Abstract
We interviewed 15 individuals who completed a behavioral weight loss treatment study with the aim of exploring participants’ reflections on their feelings, attitudes and behaviors while using a paper diary to self-monitor their diet. Constant comparative and matrix analysis procedures were used to analyze interview data; the qualitative results were then interfaced with descriptive numerical data on individuals’ adherence to self-monitoring and weight loss. Three categories of self-monitoring experience were identified (a) Well-Disciplined – those who had high adherence to self-monitoring, high weight loss and a “can do” positive approach, (b) Missing the Connection – those who had moderate adherence, moderate to low weight loss, and an “it’s an assignment” approach without integrating self-monitoring into every day life, and (c) Diminished Support – those who had poor adherence, poor weight control, and were adversely affected by co-existing negative factors. Given the variations in how individuals integrated the process of self-monitoring, we need to consider individualizing self-monitoring strategies to improve adherence.
Keywords: adherence, behavior, change, obesity, weight management
According to the 1999–2000 National Health and Nutrition Examination Survey (NHANES), obesity is increasing at an alarming rate (Mokdad et al., 2001). Globally, one billion people are overweight and 300 million are obese (World Health Organization, 2008). Excess weight is associated with several chronic conditions, including type 2 diabetes, dyslipidemia, hypertension, osteoarthritis and sleep apnea.
One approach to the treatment of overweight and obesity, behavior modification, uses a wide range of behavioral strategies, including goal setting and self-monitoring (Wing, 2004). Self-regulation is integral to behavior modification for weight control. Kanfer described self-regulation as a process having three distinct stages: self-monitoring, self-evaluation, and self-reinforcement, and suggests that changing habits requires developed self-regulatory skills (Kanfer, 1970, 1971, 1980).
Self-monitoring is a method of systematic self-observation, periodic measurement and recording of target behaviors with the goal of increasing self-awareness (Kanfer, 1970; Wilde & Garvin, 2007). The awareness fostered during self-monitoring is an essential initial step in promoting behavioral change. The interplay among awareness, self-observation, recording, and self-evaluation can enhance self-management by improving how individuals self-monitor or attend to their health (Wilde & Garvin, 2007). Self-monitoring has been used to enhance self-management in numerous chronic illnesses including diabetes (Davis & Alonso, 2004), asthma (Hendricson et al., 1996), heart disease (Halm & Penque, 2000) and cancer (Larson et al., 1999).
Support for the role of self-monitoring in weight control first emerged in 1993 in a study conducted by Baker and Kirschenbaum (Baker & Kirschenbaum, 1993). Their seminal, cross-sectional study showed a strong relationship between self-monitoring and increased weight loss and longer-term maintenance of weight loss. Later, Boutelle and colleagues used self-monitoring in a clinical trial as an intervention to prevent weight gain around the end-of-the-year holidays and demonstrated the benefits of using self-monitoring to manage weight control (Boutelle, Kirschenbaum, Baker, & Mitchell, 1999.). More recently, other studies have confirmed these earlier findings (Burke et al., 2008; Wadden et al., 2005).
Although self-monitoring has been part of numerous weight loss programs and its effectiveness is well accepted, individuals’ responses to self-monitoring and success with the strategy vary greatly. Little is known about the actual experience of those who use self-monitoring, or the personal or environmental factors that contribute to or are barriers to successful use of this behavioral weight loss strategy. The purpose of this study was to gain insight into the experience of self-monitoring and to describe weight loss program participants’ feelings, attitudes and behaviors while using a diary to self-monitor their diet and exercise.
Method
This descriptive study was ancillary to a randomized clinical trial (PREFER Trial) involving 176 adults in three cohorts enrolled in a 12-month behavioral weight loss intervention followed by a 6-month maintenance period. The details of the PREFER Trial have been reported previously (Burke, Choo et al., 2006). A cognitive behavioral intervention was delivered through 32 group sessions over 12 months. The group sessions occurred weekly during the first six months, bi-weekly for three months and then monthly for the last three months. According to baseline weight, each person was given a daily goal of calories (e.g., 1200–1500 calories per day for females), a fat gram goal (25% of daily calories) and a physical activity goal. They were instructed to record their daily food (calorie and fat grams) intake and engagement in physical activity in their weekly paper diary. The participants met in groups of 14 to 20; two groups met on the same evening (6 PM and 7 PM). At each session, the participants were weighed privately and submitted their diaries from the previous week(s). Group sessions focused on cognitive-behavioral strategies and included an opportunity to share experiences of self-monitoring.
Our ancillary study was conducted in two sequential parts: (a) an instrumented paper diary was used to electronically record participants’ adherence to self-monitoring during the trial (Burke, Sereika et al., 2006), and (b) an interview-based exploratory study of participants’ experience of self-monitoring was conducted after completion of the trial. In this article we are reporting on the results of Part b; the results of Part a have been reported elsewhere (Burke, Sereika et al., 2006; Burke et al., 2008). Approval for both arms of the ancillary study was obtained from the University of Pittsburgh Institutional Review Board.
Participants
We purposefully recruited our sample from the group of 36 participants in Part a of the ancillary study who recorded their diet and exercise using a specially formatted, electronic paper and pencil diary and had most recently completed the 18 month study. Participants were contacted by phone by the project director and were invited to take part in a one-hour interview about what it was like to self-monitor. Fifteen individuals responded. Each was offered $25 for the time and effort involved.
Of the 15 participants, 12 (75%) were women and 9 (56%) were White. Participants ranged in age from 38 years to 56 years, with the average age being 48 years. The group, on average, had completed 15 years of formal education. Thirteen were married or living with a partner, one had never married, and one was divorced. Their BMI at entrance to the program ranged from 28.4 to 41.1 kg/m2 (mean: 35.2 kg/m2). Fifty percent of the participants had participated in organized weight loss programs prior to enrolling in the PREFER trial, e.g., Weight Watchers.
Examination of the PREFER trial data for this group of 15 individuals revealed that the average weight loss from baseline to six months was 13.2 kg; the range was 3.2 to 30.1 kg. At the end of the study (18 months), which followed the 6-month, no-contact maintenance phase, the range of weight change from baseline was a loss of 29.7 kg to a gain of 2.5 kg with a mean of 5.1 kg lost for the women and a mean of 21.2 kg lost for the men.
The PREFER trial also provided data on the interview-based study participants’ rate of adherence to self-monitoring. Since participants were advised to record daily, adherence to self-monitoring was defined as the number of days that participants recorded a full day of food intake; for example, if a person completed recordings of breakfast, lunch and dinner for 3 of 7 days, their adherence was 43%.
Data Collection
We developed a semi-structured interview format consisting of ten open-ended statements and questions. The opening statement, “Please tell me about your experience using the diary” was designed to encourage participants to express their own views and experiences. Using open-ended statements and probes, participants were encouraged to discuss whether they had prior experience keeping a diet and exercise diary for weight loss, the most difficult problems in using the diary, the easiest part about using the diary, the setting in which they wrote in the diary and whether other persons influenced their self-monitoring. During the interview, participants were asked to remember a time writing in the diary and describe their feelings while using the diary. Additionally, participants were urged to discuss how events in their lives influenced self-monitoring.
The interview format was tested during interviews of two volunteers from our work environment who had participated in a weight reduction program involving the use of a diet and exercise diary. The interview format continued to develop over the course of the study, with additional inquiries seeking clarification of ideas and hypotheses developed during analysis.
Participants were interviewed one to five months after completion of the weight loss program. Informed consent was obtained prior to the interview. All interviews were conducted in a private room in the School of Nursing Clinical Research Center by the first author and audio-taped on two tape recorders. Recorded interviews were transcribed, checked by the interviewer for accuracy and observations were added.
Data Analysis
We used an inductive approach to qualitative content analysis. The team (an expert in behavioral intervention for weight reduction, an expert in qualitative research methods, a doctoral and a bachelor-level nursing student) met weekly during data collection and analysis.
After completing the first three interviews, we initiated development of a coding scheme and followed standard procedures for coding qualitative data (Field & Morse, 1991; Miles & Huberman, 1994), assigning labels to text passages that contained a pertinent concept or notion. For example, nearly all interviewees described the experience of examining their written record of dietary intake as both shocking and informative. The term “seeing it in black and white” was used by participants and that phrase became a code for identifying the text describing these reactions. Another example of a code identified early in the analysis process was “playing catch up,” i.e. neglecting to record daily and then attempting to fill in the diary more than a day or two later. Our fully developed code list contained 26 items. We clearly defined each item and provided examples of each one. At least two members of the team coded each interview, compared codes and negotiated final decisions. We combined several codes, reducing the total number of codes to 20. ATLAS-Ti software (ATLAS-Ti, 5.0, Scientific Software, Berlin) was used to assist with code entry, filing, organization and retrieval of data.
The research team studied each interview and met weekly for discussion. We used constant comparative analysis techniques, i.e. comparing and contrasting sections of the participants’ narratives to identify themes and linkages within and between interviews. We recorded analytic memos, drawings, and references to existing literature. A summary of each interview and the analytic work of the team were then circulated to all members. The record of coding decisions and the collected summaries formed an audit trail for tracking our decisions.
When we had completed analysis of 12 of the 15 interviews, we were finding repetition of the themes being identified and recognized that we were nearing saturation. Until that point, in order to maintain neutrality, we had remained uninformed of individual participant’s success in losing weight or rate of adherence to diary keeping. The data providing that information was introduced and transformed to qualitative indicators (high, medium and low) for weight loss and rate of adherence. When the qualified quantitative data were interfaced with the interview data we were able to explore convergence, complementarity and dissonance (Creswell & Plano Clark, 2007; Farmer, Robinson, Elliot, & Eyles, 2006) between the two data sets. We then re-examined each individual’s (a) story of his/her self-monitoring experience, (b) weight loss data, and (c) patterns of adherence. In addition, we used matrix evaluation (Miles & Huberman, 1994) to examine the relationship of categories of the quantitative data with categories generated from the qualitative data. This part of the analysis resulted in the identification of three groups, each with a different self-monitoring experience and a different outcome for weight loss and adherence pattern.
Results
Participants provided retrospective reflections of their experience while self-monitoring their diet. Even though the diary was used for recording eating and exercise behaviors, the focus of participants’ descriptions of their experience was on food and eating, and our findings reflect that focus. They related stories about their actions, feelings, thoughts and attitudes, and they discussed self-monitoring within their social and work environments. We begin our description of results by presenting concepts that were reported by all of the participants.
Concepts Common across Cases
New Beginnings
All participants expressed positive feelings about self-monitoring during the first few months of the program and most lost weight during the first 3–6 months. Optimism was expressed in numerous comments exemplified by the comment, “I think in the beginning you are so revved up. In the beginning it is so much easier.”
Accuracy
Additionally, early in the program most participants reported high interest in maintaining an accurate diary.
Especially in the beginning, the beginning was like I mean I put down everything, like I was taking a pill, you know. I wrote everything down. Everything that I put into my mouth I wrote down.
Seeing it in Black and White
As participants learned about the calorie and fat content of foods, the examination of their diaries heightened their awareness of their eating behaviors and excessive calorie and fat consumption. They expressed surprise and simultaneously, recognition of their overeating and expressed a need to make significant changes in their eating habits.
When I started finding out the calorie content of stuff and the fat grams, I was like “Oh, my God, no wonder, I am fat.”
You don’t think you are eating what you are eating, but when you see it on paper and you have to add a total, you think, “Oh boy, I really over did it.”
A Tool for Staying on Track
At some point, participants recognized the value of self-monitoring as a method for maintaining limits or staying on track. “When you look at the numbers you see you are already over half way or however far, you know you shouldn’t be eating anything else that day.”
Everyone Played “Catch Up”
All participants admitted that on some days they were unable to complete an accurate record of food intake. Changes in schedule, lack of time, forgetting to carry the diary with them, or lack of organization for making entries interfered with daily completion of the diary.
Most of the time I would strive to maintain that 1800 [calories], and a lot of times I did. But the weekends … I was not on the same schedule.
Any recording you do is better than no recording at all. So if you can go back and kind of reconstruct it, not that you want to do that all the time … it is better to get an idea of what you did for the week—than to just throw up your hands and say “My God, I can’t remember anything.”
Group Support
Most participants indicated that the group meetings were an important source of social support and motivation to complete the diary. They discussed the impact of the reduction in the frequency of the group sessions.
During the first few months, the group was good, but whenever we went to not coming every week. Every two weeks I still did well, but when we ended up coming a month at a time or whenever, I didn’t do as well.
Being Part of a Research Study
Participants expressed a sense of commitment to being part of a research project. Many indicated that they felt a responsibility to be more precise with self-monitoring because this influenced the quality of the information being collected.
Even though (the program) was for yourself, it was still like, I knew I was part of the study. I knew that the data I was providing, or not providing, would impact it somehow.
New Knowledge and Skills
All participants reported that the most persistent behavior changes were label reading, monitoring of fat intake, and control of portion size.
Everything I purchase or pick up to buy, I read the labels. Some things I won’t buy if it has too much sodium or too much sugar … Even if I am buying junk, I compare what has the least of evils of junk <laughs> and that’s something that I never did before.
We just stopped going to fast food restaurants. We make sure we eat before we leave, and go home and eat something better.
The above concepts, identified early in our analysis and present in all cases, were familiar to those team members who had worked with persons in a weight loss program. The novelty of a new program, the learning process, use of the diary, and group support during the first six months of the program were accompanied by weight loss for all participants. Although the participants’ reports of early optimism and ways of adapting to self-monitoring were similar, differences in attitude toward self-monitoring, skills and persistence in maintaining the diary, and ability to internalize the self-monitoring process became evident over time.
Emergence of Well-Disciplined, Missing the Connection and the Diminished Support Groups
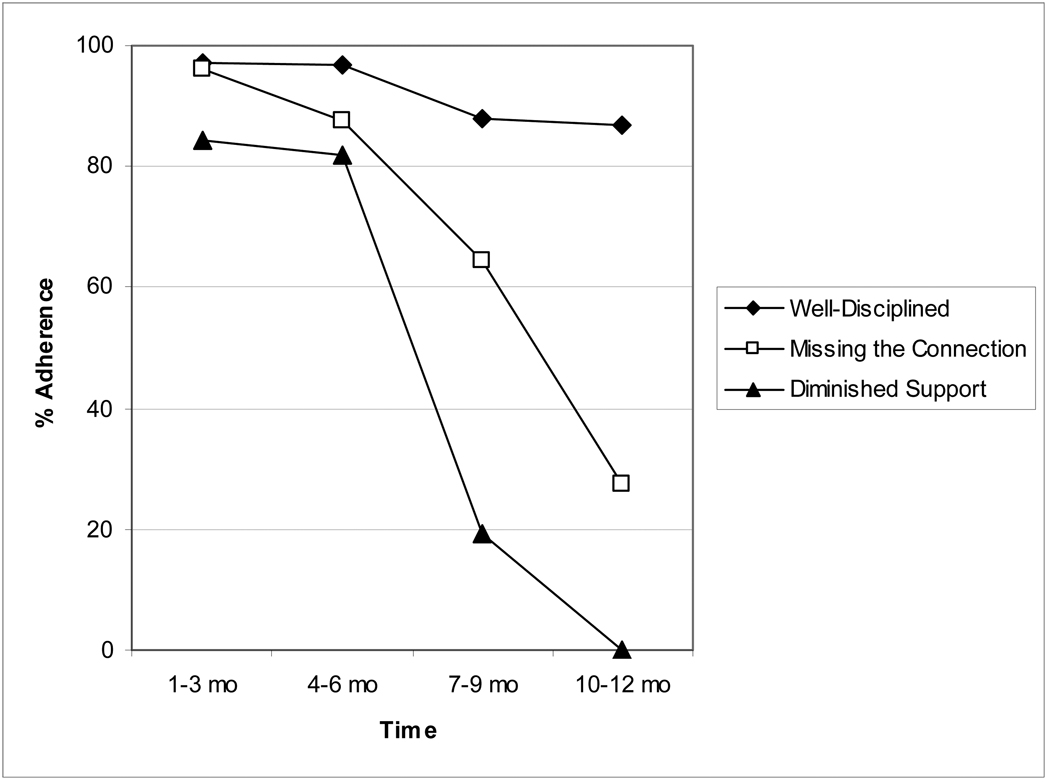
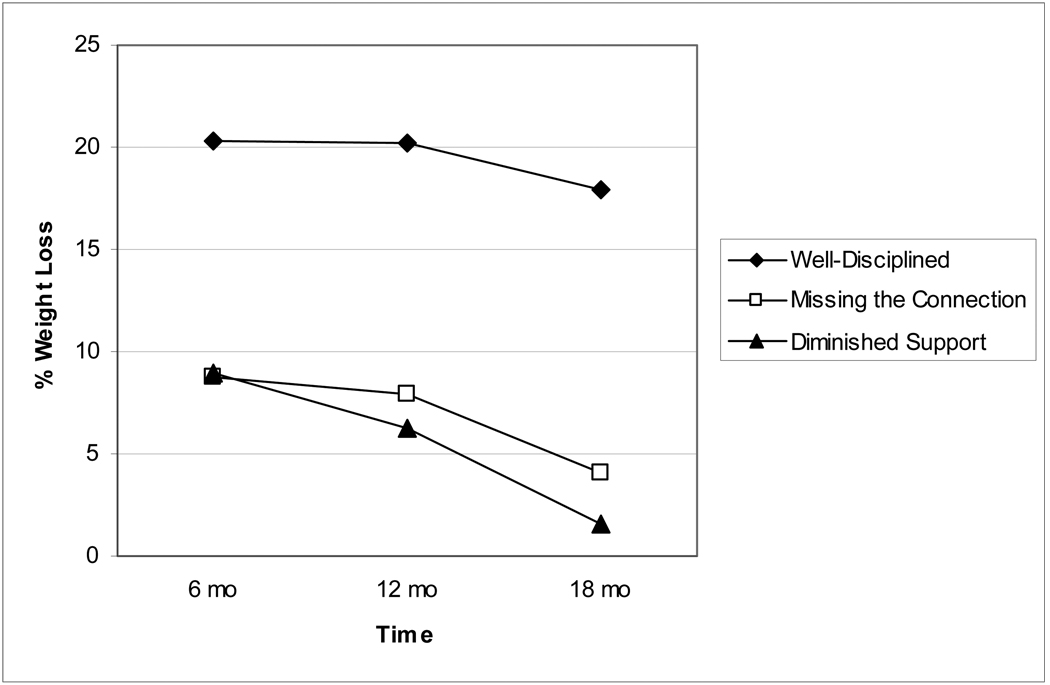
Our analysis revealed three categories of self-monitoring experience: (a) the Well-Disciplined – those who had high adherence to self-monitoring, high weight loss and a positive approach characterized by an attitude of “can do,” “do for myself,” and “it just becomes part of your thinking,” (b) the Missing the Connection – those who had moderate adherence, moderate to low weight loss, and a negative “never got easy,” “boring,” “something you have to hand in” approach to self monitoring, and (c) the Diminished Support – those who had poor adherence, poor weight loss or weight gain, and were adversely affected by co-existing negative factors such as “difficult life changes,” “sugar or food addiction,” or lack of support from significant others.
Well-Disciplined
Five participants were in the Well-Disciplined category; four of them were male and had not previously participated in a weight loss program. Four were White, one was Hispanic, and ranged in age from 38 to 54 years. They were highly adherent to self-monitoring through the twelve-month intervention period. They lost 14% to 26% of their body weight at 6 months and at 18 months were able to maintain that loss so that their weight loss was 12% to 25%.
Commitment
The Well-Disciplined participants’ narratives revealed that self-monitoring and weight loss were given high priority in terms of time, energy and focus. They expressed commitment and independence. Three of these individuals indicated that the diary was carried with them constantly.
You had to truly commit to it, and say, “I’ll do my best with it, pass or fail. I’m gonna do my best with it.” That’s the only way to really approach it.
I’m not someone who needs a lot of encouragement to continue with something. I had a goal set and knew I had to get there.
You don’t take a day off.
Although recognizing that self-monitoring can be tedious, the Well-Disciplined participants articulated ease with using the information provided, taking on the mental tasks of calculation and working toward goals for integrating self-monitoring into their lives.
It is just a 15-minute deal … 1800 calories, 50 grams of fat, walk 25 minutes a day. That’s the formula.
Weight loss is such a physically driven item in terms of what it does to you [but] it’s the mental aspect of it that is the biggest aspect … you do it for the physical side, but the mental side is the thing that will work towards it or hinder it.
Integrating self-monitoring into everyday life
The Well-Disciplined participants verbalized an active and self-driven adoption of self-monitoring as an on-going strategy integrated into daily life. They readily moved beyond the process of calculating and recording daily intake to recognizing the value of using their recordings to plan daily or weekly food intake. Their narrations include important recognition of the inter-relationship of self-monitoring and planning.
When you are coming up to dinner, if you have consumed 1200 calories, you know that you have 500 … if you want to maintain your goal.
Self-monitoring mentally prepares you for what you are going to do the next day … after a while it just flows.
They recognized a strong linkage between self-monitoring and weight loss; thus, weight loss became a prime motivator to continue the self-monitoring process.
After I had lost a pound here, a pound there, maybe five, six pounds, after I hadn’t been able to lose in years, and really had tried hard, I just figured well this had got to be the monitoring. I wanted to monitor … I wanted to keep good track.
The Well-Disciplined participants discussed learning from the thoroughness of their efforts, noting their own individual patterns, and experienced the highest internal self-reinforcement because of their large weight loss.
With recording, you could see what you had left [for the day] or you can go back to [prior recordings] and you can actually get a pattern for what you can have and what you can’t have. Basically you don’t need books after a while because you know how many calories are in whatever.
I think that by being exact on the diary helped me to transfer into regular life because now I can kind of remember exactly what it was, how I was looking at things, different portion sizes … it prepared me for the next step … just living your life normally but encompassing all those eating habits.
They projected into the future, seeing self-monitoring as a tool, ready for use when needed.
I think if it started feeling like I’m starting to really put some weight back on then I would sit down and do that again.… I would go back to monitoring. Then it would show me what I am doing wrong.
Supportive spouses
The Well-Disciplined participants reported significant support from their spouses and co-workers.
Actually a couple times we actually called the restaurant up to find out what they put in it [the entrée] … it wasn’t hard to call them up a couple times when you have a support person to help you out.
It was positive because my husband helped me … so when we cooked I didn’t feel like I was a salmon swimming upstream.
In summary, the Well-Disciplined participants embraced the strategy of self-monitoring and integrated it into everyday life. They articulated few problems with finding the time and focus for self-monitoring, and they had cooperation from significant others to carry through with the strategy. Their narratives included learning from examining past diary records and perception of self-monitoring as a tool for weight management.
Missing the Connection
Five participants were characterized as Missing the Connection. They were all women between the ages of 40 and 56 and had all dieted previously, each having lost 10 to 20 pounds at least once in the past. Despite being moderately adherent to the self-monitoring protocol over the course of the study, weight loss was minimal, averaging 4% of their original body weight. These participants articulated a mechanistic view of self-monitoring, experiencing it as a rote activity or assignment for the study. Unlike the Well-Disciplined participants, there was no evidence that participants in the Missing the Connection group ever used the information garnered from their diaries, which could be used to plan their eating for the days or weeks ahead.
It was always a struggle … I felt like I was in school and my teacher told me to do this assignment so I did the assignment.
I didn’t necessarily look at it as something for me. I am a participant in the study.
To me it [self-monitoring] is almost like a gimmick to try to lose weight. If you write it down, you are going to lose weight. I never, in my mind, can figure it out what the connection is to make it work.
Competing responsibilities
The Missing the Connection participants described trying to maintain some focus on their own needs while meeting responsibilities to family and employers.
It was just a matter of, I guess my lifestyle. I don’t really have time for myself because when I get to work people are waiting at my door to ask me questions … meetings, 6 in an 8 hour day or 10 hour day.
I mean, none of it, nothing you really ask is difficult, it’s just time consuming … and some days you are just too busy or things happen, and I just didn’t do it.
It is like, if it is for yourself, it is not as high a priority for the day.
Organizational deficiencies
They described difficulty maintaining organization and accuracy.
Like if I am at work and my book is at home, I would write on pieces of paper and stick it in my purse. Then when I got home if I was involved in something or too tired … half the time I threw away the paper in the garbage.
At first, I was writing down every little thing. I was very good with it, but as time went on, I kind of got a little sloppier.
Emotional eating
The Missing the Connection participants described emotional issues related to their eating that interfered with attempts to alter their behaviors and negated the impact of self-monitoring on their food intake.
I am an emotional eater … and reaching for that ice cream … even if I know I have to write it down. I knew what I was doing, but it didn’t stop me from doing it.
Sometimes I get to the point where I don’t care. I’ll just eat this pack of cookies because they look good.
Slacking off
Although the Missing the Connection group maintained some adherence to self-monitoring throughout the year of the program, they indicated that it had lessening impact on what they consumed. The responses suggest that these individuals did not completely understand the purpose of self-monitoring and that they did not care or could not resist urges related to emotional arousal.
You see what you did in the morning, and you see something not so good. There is still time to redeem yourself if you are careful the rest of the day, and then you don’t.
I knew what I needed to do, I just didn’t do it.
Being part of the program
The participants were more dependent upon the structure and support of the weight loss intervention. They reported having difficulty continuing to self-monitor when the group meetings became less frequent.
The less we had to be here, I wasn’t really paying attention like I should. I just kind of slacked off, and I would miss a day recording … I think it was because, not being here, you don’t have that push.
You know, it’s hard, like it’s better for me if I have to do it for somebody else because I know they are really going to look at it and scrutinize it.
Yeah, I liked the program thing … It helps me. When I am on my own, it is just a matter of okay, I can eat this, no one cares.
Social support
Several of the Missing the Connection participants received little support from significant others or coworkers. Embarrassment related to previous failed attempts to lose weight interfered with communication.
My husband is not very supportive about weight loss, he never has been. He accepts me as I am. But I think often when I am getting successful he is bringing home things that would be difficult for me not to eat, like ice cream. And that’s a problem for me. So you know I would say that, yeah, he would sabotage me.
No one at work knew … I think that was probably my problem. If I could just have put my diary right out in the middle [of the desk] I probably would have done it better, but I didn’t want people to know because I had been on so many other things.
Collectively, the individuals in the Missing the Connection group had a difficult time persevering in their self-monitoring and weight-loss efforts. They were challenged by “emotional eating” that often surpassed the desire to control their food intake. They felt the need to focus on the care of others rather than themselves and most did not have strong social support networks outside of the program.
Diminished Support
The four participants in the Diminished Support group were all women aged 37 to 55; they had been in multiple weight reduction programs. They did well during the first six months of the program; three of them lost 12% to 13% of their initial weight while adherence to self-monitoring ranged from 66% to 98%. During the last six months, self-monitoring dropped off dramatically, and ceased at 10 months. Two participants regained approximately 6%, the third lost just 3.4% of body weight during the 6-month period but gained back 2%, and the fourth gained 3% over her baseline weight.
Inundated
Like the Missing the Connection participants, the Diminished Support participants found it difficult to consistently keep the diary with them and maintain organization of their notes and recordings. Whereas the Missing the Connection participants most often attributed the lack of organization to boredom or dislike of the task, the Diminished Support participants described “trying times” and physical exhaustion.
[The diary] was usually in my purse. Most of the time, I think I would leave it at home. But sometimes I had it in my purse. But then I would forget I had it in my purse, so I would write it on a paper. It was a trying time. I was going through a period of being exhausted and I could not think and remember anything.… I wound up having to go to the doctor because I was so exhausted.
I would forget to take the diary to work … would mark stuff down on pieces of paper … [thinking that] when I get home I’ll record. I never did. If you waited to the end of the week, it got totally overwhelming ….
Tedium
Like the Missing the Connection participants, the Diminished Support participants spoke of tedium; but for the Diminished Support participants, the tedium was related to underlying problems and responsibilities. In the following quote, the participant indicates the existence of competing problems. The “other things going on” in her life included a new marriage, having children to care for, and starting back to college. She clearly admits her inability to continue keeping the diary.
After a while because of all the other things that were going on in my life, it became tedious. I am not real good at doing things ritualistically … I get bored, and something like snaps inside of me and I will not do it <growls> … so eventually [recording] just kind of went to the wayside.
Truthfulness
The Diminished Support group readily admitted their eventual inability to maintain the diary and abandonment of attempts to catch up or pretend to be maintaining. They expressed concern about truthfulness and fulfilling promises.
If I didn’t remember, then I wouldn’t put any data in, but it made me feel bad. But I wouldn’t put false stuff in … it would have been a lie.
Some of the books were half done. Then finally it was like I’ll get it to you, but then I didn’t. That was hard for me because I am not a liar. It’s like I don’t promise unless I am going to deliver.
Assume responsibility for behavior
Whereas the Missing the Connection group described difficulty with weighing, measuring and computing, the Diminished Support participants’ comments revealed their willingness to assume responsibility for their own actions regarding self-monitoring and lack of weight loss; they were more likely to self-blame for the lack of continuing progress in diary keeping and weight loss.
It is not like the study required too much from a person. It didn’t … I just didn’t follow through … that’s what makes the difference.
It boils down to personal choices. I chose not to take advantage of all of the opportunities presented.
Inability to self-nurture
Like Missing the Connection, the Diminished Support group was unable to focus on their own health-related needs when faced with competing responsibilities.
I just didn’t have time … [there was] my job or helping my kids with their homework more. My life just became more demanding in other areas. What I did was I stopped thinking about taking care of me and started thinking about everybody else again. I got sucked back into doing what I’ve been doing for the past 19 years.
Sabotage by others
Many participants experienced unsupportive or sabotaging behaviors from coworkers or significant others from time to time; however, all four Diminished Support participants had significant others who thwarted their efforts to change. The unsupportive behaviors of the family members of the Diminished Support participants were described as follows.
My mother, I think she was really the hardest person on me … when I gained it back she said, “I can’t believe you gained all that weight back.”
He [husband] will say things like, “Well, it’s after ten o’clock at night. I don’t know why you are eating that.” He is not subtle at all, he’s not.
I never mentioned it to my husband. He doesn’t pay attention to stuff like that, and I probably didn’t do it [self-monitoring] around him. I would write it in our computer room. I would do it up there. He wouldn’t know.
The Diminished Support participants shared many of the problems of the Missing the Connection group, e.g., difficulty maintaining self-nurturing behaviors (Nemcek, 1987), and problems with organization of diary materials. All four Diminished Support participants were forthright about their inability to maintain their diaries after the first six months, citing competing responsibilities, physical illness, relocation of a significant supporter and sabotaging or uninvolved husbands. Whereas the struggling Missing the Connection group had one or two of the above factors impeding self-monitoring and weight loss, the Diminished Support participants were overwhelmed as they experienced difficulty in several areas simultaneously. They stopped recording food intake and ceased losing weight or regained weight.
Writing it Down was Not Natural
All but one participant could be described as a Well-Disciplined, Missing the Connection or Diminished Support participant. This participant lost 13% of her body weight over the 18 months of the program. She was 98% adherent to self-monitoring for the first three months and 55% during the next three months; then she stopped using the diary. This pattern of persistent weight loss after discontinuation of self-monitoring was not observed in any of the other 14 participants. During the interview this participant candidly revealed, “It was very hard to self-monitor myself … I think it is human nature not to write things down. I would get stressed out … cheat … pick up a candy bar and say, ‘Well, I just won’t write it down.’” This participant readily indicated that she learned a lot during her early self-monitoring, saying, “It taught you how to eat and make better choices.” She indicated that “getting on the scale” became her major motivating factor. She described an older daughter who provided support for weight control. Her final comments reflected a spirit of independence and self-assurance, “I had certain goals I set for myself. I wanted to lose weight wise, and I met that.” In an article focused on adherence and non-adherence in diabetes, Ingadottir and Halldorsdottir (2008) provide a possible explanation for this variant case in their discussion of the notion that, for some persons, adherence threatens autonomy and the need to feel normal. This participant may have acted to protect her own sense of self.
The categorization of 14 of the cases as Well-Disciplined, Missing the Connection and Diminished Support is supported by analysis of interview data and interface of that analysis with descriptive numerical data including weight loss and adherence to self-monitoring. The characteristics of the Well-Disciplined group, mostly males who were new (or had made few attempts) to lose weight in an organized program, were positive, committed, self-nurturing, and well-organized. They had excellent social support and were able to integrate the self-monitoring strategy into everyday thinking and living. They also had the most reinforcing feedback from the weight loss they experienced. The Missing the Connection participants were women, more likely to have participated in prior weight reduction programs, self-sacrificing, disorganized, task oriented and likely to view the self-monitoring as an assignment rather than an integral part of everyday life. The Diminished Support participants experienced barriers to both weight loss and self-monitoring; they were honest, apologetic, and even remorseful regarding their lack of success; they described lack of support from significant others and inability to overcome their emotional need to eat.
Although we have described three categories of the experience of self-monitoring, the clear differences were between the category of Well-Disciplined and the categories of Missing the Connection and Diminished Support. All of the participants took on the responsibility to self-monitor, turned in their diaries, came to weekly meetings, and lost weight during the first six months of the program. Key differences occurred during the last 12 months of the study. The Well-Disciplined participants were able to maintain their weight loss through the last six-month maintenance period, and the Missing the Connection and Diminished Support participants were not. The weight loss and adherence data of the three groups are summarized in Figure 1 and Figure 2.
Figure 1.
Trajectory of Mean Adherence to Self-Monitoring
Figure 2.
Trajectory of Mean Percent Weight Loss
Discussion
We explored the experiences and feelings related to the self-monitoring of eating behaviors among participants who had completed an 18-month behavioral weight loss study. Our results suggest that positive personal feelings, attitudes characterized by commitment and determination, aptitudes favoring organization and computation, and support from significant others promote and sustain self-monitoring. Whereas, participation in multiple prior programs and attempts to lose weight, intolerance of the time, computational and organizational burdens of self-monitoring, inability to focus on and nurture one’s self, and lack of social support lead to decreased self-monitoring.
The descriptions provided by the Well-Disciplined group provide a vivid portrayal of the elements of the highly disciplined self-regulation behaviors described by Kirschenbaum and Karoly (Kirschenbaum & Karoly, 1977), as well as other investigators (Baker & Kirschenbaum, 1993; Kirschenbaum & Tomarken, 1982). Weight loss clearly was a motivator for continuing self-monitoring and for actively integrating the practice of self-monitoring into every day life. The combination of personal attributes favoring “keeping track”, commitment to the techniques of self-monitoring, recurrent self-examination, and strong social support provided a foundation for continuing the ability to lose or maintain body weight despite internal and external demands over the 18 month period. Conversely, minimal or lack of weight loss by the groups who completed their diaries as an obligatory assignment without integrating the self-monitoring process practically or cognitively into their every day lives did not receive the positive feedback that weight loss provides.
We found that strong social support was common among the Well-Disciplined group, a finding also reported in the weight loss literature (Verheijden, Bakx, van Weel, Koelen, & van Staveren, 2005; Wing & Jeffery, 1999) and noted as a contributing factor to weight loss maintenance (Elfhang & Rossner, 2005). In conditions, like obesity, that may be stigmatizing (Inouye, Flannelly, & Flannelly, 2001; Piwonka & Merino, 1999) individuals, particularly after repeated failures at weight loss maintenance, are vulnerable and need supporting others. Support may be needed for the person to initiate self-monitoring as well as to continue or maintain it for the long-term (Wilde & Garvin, 2007). The literature notes that spousal involvement in weight loss treatment is not always helpful (McLean, Griffin, Toney, & Hardeman, 2003) as was demonstrated by the responses of several of the Missing the Connection or Diminished Support participants who described spousal antagonism or sabotage. For those who are lacking supportive relationships, the support of others in the program, i.e., group members and interventionists, becomes more important. For some persons, more frequent group meetings or finding a substituting situation that provides needed support may increase the likelihood of successful self-monitoring.
The conceptual linkage of three attributes, (a) failure to cognitively integrate selfmonitoring into everyday life (persistent sense that this was “just an assignment”), (b) lack of self-nurturing (or pre-occupation with taking care of others), and (c) emotional eating were dominant in the Missing the Connection group and also present in the Diminished Support group. These participants focused on meeting the needs of others over themselves and may have used food to fulfill their own needs. The Missing the Connection group continued to turn in their diaries as requested; their adherence rate was over 80% during the first six months and continued at a lower rate through a year. Yet, they were unable to maintain a desirable rate of weight loss. Although they were able to understand the value of self-monitoring, emotional difficulties, the need to eat and inability to focus on their own needs dominated.
A characteristic that was unique to the Well-Disciplined group was that it was their first experience seeking weight loss treatment. It is not clear how much of an impact their naiveté to organized weight loss programs had on their behavior. However, not having experienced a prior failure in losing or maintaining a weight loss, these participants were experiencing first time success and mastery and thus an enhanced self-efficacy. The highly disciplined individual and the novice in weight loss are not well represented in the population seeking weight loss treatment today. This information might point to a possible advantage to identifying individuals’ personality characteristics and then guiding them toward approaches to self-monitoring that are most congruent with individual attributes.
Another important difference in the Well-Disciplined group from the other two groups is the gender composition; this group consisted of four males and one female. Little is known about male’s pattern of weight loss since many studies exclude males and those that do not, enroll such a small percent that it precludes examining the gender differences (Burke, Warziski et al., 2006). What we observed in our small group was that spouse support for the participants’ weight loss efforts was highly evident, that these men were attempting weight loss for the first time, and that they reported experiencing the needed self-reinforcement related to self-monitoring and self-evaluation that Kanfer proposes is required for ongoing self-regulation. This is an area that is in great need of further study.
All participants discussed the burden of needing to look up in a reference guide the calorie and fat content of all foods eaten, a time consuming exercise in itself, and then manually writing the values in the diary. Participants often addressed the tedium associated with these activities. A few participants managed the burden by frequently limiting their choices to foods of which they knew the calorie and fat content. A problem with this approach is that eventually boredom with eating the same foods might occur, and the individual does not develop an expansive repertoire of healthy foods to eat. Technology is permitting some alternative approaches to the required searching for calorie and fat content of foods by providing dietary software for personal digital assistants that can be used for self-monitoring (Burke, Music, Styn, & Warziski, 2006; Burke et al., 2005). Some of our current research is examining how using a personal digital assistant compares to the use of a paper diary in terms of adherence to the self-monitoring protocol and weight loss. Tate and colleagues have used online self-monitoring successfully in weight loss trials (Tate, Jackvony, & Wing, 2003; Tate, Jackvony, & Wing, 2006; Tate, Wing, & Winett, 2001). However, one limitation to the Internet programs is that they require access to a personal computer. The Diabetes Prevention Program (DPP) took a less demanding approach and required participants to record daily only for the first six months and then one week per month for the remainder of the study (Wing et al., 2004). Another approach might permit the individual to participate more in the decision as to what, when, and how often to record.
Despite the challenges that self-monitoring presents, there is growing evidence of the importance of this strategy in weight loss success. Recently, Wadden and colleagues (2005) as well as Hollis et al. (2008) confirmed the relationship between higher levels of self-monitoring and improved weight loss outcomes. Finally, in a previous study we demonstrated that not only was increased self-monitoring related to better weight loss, but also the timing of the recording in relation to the eating episode (Burke, Sereika et al., 2006; Burke et al., 2008).
This study illustrating a wide variation in personal attitudes, self-assessed aptitudes, and abilities to use self-monitoring techniques over time supports more individualized approaches to using self-monitoring in weight loss treatment. A tailored approach would include self-determined goals, variation of procedures according to personal preferences, and refocusing from adherence and the practical procedures of diary keeping to providing an environment where participants and professionals work together in partnership. Zoffman, Harder & Kirkevold (2008) point out the importance of using a shared decision making (SDM) model, which uses person-centered communication and mutual situational reflection to work towards understanding a person’s difficulties in not being able to successfully manage specific aspects of treatment (e.g. our participants’ difficulties with emotional eating, disorganization with diary keeping, or failure to allot time for self-care). Applying the SDM model to self-monitoring would shift the emphasis from diary-keeping techniques and adherence to the participants’ perspectives and decisions about weight control practices.
Limitations and Strengths
The results of this study should be interpreted with consideration that the data were collected retrospectively, after completion of the study and not while participants were actively engaged in self-monitoring. Thus, the saliency of participants’ experiences may have been influenced by retrospective recall. One study that assessed concurrent and retrospective experiences during weight loss found the retrospective reports of mood greatly exaggerated the negative experiences when compared to the concurrent reports (Wadden, Stunkard, & Smoller, 1986). Other issues that could be considered as limitations include the use of a fairly formal interview room at the same location as the program, and interview by a member of the research team that may have produced some tension or lack of forthrightness in some participants. The interviewer (the first author) had little prior contact with participants, but they knew her as the principal investigator. She reminded them that she was particularly interested in learning about the experience of self-monitoring.
The strengths of this study include interviewer training that emphasized techniques to relax the interviewee and encourage open communication. In addition, the trustworthiness of data collection and analysis procedures were supported by use of tape-recording, computer-based data management, and an audit trail via summaries and memos. Interviews lasting over an hour provided copious opportunity for re-statement or clarifications of individual participant’s descriptions of their experience. Furthermore, we were able to interview individuals across the widely varying weight loss and adherence patterns. Credibility was enhanced by triangulating procedures, examining both qualitative and quantitative data. This predominantly qualitative study, providing a unique and vivid description of the self-monitoring process, supports the individuation of self-monitoring strategies.
Acknowledgments
We would like to thank the individuals who participated in the study for sharing their experiences and time, and to acknowledge Margaret H. Crighton, PhD, RN for her thoughtful review of the paper. Research was funded by NIH-NIDDK (#R01-DK058631 and DK058631-04S1) and the Center for Research in Chronic Disorders (NIH-NINR, #P30-NR03924).
References
- Baker RC, Kirschenbaum DS. Self-monitoring may be necessary for successful weight control. Behavior Therapy. 1993;24:377–394. [Google Scholar]
- Boutelle KN, Kirschenbaum DS, Baker RC, Mitchell ME. How can obese weight controllers minimize weight gain during the high risk holiday season? By self-monitoring very consistently. Health Psychology. 1999;18(4):364–368. doi: 10.1037//0278-6133.18.4.364. [DOI] [PubMed] [Google Scholar]
- Burke LE, Choo J, Music E, Warziski M, Styn MA, Kim Y, et al. PREFER study: A randomized clinical trial testing treatment preference and two dietary options in behavioral weight management -- rationale, design and baseline characteristics. Contemporary Clinical Trials. 2006;27(1):34–48. doi: 10.1016/j.cct.2005.08.002. [DOI] [PubMed] [Google Scholar]
- Burke LE, Music E, Styn MA, Warziski M. Using technology to improve self-monitoring in weight loss. International Journal of Behavioral Medicine. 2006;13 suppl:192. [Google Scholar]
- Burke LE, Sereika S, Choo J, Warziski M, Music E, Styn MA, et al. Ancillary study to the PREFER trial: A descriptive study of participants' patterns of self-monitoring: Rationale, design and preliminary experiences. Contemporary Clinical Trials. 2006;27(1):23–33. doi: 10.1016/j.cct.2005.10.006. [DOI] [PubMed] [Google Scholar]
- Burke LE, Sereika SM, Music E, Warziski M, Styn MA, Stone AA. Using instrumented paper diaries to document self-monitoring patterns in weight loss. Contemporary Clinical Trials. 2008;29(2):182–193. doi: 10.1016/j.cct.2007.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke LE, Warziski M, Acharya S, Styn MA, Steenkiste A, Music E, et al. PREFER Trial: A randomized clinical trial testing treatment preference and two dietary options combined with behavioral weight management. Obesity. (Suppl.) 2006;14:A32. doi: 10.1038/oby.2006.235. [DOI] [PubMed] [Google Scholar]
- Burke LE, Warziski M, Starrett T, Choo J, Music E, Sereika S, et al. Self-monitoring dietary intake: Current and future practices. Journal of Renal Nutrition. 2005;15(3):281–290. doi: 10.1016/j.jrn.2005.04.002. [DOI] [PubMed] [Google Scholar]
- Creswell JW, Plano Clark VL. Designing and conducting mixed methods research. Thousand Oaks, CA: Sage; 2007. [Google Scholar]
- Davis S, Alonso MD. Hypoglycemia as a barrier to glycemic control. Journal of Diabetes Complications. 2004;18(1):60–68. doi: 10.1016/S1056-8727(03)00058-8. [DOI] [PubMed] [Google Scholar]
- Elfhang K, Rossner S. Who succeeds in maintaining weight loss? A conceptual review of factors associated with weight loss maintenance and weight regain. Obesity Reviews. 2005;6:67–85. doi: 10.1111/j.1467-789X.2005.00170.x. [DOI] [PubMed] [Google Scholar]
- Farmer T, Robinson K, Elliot SJ, Eyles J. Developing and implementing a triangulation protocol for qualitative health research. Qualitative Health Research. 2006;16:377–396. doi: 10.1177/1049732305285708. [DOI] [PubMed] [Google Scholar]
- Field PA, Morse JM. Nursing research: The application of qualitative approaches. London: Chapman and Hall; 1991. [Google Scholar]
- Halm MA, Penque S. Heart failure in women. Progress in Cardiovascular Nursing. 2000;15(4):121–133. doi: 10.1111/j.0889-7204.2000.080399.x. [DOI] [PubMed] [Google Scholar]
- Hendricson WD, Wood PR, Hidalgo HA, Ramirez AG, Kromer ME, Selva M, et al. Implementation of individualized patient education for Hispanic children with asthma. Patient Education & Counseling. 1996;29(2):155–165. doi: 10.1016/0738-3991(96)00861-0. [DOI] [PubMed] [Google Scholar]
- Hollis JF, Gullion CM, Stevens VJ, Brantley PJ, Appel LJ, Ard JD, et al. Weight loss during the intensive intervention phase of the weight-loss maintenance trial. Am J Prev Med. 2008;35(2):118–126. doi: 10.1016/j.amepre.2008.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ingadottir B, Halldorsdottir S. To discipline a "dog": the essential structure of mastering diabetes. Qualitative Health Research. 2008;18(5):606–619. doi: 10.1177/1049732308316346. [DOI] [PubMed] [Google Scholar]
- Inouye J, Flannelly L, Flannelly KJ. The effectiveness of self-management training for individuals with HIV/AIDS. Journal of the Association of Nurses in AIDS Care. 2001;12(5):71–82. doi: 10.1016/S1055-3290(06)60264-1. [DOI] [PubMed] [Google Scholar]
- Kanfer FH. Self-monitoring: Methodological limitations and clinical applications. Journal of Consulting & Clinical Psychology. 1970;35:148–152. [Google Scholar]
- Kanfer FH. The maintenance of behavior by self-generated stimuli and reinforcement. In: Jacobs A, Sachs LB, editors. The psychology of private events. New York: Academic Press; 1971. [Google Scholar]
- Kanfer FH. Self-management methods. In: Kanfer EF, Goldstein AP, editors. Helping people change: A textbook of methods. 2nd ed. Elmsford, NY: Pergamon Press; 1980. [Google Scholar]
- Kirschenbaum DS, Karoly P. When self-regulation fails: Tests of some preliminary hypotheses. Journal of Consulting & Clinical Psychology. 1977;45:1116–1125. [Google Scholar]
- Kirschenbaum DS, Tomarken AJ. On facing the generalization problem: The study of self-regulatory failure. In: Kendall PC, editor. Advances in cognitive-behavioral research and therapy. Vol. 1. New York: Academic Press; 1982. [Google Scholar]
- Larson PJ, Uchinuno A, Izumi S, Kawano A, Takemoto A, Shigeno M, et al. An integrated approach to symptom management. Nursing & Health Sciences. 1999;1(4):203–210. [Google Scholar]
- McLean N, Griffin S, Toney K, Hardeman W. Family involvement in weight control, weight maintenance and weight-loss interventions: A systematic review of randomised trials. International Journal of Obesity. 2003;27(9):987–1005. doi: 10.1038/sj.ijo.0802383. [DOI] [PubMed] [Google Scholar]
- Miles MB, Huberman AM. An expanded sourcebook: Qualitative data analysis. Thousand Oaks, CA: Sage; 1994. [Google Scholar]
- Mokdad AH, Ford ES, Bowman BA, Dietz WH, Vinicor F, Bales VS, et al. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA. 2001;289(1):76–79. doi: 10.1001/jama.289.1.76. [DOI] [PubMed] [Google Scholar]
- Nemcek MA. Self-nurturing: A concept analysis. Journal of the American Association of Occupational Health Nurses. 1987;35(8):349–351. [PubMed] [Google Scholar]
- Piwonka MA, Merino JM. A multidimensional modeling of predictors influencing the adjustment to a colostomy. Journal of Wound, Ostomy, & Continence Nursing. 1999;26(6):298–305. doi: 10.1016/s1071-5754(99)90065-7. [DOI] [PubMed] [Google Scholar]
- Tate DF, Jackvony EH, Wing RR. Effects of Internet behavioral counseling on weight loss in adults at risk for type 2 diabetes: A randomized trial. JAMA. 2003;289(14):1833–1836. doi: 10.1001/jama.289.14.1833. [DOI] [PubMed] [Google Scholar]
- Tate DF, Jackvony EH, Wing RR. A randomized trial comparing human e-mail counseling, computer-automated tailored counseling, and no counseling in an Internet weight loss program. Archives of Internal Medicine. 2006;166:1620–1625. doi: 10.1001/archinte.166.15.1620. [DOI] [PubMed] [Google Scholar]
- Tate DF, Wing RR, Winett RA. Using Internet technology to deliver a behavioral weight loss program. JAMA. 2001;285(9):1172–1177. doi: 10.1001/jama.285.9.1172. [DOI] [PubMed] [Google Scholar]
- Verheijden MW, Bakx JC, van Weel C, Koelen MA, van Staveren WA. Role of social support in lifestyle-focused weight management interventions. European Journal of Clinical Nutrition. 2005;59 Suppl 1:S179–S186. doi: 10.1038/sj.ejcn.1602194. [DOI] [PubMed] [Google Scholar]
- Wadden TA, Berkowitz RI, Womble LG, Sarwer DB, Phelan S, Cato RK, et al. Randomized trial of lifestyle modification and pharmacotherapy for obesity. New England Journal of Medicine. 2005;353(20):2111–2120. doi: 10.1056/NEJMoa050156. [DOI] [PubMed] [Google Scholar]
- Wadden TA, Stunkard AJ, Smoller JW. Dieting and depression: A methodological study. Journal of Consulting and Clinical Psychology. 1986;54(6):869–871. doi: 10.1037//0022-006x.54.6.869. [DOI] [PubMed] [Google Scholar]
- Wilde MH, Garvin S. A concept analysis of self-monitoring. Journal of Advanced Nursing. 2007;57(3):339–350. doi: 10.1111/j.1365-2648.2006.04089.x. [DOI] [PubMed] [Google Scholar]
- Wing RR. Behavioral approaches to the treatment of obesity. In: Bray GA, Bourchard C, James WPT, editors. Handbook of obesity: Clinical applications. 2nd ed. New York: Marcel Dekker; 2004. pp. 147–167. [Google Scholar]
- Wing RR, Hamman RF, Bray GA, Delahanty L, Edelstein SL, Hill JO, et al. Achieving weight and activity goals among diabetes prevention program lifestyle participants. Obesity Research. 2004;12(9):1426–1434. doi: 10.1038/oby.2004.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wing RR, Jeffery RW. Benefits of recruiting participants with friends and increasing social support for weight loss and maintenance. Journal of Consulting & Clinical Psychology. 1999;67(1):132–138. doi: 10.1037//0022-006x.67.1.132. [DOI] [PubMed] [Google Scholar]
- World Health Organization. [Retrieved February 5, 2008];Obesity and overweight. 2008 from http://www.who.int/mediacentre/factsheets/fs2311/en/index.html.
- Zoffmann V, Harder I, Kirkevold M. A person-centered communication and reflection model: sharing decision-making in chronic care. Qualitative Health Research. 2008;18(5):670–685. doi: 10.1177/1049732307311008. [DOI] [PubMed] [Google Scholar]