Abstract
Purpose
This study examined the quality of life correlates of family caregiving and caregiving strain in a large national epidemiological sample.
Methods
Structured telephone interviews were conducted with 43,099 participants as part of the REasons for Geographic and Racial Differences in Stroke (REGARDS) study. Participants completed the 12-item short form health survey (SF-12) and brief measures of depressive symptoms, social contacts, and caregiving strain.
Results
Family caregiving responsibilities were reported by 12% of participants. Caregivers reported more quality of life problems than noncaregivers, but these effects were largely dependent on the perceived level of caregiving strain. High strain caregivers reported more problems with emotional distress, worse physical functioning, and fewer social contacts than noncaregivers. Conversely, caregivers who reported no strain from caregiving reported better quality of life than noncaregivers. Caregiving strain effects were not due to demographic differences or to more objective indicators of caregiving demand.
Conclusions
Psychological and social indices of quality of life indicate prevalent problems among family caregivers who experience high strain from their caregiving responsibilities. Public health programs for disabled individuals should include assessments of strain on family caregivers and support services for those who report high levels of caregiving strain.
Keywords: caregiving, caregiving strain, family caregivers, psychological health, depressive symptoms, health-related quality of life
Introduction
Family caregiving is increasingly recognized as an important public health issue. The growth of the older adult population, increased prevalence of many chronic diseases, increased survival rates among persons with disabilities, and high costs of institutional care have pressed millions of individuals into stressful roles of providing care for ailing family members [1]. As these caregiving responsibilities increase, some family members may not be sufficiently prepared or resilient enough to take on such responsibilities without putting their own health and well-being at risk. An extensive body of research suggests that providing care to a chronically ill family member can have negative effects on the caregiver’s psychological health and physical well-being over time [2–3]. In addition to depression and other forms of psychological distress, reductions in social participation and other indicators of poor quality of life have been found in previous caregiving studies [4–7]. Yet, there are limitations to many of these studies and inconsistencies in the findings. Most studies of family caregivers have relied on convenience samples or other types of non-representative samples, and these convenience samples have been shown to yield much larger estimates of caregiver psychological distress than more representative samples [2, 8].
There are many factors that might contribute to these observed associations between family caregiving, psychological well-being, social participation, and health-related quality of life. Physically healthy older adults in a population study were found to be more likely to become caregivers and to continue caregiving over a 3-year period than less healthy older adults [9]. Balancing the deleterious effects from caregiving are findings that caregiving can also lead to positive psychological effects and health benefits for some caregivers [10–12]. Many family members find meaning in providing care to a loved one, feel more useful, gain new skills, and experience other benefits from giving back to those who have helped them in the past.
Greater use of more representative sampling methods could clarify the nature and extent of the correlates of family caregiving and also contribute important new information on other related questions, such as possible racial or ethnic differences in caregiver well-being. Most family caregivers are middle-aged or older adults, but there is little normative information on possible racial differences in health-related quality of life in these age groups [13–14]. Evidence suggests that African American caregivers report fewer symptoms of depression than White caregivers [15–16], and that similar race differences are not found in matched noncaregiving samples [5, 17–18]. African American caregivers have also been found to report less caregiving-related distress [19] and more positive effects from the caregiving experience than White caregivers [10, 20–21].
Objective indicators of caregiving demand (the number of hours of care provided, whether the caregiver lives with the care recipient) and more subjective measures of perceived caregiving strain are both important to consider when examining the quality of life correlates of caregiving. Perceived strain is an appraisal of stress that can vary considerably among caregivers even after controlling for more objective indicators of caregiving demand. Demographic factors can further affect both the observed quality of life indicators and the factors that influence who is expected to take on caregiving roles within individual families [22]. While there is considerable descriptive information on caregivers in the literature, only a few studies have examined the correlates of caregiving using large population-based samples [7, 23].
The REasons for Geographic and Racial Differences in Stroke (REGARDS) study is an ongoing epidemiologic study of stroke incidence and mortality using a large sample of African American and White adults over 45 years of age from across the United States. The baseline telephone interview included key questions about caregiving responsibilities and caregiving strain. Caregivers and noncaregivers, therefore, were identified from the same large epidemiologic sample, and this allowed us to examine the prevalence of family caregiving across demographic groups; compare caregivers and noncaregivers on measures of health-related quality of life, depressive symptoms, and measures of social participation; and examine the impact of caregiving strain on these measures. Our hypotheses, based on previous caregiving studies [2–5, 16–18] were 1) that women would be more likely to report caregiving responsibilities than men, 2) that caregivers would report poorer quality of life in psychological and social domains than noncaregivers, 3) that White caregivers would report more caregiving strain than African American caregivers, and 4) that caregiving strain would be associated with quality of life measures both before and after adjusting for demographic effects and objective caregiving demands.
Methods
Participants
Potential participants for the REGARDS study were randomly selected from a commercially available nationwide list purchased through Genesys, Inc. A stratified random sampling design was used, which called for approximately one-half of the sample to be obtained from the “stroke belt” region (the states of AL, AR, GA, LA, MS, NC, SC, and TN) and the remaining half to reside in other areas throughout the 48 contiguous states. Within both regions, the design called for approximately 1/2 of the sample to be African American and 1/2 White, and within each region-race stratum, approximately 1/2 male and 1/2 female. The stratified random sampling procedure for region was applied at the initial sampling of addresses. Other relevant attributes for stratification (race and sex) were immediately confirmed during the initial telephone interview, and the sample was then partitioned into groups cumulatively to reflect the recruitment goals with respect to the design strata.
Potential participants were first contacted by mail with a brief description of the project, and a subsequent telephone contact was attempted. Respondents were briefly screened for eligibility and then invited to participate. Exclusion criteria included age less than 45, self-identified race other than African American or White, previous diagnosis of cancer requiring chemotherapy, inability to communicate in English, or residence in or on a waiting list for a nursing home. Enrollment began in January of 2003 and ended in October of 2007 after the overall recruitment goals were accomplished. Using standards recommended by Morton and colleagues, the cooperation rate (the proportion of known eligible participants who agreed to be interviewed) has been found to be over 60% [24–25]. All recruitment, interview, and informed consent procedures were reviewed and approved by the Institutional Review Boards of each involved REGARDS organizational unit. The sampling, recruitment, and interviewing procedures for REGARDS have been previously described in more detail elsewhere [25–26].
Procedures and Measures
Trained interviewers contacted potential participants and first established eligibility for participation. Once eligibility was confirmed and verbal informed consent was obtained, a computer-assisted telephone interview was administered that obtained information on demographic variables, medical history, health-related quality of life, depressive symptoms, and caregiving questions. Education was included as a measure of socioeconomic status and was coded into four ordinal categories (less than high school graduate, high school graduate, some college, college graduate or more). The following measures were used in the present analyses:
Health-Related Quality of Life
The SF-12 was used to assess general mental and physical health functioning [27]. The Mental Component Summary (MCS) and Physical Component Summary (PCS) scores were calculated using weighted item composites. These scores are standardized to have population means of 50 and standard deviations of 10, with higher scores reflecting better functioning. The MCS and PCS scores were designed to be uncorrelated with each other and have been shown to be reliable and valid independent indicators of health-related quality of life [27].
Depressive Symptoms
The 4-item short form of the Center for Epidemiological Studies-Depression scale (CESD-4) was used to screen for depressive symptoms [28]. Participants indicated how many days during the past week they felt depressed, lonely, sad, or had crying spells. Response options included less than 1 day, 1–2 days, 3–4 days, or 5 or more days. Total scores ranged from 0 to 12, with a score of 4 or more suggestive of significant psychological distress. The reliability and validity of the CESD-4 have been shown to be sufficient in comparison with the full 20-item CESD [28].
Social Contacts
Social participation was broadly assessed with three interview questions about the number of social contacts. Participants were asked 1) “how many close friends do you have, that is, people who you feel at ease with, can talk to about private matters, and can call on for help?” 2) “how many relatives do you have that you feel close to?” and 3) “how many of these friends or relatives do you see at least once a month?” Responses ranged from 0 to 50 for each question.
Caregiving Variables
Toward the end of the interview, each participant was asked: “Are you currently providing care on an on-going basis to a family member with a chronic illness or disability? This would include any kind of help such as watching your family member, dressing or bathing this person, arranging care, or providing transportation.” Respondents who answered affirmatively to this question were categorized as “caregivers” and subsequently asked 1) whether they lived in the same residence with the care recipient, 2) the nature of their relationship with the care recipient, 3) how many hours per week they spent providing care to this person, and 4) how much of a mental or emotional strain it was on them to provide this care. Response options for the caregiving strain question were “no strain,” “some strain,” or “a lot of strain.” This caregiving strain question and its response options were the same as those used in a previous population-based study of caregiver mortality [23]. The hours of care variable was highly skewed and was recoded into four categories for analysis purposes (< 10, 10–19, 20–29, and ≥ 30 hours per week).
Statistical Analysis
All statistical analyses were conducted using version 9.1 of SAS. Descriptive chi-square tests and univariate analyses of variance were used to compare all caregivers with the noncaregivers on demographic and quality of life variables. When the caregiving strain rating was considered along with caregiving status, four groups of participants were identified – 1) noncaregivers, 2) caregivers who reported no caregiving strain, 3) caregivers who reported moderate strain, and 4) caregivers who reported high strain. One-way analyses of variance and covariance were then conducted to examine differences among these four groups on the PCS, MCS, CESD-4, and the social contact variables. In the covariate-adjusted analyses, the effects of caregiving strain grouping variable were examined after adjusting for the effects of age, gender, race, and education level. These analyses adjusted for the effects of demographic differences among the four groups.
Significant omnibus main effects for the caregiving strain group variable from these analyses of variance and covariance were further examined with pairwise comparisons of each caregiving group with the noncaregivers. This resulted in three separate pairwise comparisons, and a Bonferroni-adjusted type I error rate of .0167 (.05/3) was used for these comparisons. The pattern of differences between the caregiving groups and the noncaregivers was similar and did not change from before to after adjustment for covariates, so only the covariate-adjusted pairwise comparisons are reported here.
Additional analyses of covariance were conducted for the three groups of caregivers that added the hours of care, residence (with or without the care recipient), and the care recipient’s relationship with the caregiver (spouse, parent, sibling, child, other) as additional covariates and predictors of PCS, MCS, CESD-4, and the number of social contacts seen per month. These analyses were conducted to determine whether the effects of the more subjective caregiving strain appraisals were overlapping with or distinct from the effects of the more objective indicators of caregiving demand. Covariate-adjusted means were again examined to identify the direction of any significant omnibus effects.
Results
Caregiving Status
A total of 43,176 participants 45 years of age or older completed the initial telephone interview and provided valid race and gender data. Of these, 43,099 (99.8%) answered the interview questions about caregiving status and, if relevant, caregiving strain. These 43,099 participants constituted the sample for the present analyses and consisted of 12,591 African American women, 7,523 African American men, 11,897 White women, and 11,088 White men. Concerning caregiving status, 5,159 (12.0%) reported providing care on an ongoing basis to a family member with a chronic illness or disability. Descriptive data for the three groups of caregivers (no strain, moderate strain, high strain) and the noncaregivers are summarized in Table 1.
Table 1.
Descriptive Information for Caregiving Groups and Noncaregivers
| Caregivers | Non-caregivers (n = 37,940) | Total (n = 43,099) | |||
|---|---|---|---|---|---|
| Variable | No Strain (n = 1718) | Moderate Strain (n = 2525) | High Strain (n = 916) | ||
| Age | |||||
| M | 64.28 | 63.20 | 62.82 | 65.72 | 65.45 |
| SD | 9.24 | 9.18 | 9.04 | 9.79 | 9.75 |
| Race | |||||
| # African Amer. | 929 | 1155 | 415 | 17,615 | 20,114 |
| % African Amer. | 54.07 | 45.74 | 45.31 | 46.43 | 46.67 |
| Gender | |||||
| # Female | 911 | 1681 | 715 | 21,181 | 24,488 |
| % Female | 53.03 | 66.57 | 78.06 | 55.83 | 56.82 |
| SF-12 PCS | |||||
| M | 46.95 | 46.41 | 44.04 | 46.11 | 46.12 |
| SD | 10.03 | 10.39 | 12.33 | 10.56 | 10.58 |
| SF-12 MCS | |||||
| M | 52.97 | 50.69 | 44.77 | 51.86 | 51.68 |
| SD | 6.74 | 7.70 | 10.65 | 7.79 | 7.89 |
| CESD-4 | |||||
| M | 1.00 | 1.32 | 2.96 | 1.23 | 1.26 |
| SD | 2.01 | 2.13 | 3.13 | 2.14 | 2.17 |
| # of friends | |||||
| M | 5.85 | 5.56 | 4.79 | 5.91 | 5.86 |
| SD | 7.06 | 6.62 | 5.67 | 7.22 | 7.15 |
| # of relatives | |||||
| M | 7.94 | 6.74 | 5.36 | 7.04 | 7.02 |
| SD | 8.97 | 7.28 | 5.85 | 7.82 | 7.81 |
| # of social contacts seen per month | |||||
| M | 8.57 | 7.31 | 6.05 | 7.32 | 7.34 |
| SD | 9.05 | 7.33 | 6.59 | 7.94 | 7.93 |
Chi-square tests indicated that women were more likely to be caregivers than men (13.50% vs. 9.95%, p < .0001) and that African Americans were more likely to be caregivers than Whites (12.42% vs. 11.57%, p = .006). Caregivers were also found to be younger, on average, than noncaregivers (Ms = 63.49 vs. 65.72, p < .0001). Other comparisons between all caregivers and the noncaregivers revealed that the caregivers had lower SF-12 MCS scores (Ms = 50.42 vs. 51.86, p < .0001) and higher CESD-4 scores (Ms = 1.51 vs. 1.23, p < .0001). More caregivers (15.15%) than noncaregivers (12.05%) were found to have CESD-4 scores of 4 or greater (p < .0001). No significant difference between all caregivers and the noncaregivers was found on the SF-12 PCS score. For the social contact variables, caregivers had fewer friends than noncaregivers (Ms = 5.52 vs. 5.92, p < .0001), but no significant differences were found on the number of close relatives or the number of friends or relatives that are seen at least once per month.
Caregiving Strain
Statistically significant omnibus main effects were found for the caregiving strain grouping variable on the PCS, MCS, CESD-4 and each social contact variable both before and after adjusting for the demographic covariates (all ps < .0001). The results of the pairwise comparisons of each caregiving strain group with the noncaregivers on the covariate-adjusted means are summarized in Table 2. The covariate-adjusted mean differences are reported in the metric used by each dependent variable, and each of these mean differences was then divided by the total sample standard deviation for that measure to yield a standardized effect in standard deviation units. Significance tests after the Bonferroni adjustment are noted for the raw differences, whereas the standardized effects allow comparisons across the different measures and facilitate interpretations of the size of these effects.
Table 2.
Comparisons of Caregiving Strain Groups to Noncaregivers after Adjusting for Demographic Covariate Effects
| Variable | No Strain Caregivers | Moderate Strain Caregivers | High Strain Caregivers |
|---|---|---|---|
| PCS | |||
| Adjusted Mean Difference | 0.82* | 0.03 | −1.90** |
| Standardized Effect | 0.08 | 0.00 | −0.18 |
| MCS | |||
| Adjusted Mean Difference | 1.29** | −0.90** | −6.55** |
| Standardized Effect | 0.16 | −0.11 | −0.83 |
| CESD-4 | |||
| Adjusted Mean Difference | −0.27** | 0.06 | 1.61** |
| Standardized Effect | −0.12 | 0.03 | 0.74 |
| # of Friends | |||
| Adjusted Mean Difference | 0.08 | −0.16 | −0.73* |
| Standardized Effect | 0.01 | −0.02 | −0.10 |
| # of Relatives | |||
| Adjusted Mean Difference | 0.89** | −0.08 | −1.35** |
| Standardized Effect | 0.11 | −0.01 | −0.17 |
| # of social contacts seen per month. | |||
| Adjusted Mean Difference | 1.31** | 0.11 | −1.12** |
| Standardized Effect | 0.17 | 0.01 | −0.14 |
Note: All effects after adjusting for race, gender, age, and education. PCS = Physical Component Summary score of the SF-12. MCS = Mental Component Summary score of the SF-12. CESD-4 = 4-item Center for Epidemiological Studies-Depression scale
significantly different from 0, p < .0167
significantly different from 0, p < .0001
Most of the statistically significant differences between subgroups of caregivers and the noncaregivers in Table 2 are small and less than 1/5th of a standard deviation in magnitude, with two notable exceptions. The caregivers who reported high caregiving strain were found to report significantly worse functioning than the noncaregivers on all six dependent variables, and relatively strong effects, with absolute standardized effect sizes exceeding 0.70 standard deviation units, were found on the MCS and CESD-4 measures of quality of life and psychological well-being. Interestingly, the caregivers who reported no caregiving strain were found to have significantly better functioning than the noncaregivers on five of the six dependent measures, but the standardized effect sizes for these differences were all quite small. The differences between the moderate strain caregivers and the noncaregivers were very small and, with the exception of the MCS, not statistically significant. For the CESD-4, scores of 4 or more suggestive of significant emotional distress were observed for 33.92% of the high strain caregivers compared to 12.54% of the moderate strain caregivers and 8.93% of the no strain caregivers.
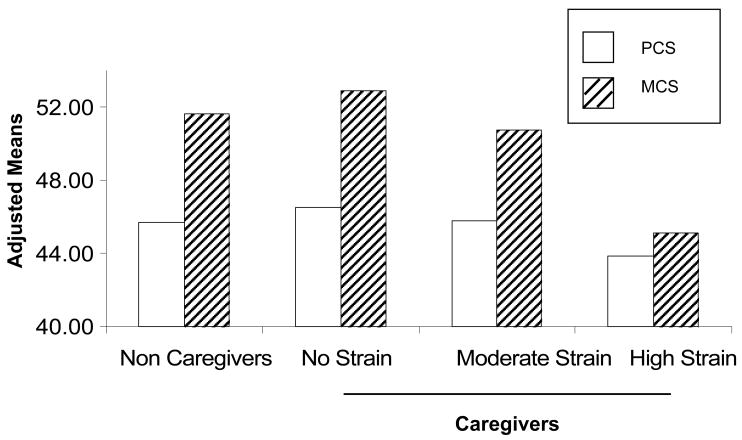
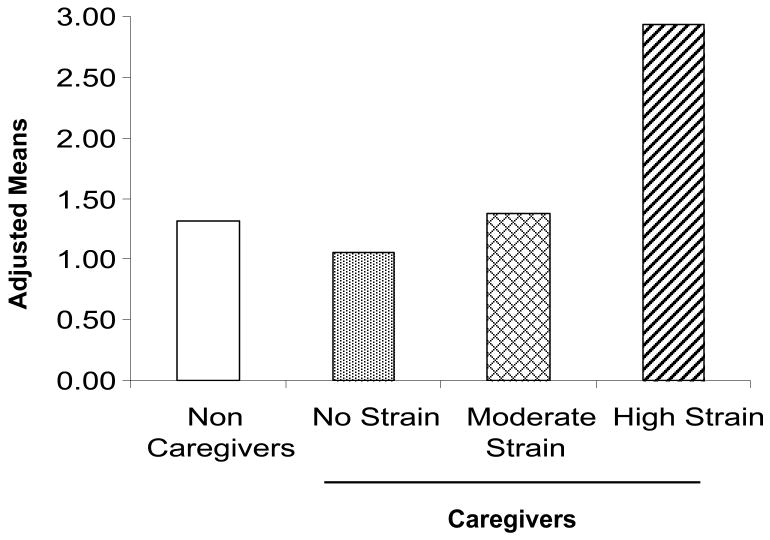
The covariate-adjusted means for all four groups on the SF-12 component summary scores are displayed in Figure 1. PCS scores were lower than MCS scores in all four groups due to the high average age of the REGARDS participants. As the amount of caregiving strain increased among the caregivers, the corresponding decrease in the MCS was striking and much more severe than the milder decrease observed for the PCS. The covariate-adjusted means for the CESD-4 are displayed in Figure 2 and show a similar pattern, with a large increase in depressive symptoms associated with high caregiving strain.
Figure 1.
Covariate-Adjusted Means for the Noncaregivers and the Caregiving Strain Groups on the Physical Component Summary (PCS) and Mental Component Summary (MCS) of the SF-12.
Figure 2.
Covariate-Adjusted Means for the Noncaregivers and the Caregiving Strain Groups on the 4-item Center for Epidemiological Studies-Depression Measure
Differences Among Caregivers
The additional analyses conducted solely for the three groups of caregivers that added the hours of care, residence (with or without the care recipient), and caregiver-care recipient relationship as additional predictors of quality of life indicated that caregiving strain still had statistically significant unique effects on each measure (all ps < .0001). Caregiving strain was clearly the strongest predictor of quality of life among the four caregiving variables examined. Hours of care was not a significant unique predictor of the PCS or the MCS, but it was a significant unique predictor of CESD-4 (F(3,4468) = 3.99, p = .008) and the number of social contacts (F(3,4426) = 4.07, p = .007). Covariate-adjusted means indicated that those providing 20 or more hours of care per week reported higher levels of depressive symptoms than those providing less than 20 hours of care per week (Ms = 2.07 and 1.79, respectively), whereas those reporting less than 10 hours of care per week reported fewer social contacts than those providing 10 or more hours of care (Ms = 6.83 and 7.76, respectively).
Co-residence was related to the MCS (F(1,4337) = 8.26, p = .004) and the number of social contacts (F(1,4426) = 22.77, p < .0001). Caregivers who resided with their care recipients reporting slightly poorer mental health (Ms = 48.83 and 49.72, respectively) and fewer social contacts (Ms = 6.82 and 8.29, respectively) than caregivers who resided elsewhere. The care recipient-caregiver relationship uniquely predicted PCS (F(4,4437) = 2.59, p = .04) and the number of social contacts (F(4,4426) = 4.73, p = .001). Adult children caregivers reported better physical functioning than other subgroups (Ms = 46.03 and 44.95, respectively) and sibling caregivers reporting fewer social contacts than the other subgroups (Ms = 6.70 and 7.78, respectively).
Potential racial differences were also examined on the caregiving variables and these findings are summarized in Table 3. Chi-square tests indicated that African American caregivers were more likely to be living with their care recipients, less likely to be providing care for a spouse, and more likely to be providing care for a sibling than White caregivers (ps < .0001). Both African Americans and Whites reported similar parental care provision rates, but the African American caregivers who were providing care to a parent were almost twice as likely to be living with that parent than their White counterparts (45.23% vs. 22.94%, p < .0001). Consistent with our hypothesis, White caregivers were more likely than African American caregivers to report some mental or emotional strain as a result of caregiving (70.34% vs. 62.83%, p < .0001). On the other hand, African Americans provided more hours of care per week (Ms = 43.60 and 31.57 hours, respectively, p < .0001).
Table 3.
Race Differences in Caregiving Variables
| African American (N = 2,499) | White (N = 2,660) | p* | |
|---|---|---|---|
| Residence with CR? (% Yes) | 58.53 | 49.27 | <.0001 |
| Relationship of CR to CG | <.0001 | ||
| % Parent | 32.85 | 33.36 | |
| % Spouse | 19.82 | 26.91 | |
| % Child | 14.32 | 11.84 | |
| % Sibling | 12.92 | 6.29 | |
| % Other | 20.10 | 21.60 | |
| Hours of Care per week | <.0001 | ||
| % < 10 | 31.22 | 42.77 | |
| % 10–19 | 15.19 | 18.60 | |
| % 20–29 | 13.85 | 12.64 | |
| % ≥ 30 | 39.74 | 25.99 | |
| Caregiving Strain | <.0001 | ||
| % None | 37.17 | 29.66 | |
| % Moderate | 46.22 | 51.50 | |
| % High | 16.61 | 18.83 |
Note: CR = Care recipient, CG = Caregiver
p-values from chi-square tests of independence
After adjusting for age, gender, education level, co-residence, caregiver relationship, and hours of care, African American caregivers were found to report slightly but significantly poorer physical functioning on the PCS than White caregivers (F(1,4339) = 5.78, p = .02, adjusted Ms = 45.19 and 45.98, respectively). No significant race differences were found on the MCS or CESD-4 after adjusting for these demographic and caregiving demand covariates.
Discussion
In this large national sample of over 43,000 adults age 45 or over, ongoing family caregiving responsibilities were found to be common, with 12% of the participants reporting that they were currently providing care on an ongoing basis to a family member with a chronic illness or disability. Caregivers were found to report more problems with psychological health than noncaregivers, but the effect sizes were substantially smaller than those reported by Pinquart and Sörensen for either convenience samples or representative samples from their meta-analysis [2]. Furthermore, previous reports of the deleterious effects of caregiving on physical health were not confirmed in the present sample with the PCS when comparing all caregivers to noncaregivers.
Analyses that took into account the subjective strain of caregiving confirmed that the subgroup of caregivers who reported high caregiving strain had poorer quality of life than less-strained caregivers and noncaregivers. These effects were observed on measures of physical health, psychological problems, and the number of social contacts per month. Standardized effect sizes indicated large effects for measures of depressive symptoms and the SF-12 mental health composite score, whereas the physical health and social contact effects were substantially smaller. Interestingly, caregivers who reported minimal or no caregiving—strain about one-third of the caregivers in our national sample—were the most functional group of all and reported fewer physical health problems, better mental health, and more social contacts, on average, than the noncaregivers.
The present findings suggest that the deleterious effects of family caregiving on health-related quality of life may be mostly limited to the psychological or mental health problems experienced by those caregivers who also report high caregiving strain. The standardized effect sizes for caregiving strain were strong on measures of mental health and largely unchanged after adjusting for demographic variables and indicators of objective care demands. The present results are consistent with previous findings that appraisals of stressfulness can be more important predictors of health and well-being among caregivers than more objective indicators of care demand such as the number of hours spent providing care [29] and that the adverse mental health correlates of caregiving are stronger than the corresponding physical health effects [7]. Other recent findings have shown that older adults who provide more hours of care to a spouse with a disability are healthier than spouse-caregivers who provide fewer hours of care [12], suggesting that even a seemingly straightforward indicator of caregiving demand such as number of hours of care provided can actually represent a more complex combination of caregiver and care recipient health and functional limitations.
Multiple mechanisms may be responsible for the observed findings of better psychological health and physical functioning among the caregivers who reported no caregiving strain in the present analyses. Selection factors may be partly responsible for these effects, an interpretation that is consistent with findings that healthier older adults are more likely to take on caregiving roles and to continue caregiving over longer periods of time than less healthy older adults [9]. In addition, once a person takes on a caregiving role, psychological benefits and other positive effects may be experienced as a result of providing care to a family member [10–11, 21].
Race-specific differences in caregiving were found that show some similarities, but also differences, with findings from previous studies. As hypothesized, African American caregivers were less likely to report strain from caregiving than White caregivers, even though the African American caregivers reported greater caregiving involvement including more hours of care per week and higher co-residence rates with their care recipients. The caregiving strain finding is consistent with previous reports of racial differences in the stress experienced by dementia caregivers in reaction to care recipient functional limitations and behavior problems [19–20, 30]. However, in contrast with previous studies [5, 16–17], African American caregivers in the REGARDS sample were not less depressed than their White counterparts. Thus, data from this large epidemiologic sample suggest that race is associated in complex ways with the amount of caregiving involvement, the subjective experiences of caregiving strain, and the associated experiences of significant emotional distress.
The construct of caregiving strain has been defined in multiple ways by previous investigators and measured using more comprehensive instruments [31–32]. The purpose of the REGARDS study necessitated that the caregiving experience be captured with a few brief questions, including single items about caregiving status and caregiving strain. Caregiving status was restricted to a question about providing care for a family member even though many individuals serve as informal caregivers for individuals who are not family members [33]. The population inferences that can be drawn are further limited by the cross-sectional nature of the research design and by the purposeful oversampling of African Americans and residents of southern states. This oversampling may call into question whether the REGARDS sample can truly provide a representative, population-based analysis of caregiving and its correlates. Additional research using large, multi-ethnic, representative samples and longitudinal designs would be useful for clarifying whether race differences persist over time and whether they are due to specific regional or cultural factors such as different family role expectations [21, 34–36].
This study is one of few to examine caregiving strain in the context of a large epidemiologic study, and our findings reinforce recommendations that interventions for family caregivers should aim to reduce not only objective caregiving stressors but also subjective perceptions of emotional or mental strain. Multicomponent interventions that teach caregivers coping skills have been found to be more potent for reducing caregiver distress than respite care interventions that are primarily aimed at reducing caregiving demands [37], and respite care interventions that also address caregivers’ perceptions of role overload can be effective for reducing caregiver depression [38]. The reductions in depression following a counseling intervention for spouse caregivers of persons with dementia have been shown to be linked to reductions in the caregivers’ stress responses to care recipient behavior problems and to improvements in the caregivers’ satisfaction with their social support networks [39]. With increasing numbers of people taking on potentially stressful caregiving roles, it is important to identify highly strained caregivers as early as possible and to determine whether evidence-based interventions are needed to protect and enhance caregiver quality of life.
Acknowledgments
This research project is supported by a cooperative agreement U01 NS041588 from the National Institute of Neurological Disorders and Stroke (NINDS), National Institutes of Health, Department of Health and Human Services. Additional funding was provided by an investigator-initiated grant R01 NS045789 from NINDS. The content is solely the responsibility of the authors and does not necessarily represent the official views of NINDS or the National Institutes of Health. Representatives of the funding agency have been involved in the review of the manuscript but not directly involved in the collection, management, analysis or interpretation of the data. The authors acknowledge the participating investigators and institutions of REGARDS for their valuable contributions: The University of Alabama at Birmingham, Birmingham, Alabama (Study PI, Statistical and Data Coordinating Center, Survey Research Unit): George Howard DrPH, Leslie McClure PhD, Virginia Howard PhD, Libby Wagner MA, Virginia Wadley PhD, Rodney Go PhD, Monika Safford MD, Ella Temple PhD, Margaret Stewart MSPH, J. David Rhodes BSN; University of Vermont (Central Laboratory): Mary Cushman MD; Wake Forest University (ECG Reading Center): Ron Prineas MD, PhD; Alabama Neurological Institute (Stroke Validation Center, Medical Monitoring): Camilo Gomez MD, Susana Bowling MD; University of Arkansas for Medical Sciences (Survey Methodology): LeaVonne Pulley PhD; University of Cincinnati (Clinical Neuroepidemiology): Brett Kissela MD, Dawn Kleindorfer MD; Examination Management Services, Incorporated (In-Person Visits): Andra Graham; Medical University of South Carolina (Migration Analysis Center): Daniel Lackland DrPH; Indiana University School of Medicine (Neuropsychology Center): Frederick Unverzagt PhD; National Institute of Neurological Disorders and Stroke, National Institutes of Health (funding agency): Claudia Moy PhD.
Contributor Information
David L. Roth, Email: droth@uab.edu.
Virginia G. Wadley, Email: vwadley@uab.edu.
William E. Haley, Email: whaley@cas.usf.edu.
References
- 1.Talley RC, Crews JE. Framing the public health of caregiving. American Journal of Public Health. 2007;97:224–228. doi: 10.2105/AJPH.2004.059337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pinquart M, Sörensen S. Differences between caregivers and noncaregivers in psychological health and physical health: A meta-analysis. Psychology and Aging. 2003;18:250–267. doi: 10.1037/0882-7974.18.2.250. [DOI] [PubMed] [Google Scholar]
- 3.Schulz R, O’Brien A, Bookervale J, Fleissner K. Psychiatric and physical morbidity effects of dementia caregiving: Prevalence, correlates and causes. The Gerontologist. 1995;35:771–776. doi: 10.1093/geront/35.6.771. [DOI] [PubMed] [Google Scholar]
- 4.Brummett BH, Babyak MA, Siegler IC, Vitaliano PP, Ballard EL, Gwyther LP, Williams RB. Associations among perceptions of social support, negative affect, and quality of sleep in caregivers and noncaregivers. Health Psychology. 2006;25:220–225. doi: 10.1037/0278-6133.25.2.220. [DOI] [PubMed] [Google Scholar]
- 5.Haley WE, West CA, Wadley VG, Ford GR, White FA, Barrett JJ, Harrell LE, Roth DL. Psychological, social, and health impact of caregiving: A comparison of Black and White dementia family caregivers and noncaregivers. Psychology and Aging. 1995;10:540–552. [PubMed] [Google Scholar]
- 6.Mausbach BT, Patterson TL, Grant I. Is depression in Alzheimer’s caregivers really due to activity restriction? A preliminary mediational test of the activity restriction model. Journal of Behavior Therapy and Experimental Psychiatry. 2008;39:459–466. doi: 10.1016/j.jbtep.2007.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Neugaard B, Andresen E, McKune SL, Jamoom EW. Health-related quality of life in a national sample of caregivers: Findings from the behavioral risk factor surveillance system. Journal of Happiness Studies. 2008;9:559–575. [Google Scholar]
- 8.Pruchno RA, Brill JE, Shands Y, Gordon JR, Genderson MW, Rose M, Cartwright F. Convenience samples and caregiving research: How generalizable are the findings? The Gerontologist. 2008;48:820–827. doi: 10.1093/geront/48.6.820. [DOI] [PubMed] [Google Scholar]
- 9.McCann JJ, Hebert LE, Bienias JL, Morris MC, Evans DA. Predictors of beginning and ending caregiving during a 3-year period in a biracial community population of older adults. American Journal of Public Health. 2004;94:1800–1806. doi: 10.2105/ajph.94.10.1800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Foley KL, Tung HJ, Mutran EJ. Self-gain and self-loss among African-American and White caregivers. Journals of Gerontology series B: Psychological Sciences and Social Sciences. 2002;57:S14–S22. doi: 10.1093/geronb/57.1.s14. [DOI] [PubMed] [Google Scholar]
- 11.Miller B, Lawton M. Symposium: positive aspects of caregiving. The Gerontologist. 1997;37:216–217. [Google Scholar]
- 12.Brown SL, Smith DM, Schulz R, Kabeto MU, Ubel PA, Poulin M, Yee J, Kim C, Langa KM. Caregiving behavior is associated with decreased mortality risk. Psychological Science. doi: 10.1111/j.1467-9280.2009.02323.x. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kovac SH, Mikuls TR, Mudano A, Saag KG. Health-related quality of life among self-reported arthritis sufferers: Effects of race/ethnicity and residence. Qualtiy of Life Research. 2006;15:451–460. doi: 10.1007/s11136-005-3213-0. [DOI] [PubMed] [Google Scholar]
- 14.Skarupski KA, Mendes de Leon CF, Bienias JL, Sherr PA, Zack MM, Moriarty DG, Evans DA. Black-white differences in health-related quality of life among older adults. Quality of Life Research. 2007;16:287–296. doi: 10.1007/s11136-006-9115-y. [DOI] [PubMed] [Google Scholar]
- 15.Dilworth-Anderson P, Williams IC, Gibson BE. Issues of race, ethnicity, and culture in caregiving research: A 20-year review (1980–2000) The Gerontologist. 2002;42:237–272. doi: 10.1093/geront/42.2.237. [DOI] [PubMed] [Google Scholar]
- 16.Roth DL, Ackerman ML, Okonkwo OC, Burgio LD. The four factor model of depressive symptoms in dementia caregivers: A structural equation model of ethnic differences. Psychology and Aging. 2008;23:567–576. doi: 10.1037/a0013287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Roth DL, Haley WE, Owen JE, Clay OJ, Goode KT. Latent growth models of the longitudinal effects of dementia caregiving: A comparison of African American and White caregivers. Psychology and Aging. 2001;16:427–436. [PubMed] [Google Scholar]
- 18.Pinquart M, Sörensen S. Ethnic differences in stressors, resources, and psychological outcomes of family caregiving: A meta-analysis. The Gerontologist. 2005;45:90–106. doi: 10.1093/geront/45.1.90. [DOI] [PubMed] [Google Scholar]
- 19.Roth DL, Burgio LD, Gitlin LN, Gallagher-Thompson D, Coon DW, Belle SH, Stevens AB, Burns R. Psychometric analysis of the Revised Memory and Behavior Problems Checklist: Factor structure of occurrence and reaction ratings. Psychology and Aging. 2003;18:906–915. doi: 10.1037/0882-7974.18.4.906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Haley WE, Gitlin LN, Wiszniewski S, Mahoney DF, Coon DW, Winter L, Corcoran M, Schinfeld S, Ory M. Well-being, appraisal, and coping in African-American and Caucasian dementia caregivers: Findings from the REACH study. Aging and Mental Health. 2004;8:316–329. doi: 10.1080/13607860410001728998. [DOI] [PubMed] [Google Scholar]
- 21.Roff LL, Burgio LD, Gitlin L, Nichols L, Chaplin W, Hardin JM. Positive aspects of Alzheimer’s caregiving: The role of race. Journals of Gerontology series B: Psychological Sciences and Social Sciences. 2004;59:P185–P190. doi: 10.1093/geronb/59.4.p185. [DOI] [PubMed] [Google Scholar]
- 22.Roth DL, Haley WE, Wadley VG, Clay OJ, Howard G. Race and gender differences in perceived caregiver availability for community-dwelling middle-aged and older adults. The Gerontologist. 2007;47:721–729. doi: 10.1093/geront/47.6.721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schulz R, Beach S. Caregiving as a risk factor for mortality: The caregiver health effects study. The Journal of the American Medical Association. 1999;282:2215–2219. doi: 10.1001/jama.282.23.2215. [DOI] [PubMed] [Google Scholar]
- 24.Morton LM, Cahill J, Hartge P. Reporting participation in epidemiologic studies: A survey of practice. American Journal of Epidemiology. 2006;163:197–203. doi: 10.1093/aje/kwj036. [DOI] [PubMed] [Google Scholar]
- 25.Howard G, Safford MM, Meschia JF, Moy C, Howard VJ, Pulley L, Gomez C, Crowther M. Stroke symptoms in individuals reporting no stroke or transient ischemic attack are associated with a decrease in indices of mental and physical functioning. Stroke. 2007;38:2446–2452. doi: 10.1161/STROKEAHA.106.478032. [DOI] [PubMed] [Google Scholar]
- 26.Howard VJ, Cushman M, Pulley L, Gomez CR, Go RC, Prineas RJ, Graham A, Moy CS, Howard G. The REasons for Geographic and Racial Differences in Stroke study: Objectives and design. Neuroepidemiology. 2005;25:135–143. doi: 10.1159/000086678. [DOI] [PubMed] [Google Scholar]
- 27.Ware JE, Kosinski M, Keller SD. A 12-item short-form health survey: Construction of scales and preliminary tests of reliability and validity. Medical Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 28.Melchior LA, Huba GJ, Brown VB, Reback CJ. A short depression index for women. Educational and Psychological Measurement. 1993;53:1117–1125. [Google Scholar]
- 29.Haley WE, LaMonde LA, Han B, Burton AM, Schonwetter R. Predictors of depression and life satisfaction among spousal caregivers in hospice: Application of a stress process model. Journal of Palliative Medicine. 2003;6:215–224. doi: 10.1089/109662103764978461. [DOI] [PubMed] [Google Scholar]
- 30.Gitlin LN, Roth DL, Burgio LD, Loewenstein DA, Winter L, Nichols L, Argüelles S, Corcoran M, Burns R, Martindale J. Caregiver appraisals of functional dependence in individuals with dementia and associated caregiver upset: Psychometric properties of a new scale and response patterns by caregiver and care recipient characteristics. Journal of Aging and Health. 2005;17:148–171. doi: 10.1177/0898264304274184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schwarz K, Roberts B. Social support and strain of family caregivers of older adults. Holistic Nursing Practice. 2000;14:77–90. doi: 10.1097/00004650-200001000-00012. [DOI] [PubMed] [Google Scholar]
- 32.Hunt C. Concepts in caregiver research. Journal of Nursing Scholarship. 2003;35:27–32. doi: 10.1111/j.1547-5069.2003.00027.x. [DOI] [PubMed] [Google Scholar]
- 33.National Alliance for Caregiving and the American Association of Retired Persons. Caregiving in the US. Washington, DC: NAC and AARP; 2004. [Google Scholar]
- 34.Connell CM, Shaw BA, Holmes SB, Foster NL. Caregivers’ attitudes toward their family members’ participation in Alzheimer disease research: Implications for recruitment and retention. Alzheimer Disease and Associated Disorders. 2001;15:137–45. doi: 10.1097/00002093-200107000-00005. [DOI] [PubMed] [Google Scholar]
- 35.Drentea P, Goldner MA. Caregiving outside of the home: The effects of race on depression. Ethnicity and Health. 2006;11:41–57. doi: 10.1080/13557850500286396. [DOI] [PubMed] [Google Scholar]
- 36.Hebert RS, Koenig HG, Arnold RM, Schulz R. Caregiver intervention research: An opportunity for collaboration between caregiving investigators and African American faith communities. Journal of the National Medical Association. 2006;98:1510–1514. [PMC free article] [PubMed] [Google Scholar]
- 37.Sörensen S, Pinquart M, Duberstein P. How effective are interventions with caregivers? An updated meta-analysis. The Gerontologist. 2002;42:356–372. doi: 10.1093/geront/42.3.356. [DOI] [PubMed] [Google Scholar]
- 38.Zarit SH, Stephens MA, Townsend A, Greene R. Stress reduction for family caregivers: Effects of day care use. Journals of Gerontology series B: Psychological Sciences and Social Sciences. 1998;53B:S267–S277. doi: 10.1093/geronb/53b.5.s267. [DOI] [PubMed] [Google Scholar]
- 39.Roth DL, Mittelman MS, Clay OJ, Madan A, Haley WE. Changes in social support as mediators of the impact of a psychosocial intervention for spouse caregivers of persons with Alzheimer’s disease. Psychology and Aging. 2005;20:634–644. doi: 10.1037/0882-7974.20.4.634. [DOI] [PubMed] [Google Scholar]