Abstract
Background
Few genetically informative studies have examined the effects of different types of trauma on risk for depression over time. The aim of the present study was to examine the relative contributions over time of assaultive trauma, non-assaultive trauma, and familial effects to risk for depression.
Method
Histories of depression and trauma were obtained during structured diagnostic interviews with 5266 (mean age 29.9 years, S.D. =2.4) members of a volunteer Australian twin panel from the general population. Age at first onset of a DSM-IV major depressive episode was the dependent variable. Associations of depression with traumatic events were examined while accounting for the temporal sequence of trauma and depression and familial effects.
Results
Assaultive traumatic events that occurred during childhood had the strongest association with immediate and long-term risk for depression, and outweighed familial effects on childhood-onset depression for most twins. Although men and women endorsed equal rates of assaultive trauma, women reported a greater accumulation of assaultive events at earlier ages than men, whereas men reported a greater accumulation of non-assaultive events at all ages.
Conclusions
Early exposure to assaultive trauma can influence risk for depression into adulthood. Concordance for early trauma is a significant contributor to the familiality of early-onset depression.
Keywords: Childhood abuse, depression, trauma, twin study
Introduction
Trauma experienced during childhood is associated with increased risk for depression (Kessler & Magee, 1993; Fergusson et al. 1996; Kessler et al. 1997; Felitti et al. 1998; Kendler et al. 2000, 2002, 2006; Jaffee et al. 2002; Nelson et al. 2002; Dube et al. 2003; Maercker et al. 2004) and an early age at onset (Spatz-Widom et al. 2007). The greater aggregation of depression observed in families of early-onset cases has been interpreted as evidence for higher genetic risk associated with early-onset versus adult-onset depression (Todd et al. 1993; Williamson et al. 1995; Kovacs et al. 1997; Wickramaratne et al. 2000) but increased aggregation of childhood trauma in some families may also contribute. Twin designs have been used within diathesis-stress frameworks (Meehl, 1989; Monroe & Simons, 1991) to examine the contributions of trauma and genetic vulnerability to risk for depression. Twin studies that include only stressors that occur within 1 year of the onset of depression (Kendler et al. 1995, 1999; Kendler & Karkowski-Shuman, 1997; Sullivan et al. 2002) permit a closer approximation of causation than would be possible when using temporally distant events, but are inconsistent with evidence that childhood trauma can have long-lasting effects (Fergusson et al. 1996; Kessler et al. 1997; Felitti et al. 1998; Nelson et al. 2002; Dube et al. 2003). Twin studies that examine the association of temporally distant events with risk for lifetime depression (Dinwiddie et al. 2000; Kendler et al. 2000; Nelson et al. 2002) often focus on individual events, such as childhood sexual abuse, and do not examine the influence of a range of traumatic events experienced at different developmental periods. As many individuals who experience one traumatic event experience additional events during their lifetimes (Kessler et al. 1995, 1997; Breslau et al. 1998, 1999), examination of events in isolation may overestimate their influence on risk for depression, which may be correlated with other events in a broader context (Kessler et al. 1997). Differences in risk due to type and timing of events have been examined in relation to post-traumatic stress disorder (PTSD), and can guide similar explorations of trauma and depression. Assaultive events, such as rape, that occur during childhood have been found to increase risk for PTSD in adults after subsequent trauma, but risk from non-assaultive events such as accidents decays over time (Breslau et al. 1999).
The present study used a twin sample to examine how the age at occurrence of nine distinct traumatic events influenced risk for major depressive disorder. The aims of this analysis were to examine: (i) the lifetime prevalence, by gender, of assaultive and non-assaultive trauma in a volunteer twin sample from the general population, (ii) the accumulation of trauma over time, (iii) differences in risk for depression according to age at trauma occurrence, and (iv) the contributions of assaultive trauma, non-assaultive trauma, and familial effects to risk for depression.
Method
Participants
Subjects were members of the young adult cohort of the Australian Twin Register, a volunteer twin panel, born in 1964–1971 (Nelson et al. 2002; Lynskey et al. 2004). Almost all twins were registered by their parents in response to approaches through the school systems or mass media appeals. The data presented here are derived from a structured diagnostic interview (Bucholz et al. 1994) adapted for telephone administration from 1996 to 2000. The institutional review boards of Washington University (St Louis, MO, USA) and the Queensland Institute of Medical Research (Brisbane, Australia) approved the informed consent procedure. Of 4010 pairs that could be traced, interviews were completed with both members of 2765 pairs (69% pairwise response rate) and one member of another 735 pairs (78% individual response rate). Details about sample recruitment, composition and non-response are available in previous studies (Heath et al. 1997, 2001). Individuals with complete data on depression, trauma and age at onset (84% of interviewed subjects, n=5266 individuals) were selected for our sample [672 monozygotic (MZ) female pairs, 476 MZ male pairs, 481 dizygotic (DZ) female pairs, 375 DZ male pairs, 629 DZ opposite-sex pairs]. The sample was 55.7% female and the mean (S.D.) age at the time of interview was 29.9 (2.4) years with a range of 24 to 36 years. Twins excluded from the sample, compared to the analysis sample, were more likely to be from DZ pairs, had a higher prevalence of adult-onset depression and greater endorsement of childhood neglect and physical abuse, rape before age 18, physical assault after age 17, and being threatened with a weapon or kidnapped at any age.
Assessments
A version of the Semi-Structured Assessment for the Genetics of Alcoholism (SSAGA; Bucholz et al. 1994; Hesselbrock et al. 1999), a diagnostic interview, was adapted for telephone use in Australia and administered by trained lay interviewers. The interview incorporates items from validated instruments, including the Diagnostic Interview Schedule (DIS; Robins et al. 1981), the Composite International Diagnostic Interview – Substance Abuse Module (CIDISAM; Cottler et al. 1989), the Structured Clinical Interview for DSM-III-R (SCID; Spitzer et al. 1992; Williams et al. 1992), and the Home Environment Interview (Robins et al. 1985; Holmes & Robins, 1987, 1988), and has good reliability for assessing depression (Bucholz et al. 1994). The interview assessed lifetime history of DSM-IV (APA, 1994) depression and experience of traumatic events. Telephone assessments of depression have been found to have good inter-rater agreement with face-to-face interviews (Rohde et al. 1997; Aziz & Kenford, 2004).
History of traumatic events was based on items from the National Comorbidity Survey (NCS; Kessler et al. 1994, 1995), which queried 12 events and experiences that qualified as traumatic events according to DSM-III-R criteria for PTSD. Details about trauma questions are available elsewhere (Kessler et al. 1995). Respondents who endorsed an event reported their age at first and last occurrence. Participants were asked to report each event only once, so that, for example, serious physical assault by a parent would not also be reported as childhood physical abuse. The sexual molestation variable incorporates data about early sexual experience inside and outside the home, elicited in a separate section of the interview, in addition to the single question about sexual molestation from the NCS items.
To check whether mood at the time of interview influenced reporting of traumatic events, we compared trauma endorsement of individuals with current versus lifetime depression. Endorsement of neglect was greater among the currently depressed [4% v. 1%, odds ratio (OR) 3.2, p=0.04], but there were no other differences. To check for recall bias associated with time since interview, we tested for interactions of trauma with age at assessment in predicting depression, but found none for assaultive trauma, with a single significant interaction only with disaster [hazard ratio (HR) 1.1, p=0.02], which may reflect historical reality (i.e. the timing of a major disaster in Australia that would have impacted some respondents).
Statistical analysis
Cox regression with time-varying covariates was used because it takes into account the temporal ordering of trauma with depression, so that only traumatic events that pre-date depression onset contribute to risk. The association of trauma with depression was modeled to detect variation in risk as a function of timing in two ways: (i) differences in risk based on the developmental age at first trauma occurrence and (ii) variation in risk as a function of time since trauma occurrence.
Age categories were defined to distinguish childhood (ages 0–12), adolescent (ages 13–17) and adult (ages 18 and older) occurrence of first trauma and first depressive episode. Differences in risk by age at trauma occurrence were investigated by subdividing each individual event variable into three dummy variables representing childhood, adolescent and adult age groups, based on age at first experience of the event. In addition to investigating events individually, three trauma categories were formed based on the distinction between childhood/assaultive events and non-assaultive traumatic events (Breslau et al. 1999). These categories were: (i) no trauma (reference group), (ii) non-assaultive trauma only (life-threatening accident; witnessing injury or killing; fire, flood, or natural disaster), and (iii) childhood/assaultive trauma (childhood physical abuse, childhood neglect, rape, sexual molestation, severe physical assault, being threatened with a weapon or kidnapped). Although childhood neglect is not by definition an assaultive event, its strong co-occurrence with childhood physical and sexual abuse (Dong et al. 2004) warrants its inclusion in this category.
To detect differences in risk according to the age at which specific traumatic events occurred, we entered the three age-defined dummy variables into a regression analysis with age at onset of depression as the outcome. Wald χ2 tests, corrected for familial clustering, were used to determine differences in risk by first event occurrence during childhood, adolescence or adulthood. Where statistically significant (p≤0.05) differences between the dummy variables were not observed, they were combined to represent broader age categories.
Variations in risk for depression over time were detected by testing the assumption of proportional hazards using the Stata (Stata Corporation, 2004) statistical program for survival analysis. The Cox model assumes that the hazard for each level of a nominal covariate is proportional over time, so that, for example, individuals who are assaulted may have greater risk for depression than those who are not, but the hazards are roughly parallel over time. One way to check the assumption of proportional hazards uses Schoenfeld residuals (Grambsch & Therneau, 1994) to test the null hypothesis that the ratio of hazards is constant over time (Cleves et al. 2004). When the hazards are not proportional, interactions of time with the variable are created such that hazards are comparable within each time strata. The model makes no assumptions about the shape of the hazard over time, thus allowing that the increase in risk associated with early trauma may be greater for early-onset than for adult-onset depression. In our study, when the proportional hazards assumption was not satisfied for a given variable, we created interaction terms of the variable with age groups representing childhood, adolescent or adult periods. Interaction terms that did not differ significantly based on Wald tests were recombined until the simplest model satisfying the proportional hazards assumption was found.
Genetic effects on risk for depression were modeled as the interaction between twin zygosity (MZ or DZ) and co-twin lifetime status for depression. The age at onset of first depressive episode in the co-twin was used to define three mutually exclusive categories of familial risk for the respondent: childhood, adolescent, and adult. Co-twin status on depression was not coded as time varying but was always coded either ‘0’ or ‘1’, providing a constant level of familial risk as a counterpoint against which to examine the contribution of the respondent’s trauma experience to risk.
The final model including familial effects was determined by first testing a model with the trauma categories and the interaction terms for genetic risk. After the simplest model satisfying the proportional hazards assumption was found, the results were reparameterized using an equivalent model (same number of parameters) to reflect familial risk by zygosity, enabling direct comparison of hazard ratios for MZ and DZ twins. Gender was included as a covariate in all regressions. Interactions of gender with each trauma term and with genetic terms were tested. Interactions with a trend (p≤0.10) were reparameterized and reported separately for men and women.
Descriptive statistics and person-year data were created using SAS version 9 statistical software (SAS Institute, 2004). All regressions were performed using the Stata (Stata Corporation, 2004) statistical program and standard errors were adjusted for the non-independence of observations in twin data. Confidence intervals (CIs) for the final regression model were estimated using bootstrapping to correct for the non-independence of person-year data on twin pairs.
Results
Lifetime prevalence of trauma exposure
Endorsement rates of traumatic events by gender are presented in Table 1, with the percentage of individuals exposed to trauma who had a first onset of depression subsequent to trauma exposure. Fifty-three per cent of the sample overall reported experiencing at least one traumatic event. Women were less likely than men to endorse any event (OR 0.55, 95% CI 0.49–0.62), a difference specific to non-assaultive events (OR 0.41, 95% CI 0.37–0.47). Men and women did not differ in endorsement of childhood and assaultive events overall (OR 0.96, 95% CI 0.84–1.09), although there were gender differences in endorsement of individual events.
Table 1.
Lifetime prevalence of traumatic events and post-trauma depression, by gender
| Men |
Women |
|||
|---|---|---|---|---|
| Trauma endorsement |
Trauma endorsement |
|||
| % of all men (n=2331) | % Depression after trauma | % of all women (n=2935) | % Depression after trauma | |
| Any event | 61.3 | 19.5 | 46.5 | 31.5 |
| One event | 31.6 | 14.6 | 27.6 | 22.5 |
| Two events | 17.0 | 18.4 | 11.6 | 36.3 |
| Three or more | 12.7 | 33.0 | 7.3 | 57.9 |
| Assaultive events | 25.8 | 23.8 | 24.9 | 39.1 |
| Childhood neglect | 0.6 | 38.5 | 0.8 | 64.0 |
| Serious physical assault | 14.1 | 21.6 | 5.5 | 29.4 |
| Other childhood physical abuse | 2.2 | 47.1 | 2.8 | 55.6 |
| Rape | 1.3 | 33.3 | 8.0 | 38.5 |
| Sexual molestation | 5.5 | 33.3 | 14.5 | 44.5 |
| Threatened with weapon or kidnapped | 10.9 | 20.1 | 4.4 | 24.8 |
| Non-assaultive events | 53.8 | 17.0 | 32.8 | 26.6 |
| Life-threatening accident | 26.6 | 17.0 | 12.7 | 25.9 |
| Fire, flood or natural disaster | 16.7 | 15.9 | 11.6 | 30.8 |
| Witness to injury or killing | 32.6 | 14.9 | 16.0 | 24.9 |
Associations of individual events with depression
Twenty-seven per cent of the sample (n=1405) met lifetime criteria for depression (men 21.4%, women 30.8%). Of these, 6.4% were currently depressed, and 4.1% reported their first depressive episode during childhood, 15.0% during adolescence, and the remainder after age 17. Table 2 shows associations of individual traumatic events with depression risk, by age at event occurrence, with hazard ratios reported separately by age period or by gender, in cases where significant interactions were found. Three general trends are apparent regarding the difference between assaultive and non-assaultive events. First, assaultive events, including neglect, are associated with greater risk for depression onset than are non-assaultive events. Second, younger age at occurrence of assaultive events is associated with greater risk than later occurrence. Third, risk from assaultive events (excepting physical assault) varies over time, whereas the risk from non-assaultive events (excepting life-threatening accident) remains constant. The influence of trauma on risk for depression differs by gender for all events except childhood neglect, rape, and disaster. Including event recency as a covariate substantially increases the risk attributable to childhood experience of physical assault or being threatened with a weapon or kidnapped, and slightly decreases the risk from first experience of a disaster and of witnessing an injury or killing (see footnotes to Table 2).
Table 2.
Associations of individual traumatic events with depression, and their variation as a function of age and of age at trauma occurrence
| Associations with depression onset |
|||
|---|---|---|---|
| Traumatic event Age at occurrence | 0–12 years | 13–17 years | 18+ years |
| Assaultive events | |||
| Childhood neglect | |||
| 0–17a | 32.12 (14.87–69.41) | 5.56 (2.41–12.83) | 1.82 (0.86–3.83) |
| Serious physical assaultR | |||
| 0–12, Men | 4.13 (2.27–7.49)R1 | ||
| 0–12, Women | 10.67 (5.22–21.83)R2 | ||
| 13–17 | – | 2.64 (1.97–3.54) | |
| 18+, Men | – | – | 1.47 (1.03–2.09) |
| 18+, Women | – | – | 2.36 (1.60–3.50) |
| Childhood physical abuse | |||
| 0–12, Menb | 10.91 (5.53–21.52) | 7.48 (3.50–15.98) | 2.26 (1.65–3.10) |
| 0–12, Womenb | 10.91 (5.53–21.52) | 3.19 (1.65–6.16) | 2.26 (1.65–3.10) |
| 13–17 | – | 1.19 (0.37–3.79) | |
| Rape | |||
| 0–12c | 5.17 (3.06–8.74) | 1.84 (1.21–2.79) | |
| 13+ | – | 2.71 (2.14–3.42) | |
| Sexual molestation | |||
| 0–12d | 6.98 (3.66–13.30) | 2.39 (1.80–3.17)i | 1.83 (1.46–2.30)j |
| 13–17, Mene | – | 7.97 (3.67–17.33) | 1.77 (1.33–2.35) |
| 13–17, Womene | – | 2.50 (1.24–5.03) | 1.77 (1.33–2.35) |
| 18+ | – | – | 2.58 (1.57–4.23) |
| Threatened with weapon/kidnappedR | |||
| 0–12, Menf | 7.85 (4.02–15.26)R3 | 1.46 (0.60–3.54) | |
| 0–12, Womenf | 7.85 (4.02–15.26)R3 | 5.14 (2.93–9.02)R4 | |
| 13+ | – | 1.40 (1.09–1.81) | |
| Non-assaultive events | |||
| Life-threatening accident | |||
| 0–12, Men | 1.88 (1.34–2.64) | ||
| 0–12, Women | 1.10 (0.77–1.59) | ||
| 13–17, Meng | – | 4.19 (2.39–7.36) | 1.07 (0.68–1.69) |
| 13–17, Womenh | – | 4.19 (2.39–7.36) | 2.13 (1.38–2.39) |
| 18+ | – | – | 1.84 (1.53–2.21) |
| DisasterR | |||
| All ages | 1.25 (1.05–1.50)R5 | ||
| Witness injury/killingR | |||
| All ages, Men | 1.12 (0.91–1.38)R6 | ||
| All ages, Women | 1.48 (1.22–1.80)R7 | ||
Data are given as hazard ratio (HR) with 95% confidence interval (CI) in parentheses.
Arrows indicate continuation of HR into subsequent age period(s), i.e. risk from event occurrence does not decrease over the time indicated by arrows.
Associations prior to modeling age interactions, HR (95% CI):
3.66 (2.15–6.25),
2.97 (2.26–3.91),
2.54 (1.79–3.60),
2.16 (1.82–2.58),
2.02 (1.56–2.61),
3.60 (2.31–5.61),
1.37 (0.91–2.04),
2.32 (1.57–3.43).
Age different from column indicators:
ages 13–20,
ages 21+.
Controlling for event recency (event occurring in later time period) for events where multiple occurrence significant. Associations unadjusted for event recency, HR (95% CI):
R13.09 (1.73–5.49),
R2 5.45 (2.43–12.21),
R3 6.85 (3.53–13.31),
R4 3.75 (1.91–7.36),
R5 1.36 (1.15–1.59),
R6 1.20 (0.98–1.46),
R7 1.55 (1.28–1.87).
Accumulation of trauma over time
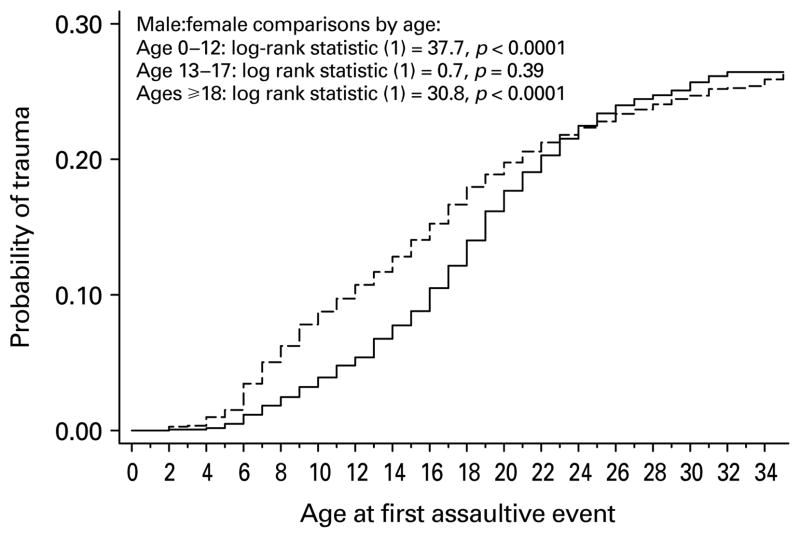
Although lifetime endorsement of assaultive events is equal by gender, women comprise the majority of the assaultive trauma category until age 22 (Fig. 1). Women are more likely than men to report assaultive trauma before age 13, risk is equal by gender from ages 13 to 17, and men are more likely than women to report assaultive trauma from age 18 on. Non-assaultive events have a greater accumulation among men than women through all periods of risk [log rank statistic (1)=238.83, p<0.0001].
Fig. 1.
Cumulative incidence of assaultive trauma by gender (—, male; - - -, female) (n = 5266 subjects, n = 162 691 observations in person-year data).
Associations of assaultive and non-assaultive trauma with depression
The cumulative incidence of first-onset depression is highest in the assaultive trauma category for both men [log rank statistic (2)=71.68, p<0.0001] and women [log rank statistic (2)=198.06, p<0.0001]. In a model including only the trauma categories and gender (not shown), the risk for depression associated with assaultive trauma history attenuated with age, with greatest risk before age 13 (HR 13.16, 95% CI 7.48–23.16), less between ages 13 and 17 (HR 3.70, 95% CI 2.76–4.98), and less again after age 17 (HR 2.28, 95% CI 1.99–2.61). Non-assaultive trauma history carried a more moderate risk for depression (HR 1.53, 95% CI 1.33–1.76) that did not vary with age.
Associations of trauma and familial effects with depression
Controlling for trauma history, risks of respondent depression onset associated with co-twin childhood and adolescent onset could be pooled [χ2(1)=0.5, p=0.48], and were the same across the respondent’s childhood and adolescent periods [χ2(1)=0.3, p=0.57]. Likewise, respondent risk of depression onset associated with co-twin adult-onset depression was the same across childhood and adolescent periods [χ2(1)=2.7, p=0.10]. We hereafter refer to the pooled childhood/adolescent onset category as early-onset. Table 3 summarizes respondent risk of depression onset, by developmental period, as a function of own trauma history and co-twin’s depression history, with the latter categorized by twin pair zygosity and by the age of co-twin depression onset. It thus summarizes the combined effects of genetic risk (contrasting risk associated with MZ versus DZ exposure) and trauma exposure across developmental periods. No significant genotype-by-environment interaction effects were found, nor did we find significant interactions of trauma with gender.
Table 3.
Effects of history and timing of trauma and co-twin depression on risk for respondent first-onset depression, by age
| Associations with depression onset |
|||
|---|---|---|---|
| 0–12 years | 13–17 years | 18+ years | |
| Respondent trauma history | |||
| Assaultivea | 11.40 (6.79–21.39) | 3.28 (2.37–4.30) | 2.14 (1.87–2.46) |
| Non-assaultive | 1.46 (1.27–1.69) | ||
| Co-twin depression history and age at onset | |||
| Monozygous twins | |||
| 0–17, Menb | 12.00 (3.48–25.47) | 2.03 (1.32–2.96) | |
| 0–17, Womenc | 4.37 (1.88–8.53) | 2.03 (1.32–2.96) | |
| 18+, Men and womend | 1.53 (0.98–2.28) | 2.14 (1.63–2.77) | |
| Dizygous twins | |||
| 0–17, Mene | 4.26 (1.73–8.74) | 1.56 (1.11–2.07) | |
| 0–17, Womenf | 0.80 (0.23–2.74) | 1.56 (1.11–2.07) | |
| 18+, Men and womeng | 1.50 (1.03–2.09) | 1.16 (0.89–1.49) | |
Data are given as hazard ratio (HR) with 95% confidence interval (CI) in parentheses.
Adjusted for zygosity and gender. Confidence intervals are bootstrapped, bias-corrected, and stratified by twin zygosity, except for dizygous childhood and adolescent females, where data were too sparse to permit bootstrapped estimates.
Associations prior to modeling interactions with respondent age, HR (95% CI):
2.43 (2.15–2.75),
4.51 (2.18–9.35),
2.62 (1.72–3.99),
2.03 (1.61–2.55),
1.65 (1.02–2.67),
1.67 (1.17–2.38),
1.22 (0.99–1.51).
Five notable findings illustrate the contributions of genetic effects and trauma to risk for depression (Table 3). (i) Assaultive trauma history has a potent effect on risk, especially during childhood. Its association with risk for childhood-onset depression is comparable to the risk associated with having a male [HRs=11.4 v. 12.0, χ2(1)=0.0, p=0.93] or female [11.4 v. 4.4, χ2(1)=3.6, p=0.06] MZ co-twin with early depression onset, and greater than the risk associated with having a male [11.4 v. 4.3, χ2(1)=4.2, p=0.04] or female [11.4 v. 0.8, χ2(1)=13.5, p<0.01] DZ co-twin with early depression onset. The association of assaultive trauma history with adult-onset depression, though reduced, is nonetheless equal to the risk associated with having an MZ co-twin with adult-onset depression [2.1 v. 2.1, χ2(1)=0.0, p=1.0], and greater than that associated with having a DZ co-twin with adult-onset depression [2.1 v. 1.2, χ2(1)=17.7, p<0.01]. (ii) Non-assaultive trauma history is associated with a modest increase in risk for depression that does not vary by age. (iii) Comparison of HRs for MZ and DZ twins reveals significant genetic effects on early depression onset in women. The association of co-twin early-onset depression with respondent risk for early-onset is stronger for MZ than DZ twins among women [4.37 v. 0.80, χ2(1)=5.9, p=0.01], with a similar trend among men [12.00 v. 4.26, χ2(1)=3.5, p=0.06]. (iv) The effect of co-twin adult-onset depression on respondent adult-onset is also stronger among MZ than DZ twins in both genders [HRs=2.14 v. 1.16, χ2(1)=11.9, p<0.01]. Finally, there is a lack of evidence for genetic contributions in pairs concordant for depression but discordant for early- versus adult-onset, raising the possibility that, even after adjustment for trauma history, family environmental mechanisms are important for this subgroup. Specifically, the association of co-twin adult-onset depression with risk for early-onset depression in the respondent does not vary by zygosity [HRs=1.53 v. 1.50, χ2(1)=0.0, p=0.94]. Similarly, the association of co-twin early-onset depression with risk for respondent adult-onset depression does not vary significantly by zygosity [2.03 v. 1.56, χ2(1)=1.0, p=0.32].
Discussion
The present study found that early assaultive trauma increased risk for early-onset depression and had an enduring influence on risk for adult-onset depression, independent of familial effects. All early assaultive events and childhood neglect were associated with heightened risk during childhood and into adulthood, suggesting that focusing on individual events, such as childhood sexual abuse, may obscure a general vulnerability that is associated with exposure to any interpersonal assaultive trauma during early development.
The co-occurrence of depression with PTSD is well documented (Breslau et al. 1991; Kessler et al. 1995; North et al. 1997, 1999; Creamer et al. 2001; O’Donnell et al. 2004), but as PTSD was not assessed in this sample we cannot address the possibility that our findings for depression are limited to individuals with co-occurring PTSD. Nonetheless, differences in risk for depression according to the type and timing of trauma are similar to findings regarding PTSD. Breslau et al. (1998 (1999) found greater risk for PTSD following assaultive events compared to non-assaultive events. Early exposure to assaultive violence increased risk for PTSD following subsequent trauma among individuals who developed PTSD after the initial trauma (Breslau et al. 1999, 2008). Recent findings from prospective studies are similar. Copeland et al. (2007) found that traumatic events reported by age 13 were associated with increased risk for PTSD symptoms and with depressive and anxiety disorders by age 16. Childhood trauma has been found to carry greater risk for depression than adolescent trauma, given endorsement of a PTSD-qualifying event (Maercker et al. 2004). An enduring risk for depression was found among adults with court-documented histories of physical abuse and neglect that occurred before age 11 (Spatz-Widom et al. 2007). These findings of strong effects of early trauma with risk for depression, combined with the possibility that PTSD–depression comorbidity following trauma exposure represents a shared vulnerability rather than distinct liabilities (O’Donnell et al. 2004), suggest that exposure to early trauma increases vulnerability to stress across the lifespan. Although we were unable to examine PTSD, our findings are consistent with these earlier studies and, furthermore, specify the particular influence of individual events.
Our study extends earlier findings regarding trauma by including familial effects, as did another recent study. Zimmerman et al. (2008) included familial effects in their examination of the influence of various adversities on a first onset of depression over a 10-year period. They defined familial liability as a history of at least subthreshold parental depression, and history of traumatic events was determined using items similar to those in our analysis. They found that a history of trauma predicted increased risk for depression among individuals with familial liability but not those without (Zimmermann et al. 2008). We found no evidence in our study that sensitivity to the effects of trauma was greater among individuals with familial liability to depression, as would have been indicated by gene–environment interactions. Our findings are similar, however, in that we found independent effects of trauma and familial liability and evidence for long-term associations of early trauma with risk for a first onset of depression. The similarity of our findings, based on retrospective data, with findings from a prospective study increases our confidence that our data provide valid results.
Our examination of a range of traumatic events suggests that the type and timing of trauma are important considerations in research that examines the interplay of environmental and genetic factors across the lifespan. In the present study, the influence of early assaultive trauma on risk for childhood-onset depression was equal to familial effects for MZ twins and greater than familial effects for DZ twins; substantial influence on risk for adolescent and adult-onset depression was also observed. By contrast, non-assaultive trauma had a moderate association with risk, contributing less than either assaultive trauma or familial effects. The results also challenge the assumption that early-onset depression in a relative is necessarily associated with increased genetic risk for adult-onset depression because we failed to find higher MZ than DZ concordance in pairs concordant for depression but discordant for early versus adult-onset.
In the present study, as in the NCS (Kessler et al. 1995), women endorsed more rape and sexual molestation than men, events associated with strong risk for childhood- and adolescent-onset depression (Swanston et al. 2003). The finding in this study that rates of assaultive trauma history are similar by gender differs from studies of trauma in relation to PTSD, which find that men have greater exposure to assaultive violence than do women (Breslau et al. 1998, 2004). However, those studies did not directly inquire about childhood rape, molestation, or physical abuse, and this difference alone may account for the discrepancy in male-to-female ratios of assaultive trauma between studies.
The marked gender difference in the timing of assaultive trauma, with women reporting assaultive events at earlier ages, warrants investigation of possible gender differences in the effects of early trauma on development, which may influence lifetime risk for depression. One twin study found that women with histories of childhood sexual abuse, compared to those without such histories, were indeed more sensitive to the effects of recent stress, and more likely to experience current depression (Kendler et al. 2004). If, as recent evidence suggests, early deprivation and adversity can influence the development of the stress response system (Heim et al. 2000, 2001; Penza et al. 2003) and the brain (De Bellis et al. 2002; De Bellis & Keshavan, 2003; Teicher et al. 2004; De Bellis & Kuchibhatla, 2006), which in turn may increase risk for depression, then evidence that women experience assaultive trauma at earlier ages than men is an important consideration for research on depression. Although gene–environment interactions have been found to account for some of the variation in risk for depression following adversity (Caspi et al. 2003; Eley et al. 2004; Kaufman et al. 2004; Kendler et al. 2005; Wilhelm et al. 2006), there may be important gender differences in risk as a function of the timing of exposure that should be considered within a developmental framework.
This report has several limitations. It is a cross-sectional study based on retrospective recall of lifetime trauma, depressive episodes, and their ages at occurrence. We cannot rule out the possibility that adult subjects may forget early depression or trauma or misreport their ages at occurrence, or that current depression might influence recall. Caution must be used in interpretation of findings on neglect, given its low endorsement and the broad confidence intervals around the estimate. The same informant was used for both the dependent and independent variables, which may result in recall bias and inflated effects of the trauma variables on risk for depression, for example through misspecification of the temporal relationship between trauma occurrence and first onset of depression. The group excluded from analysis due to missing data had a greater endorsement of early assaultive trauma and depression than the analysis group. However, we found strong associations of early assaultive trauma with increased risk for depression despite their exclusion. In our final analysis, we collapsed all assaultive events and neglect into a single category, which may mask differential effects of different events. Finally, using a person-year design in these data afforded a closer approximation of causality than lifetime status variables; nonetheless, direction of causality is best determined using truly prospective data. Despite these limitations, these findings help to clarify the association between depression and trauma in ways that can inform future investigations into etiology and treatment in trauma-exposed individuals.
The current study found that experiencing assaultive trauma in the first decade of life influences risk for depression into adulthood. This extended period of risk provides a window of opportunity for prevention and intervention in individuals exposed to early trauma. It is possible that a history of early assaultive trauma might signal a type of depression that is etiologically distinct from depression in individuals with no early trauma history, regardless of level of genetic risk. A study of treatment outcome among patients with chronic depression found that patients with a history of early childhood trauma responded better to psychotherapy than to antidepressant treatment, in contrast to patients with no early trauma history, who responded equally well to either treatment (Nemero. et al. 2003). Knowledge about the type and timing of trauma thus may enable clinicians to specify treatment options with greater precision, and may help clinical researchers to specify developmental periods when preventive interventions can be most fruitful.
Acknowledgments
This work was supported by grants AA07728, AA10240, AA11998, 5 T32 MH19960-08, T32 AA07580, AA12640, and F31 MH071039-01. We thank the Australian Twin Registry and the twins for participating in this research.
Footnotes
Portions of this paper were presented as a poster at the 97th Annual American Psychopathological Association Meeting, New York, NY, 1 March 2007, and were based in part upon work completed for the first author’s doctoral dissertation in Social Work at Washington University.
Declaration of Interest
None.
References
- APA. Diagnostic and Statistical Manual of Mental Disorders (DSM-III-R) 3. American Psychiatric Association; Washington, DC: 1994. revised. [Google Scholar]
- Aziz MA, Kenford S. Comparability of telephone and face-to-face interviews in assessing patients with posttraumatic stress disorder. Journal of Psychiatric Practice. 2004;10:307–313. doi: 10.1097/00131746-200409000-00004. [DOI] [PubMed] [Google Scholar]
- Breslau N, Chilcoat HD, Kessler RC, Davis GC. Previous exposure to trauma and PTSD effects of subsequent trauma: results from the Detroit Area Survey of Trauma. American Journal of Psychiatry. 1999;156:902–907. doi: 10.1176/ajp.156.6.902. [DOI] [PubMed] [Google Scholar]
- Breslau N, Davis GC, Andreski P, Peterson E. Traumatic events and posttraumatic stress disorder in an urban population of young adults. Archives of General Psychiatry. 1991;48:216–222. doi: 10.1001/archpsyc.1991.01810270028003. [DOI] [PubMed] [Google Scholar]
- Breslau N, Kessler RC, Chilcoat HD, Schultz LR, Davis GC, Andreski P. Trauma and posttraumatic stress disorder in the community: the 1996 Detroit Area Survey of Trauma. Archives of General Psychiatry. 1998;55:626–632. doi: 10.1001/archpsyc.55.7.626. [DOI] [PubMed] [Google Scholar]
- Breslau N, Peterson EL, Schultz LR. A second look at prior trauma and the posttraumatic stress disorder effects of subsequent trauma: a prospective epidemiological study. Archives of General Psychiatry. 2008;65:431–437. doi: 10.1001/archpsyc.65.4.431. [DOI] [PubMed] [Google Scholar]
- Breslau N, Wilcox HC, Storr CL, Lucia VC, Anthony JC. Trauma exposure and posttraumatic stress disorder: a study of youths in urban America. Journal of Urban Health. 2004;81:530–544. doi: 10.1093/jurban/jth138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bucholz KK, Cadoret R, Cloninger CR, Dinwiddie SH, Hesselbrock VM, Nurnberger JI, Jr, Reich T, Schmidt I, Schuckit MA. A new, semi-structured psychiatric interview for use in genetic linkage studies: a report on the reliability of the SSAGA. Journal of Studies on Alcohol. 1994;55:149–158. doi: 10.15288/jsa.1994.55.149. [DOI] [PubMed] [Google Scholar]
- Caspi A, Sugden K, Moffitt TE, Taylor A, Craig IW, Harrington H, McClay J, Mill J, Martin J, Braithwaite A, Poulton R. Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene. Science. 2003;301:386–389. doi: 10.1126/science.1083968. [DOI] [PubMed] [Google Scholar]
- Cleves MA, Gould WW, Gutierrez RG. An Introduction to Survival Analysis Using Stata. College Station, TX: Stata Press; 2004. revised. [Google Scholar]
- Copeland WE, Keeler G, Angold A, Costello EJ. Traumatic events and posttraumatic stress in childhood. Archives of General Psychiatry. 2007;64:577–584. doi: 10.1001/archpsyc.64.5.577. [DOI] [PubMed] [Google Scholar]
- Cottler LB, Robins LN, Helzer JE. The reliability of the CIDI-SAM: a comprehensive substance abuse interview. British Journal of Addiction. 1989;84:810–814. doi: 10.1111/j.1360-0443.1989.tb03060.x. [DOI] [PubMed] [Google Scholar]
- Creamer M, Burgess P, McFarlane AC. Post-traumatic stress disorder: findings from the Australian National Survey of Mental Health and Well-being. Psychological Medicine. 2001;31:1237–1247. doi: 10.1017/s0033291701004287. [DOI] [PubMed] [Google Scholar]
- De Bellis MD, Keshavan MS. Sex differences in brain maturation in maltreatment-related pediatric posttraumatic stress disorder. Neuroscience and Biobehavioral Reviews. 2003;27:103–117. doi: 10.1016/s0149-7634(03)00013-7. [DOI] [PubMed] [Google Scholar]
- De Bellis MD, Keshavan MS, Shifflett H, Iyengar S, Beers SR, Hall J, Moritz G. Brain structures in pediatric maltreatment-related posttraumatic stress disorder: a sociodemographically matched study. Biological Psychiatry. 2002;52:1066–1078. doi: 10.1016/s0006-3223(02)01459-2. [DOI] [PubMed] [Google Scholar]
- De Bellis MD, Kuchibhatla M. Cerebellar volumes in pediatric maltreatment-related posttraumatic stress disorder. Biological Psychiatry. 2006;60:697–703. doi: 10.1016/j.biopsych.2006.04.035. [DOI] [PubMed] [Google Scholar]
- Dinwiddie S, Heath AC, Dunne MP, Bucholz KK, Madden PA, Slutske WS, Bierut LJ, Statham DB, Martin NG. Early sexual abuse and lifetime psychopathology: a co-twin-control study. Psychological Medicine. 2000;30:41–52. doi: 10.1017/s0033291799001373. [DOI] [PubMed] [Google Scholar]
- Dong M, Anda RF, Felitti VJ, Dube SR, Williamson DF, Thompson TJ, Loo CM, Giles WH. The interrelatedness of multiple forms of childhood abuse, neglect, and household dysfunction. Child Abuse and Neglect. 2004;28:771–784. doi: 10.1016/j.chiabu.2004.01.008. [DOI] [PubMed] [Google Scholar]
- Dube SR, Felitti VJ, Dong M, Giles WH, Anda RF. The impact of adverse childhood experiences on health problems: evidence from four birth cohorts dating back to 1900. Preventive Medicine. 2003;37:268–277. doi: 10.1016/s0091-7435(03)00123-3. [DOI] [PubMed] [Google Scholar]
- Eley TC, Sugden K, Corsico A, Gregory AM, Sham P, McGuffin P, Plomin R, Craig IW. Gene–environment interaction analysis of serotonin system markers with adolescent depression. Molecular Psychiatry. 2004;9:908–915. doi: 10.1038/sj.mp.4001546. [DOI] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Koss MP, Marks JS. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine. 1998;14:245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Horwood LJ, Lynskey MT. Childhood sexual abuse and psychiatric disorder in young adulthood. II. Psychiatric outcomes of childhood sexual abuse. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35:1365–1374. doi: 10.1097/00004583-199610000-00024. [DOI] [PubMed] [Google Scholar]
- Grambsch PM, Therneau TM. Proportional hazards tests in diagnostics based on weighted residuals. Biometrika. 1994;81:515–526. [Google Scholar]
- Heath AC, Bucholz KK, Madden PA, Dinwiddie SH, Slutske WS, Bierut LJ, Statham DJ, Dunne MP, Whitfield JB, Martin NG. Genetic and environmental contributions to alcohol dependence risk in a national twin sample: consistency of findings in women and men. Psychological Medicine. 1997;27:1381–1396. doi: 10.1017/s0033291797005643. [DOI] [PubMed] [Google Scholar]
- Heath AC, Howells W, Kirk KM, Madden PA, Bucholz KK, Nelson EC, Slutske WS, Statham DJ, Martin NG. Predictors of non-response to a questionnaire survey of a volunteer twin panel: findings from the Australian 1989 twin cohort. Twin Research. 2001;4:73–80. doi: 10.1375/1369052012182. [DOI] [PubMed] [Google Scholar]
- Heim C, Newport DJ, Bonsall R, Miller AH, Nemero CB. Altered pituitary–adrenal axis responses to provocative challenge tests in adult survivors of childhood abuse. American Journal of Psychiatry. 2001;158:575–581. doi: 10.1176/appi.ajp.158.4.575. [DOI] [PubMed] [Google Scholar]
- Heim C, Newport DJ, Heit S, Graham YP, Wilcox M, Bonsall R, Miller AH, Nemero CB. Pituitary–adrenal and autonomic responses to stress in women after sexual and physical abuse in childhood. Journal of the American Medical Association. 2000;284:592–597. doi: 10.1001/jama.284.5.592. [DOI] [PubMed] [Google Scholar]
- Hesselbrock M, Easton C, Bucholz KK, Schuckit M, Hesselbrock V. A validity study of the SSAGA – a comparison with the SCAN. Addiction. 1999;94:1361–1370. doi: 10.1046/j.1360-0443.1999.94913618.x. [DOI] [PubMed] [Google Scholar]
- Holmes SJ, Robins LN. The influence of childhood disciplinary experience on the development of alcoholism and depression. Journal of Child Psychology and Psychiatry and Allied Disciplines. 1987;28:399–415. doi: 10.1111/j.1469-7610.1987.tb01762.x. [DOI] [PubMed] [Google Scholar]
- Holmes SJ, Robins LN. The role of parental disciplinary practices in the development of depression and alcoholism. Psychiatry. 1988;51:24–36. doi: 10.1080/00332747.1988.11024377. [DOI] [PubMed] [Google Scholar]
- Jaffee SR, Moffitt TE, Caspi A, Fombonne E, Poulton R, Martin J. Differences in early childhood risk factors for juvenile-onset and adult-onset depression. Archives of General Psychiatry. 2002;59:215–222. doi: 10.1001/archpsyc.59.3.215. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Yang BZ, Douglas-Palumberi H, Houshyar S, Lipschitz D, Krystal JH, Gelernter J. Social supports and serotonin transporter gene moderate depression in maltreated children. Proceedings of the National Academy of Sciences USA. 2004;101:17316–17321. doi: 10.1073/pnas.0404376101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Bulik CM, Silberg J, Hettema JM, Myers J, Prescott CA. Childhood sexual abuse and adult psychiatric and substance use disorders in women: an epidemiological and cotwin control analysis. Archives of General Psychiatry. 2000;57:953–959. doi: 10.1001/archpsyc.57.10.953. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Gardner CO, Prescott CA. Toward a comprehensive developmental model for major depression in women. American Journal of Psychiatry. 2002;159:1133–1145. doi: 10.1176/appi.ajp.159.7.1133. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Gardner CO, Prescott CA. Toward a comprehensive developmental model for major depression in men. American Journal of Psychiatry. 2006;163:115–124. doi: 10.1176/appi.ajp.163.1.115. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Karkowski LM, Prescott CA. Causal relationship between stressful life events and the onset of major depression. American Journal of Psychiatry. 1999;156:837–841. doi: 10.1176/ajp.156.6.837. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Karkowski-Shuman L. Stressful life events and genetic liability to major depression: genetic control of exposure to the environment? Psychological Medicine. 1997;27:539–547. doi: 10.1017/s0033291797004716. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Kessler RC, Walters EE, MacLean C, Neale MC, Heath AC, Eaves LJ. Stressful life events, genetic liability, and onset of an episode of major depression in women. American Journal of Psychiatry. 1995;152:833–842. doi: 10.1176/ajp.152.6.833. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Kuhn JW, Prescott CA. Childhood sexual abuse, stressful life events and risk for major depression in women. Psychological Medicine. 2004;34:1475–1482. doi: 10.1017/s003329170400265x. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Kuhn JW, Vittum J, Prescott CA, Riley B. The interaction of stressful life events and a serotonin transporter polymorphism in the prediction of episodes of major depression: a replication. Archives of General Psychiatry. 2005;62:529–535. doi: 10.1001/archpsyc.62.5.529. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Davis CG, Kendler KS. Childhood adversity and adult psychiatric disorder in the US National Comorbidity Survey. Psychological Medicine. 1997;27:1101–1119. doi: 10.1017/s0033291797005588. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Magee WJ. Childhood adversities and adult depression: basic patterns of association in a US national survey. Psychological Medicine. 1993;23:679–690. doi: 10.1017/s0033291700025460. [DOI] [PubMed] [Google Scholar]
- Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen HU, Kendler KS. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Archives of General Psychiatry. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Kovacs M, Devlin B, Pollock M, Richards C, Mukerji P. A controlled family history study of childhood-onset depressive disorder. Archives of General Psychiatry. 1997;54:613–623. doi: 10.1001/archpsyc.1997.01830190033004. [DOI] [PubMed] [Google Scholar]
- Lynskey MT, Glowinski AL, Todorov AA, Bucholz KK, Madden PA, Nelson EC, Statham DJ, Martin NG, Heath AC. Major depressive disorder, suicidal ideation, and suicide attempt in twins discordant for cannabis dependence and early-onset cannabis use. Archives of General Psychiatry. 2004;61:1026–1032. doi: 10.1001/archpsyc.61.10.1026. [DOI] [PubMed] [Google Scholar]
- Maercker A, Michael T, Fehm L, Becker ES, Margraf J. Age of traumatisation as a predictor of post-traumatic stress disorder or major depression in young women. British Journal of Psychiatry. 2004;184:482–487. doi: 10.1192/bjp.184.6.482. [DOI] [PubMed] [Google Scholar]
- Meehl PE. Schizotaxia revisited. Archives of General Psychiatry. 1989;46:935–944. doi: 10.1001/archpsyc.1989.01810100077015. [DOI] [PubMed] [Google Scholar]
- Monroe SM, Simons AD. Diathesis-stress theories in the context of life stress research: implications for the depressive disorders. Psychological Bulletin. 1991;110:406–425. doi: 10.1037/0033-2909.110.3.406. [DOI] [PubMed] [Google Scholar]
- Nelson EC, Heath AC, Madden PA, Cooper ML, Dinwiddie SH, Bucholz KK, Glowinski A, McLaughlin T, Dunne MP, Statham DJ, Martin NG. Association between self-reported childhood sexual abuse and adverse psychosocial outcomes: results from a twin study. Archives of General Psychiatry. 2002;59:139–145. doi: 10.1001/archpsyc.59.2.139. [DOI] [PubMed] [Google Scholar]
- Nemeroff CB, Heim CM, Thase ME, Klein DN, Rush AJ, Schatzberg AF, Ninan PT, McCullough JP, Jr, Weiss PM, Dunner DL, Rothbaum BO, Kornstein S, Keitner G, Keller MB. Differential responses to psychotherapy versus pharmacotherapy in patients with chronic forms of major depression and childhood trauma. Proceedings of the National Academy of Sciences USA. 2003;100:14293–14296. doi: 10.1073/pnas.2336126100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- North CS, Nixon SJ, Shariat S, Mallonee S, McMillen JC, Spitznagel EL, Smith EM. Psychiatric disorders among survivors of the Oklahoma City bombing. Journal of the American Medical Association. 1999;282:755–762. doi: 10.1001/jama.282.8.755. [DOI] [PubMed] [Google Scholar]
- North CS, Smith EM, Spitznagel EL. One-year follow-up of survivors of a mass shooting. American Journal of Psychiatry. 1997;154:1696–1702. doi: 10.1176/ajp.154.12.1696. [DOI] [PubMed] [Google Scholar]
- O’Donnell ML, Creamer M, Pattison P. Posttraumatic stress disorder and depression following trauma: understanding comorbidity. American Journal of Psychiatry. 2004;161:1390–1396. doi: 10.1176/appi.ajp.161.8.1390. [DOI] [PubMed] [Google Scholar]
- Penza KM, Heim C, Nemero CB. Neurobiological effects of childhood abuse: implications for the pathophysiology of depression and anxiety. Archives of Women’s Mental Health. 2003;6:15–22. doi: 10.1007/s00737-002-0159-x. [DOI] [PubMed] [Google Scholar]
- Robins LN, Helzer JE, Croughan J, Ratcli KS. National Institute of Mental Health Diagnostic Interview Schedule. Its history, characteristics, and validity. Archives of General Psychiatry. 1981;38:381–389. doi: 10.1001/archpsyc.1981.01780290015001. [DOI] [PubMed] [Google Scholar]
- Robins LN, Schoenberg SP, Holmes SJ, Ratcli KS, Benham A, Works J. Early home environment and retrospective recall: a test for concordance between siblings with and without psychiatric disorders. American Journal of Orthopsychiatry. 1985;55:27–41. doi: 10.1111/j.1939-0025.1985.tb03419.x. [DOI] [PubMed] [Google Scholar]
- Rohde P, Lewinsohn PM, Seeley JR. Comparability of telephone and face-to-face interviews in assessing axis I and II disorders. American Journal of Psychiatry. 1997;154:1593–1598. doi: 10.1176/ajp.154.11.1593. [DOI] [PubMed] [Google Scholar]
- SAS Institute. SAS Statistical Software: Release 9.1. SAS Institute, Inc; Cary, NC: 2004. [Google Scholar]
- Spatz-Widom C, DuMont K, Czaja SJ. A prospective investigation of major depressive disorder and comorbidity in abused and neglected children grown up. Archives of General Psychiatry. 2007;64:49–56. doi: 10.1001/archpsyc.64.1.49. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Williams JB, Gibbon M, First MB. The Structured Clinical Interview for DSM-III-R (SCID). I: History, rationale, and description. Archives of General Psychiatry. 1992;49:624–629. doi: 10.1001/archpsyc.1992.01820080032005. [DOI] [PubMed] [Google Scholar]
- Stata Corporation. Stata Statistical Software: Release 8.0. Stata Corporation; College Station, TX: 2004. [Google Scholar]
- Sullivan PF, Prescott CA, Kendler KS. The subtypes of major depression in a twin registry. Journal of Affective Disorders. 2002;68:273–284. doi: 10.1016/s0165-0327(00)00364-5. [DOI] [PubMed] [Google Scholar]
- Swanston HY, Plunkett AM, O’Toole BI, Shrimpton S, Parkinson PN, Oates RK. Nine years after child sexual abuse. Child Abuse and Neglect. 2003;27:967–984. doi: 10.1016/s0145-2134(03)00143-1. [DOI] [PubMed] [Google Scholar]
- Teicher MH, Dumont NL, Ito Y, Vaituzis C, Giedd JN, Andersen SL. Childhood neglect is associated with reduced corpus callosum area. Biological Psychiatry. 2004;56:80–85. doi: 10.1016/j.biopsych.2004.03.016. [DOI] [PubMed] [Google Scholar]
- Todd RD, Neuman R, Geller B, Fox LW, Hickok J. Genetic studies of affective disorders: should we be starting with childhood onset probands? Journal of the American Academy of Child and Adolescent Psychiatry. 1993;32:1164–1171. doi: 10.1097/00004583-199311000-00008. [DOI] [PubMed] [Google Scholar]
- Wickramaratne PJ, Greenwald S, Weissman MM. Psychiatric disorders in the relatives of probands with prepubertal-onset or adolescent-onset major depression. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39:1396–1405. doi: 10.1097/00004583-200011000-00014. [DOI] [PubMed] [Google Scholar]
- Wilhelm K, Mitchell PB, Niven H, Finch A, Wedgwood L, Scimone A, Blair IP, Parker G, Schofield PR. Life events, first depression onset and the serotonin transporter gene. British Journal of Psychiatry. 2006;188:210–215. doi: 10.1192/bjp.bp.105.009522. [DOI] [PubMed] [Google Scholar]
- Williams JB, Gibbon M, First MB, Spitzer RL, Davies M, Borus J, Howes MJ, Kane J, Pope HG, Rounsaville B, Wittchen H. The Structured Clinical Interview for DSM-III-R (SCID). II. Multisite test–retest reliability. Archives of General Psychiatry. 1992;49:630–636. doi: 10.1001/archpsyc.1992.01820080038006. [DOI] [PubMed] [Google Scholar]
- Williamson DE, Ryan ND, Birmaher B, Dahl RE, Kaufman J, Rao U, Puig-Antich J. A case-control family history study of depression in adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 1995;34:1596–1607. doi: 10.1097/00004583-199512000-00010. [DOI] [PubMed] [Google Scholar]
- Zimmermann P, Bruckl T, Lieb R, Nocon A, Ising M, Beesdo K, Wittchen H-U. The interplay of familial depression liability and adverse events in predicting the first onset of depression during a 10-year follow-up. Biological Psychiatry. 2008;63:406–414. doi: 10.1016/j.biopsych.2007.05.020. [DOI] [PubMed] [Google Scholar]