Abstract
Background
This study was designed to determine risk factors and potential harm associated with medication errors at hospital admission.
Methods
Study pharmacist and hospital-physician medication histories were compared with medication orders to identify unexplained history and order discrepancies in 651 adult medicine service inpatients with 5,701 prescription medications. Discrepancies resulting in order changes were considered errors. Logistic regression was used to analyze the association of patient demographic and clinical characteristics including patients’ number of pre-admission prescription medications, pharmacies, prescribing physicians and medication changes; and presentation of medication bottles or lists. These factors were tested after controlling for patient demographics, admitting service and severity of illness.
Results
Over one-third of study patients (35.9%) experienced 309 order errors; 85% of patients had errors originate in medication histories, and almost half were omissions. Cardiovascular agents were commonly in error (29.1%). If undetected, 52.4% of order errors were rated as potentially requiring increased monitoring or intervention to preclude harm; 11.7% were rated as potentially harmful. In logistic regression analysis, patient’s age ≥65 [odds ratio (OR), 2.17; 95% confidence interval (CI), 1.09–4.30] and number of prescription medications (OR, 1.21; 95% CI, 1.14–1.29) were significantly associated with errors potentially requiring monitoring or causing harm. Presenting a medication list (OR, 0.35; 95% CI, 0.19–0.63) or bottles (OR, 0.55; 95% CI, 0.27–1.10) at admission was beneficial.
Conclusion
Over one-third of the patients in our study had a medication error at admission, and of these patients, 85% had errors originate in their medication histories. Attempts to improve the accuracy of medication histories should focus on older patients with a large number of medications. Primary care physicians and other clinicians should help patients utilize and maintain complete, accurate and understandable medication lists.
KEY WORDS: medication reconciliation, medication errors, medication history taking
Obtaining medication histories among hospitalized patients is an error-prone process.1–11 Factors affecting the quality and completeness of medication histories at the time of hospital admission include language and cultural barriers, which can be compounded by multiple prescribing physicians or use of multiple pharmacies due to economic, insurance and/or convenience factors.
Older patients taking a large number of medications may not recall indications or doses. Look-alike/sound-alike medications increase the risk of inaccurate histories, especially if patients are unclear about the rationale for use.12 Patients or their surrogates with low health literacy may be poor historians or may withhold medication compliance information.13,14 Clinician time constraints and interview skills may also affect the quality of medication histories. Even medication lists in electronic medical records (EMR) can lag behind prescription changes and be incomplete.11
This prospective study was designed to identify and analyze the frequency and types of admission medication errors in our hospital’s medicine service. Ratings for each error’s potential for patient harm during hospitalization are presented. Finally, the complex association of medication errors with individual patient risk factors was analyzed.
METHODS
Sample Selection
This study was conducted at Northwestern Memorial Hospital in Chicago, Illinois, and approved by the Institutional Review Board of Northwestern University. The study was designed to obtain in-depth, pharmacist interviews within 24–48 h of hospital admission with at least 400 adult medicine service patients. Our sample size was derived from preliminary power calculations indicating that a two-group chi-square test with p < 0.05 two-sided significance level will have 88% power to detect the difference between a group of patients with a risk factor proportion of 0.20 and another group of patients with a risk factor proportion of 0.35 (odds ratio of 2.15) when the sample sizes are 134 and 267, respectively (a total sample size of 400).
Over 14 months in 2006–2007, study pharmacists obtained a list of patients admitted the previous day. Patients with limited English proficiency (LEP), reporting their understanding of English as “fair,” “poor” or “not at all” during hospital registration (less than 5% of medicine service admissions), were prioritized and interviewed using a language line phone service. All other eligible, sampled inpatients were approached sequentially, based on daily generated random numbers, by one of two study pharmacists during their available (Monday through Friday) research time. Any patient who was too ill or unwilling to participate and for whom the family/caregiver was unavailable, who was unavailable to be interviewed despite two attempts due to tests or procedures, transferred to another service or already discharged was excluded.
Medication History Interview
Prior to interviewing the patient, the study pharmacist reviewed the patient’s EMR and recorded the physician-obtained medication history, admission medication orders and the patient’s demographic information. A comprehensive interview with the patient and/or their caregiver was then conducted by the study pharmacist to obtain the patient’s current medication regimen. The study pharmacist inquired about all prescriptions, investigational therapies, over-the-counter medications, vitamins, herbals and any other products used to supplement the patient’s health. Other sources of information included the patient’s prescription bottle labels, self-prepared medication lists and/or consultation with community pharmacies. If the patient was previously hospitalized or cared for by a hospital or university-affiliated outpatient physician utilizing the EMR system within their clinic, available discharge summaries and outpatient medication lists were also reviewed.
Reconciliation of Medication Histories and Admission Medication Orders
Study pharmacist-obtained medication histories were compared with hospital physician-obtained medication histories and admission medication orders. Progress notes and changes made to patients’ medication orders since admission were reviewed to identify intentional discrepancies (e.g., formulary substitutions or modifications to pre-admission medications in response to a patient’s clinical status). The prescribing physician was then contacted regarding remaining unexplained discrepancies. Clarifications of unexplained discrepancies resulting in order changes were considered medication errors. This restrictive error definition should be more clinically meaningful as changes would be deemed appropriate to incorporate into patients’ treatment plans.
All medication results reported are for prescription medications only. Over-the-counter medications and herbals were excluded from analysis, although aspirin taken for cardiovascular purposes was classified as a “prescription” medication for analysis, similar to other published studies.2
Classification of Medication Errors and Potential Harm Assessment
Medication errors were classified by drug class and type of error: omission of a pre-admission prescription medication, incorrect addition of a medication not part of the patient’s pre-admission regimen (commission), different dose, different route and different frequency or different medication (within the same drug class). Each medication error was rated for its potential to cause harm during hospitalization if the error had not been identified and corrected. The National Coordinating Council for Medication Error Reporting and Prevention (NCC MERP) Index for Categorizing Medication Errors was adapted and utilized for rating potential harm.15,16 This nationally recognized NCC MERP harm level taxonomy was chosen because it is widely utilized by hospitals participating in the largest adverse drug event reporting system developed by the United States Pharmacopeia (USP).17 NCC MERP criteria were collapsed to group errors into three categories: (1) no potential harm (NCC MERP category C); (2) monitoring or intervention potentially required to preclude harm (NCC MERP category D); (3) potential harm (NCC MERP categories E and above).5
Ratings of potential rather than actual harm are based on face validity only. The two study pharmacists collaboratively rated each medication error for potential harm followed by blinded, independent review by one of two board-certified internists. Pharmacist-physician harm ratings were then analyzed to determine inter-rater reliability of harm ratings across the three categories. There was a high overall initial agreement rate between pharmacist and physician ratings (Cohen’s kappa = 0.84). Remaining disagreements were independently re-rated by the second board-certified physician to obtain the final harm rating.
Risk Factor Interview
Following the medication interview, the study pharmacist continued with further interview questions to identify risk factors including the number of prescribing physicians involved in the patient’s pre-hospitalization care, number of pharmacies utilized to fill prescriptions and recent changes (additions, deletions or modifications) within the last month to their medications. Study pharmacists also inquired whether patients’ medication bottles and/or medication lists were presented to the health care team upon hospitalization. Study patients lacking at least one prescription medication prior to hospitalization or patients admitted from a nursing home or rehabilitation facility where medications were managed by health care professionals were not evaluated.
Patient Medication Error Risk Factors
For all study patients, demographic factors analyzed for their association with medication errors included patients’ age, sex, race and ethnicity, and LEP, if applicable. Measures of potential clinical and severity of illness factors included the number of home medications, Medicare Diagnosis-Related Group (DRG) case mix index weight, length of stay and whether the patient was transferred to the intensive care unit during hospitalization. Finally, we controlled for whether the admission was to a hospitalist or teaching (resident care) service.
Statistical Analysis
For study patients with complete risk factor interviews, chi-square tests were used to determine the significance of categorical variables and t-tests for continuous variables. Multiple logistic regression analyses were estimated for the combined likelihood of errors rated as either potentially requiring additional monitoring or intervention to preclude harm, or errors rated as potentially harmful. Controlling for the same clinical and demographic variables described above, regression models tested the significance of patients’ multiple pharmacy use, whether multiple physicians were involved in the patient’s pre-hospitalization care, history of recent medication or dosage changes, and whether the patient presented a medication list or bottles on admission. SPSS software version 16 (SPSS Inc., Chicago, IL) was used for all statistical analyses. A p value ≤ 0.05 was considered statistically significant.
RESULTS
Comparison of Patients with and without Medication Order Errors
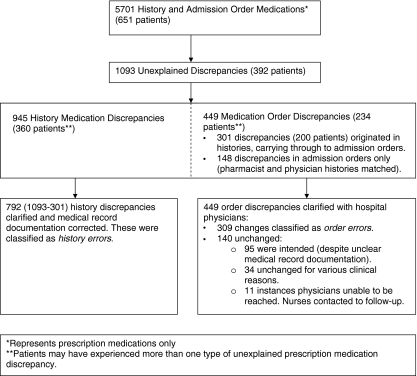
Study pharmacists performed medication history interviews and reconciliation on 651 patients. Figure 1 describes the medication reconciliation process. The mean time per patient for completion of pharmacists’ chart reviews, patient/caregiver interviews, reconciliation and interventions was 21.2 min (SD = 13.2). After clarification with hospital physicians, 309 out of 449 prescription medications flagged as unexplained discrepancies resulted in physician order changes; these were classified as medication order errors. These errors affected 234 (35.9%) study patients; 85% of these patients had medication errors originate in their medication histories and carry through to their inpatient orders. While 90 patients (14%) had a single medication order error, 47 (7%) had two errors, 21 (3%) had three and 13 (2%) had four or more errors. Additionally, 792 unexplained prescription medication history discrepancies were clarified and classified as history errors; documentation was subsequently corrected in patients’ medical records (Figure 1). These historical medications were intentionally not ordered primarily due to patients’ clinical status. However, correction of medication history documentation was important to prevent errors and potential harm when historical medications were reviewed at discharge.
Fig. 1.
Medication reconciliation process (n = 651 patients).
Patient demographic and clinical characteristics are presented in Table 1. The only patient factors with significant univariate association with the frequency of medication errors were older patient age, female sex and a greater number of prescription medications on admission.
Table 1.
Patient Demographics and Clinical Characteristics by Prescription Medication Order Errors (n = 651 patients)
| Characteristic | Patients without errors (row percentages) (N = 417) | Patients with errors (row percentages) (N = 234) | p value |
|---|---|---|---|
| Demographics | |||
| Age, years | <0.0001 | ||
| ≤45 | 154 (78.6%) | 42 (21.4%) | |
| 46–64 | 145 (66.2%) | 74 (33.8%) | |
| ≥65 | 118 (50%) | 118 (50%) | |
| Sex | 0.02 | ||
| Male | 206 (68.9%) | 93 (31.1%) | |
| Female | 211 (59.9%) | 141 (40.1%) | |
| Ethnicity | |||
| White/other | 295 (62.6%) | 177 (37.4%) | 0.20 |
| African-American | 94 (69.1%) | 42 (30.9%) | 0.17 |
| Hispanic | 28 (65.1%) | 15 (34.9%) | 0.88 |
| English proficiency (self-reported) | 390 (64.4%) | 216 (35.6%) | 0.56 |
| Excellent/very good Good/fair/poor/not at all | 27 (60%) | 18 (40%) | |
| Clinical characteristics | |||
| Mean hospital length of stay, days (SD) | 4.83 (±5.54) | 4.91 (±4.07) | 0.85 |
| Admission service | 0.50 | ||
| Hospitalist | 190 (62.7%) | 113 (37.3%) | |
| Teaching/resident | 227 (65.2%) | 121 (34.8%) | |
| Mean Medicare Case Mix Index (final DRG weight) (SD) | 1.14 (±1.23) | 1.20 (±1.45) | 0.58 |
| Intensive care unit (ICU) stay during hospitalization | |||
| Yes | 12 (60%) | 8 (40%) | 0.70 |
| No | 405 (64.2%) | 226 (35.8%) | |
| Mean number of prescription home medications (SD) | 4.56 (±4.14) | 8.95 (±4.62) | <0.0001 |
Error Types, Drug Classes and Potential Harm Ratings
The most frequent type of error was an omission (48.9%) followed by different dose (30.4%) and then by different frequency (11.0%); 7% involved errors in both dose and frequency. The five most common medication classes involved in errors were cardiovascular agents, antidepressants, gastrointestinal agents, neurological agents and anti-diabetics. Classes with the largest proportion of errors included ophthalmic/otic agents, genitourinary agents, neurological agents, antivirals and antidepressants.
Among the 309 prescription medication order errors, 4 (1.3%) were rated as involving potentially longer hospitalization, 32 (10.4%) rated as potentially causing temporary harm, and 162 (52.4%) rated as potentially requiring increased monitoring or intervention to preclude harm. Remaining errors were classified as not likely to have been harmful. Table 2 provides examples of medication errors with potential harm ratings.
Table 2.
Examples of Potential Harm Ratingsa for Prescription Medication Order Errors
| Potential harm rating | Examples of prescription medication order errors |
|---|---|
| No potential harm (NCC MERP category C) | Example 1. Simvastatin 10 mg omitted from physician’s history and admission orders |
| Example 2. Escitalopram 5 mg daily recorded in physician’s history and admission orders. Patient’s community pharmacy verified dose as 10 mg | |
| Example 3. Sucralfate 1,000 mg four times daily ordered at admission. Pharmacist verified patient no longer taking | |
| Potential for increased monitoring or intervention to preclude harm (NCC MERP category D) | Example 1. Baclofen 10 mg every morning and 20 mg every evening recorded in physician’s history. Order omitted despite hospital progress notes to continue |
| Example 2. Lisinopril 20 mg daily recorded in physician’s history and admission orders. Verification with patient and outpatient physician’s records noted frequency was twice daily | |
| Example 3. Glipizide XL 2.5 mg daily recorded in physician’s history and admission orders. Verification with patient and outpatient physician’s records noted medication was glyburide 2.5 mg daily | |
| Potential harm (NCC MERP category E-F) | Example 1. Warfarin 5 mg daily at bedtime recorded in physician’s history and admission orders. Verification with patient and spouse noted dose recently decreased to 4 mg daily at bedtime. (Admission INR 3.2. Ciprofloxacin also ordered as continuation of outpatient therapy) |
| Example 2. Tacrolimus 2 mg twice daily recorded in physician’s history and admission orders. Verification with patient and outpatient physician’s records noted tacrolimus 0.5 mg daily | |
| Example 3. Patient with history of Addison’s disease. Physician’s history listing hydrocortisone 20 mg every morning and 10 mg every evening verified by pharmacist. Prednisone 40 mg every morning and 20 mg every evening ordered instead | |
| Example 4. Digoxin 125 mcg every other day recorded in physician’s history for a hemodialysis patient. Digoxin ordered daily. Pharmacist verified patient’s dose was digoxin 125 mcg three times per week |
aAdapted from the National Coordinating Council for Medication Error Reporting and Prevention (NCC MERP) (www.nccmerp.org)
Logistic Regression Results for Risk Factors
Among the 651 study patients, a further risk factor interview was completed with 428 (65.7%) patients. Excluded patients included 98 patients who lacked a prescription medication prior to admission, 24 patients whose pre-hospital prescription medications were controlled by health professionals, and 101 patients where the risk factor interview could not be completed because of severity of illness or inability to answer all questions. There were no significant differences in study demographic or clinical severity measures between excluded patients and the subset of 428 patients with completed risk factor interviews.
Table 3 presents multiple logistic regression results for the association of each risk factor with the likelihood of a patient having a medication error rated as either potentially requiring monitoring or intervention (n = 162) or potentially causing harm (n = 36). These regression results differed little from models solely based on estimating the likelihood of the smaller (n = 36) number of potentially harmful errors. Advanced age (≥65 years old) (OR = 2.17; 95% CI, 1.09–4.30) and increased number of prescription medications (OR = 1.21; 95% CI, 1.14–1.29) were the only risk factors independently associated with an increased risk for these errors. Presenting a medication list (OR = 0.35; 95% CI, 0.19–0.63) upon admission was a significant protective factor for avoiding errors. Although presenting medication bottles was also beneficial, it was not quite statistically significant (OR = 0.55; 95% CI, 0.27–1.10).
Table 3.
Multiple Logistic Regression Results: Risk Factors for Patients with Prescription Medication Order Errors Rated as Potentially Requiring Monitoring or Intervention or Potentially Causing Harm (N = 428)
| Variables (number of patients except where noted) | Odds ratio (95% confidence interval) |
|---|---|
| Demographics | |
| Age ≥65 years (n = 165) | 2.17 (1.09–4.30) |
| Age ≥45–64 years (n = 148) | 1.36 (0.69–2.69) |
| Age <45 (n = 115) | 1.0 Reference |
| Male (n = 180) | 0.89 (0.54–1.47) |
| Ethnicity-Hispanic (n = 28) | 0.92 (0.32–2.62) |
| Ethnicity-African American (n = 88) | 1.12 (0.67–2.06) |
| Ethnicity-White/other (n = 313) | 1.0 Reference |
| Limited English proficiency (n = 29) | 1.1 (0.42–2.84) |
| Clinical characteristics | |
| Admitted to hospitalist service (n = 210) vs. teaching service (n = 218) upon hospitalization | 0.99 (0.60–1.61) |
| Final DRG weight (range = 0.27–6.139) | 0.83 (0.55–1.25) |
| ICU stay during hospitalization (n = 14) | 1.33 (0.24–7.38) |
Number scheduled pre-admission prescription medications (range = 0–27;  ) ) |
1.21 (1.14–1.29) |
| Number of different outpatient physicians prescribing patient’s medications | 1.04 (0.83–1.29) |
| Patient presented a medication list upon admission (n = 129) | 0.35 (0.19–0.63) |
| Patient presented medication bottle(s) upon admission (n = 69) | 0.55 (0.27–1.10) |
| Changes to pre-admission prescription medications within last month (n = 182) | 1.57 (0.96–2.55) |
| Patient utilizes different outpatient pharmacies to fill prescription medications (n = 86) | 0.51 (0.27–0.97) |
DISCUSSION
Study Implications for Improving Medication Safety at Hospital Admission
To our knowledge, this is the largest study analyzing admission medication reconciliation risk factors for a hospitalized general medicine population. There are limited data available identifying patient or medication risk factors associated with medication errors.18 The Joint Commission National Patient Safety Goal on medication reconciliation put a spotlight on medication discrepancies and gaps in communication and handoffs.19 Admission medication errors are not surprising given patients’ large number of medicines, complexity of medication regimens, look-alike/sound-alike medication name confusion and increased number of drug formulations. In our study, medication classes such as cardiovascular agents, antidiabetics, antidepressants, and anticonvulsants with various formulations such as regular and extended release, with similar strengths and directions, frequently resulted in error. With the complexity of medication regimens for common co-morbidities such as heart disease, diabetes and depression, medications to treat glaucoma, allergies or dermatological issues were often missed.
Although the number of unexplained prescription medication discrepancies requiring clarification (n = 1,093, Fig. 1) was large in this study population, the actual number of potentially harmful errors (n = 36) or errors potentially requiring increased monitoring or intervention to preclude harm (n = 162) was relatively small. Potential harm was driven by type of medication class and type of error; drug omissions, incorrect medications prescribed or dosing discrepancies in cardiovascular medications, anti-diabetics, anticonvulsants or anticoagulants were found to be most likely to result in patient harm.
Our error findings during medication history taking and performing reconciliation are similar to other studies. In a smaller sample of 180 general medicine inpatients by Pippen and colleagues,18 186 (72%) of unintended, potentially harmful discrepancies were more often medication history-taking errors rather than reconciliation errors. A systematic review by Tam and coworkers4 of medication history errors upon hospitalization revealed up to 54% of patients experienced at least one medication history discrepancy. For this review, an “error” was defined as “discrepancy between physician-acquired medication history and comprehensive medication history.”4 In our study, only unexplained discrepancies clarified with hospital physicians resulting in order changes were considered medication errors. Our restrictive error definition may have accounted for a lower number of errors in patients (e.g., 35.9% of study patients) compared to prior studies.
Medication History Taking: a System Defect?
Our study and others3–5,7,18 found the majority of unexplained inpatient medication errors originated in obtaining patients’ medication histories, a process relying heavily on clinicians’ interview skills, patients’ ability to participate, and access and accuracy of patients’ outpatient medication lists or community pharmacy dispensing records. Pharmacists’ ability to obtain more complete and accurate medication histories has been previously demonstrated.5,18,20 Incorporating teaching on medication history taking and reconciliation in medical school curriculums may increase students’ knowledge and comfort in these areas.21 As physicians, nurses and pharmacists play key roles in medication management including ordering, monitoring and educating patients during hospitalization and at discharge, a multidisciplinary team approach to medication reconciliation becomes even more important, especially with errors often originating in medication histories.
Patient and System Risk Factors
A prior study of patient risk factors for actual adverse drug events (ADEs) in hospitalized patients found no independent predictors of preventable ADEs, leading authors to suggest improving medication systems rather than focusing on individual patient risks.22 This observation is consistent with our study, where the only statistically significant risk factors contributing to medication errors potentially causing harm were advanced age and a large number of medications. Although information technology can facilitate medication reconciliation,23,24 a well-designed process for medication history verification with patients by clinicians must still be in place to determine what patients are actually taking and uncover medication-related issues.
To our knowledge, this is also the first study to demonstrate presenting a medication list is a significant protective factor for avoiding medication errors if lists and prescription bottles are appropriately utilized and validated by clinicians. Although the prescribing inpatient physician and study pharmacist both utilized the same patient’s self-prepared medication list or pharmacy bottles, unexplained discrepancies still occurred. After pharmacist consultation with physicians, these discrepancies were attributed to physicians copying lists or prescription labels verbatim without systematically reviewing each medication. This systematic review is an important step as labels on prescription bottles may not accurately reflect patients’ current regimens and newly prescribed medications or recent changes may not be incorporated into patients’ self-prepared medication lists. These findings provide support for primary care physicians to involve patients/caregivers in the medication reconciliation process and empower patients to maintain, review and update their medication list at each health care encounter. These recommendations are summarized in the MATCH Medication Reconciliation Toolkit available at http://www.nmh.org/nm/for+physicians+match.
Study Limitations
This study has important limitations. It was conducted at a single academic hospital among a medicine service population. Because we were unable to interview patients who were too ill or unwilling to participate and had no caregivers present, we may have underestimated the number of medication errors. Our harm assessment is based on rating ‘potential’ harm determined by expert review of the medical record. The actual harm of errors intercepted by study pharmacists is unknown. If a patient had two blood pressure medications unintentionally omitted or dosed in error, we rated harm on each medication separately rather than taking all discrepant medications into account and assigning one potential harm rating per patient. Since we did not analyze cumulative effects of multiple medication errors for a single patient, and used only the highest harm level to analyze patient-level risk factors, ratings may underestimate preventable harm. Also, a shift to greater harm may occur if unidentified and unresolved medication history or order discrepancies introduced upon hospitalization continue post-discharge,2,25–28 highlighting the importance of thorough discharge planning and reliable, comprehensive continuity of care processes.
Conclusion
Despite these limitations, our findings suggest early identification and correction of admission medication errors may mitigate or prevent harm. Our findings suggest the importance of accurate, complete admission medication histories, especially in older patients with a large number of medications. When feasible, hospital pharmacists can also be invaluable in obtaining complex medication histories and collaborating with physicians, nurses and other health care providers on medication reconciliation. Finally, this study underscores the value of primary care physicians and other clinicians encouraging patients to maintain complete, accurate medication lists that can be used by multiple providers, especially during transitions and handoffs of care.
Acknowledgments
This study was supported, in part, by a grant from the Agency for Healthcare Research and Quality (AHRQ) number 5 U18 HS015886. The opinions expressed in this document are those of the authors and do not reflect the official position of AHRQ or the US Department of Health and Human Services. The funding source had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; or preparation, review, or approval of the manuscript.
Portions of this work were presented at the 9th Annual National Patient Safety Foundation (NPSF) Patient Safety Congress May, 2007, and at the AHRQ 2007 Annual Conference.
Conflict of Interest
None Disclosed
References
- 1.Aspden P, Wolcott J, Bootman JL, Cronenwett LR, editors. Preventing medication errors: quality chasm series. Washington: National Academy Press; 2006. [Google Scholar]
- 2.Vira T, Colquhoun M, Etchells E. Reconcilable differences: correcting medication errors at hospital admission and discharge. Qual. Saf. Health Care. 2006;15:122–126. doi: 10.1136/qshc.2005.015347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cornish PL, Knowles SR, Marchesano R, et al. Unintended medication discrepancies at the time of hospital admission. Arch Intern Med. 2005;165:424–429. doi: 10.1001/archinte.165.4.424. [DOI] [PubMed] [Google Scholar]
- 4.Tam VC, Knowles SR, Cornish PL, Fine N, Marchesano R, Etchells EE. Frequency, type and clinical importance of medication history errors at admission to hospital: a systematic review. CMAJ. 2005;173:510–515. doi: 10.1503/cmaj.045311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gleason KM, Groszek JM, Sullivan C, Rooney D, Barnard C, Noskin GA. Reconciliation of discrepancies in medication histories and admission orders of newly hospitalized patients. Am J Health-Syst Pharm. 2004;61:1689–1695. doi: 10.1093/ajhp/61.16.1689. [DOI] [PubMed] [Google Scholar]
- 6.Kaboli PJ, McClimon BJ, Hoth AB, Barnett MJ. Assessing the accuracy of computerized medication histories. Am J Manag Care. 2004;10(part2):872–877. [PubMed] [Google Scholar]
- 7.Lau HS, Florax C, Porsius AJ, de Boer A. The completeness of medication histories in hospital medical records of patients admitted to general internal medicine wards. Br J Clin Pharmacol. 2000;49:597–603. doi: 10.1046/j.1365-2125.2000.00204.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bedell SE, Jabbour S, Goldberg R, et al. Discrepancies in the use of medications: their extent and predictors in an outpatient practice. Arch Intern Med. 2000;160:2129–2134. doi: 10.1001/archinte.160.14.2129. [DOI] [PubMed] [Google Scholar]
- 9.Beers MH, Munekata M, Storrie M. The accuracy of medication histories in the hospital medical records of elderly persons. J Am Geriatr Soc. 1990;38:1183–1187. doi: 10.1111/j.1532-5415.1990.tb01496.x. [DOI] [PubMed] [Google Scholar]
- 10.Leister KA, Edwards WA, Christensen DB, Clarke H. A comparison of patient drug regimens as viewed by the physician, pharmacist and patient. Med Care. 1981;19:658–664. doi: 10.1097/00005650-198106000-00008. [DOI] [PubMed] [Google Scholar]
- 11.Agency for Healthcare Research and Quality (AHRQ) WebM&M: Morbidity and Mortality Rounds on the Web. Medical Informatics Case and Commentary: “Electronic Err”. October, 2005. http://webmm.ahrq.gov/case.aspx?caseID=79&searchStr=electronic+medication+lists. Accessed December 28, 2009.
- 12.U.S. Pharmacopeia 8th Annual MEDMARX® Report Indicates Look-Alike/Sound-Alike Drugs Lead to Thousands of Medication Errors Nationwide. http://www.usp.org/aboutUSP/media/newsCenter.html?article=105435. Accessed December 28, 2009.
- 13.Berkman ND, DeWalt DA, Pignone MP, et al. Literacy and Health Outcomes. Evidence Report/Technology Assessment No. 87 (Prepared by RTI International-University of North Carolina Evidence-based Practice Center under Contract No. 290-02-0016). AHRQ Publication No. 04-E007-2. Rockville, MD: Agency for Healthcare July 16, 2009.
- 14.Baker DW, Gazmararian JA, Williams MV, et al. Functional health literacy and the risk of hospital admission among Medicare managed care enrollees. Am J Public Health. 2002;92:1278–1283. doi: 10.2105/AJPH.92.8.1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.National Coordinating Council for Medication Error Reporting and Prevention. NCC MERP index for categorizing medication errors. http://www.nccmerp.org/medErrorCatIndex.html. Accessed December 28, 2009. [DOI] [PubMed]
- 16.Forrey RA, Pedersen CA, Schneider PJ. Interrater agreement with a standard scheme for classifying medication errors. Am J Health-Syst Pharm. 2007;64:175–181. doi: 10.2146/ajhp060109. [DOI] [PubMed] [Google Scholar]
- 17.MEDMARX®, U.S. Pharmacopeia. http://www.usp.org/hqi/patientSafety/medmarx/. Accessed December 28, 2009.
- 18.Pippins JR, Gandhi TK, Hamann C, et al. Classifying and predicting errors of inpatient medication reconciliation. J Gen Intern Med. 2008;23:1414–1422. doi: 10.1007/s11606-008-0687-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.The Joint Commission. Medication reconciliation National Patient Safety Goal to be reviewed, refined. http://www.jointcommission.org/PatientSafety/NationalPatientSafetyGoals/npsg8_review.htm. Accessed December 28, 2009.
- 20.Nester TM, Hale LS. Effectiveness of a pharmacist-acquired medication history in promoting patient safety. Am J Health-Syst Pharm. 2002;59:2221–2225. doi: 10.1093/ajhp/59.22.2221. [DOI] [PubMed] [Google Scholar]
- 21.Lindquist LA, Gleason KM, McDaniel MR, Doeksen A, Liss D. Teaching medication reconciliation through simulation: a patient safety initiative for second year medical students. J Gen Intern Med. 2008;23:998–1001. doi: 10.1007/s11606-008-0567-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bates DW, Miller EB, Cullen DJ, et al. Patient risk factors for adverse drug events in hospitalized patients. ADE Prevention Study Group. Arch Intern Med. 1999;159:2553–2560. doi: 10.1001/archinte.159.21.2553. [DOI] [PubMed] [Google Scholar]
- 23.Poon EG, Blumenfeld B, Hamann C, et al. Design and implementation of an application and associated services to support interdisciplinary medication reconciliation efforts at an integrated healthcare delivery network. J Am Med Inform Assoc. 2006;13:581–592. doi: 10.1197/jamia.M2142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Turchin A, Hamann C, Schnipper JL, et al. Evaluation of an inpatient computerized medication reconciliation system. J Am Med Inform Assoc. 2008;15:449–452. doi: 10.1197/jamia.M2561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Forster AJ, Murff HJ, Peterson JF, Gandhi TK, Bates DW. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003;138:161–167. doi: 10.7326/0003-4819-138-3-200302040-00007. [DOI] [PubMed] [Google Scholar]
- 26.Forster AJ, Clark HD, Menard A, et al. Adverse events among medical patients after discharge from hospital. CMAJ. 2004;170(3):345–349. [PMC free article] [PubMed] [Google Scholar]
- 27.Coleman EA, Smith JD, Raha D, Min SJ. Posthospital medication discrepancies: prevalence and contributing factors. Arch Intern Med. 2005;165:1842–1847. doi: 10.1001/archinte.165.16.1842. [DOI] [PubMed] [Google Scholar]
- 28.Society of Hospital Medicine. BOOSTing (Better Outcomes for Older adults through Safe Transitions) Care Transitions resource room. http://www.hospitalmedicine.org/ResourceRoomRedesign/RR_CareTransitions/CT_Home.cfm. Accessed December 28, 2009.