Abstract
Objective: Five years after its introduction, to evaluate the 1992 reform in the out of hours service in Denmark.
Design: Comparison of data before and after reform. Data were collected from published reports, Danish national health statistics, and the Danish trade union for general practitioners.
Setting: Denmark.
Main outcome measures: Number of out of hours services; workload of general practitioners; cost of the service; patient satisfaction.
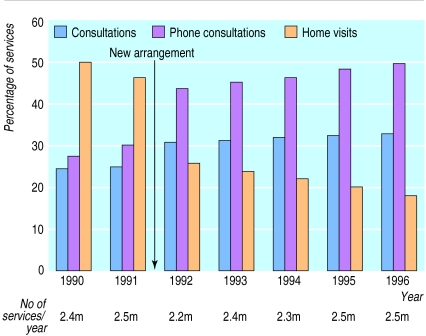
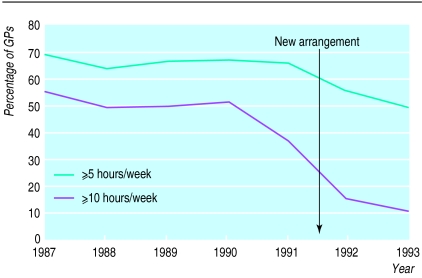
Results: Five years after the reform, the percentage of telephone consultations had almost doubled, to 48%. Consultations in doctors’ surgeries were relatively unchanged, but home visits were much reduced, to 18%. The percentage of doctors who worked 5 hours or more out of hours per week dropped from about 70% to about 50%. Overall patient satisfaction in 1995 was high (72%).
Conclusion: The organisation of the out of hours service, with a fully trained general practitioner in a telephone triage function, is working satisfactorily. Many calls that previously would have required home visits are now dealt with by telephone or through consultations. The out of hours workload for general practitioners has decreased considerably.
Key messages
The out of hours reform in Denmark has resulted in an organisation with a fully trained general practitioner performing the telephone triage function
Hours on call for general practitioners have decreased considerably
Home visits have largely been replaced by telephone consultations
Patient satisfaction has declined slightly
Introduction
During the past decade, out of hours services have been the object of attention in many countries. In Denmark more and more general practitioners became dissatisfied with the workload during out of hours periods. As a result the whole system was reformed on 1 January 1992. The new agreement was part of a reform that aimed to transfer both costs and working hours from out of hours periods to daytime.
Apart from the out of hours service provided by the general practitioners, casualty departments run accident and emergency services in most hospitals. There is an ongoing debate about how to integrate the two services.
The principles of the reform have been detailed elsewhere.1 We report the main points of the reform and describe the effects on number of out of hours services, workload for general practitioners, the cost of the service, and patient satisfaction.
The change
Before 1992, there were three main types of out of hours service in Denmark. For many years the patients’ own general practitioners provided most of the out of hours services. Later it became common for several practitioners in an area to join a rota system to run the service. In most of the larger towns there was a deputising service, in which a non-medical person answered the telephone and almost all the patients received home visits.
Since the reform, each out of hours region covers a whole county (50 000-600 000 inhabitants). The out of hours services are planned and run in cooperation by the general practitioners in a county and the regional health insurance. The organisation of out of hours services in a county has been described previously.1 The out of hours period runs from 4 pm to 8 am on weekdays and throughout Saturdays, Sundays, and public holidays. All health services in Denmark are still free of charge for the patients.
A main result of the reform is that patients now always have direct telephone access to a general practitioner during the out of hours period. This general practitioner has a triage function and decides whether the patient needs a home visit, a consultation in an out of hours consultation room, or just telephone advice. Only fully licensed general practitioners are allowed to run the triage function. Doctors training for general practice may do home visits and consultations, but these are mostly done by general practitioners.
Most counties have now introduced similar computer facilities, with record systems, electronic prescription, accounting, etc. All doctors in the county use the same computer system, with a central server. The doctors on home visits are connected to the triage centre by portable computers and cellular phones.
The doctors are paid a fee for the services and are responsible for costs relating to out of hours duty. Different fees are paid according to the type of care provided, so that the triage doctor is encouraged to use telephone advice instead of offering patients a home visit or referring them to the consultation room.
Duty sessions are kept short—typically eight hours. General practitioners must undertake only one night duty every 35 nights and one evening duty every 15 evenings, and in most places it is possible to be completely free from these duties. The duty is planned so that the doctor is busy and the income is acceptable.
Methods
Data were collected by searching the national and international literature for articles concerning out of hours services, and our own earlier studies were also used.2 The Danish national health statistics contributed data on economic aspects and the number of services used by the population. These data are highly valid because they are based on accounting figures. The Danish trade union for general practitioners makes regular questionnaire surveys of general practitioners on different aspects of their work (income, workload, etc). The response rates are typically 90%, and the surveys are considered very valid. Many counties in Denmark have surveyed patient satisfaction since the reform, and some of them have comparable studies before the reform in 1992. We report the results of the largest and methodologically best studies.
Results
Distribution of services
Figure 1 shows the distribution of the three types of service—a home visit, a consultation at the out of hours consultation room, and advice over the telephone. The reform resulted in a remarkable change in service distribution: home visits dropped from 46% to 18%, telephone consultations almost doubled to 48%, and surgery consultations were relatively unchanged (24% to 33%). The total number of services decreased by 11% just after the reform, but has now reached a level slightly (1%) higher than before the reform.
Figure 1.
Out of hours services in Denmark, 1990-65
Economic aspects
The rearrangement of the out of hours service was part of a comprehensive reform in primary health care, which also included an increase in fees for daytime services. Overall, the reform increased the income of almost every general practitioner, and general practitioners now earn a larger part of their salary on their daytime work. Though 9.6% of the general practitioners received more than a third of their salary from out of hours work in 1990, the proportion had fallen to 3.5% in 1993 and 1.8% in 1995.3,4 The expenses for all out of hours services for the whole country decreased by 16% between 1991 and 1992. However, they have now reached a level very close to that of 1991.5
Workload
Figure 2 shows that general practitioners’ out of hours workload has decreased since the introduction of the reform.3 If some general practitioners in a county like to do more than their share of the out of hours work, some of their colleagues can be let off. The proportion of general practitioners doing no out of hours work rose from 23% in 1990-1 to 36% in 1993-5 (44% of singlehanded practitioners in 1995).3,4
Figure 2.
Out of hours workload of general practitioners, Denmark, 1987-933,4
Patient satisfaction
The proportion of satisfied or partly satisfied patients was higher in 1991 than in 1992. Table 1 shows figures from one of the big counties (n=460 000).6 Patient satisfaction began to increase again as people got used to the service. In 1995 only 19% were not satisfied, but this is still significantly more than in 1991 (<0.0001). Table 2 shows the distribution of satisfaction for patients attending the out of hours service in 1995 in the county of Vejle (n=330 000).7 The patients who did not get the type of service they expected mainly received telephone advice, when they typically expected a home visit. Overall, 72% were satisfied.
Table 1.
Patient satisfaction with out of hours service before and after reform. Number (percentage) of respondents to questionnaires sent to random sample of patients contacting the out of hours service in September 1991, September 1992, and January 1995 (response rates were 76%, 75%, 77% respectively)
| Year | Not satisfied | Partly satisfied | Satisfied |
|---|---|---|---|
| Old arrangement | |||
| 1991 (n=465) | 59 (13) | 89 (19) | 317 (68) |
| New arrangement | |||
| 1992 (n=325) | 90 (28) | 71 (22) | 164 (51) |
| 1995 (n=1203) | 230 (19) | 303 (25) | 670 (56) |
Table 2.
Patient satisfaction with out of hours services in Denmark. Number (percentage) of respondents to questionnaire sent to all 2200 patients contacting the out of hours service in week 44, 1995 (response rate 53%)
| Got the type of service they expected | Not satisfied | Neutral | Satisfied |
|---|---|---|---|
| Yes (n=999) | 99 (10) | 113 (11) | 765 (77) |
| No (n=165) | 51 (30) | 37 (22) | 74 (45) |
| All patients (n=1164) | 150 (13) | 150 (13) | 839 (72) |
Discussion
Medical outcome
We could not find any Danish data that compared health status before and after the out of hours reform, but we have no reason to suspect that the reform has changed medical outcomes. A study from Leicester, England, comparing out of hours care provided by patients’ own general practitioners and commercial deputising services did not find any differences relating to health status.8 It also showed no significant differences in the number of follow up visits, prescriptions, or hospital admissions between patients treated by practice doctors and patients treated by deputising doctors, but an earlier study showed a higher (but non-significant) admission rate when out of hours services were provided by general practitioners from a nearby practice compared with doctors from the patients’ own practice.9
Some people thought that the subsequent use of health services would increase if general practitioners other than the patient’s own did the out of hours service. However, between 1991 and 1993 the total number of contacts in primary care during daytime increased only slightly (1.8%).10,11
Distribution of services
The increase in demand for out of hours services is mainly due to an increase in telephone consultations. As well, many calls that previously would have required home visits are now dealt with over the telephone or through consultations. Replacing a high proportion of out of hours contacts with daytime contacts has been shown to be medically safe.12–14 A study in England found that practice doctors were more likely to give telephone advice than deputising doctors.15 Other studies have found nearly the same overall visiting rate for doctors from the practice and doctors from a practice nearby.9 To give proper telephone advice, it is crucial that experienced general practitioners undertake the telephone triage.
The decline in home visits between 1990 and 1991 is due to the fact that some counties introduced the new arrangement on 1 October 1991. Also, the debate about the coming reform could have initiated the change in service distribution.
Workload
The workload for individual general practitioners has decreased considerably. The finding that about a third of all general practitioners have no out of hours work at all will probably remain constant, reflecting the difference between young general practitioners, who would like to do more out of hours work to earn more money, and older ones, who prefer more spare time. In addition, many general practitioners express their satisfaction with the new type of contact with their colleagues. In the United Kingdom in 1989-90, general practitioners had an average of 26 hours on call, but nearly a third of the general practitioners had no regular out of hours work.16
However, if the rise in demand for out of hours services continues, fewer general practitioners will be able to opt out of the service. And it may be difficult to maintain the upper limit of out of hours work given in the 1992 agreement.
This reform and the introduction of computer facilities have made it possible for a few doctors to manage a large population during out of hours periods. For example, only six or seven doctors are running the out of hours service at night in the county of Aarhus, which has 600 000 inhabitants. The computer record system also supplies automatic feedback to patients’ own doctors after out of hours contacts. The message is sent to the general practitioner on the next weekday by email, fax, or ordinary letter, as appropriate.
Patient satisfaction
The decrease in patient satisfaction is disappointing, but satisfaction is now rising again. Part of the explanation could be that the population has been given far too little information about the background for the reform, and also that politicians failed to tell the public about the intentions of the new arrangement. As one might predict, most of the unsatisfied patients did not have their expectations fulfilled. In time, when people have expectations that match reality better, overall satisfaction will probably be even higher. Nevertheless, patients adjusted quite easily to the changes, and patients’ evaluation is acceptable, with 72% satisfied. The Leicester study showed an overall satisfaction score for practice doctors of 71% and for deputising doctors of 62%.8 Comparisons should be made between care provided by different types of out of hours services. We are planning to compare Denmark and Britain by using a Danish version of a new English questionnaire that measures patient satisfaction with out of hours primary medical care.17
Due to a high degree of similarity over the whole country in provision of services, and to the use of computers, the new system has, as a side effect, increased possibilities for research. Large epidemiological studies on the out of hours system can now be carried out.18,19 With the increasing demand for out of hours services, more research into the possibilities of replacing out of hours with daytime services is necessary.
Footnotes
Funding: None.
Conflict of interest: None.
References
- 1.Olesen F, Jolleys JV. Out of hours service: the Danish solution examined. BMJ. 1994;309:1624–1626. doi: 10.1136/bmj.309.6969.1624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Christensen MB. ] Aarhus: Research Unit for General Practice, University of Aarhus; 1994. Smertepatienters brug af vagtlaegeordningen i Aarhus Amt. [Contacts with the out of hours service in the county of Aarhus. (In Danish.) [Google Scholar]
- 3.Andersen F. Praksisoplysninger per 21.12.93. [Information about general practice on 31.12.93.&. Ugeskr Laeger. 1994;156:6910–6921. . (In Danish.) [Google Scholar]
- 4.Andersen F. Praksisoplysninger per 21.12.95. [Information about general practice on 31.12.93.&. Ugeskr Laeger. 1996;158:6328–6341. . (In Danish.) [Google Scholar]
- 5.National Health Insurance. ] Copenhagen: NHI; 1997. Rapport om tilrettelaeggelse af akutberedskaber. [Report on organising out of hours and accident and emergency services. (In Danish.) [Google Scholar]
- 6.Hansen BL, Elverdam B, Munck A. ] Odense: Institute for General Practice, University of Odense; 1995. Brugervurdering af laegevagtordningen i Fyns Amt. [Patient evaluation of the out of hours service in the County of Funen. (In Danish.) [Google Scholar]
- 7.Rapport om patientvurdering af laegevagten i Vejle Amt. [Report of patient evaluation of the out of hours service in the County of Vejle.] Vejle: County of Vejle; 1995. Health Insurance in the County of Vejle. (In Danish.) [Google Scholar]
- 8.McKinley RK, Cragg DK, Hastings AM, French DP, Manku-Scott TK, Campbell SM, et al. Comparison of out of hours care provided by patients’ own general practitioners and commercial deputising services: a randomised controlled trial. II. The outcome of care. BMJ. 1997;314:190–193. doi: 10.1136/bmj.314.7075.190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Whitby M, Freeman G. GPs’ differing responses to out-of-hours calls. Practitioner. 1989;233:493–495. [PubMed] [Google Scholar]
- 10.National Health Insurance. ] Copenhagen: Sygesikringens forhandlingsudvalg; 1996. Sygesikrings statistik 1991-92. [Health insurance statistics 1991-92. (In Danish.) [Google Scholar]
- 11.National Health Insurance. ] Copenhagen: Sygesikringens forhandlingsudvalg; 1996. Sygesikrings statistik 1993-94. [Health insurance statistics 1993-94. (In Danish.) [Google Scholar]
- 12.Christensen MB, Olesen F. Smertepatienters brug af vagtlaegeordningen i Aarhus Amt. [Patients with pain problems attending the general practitioners’ out of hours on-call in the County of Aarhus, Denmark.&. Ugeskr Laeger. 1997;159:2375–2380. . (In Danish; English summary.) [PubMed] [Google Scholar]
- 13.Christensen MB, Olesen F. Ordination af staerke analgetika ved vagtlaegeordningen i Aarhus Amt. [Ordination of opioid analgesics in out of hours general practice service in the County of Aarhus, Denmark.&. Ugeskr Laeger. 1997;159:2381–2385. . (In Danish; English summary.) [PubMed] [Google Scholar]
- 14.Kjeldsen HC. ] Aarhus: Research Unit for General Practice, University of Aarhus; 1995. Substitutionsmuligheder i laegevagten. Er det muligt at flytte vagtydelser til dagtiden. [Possibilities of transferring services out of hours to daytime. (In Danish.) [Google Scholar]
- 15.Cragg DK, McKinley RK, Roland MO, Campbell SM, Van F, Hastings AM, et al. Comparison of out of hours care provided by patients’ own general practitioners and commercial deputising services: a randomised controlled trial. I. The process of care. BMJ. 1997;314:187–189. doi: 10.1136/bmj.314.7075.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hallam L. Primary medical care outside normal working hours: review of published work. BMJ. 1994;308:249–253. doi: 10.1136/bmj.308.6923.249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McKinley RK, Manku Scott T, Hastings AM, French DP, Baker R. Reliability and validity of a new measure of patient satisfaction with out of hours primary medical care in the United Kingdom: development of a patient questionnaire. BMJ. 1997;314:193–198. doi: 10.1136/bmj.314.7075.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Christensen MB, Bjerre-Christensen C, Olesen F. Spoergeskema paa EDB-skaerm. [Questionnaire put into computers.] Maanedsskr Prakt Laegegern 1994:1071-7. (In Danish.)
- 19.Olesen F, Kjeldsen HC, Christensen MB. Identifying patients for research in general practice. Scand J Prim Health Care. 1996;14:62–63. doi: 10.3109/02813439608997070. [DOI] [PubMed] [Google Scholar]