 26-year-old man with EA-2 whose genetic analysis disclosed reciprocal balanced translocation involving CACNA1A.3 None of his family members had EA-2. The patients in our current family had similar clinical manifestations as the patients reported previously; all of them had intermittent episodes of vertigo and ataxia, which had started before the age of 20 years. The frequency and severity of attacks were attenuated by acetazolamide therapy. In our patients, EA-2 was caused by a deletion in exon 16 of the CACNA1A gene (c.2042,_2043delAG), which has been reported previously.11
The unique feature of our patients was that the symptoms were induced or aggravated by hot food or a hot shower. This is the first description of EA provoked by a change in body temperature. Neurological symptoms provoked by a rise in the core body temperature have been reported in multiple sclerosis as Uhthoff's phenomenon. This rare phenomenon manifests as a transient visual loss, motor weakness, or dysphonia attributable to a rise in core body temperature. The motor weakness associated with Uhthoff's phenomenon has been ascribed to a conduction delay in multiple sclerosis patients.12 There has been a report on temporary hearing loss in an otherwise healthy girl induced by an increase in her core body temperature.13 Auditory brainstem responses revealed an absence of neural synchrony during the attack.13 The symptoms in our patients may have been related to a central conduction delay induced by a temperature change; however, there is currently no known relationship between calcium channelopathy and temperature-dependent conduction delay. More case reports and biochemical studies are eeded to elucidate the mechanisms underlying this condition.
References
- 1.Bain PG, O'Brien MD, Keevil SF, Porter DA. Familial periodic cerebellar ataxia: a problem of cerebellar intracellular pH homeostasis. Ann Neurol. 1992;31:147–154. doi: 10.1002/ana.410310205. [DOI] [PubMed] [Google Scholar]
- 2.Koh SH, Kim HT, Kim SH, Lee GY, Kim J, Kim MH. Spinocerebellar ataxia type 6 and episodic ataxia type 2 in a Korean family. J Korean Med Sci. 2001;16:809–813. doi: 10.3346/jkms.2001.16.6.809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yun S, Chang YJ, Jung SC, Kwon JW, Lee GH, Lee CM, et al. Episodic ataxia type 2 with downbeating nystagmus caused by mutation in the CACNA1A: a case report. J Korean Neurol Assoc. 2005;23:399–401. [Google Scholar]
- 4.Kim HJ, Jeon BS. Acetazolamide-responsive hereditary paroxysmal ataxia: report of a family. J Korean Med Sci. 1998;13:196–200. doi: 10.3346/jkms.1998.13.2.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vaamonde J, Artieda J, Obeso JA. Hereditary paroxysmal ataxia with neuromyotonia. Mov Disord. 1991;6:180–182. doi: 10.1002/mds.870060218. [DOI] [PubMed] [Google Scholar]
- 6.Browne DL, Gancher ST, Nutt JG, Brunt ER, Smith EA, Kramer P, et al. Episodic ataxia/myokymia syndrome is associated with point mutations in the human potassium channel gene, KCNA1. Nat Genet. 1994;8:136–140. doi: 10.1038/ng1094-136. [DOI] [PubMed] [Google Scholar]
- 7.Mori Y, Friedrich T, Kim MS, Mikami A, Nakai J, Ruth P, et al. Primary structure and functional expression from complementary DNA of a brain calcium channel. Nature. 1991;350:398–402. doi: 10.1038/350398a0. [DOI] [PubMed] [Google Scholar]
- 8.Fletcher CF, Lutz CM, O'Sullivan TN, Shaughnessy JD, Jr, Hawkes R, Frankel WN, Copeland NG, Jenkins NA. Absence epilepsy in tottering mutant mice is associated with calcium channel defects. Cell. 1996;87:607–617. doi: 10.1016/s0092-8674(00)81381-1. [DOI] [PubMed] [Google Scholar]
- 9.Harding AE. Clinical features and classification of inherited ataxias. Adv Neurol. 1993;61:1–14. [PubMed] [Google Scholar]
- 10.Jen J, Kim GW, Baloh RW. Clinical spectrum of episodic ataxia type 2. Neurology. 2004;62:17–22. doi: 10.1212/01.wnl.0000101675.61074.50. [DOI] [PubMed] [Google Scholar]
- 11.Denier C, Ducros A, Vahedi K, Joutel A, Thierry P, Ritz A, et al. High prevalence of CACNA1A truncations and broader clinical spectrum in episodic ataxia type 2. Neurology. 1999;52:1816–1821. doi: 10.1212/wnl.52.9.1816. [DOI] [PubMed] [Google Scholar]
- 12.Humm AM, Beer S, Kool J, Magistris MR, Kesselring J, Rosler KM. Quantification of Uhthoff's phenomenon in multiple sclerosis: a magnetic stimulation study. Clin Neurophysiol. 2004;115:2493–2501. doi: 10.1016/j.clinph.2004.06.010. [DOI] [PubMed] [Google Scholar]
- 13.Cianfrone G, Turchetta R, Mazzei F, Bartolo M, Parisi L. Temperature-dependent auditory neuropathy: is it an acoustic Uhthoff-like phenomenon? A case report. Ann Otol Rhinol Laryngol. 2006;115:518–527. doi: 10.1177/000348940611500706. [DOI] [PubMed] [Google Scholar]