Abstract
Background
Little is known about short-term bacterial fluctuations in the human vagina. This study used PCR to assess the variability in concentrations of key vaginal bacteria in healthy women and the immediate response to antibiotic treatment in women with bacterial vaginosis (BV).
Methodology/Principal Findings
Twenty-two women assessed for BV using Amsel's criteria were evaluated daily for 7 or 14 days, then at 2, 3 and 4 weeks, using a panel of 11 bacterium-specific quantitative PCR assays. Participants with BV were treated with 5 days of intravaginal metronidazole. Participants without BV had vaginal biotas dominated by lactobacilli, whose levels fluctuated with menses. With onset of menstruation, quantities of Lactobacillus jensenii and Lactobacillus crispatus decreased and were found to be inversely related to Gardnerella vaginalis concentrations (p<0.001). Women with BV had a variety of fastidious bacteria whose concentrations dropped below detection thresholds 1–5 days after starting metronidazole. Recurrent BV was characterized by initial profound decreases of BV-associated bacteria after treatment followed by subsequent increases at relapse.
Conclusions/Significance
The microbiota of the human vagina can be highly dynamic. Healthy women are colonized with Lactobacillus species, but levels can change dramatically over a month. Marked increases in G. vaginalis were observed during menses. Participants with BV have diverse communities of fastidious bacteria that are depleted by vaginal metronidazole therapy. Women with recurrent BV initially respond to antibiotic treatment with steep declines in bacterial concentrations, but these bacteria later reemerge, suggesting that antibiotic resistance in these bacteria is not an important factor mediating BV recurrence.
Introduction
The human vagina hosts communities of microbes that can impact the health of women and their neonates. Bacterial vaginosis (BV) is a common condition, affecting ∼29% of reproductive age women in the USA [1] and is associated with an increase in the risk for pre-term birth [2], HIV-1 acquisition [3] and pelvic inflammatory disease [4]. The pathogenesis of BV is poorly understood. BV is associated with loss of vaginal lactobacilli such as Lactobacillus crispatus and Lactobacillus jensenii, and acquisition of complex communities of anaerobic bacteria. Although the vaginal bacterial biota has been intensively investigated using cultivation (reviewed in [5], [6]) and molecular approaches (reviewed in [7]), few studies have measured short-term fluctuations in the vaginal microbiota using cultivation-independent methods. Persistent or relapsing BV is a common problem with relapse rates greater than 50% within 6 months of treatment [8]. Taxon-directed quantitative PCR (qPCR) has been used to measure levels of key vaginal bacteria and how they change after antibiotic treatment in women with cured and persistent BV [9], but that study did not measure immediate responses to antibiotic treatment. It is unknown whether bacterial eradication was ever achieved, particularly in women with persistent BV. This raises the question of whether the bacteria are non-responsive to antibiotic treatment in women with recurrent BV, or whether the bacteria are eradicated but return with re-inoculation. If the latter situation is most relevant, when and how women with recurrent BV are re-infected is not clear. Longitudinal studies with frequent sampling immediately after antibiotic administration are critical in addressing these questions. Furthermore, the degree of stability of the vaginal bacterial community in women without BV in not well understood. How dynamic is the vaginal microbiota and are BV-associated bacteria detected in women without BV at low concentrations? We sought to address these questions by evaluating key vaginal bacterial levels from samples collected longitudinally from healthy women and women with BV using a panel of taxon-specific bacterial qPCR assays.
Materials and Methods
Study population, clinical evaluation and sample collection
Thirty-three subjects were recruited for this longitudinal study from the Public Health - Seattle and King County Sexually Transmitted Diseases Clinic (STD clinic) between September 2006 and May 2009. The study was approved by the Institutional Review Board at the Fred Hutchinson Cancer Research Center. Written informed consent was obtained from all study participants. Participants were evaluated in clinic on Day 0 (recruitment), and returned to clinic for examination at 1 month (25–49 days; Median = 28). All participants were asked to self-collect vaginal swabs daily for 7 or 14 days, then at 2 weeks and 3 weeks. Self-collected swabs were mailed in on the day of collection at room temperature and held at −80°C before processing. In twelve additional participants, swabs were also collected at 2, 3 and 4 months after study entry. If participants were diagnosed with BV at 4 months, they were offered to re-enroll in the study, facilitating the observation of women with recurrent BV.
At clinic visits, participants were interviewed regarding medical history and sexual behaviors, and underwent a standard physical examination including a pelvic exam with speculum for collection of samples. At the enrollment visit, swabs of vaginal fluid samples were collected for Gram staining, pH, saline microscopy and KOH preparation. Samples for DNA extraction and PCR were obtained using polyurethane foam swabs (Epicenter Biotechnologies, Madison, WI) that were brushed against the lateral vaginal wall, re-sheathed and frozen immediately at −20°C and subsequently held at −80°C. At clinic visits, BV was diagnosed using Amsel's clinical criteria [10] and vaginal fluid smears were collected for Gram stains by the Nugent method [11] to confirm the presence of BV. Subjects with BV, diagnosed using Amsel's clinical criteria, were treated with 5 g 0.75% intravaginal metronidazole gel used each night for 5 days. Testing for STDs and other vaginal infections was performed as previously described [9]. A daily diary was maintained by the participants where they recorded menstruation, medication use and symptoms.
DNA extraction and quality control
DNA was extracted using the Ultra Clean Soil DNA Kit (Mobio, Carlsbad, CA) [12], eluted in 150 µl buffer and diluted 1∶1 in 1 mM Tris, 0.1 mM EDTA buffer. Two µl of the diluted DNA was used in each qPCR assay. Sham digests from swabs without human contact assessed contamination from reagents or collection swabs. Human 18S rRNA gene qPCR measured human DNA levels verifying that the swab contacted a human tissue surface and documenting successful extraction [13]. All DNA samples were tested for PCR inhibition using a sensitive qPCR approach targeting a segment of exogenously added jellyfish DNA at a concentration suitable for detection of low levels of inhibitors [13]. Inhibition was defined as a delay in the threshold cycle by ≥2 cycles compared to the no-DNA-template controls.
Quantitative PCR
Eleven qPCR assays targeting key vaginal bacteria associated with health or BV were applied to the samples. Assays for the detection of Gardnerella vaginalis, Lactobacillus crispatus, Megasphaera-like bacterium (type 1 & type 2), Atopobium vaginae, Leptotrichia and Sneathia species (single assay) and three Clostridiales Order bacteria designated as bacterial vaginosis associated bacterium 1 (BVAB1), BVAB2 and BVAB3 were applied as described previously [9]. We developed three additional assays targeting Lactobacillus jensenii, Lactobacillus iners, and a combined assay for Mobiluncus curtisii and Mobiluncus mulieris using a probe-based assay format [9] with 16S rRNA gene-specific primers, and a taxon-directed hydrolysis probe. Core reagents were from Applied Biosystems (Carlsbad, CA) and master mixes contained buffer A (1 mM), deoxynucleotide triphosphates (1 mM), magnesium (3 mM), AmpErase uracil-N-glycosylase (0.05 U) and AmpliTaq Gold polymerase (1–1.5 U) per reaction. Primers were added at 0.8 µM per reaction (Mobiluncus assay-1.2 µM forward primer) and final probe concentration was 150 µM. Assays underwent 45 cycles of amplification on the Eppendorf Mastercycler realplex Thermal cycler (Hamburg, Germany). Specificity and sensitivity were defined as described previously [9]. Plasmid standards were run in duplicate from 106 to 2.5 copies, and values are reported as 16S rRNA gene copies/swab. Assay details are provided in Table 1.
Table 1. Primer and probe sequences used in the quantitative PCR assays developed in this study.
| PCR Assay | PCR Conditions | Amplicon Size | Primer/Probe | Primer/Probe Sequence |
| Mobiluncus spp. | 60°C annealing, 39 s | 219 bp | 805F_Mob | 5′-CCACGCTGTAAACGTTGGGAA-3′ |
| 72°C extension, 30 s | 1023R_Mob_curt | 5′-TGGCCCATCTCTGGAACCA-3′ | ||
| 1024R_Mob_mul | 5′-CCACACCATCTCTGGCATG-3′ | |||
| Mob_838-861 | 5′-FAM-ATGCTATCCTGTGTTTCTGCGCCGTAG-TAMRA-3′ | |||
| Lactobacillus iners | 55°C annealing, 39 s | 76 bp | 165F_Liners | 5′-GATGCTAATACCGGATAAYAACAGAT-3′ |
| 72°C extension, 30 s | 241R_Liners | 5′-CACCGCAGGTCCATCCAAGA-3′ | ||
| Liners_186-213 | 5′-FAM-TGCCTATCAACTGTTTAAAAGATGGTTCT-TAMRA-3′ | |||
| Lactobacillus jensenii | 61°C annealing, 30 s | 69 bp | 988_Ljens | 5′-GTCTTGACATCCTTTGACCAC-3′ |
| 72°C extension, 30 s | 1057R_Ljens | 5′-CATGCACCACCTGTCTCTTT-3′ | ||
| Ljens_1009-1028 | 5′-FAM-CTAAGAGATTAGGTTTTCCC-MGBNFQ-3′ |
Statistics
To determine differences in DNA recovery in clinic-collected versus self-collected swabs, we used the Wilcoxon signed rank test to compare paired medians of the quantities of human 18S rRNA gene copies, G. vaginalis, L. jensenii and L. crispatus from 14 women without BV, obtained within one day of each other. To examine apparent patterns in levels of bacteria relative to menstruation, mean differences in log10 quantities of bacteria during menstruation were estimated using a linear mixed model, adjusting for treatment and with subjects as random effects to account for correlation in repeated measurements on each subject. Bacterial levels, when not detected, were considered to be half the detection limit.
Results
Subject characteristics
Of the 33 participants enrolled in the study, 22 collected at least 10 swabs and were included in the study analysis. Eight participants were diagnosed with BV by Amsel's clinical criteria at their initial visit, and 14 participants were not diagnosed with BV. Subject characteristics are noted in Table 2. A total of 355 swabs were processed, including 192 swabs from healthy women and 163 swabs from women with BV.
Table 2. Demographic data of the women enrolled in the longitudinal study.
| Participant characteristic | |
| Mean Age | 31.3 |
| Age Range | 22–42 |
| Median Age | 30.5 |
| 1 N (%) | |
| Race | |
| White | 13 (59.1%) |
| African American2 | 5 (22.7%) |
| Asian | 2 (9.1%) |
| Did not answer | 2 (9.1%) |
| Douching during the sampling period3 | 1 (4.2%) |
| Other vaginal medication3 | 3 (12.5%) |
| Vaginal product (not medication)3 | 5 (20.8%) |
| Sexual activity3 | 18 (75%) |
N indicates number of participants.
Four of five participants reported another race.
Data missing for 2 participants, hence the number of women included in the calculation is 20, corresponding with 24 menstrual cycles captured. The denominator used for the calculations is 24.
Comparison of self-collected and clinic-collected swabs
There was no significant difference in paired median levels of human 18S rRNA gene copies, G. vaginalis or L. jensenii levels (p>0.05) between clinic- and home-collected swabs. Median levels of L. crispatus were higher in the clinic obtained swabs (p = 0.02). These data suggest that human and bacterial DNA levels were largely similar in clinic- and home-collected swabs.
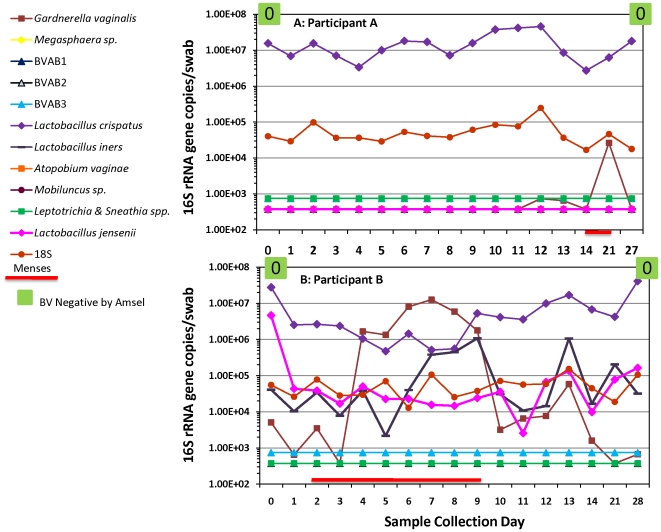
Variability in vaginal bacterial levels in women without BV
Taxon-directed bacterial qPCR assays demonstrated that healthy women were colonized with lactobacilli and typically did not harbor BV-associated bacteria with the exception of G. vaginalis. However, daily changes in bacterial concentrations were common. Quantities of human 18S rRNA gene copies by qPCR were relatively constant showing consistent loading of human cells on the swabs with good stability of DNA and fluctuations in DNA levels were not due to sample quality (Figure 1). An example of a relatively stable vaginal microbiota is provided in Figure 1A, where participant A is negative for BV at study entry. The participant was colonized with L. crispatus and quantities remained relatively stable throughout the period sampled. An increase of >1-log G. vaginalis is observed at 3 weeks during menses. In contrast, as demonstrated in Figure 1B, concentrations of Lactobacillus species can fluctuate in participants without BV. A 4-log increase in G. vaginalis levels was observed along with an increase in L. iners coincident with menses, and quantities decreased without intervention at the end of menstruation.
Figure 1. Variability of vaginal bacteria in women without BV.
The line graphs show the changes in vaginal bacteria measured as 16S rRNA gene copies per swab in a participant exhibiting a stable bacterial biota (A) and another with dynamic patterns (B). The red line indicates menses. Clinical diagnosis was performed using Amsel's criteria (green box in upper graph indicating negative for BV). Gram staining using the Nugent criteria (the score is indicated as a number from 0–10 in the box) was also performed. A score of 0–3 indicates negative for BV, 4–6 reflects intermediate BV flora and 7–10 denotes positive for BV. Levels of the human 18S rRNA gene (red circles) were used to assess the amount of vaginal fluid loaded on each swab as reflected by human cell content. BVAB denotes bacterial vaginosis associated bacterium.
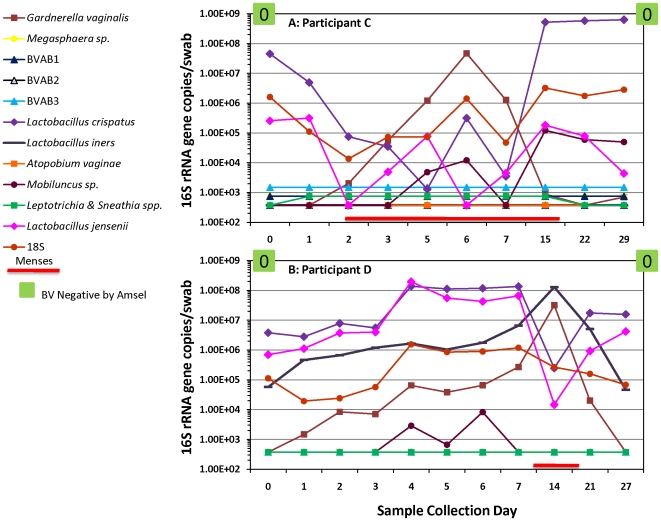
Variability of Gardnerella vaginalis during menses
An increase in G. vaginalis levels associated with menses, accompanied by decreased quantities of L. jensenii and L. crispatus were observed (Figures 1 & 2). At the end of menstruation, G. vaginalis quantities decreased to below detection limits (Figures 1 & 2) and L. iners concentrations declined as well (Figures 1B & 2B); simultaneous increases in quantities of L. crispatus and L. jensenii were observed. On average, quantities of L. crispatus were found to be lower during menstruation by 0.6 logs (p = 0.001) while G. vaginalis quantities were found to be higher by 1.38 logs after adjusting for sampling during treatment (Table 3). Quantities of L. jensenii and L. crispatus were both found to be inversely related to G. vaginalis; L. jensenii was lower by 0.19 logs per log10 increase in G. vaginalis (p<0.001) and L. crispatus by 0.17 logs (p<0.001).
Figure 2. Variability of Gardnerella vaginalis during menses.
The line graphs show increases in G. vaginalis levels during menses while concentrations of L. crispatus and L. jensenii decreased. G. vaginalis quantities declined below detection thresholds post-menses with simultaneous increases in L. jensenii and L. crispatus levels. Participant C (Figure 2A) was not colonized with L. iners while Participant D (Figure 2B) was. Levels of L. iners were observed to increase with G. vaginalis concentrations and subsequently declined post-menses. Both participants were negative for BV by Amsel's criteria (green boxes) and had Nugent scores of 0 at the entry and follow up visits.
Table 3. Differences in levels of bacteria by qPCR during menstruation.
| Bacterium | mean log10 adjusted difference (95% CI), p-value* during menstruation |
| Lactobacillus crispatus | −0.60 (−0.94, −0.25), p = 0.001 |
| Lactobacillus jensenii | −0.39 (−0.79, 0.01), p = 0.06 |
| Lactobacillus iners | 0.10 (−0.23, 0.43), p = 0.56 |
| Gardnerella vaginalis | 1.38 (0.83, 1.93), p<0.001 |
Data shown for 16 subjects who reported days with and without menses during the study period.
Mean log10 adjusted change, p-values, and 95% CIs (confidence intervals) estimated using a linear mixed model with participants as random effects and adjusted for treatment. We tested those patterns that appeared interesting upon examination of the data; thus, these p-values and 95% CIs arise from exploratory analyses and serve as a basis for future hypothesis-driven research.
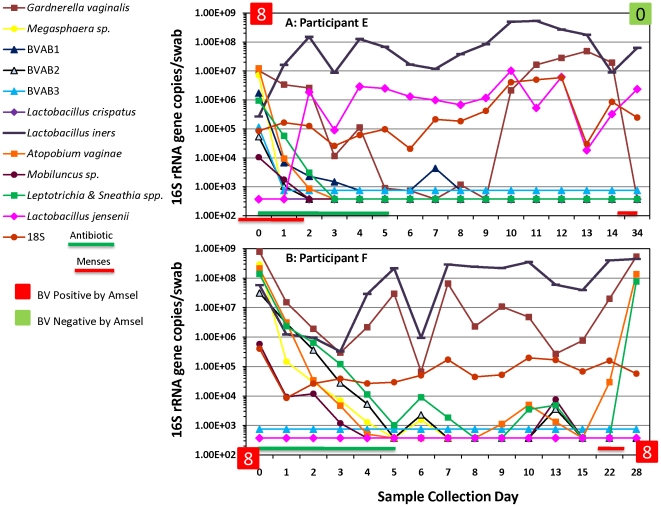
Eradication of BV-associated bacteria post antibiotic treatment
With the exception of G. vaginalis, quantities of BV-associated bacteria decreased several logs and dropped below detection thresholds between Days 1 and 5 (Median = 3.5 days) of metronidazole treatment (Figure 3) in women with BV. We show data from two representative subjects.
Figure 3. Eradication of BV bacteria post-antibiotic treatment.
Participant E (Figure 3A) and Participant F (Figure 3B) are two women with BV by Amsel criteria (red boxes) and by Nugent criteria (Score = 8) at study entry. There was a difference in the rate of decrease of BV bacteria post-metronidazole therapy. Participant E was cured of BV at the 1 month visit as determined by Amsel's (green box) and Nugent's (Score = 0) criteria. Participant F was re-colonized with A. vaginae, Leptotrichia & Sneathia spp. and G. vaginalis; BV was diagnosed at that time. The green line at the bottom of the graph shows days of metronidazole treatment and the red line denotes menses.
Participant E had high levels of BV-associated bacteria at diagnosis which declined below detection thresholds (except G. vaginalis), while concentrations of L. jensenii increased 3.5-logs. High concentrations of L. iners were observed throughout the period sampled.
In contrast, the rate of decrease of BV-associated bacteria in Participant F was slower. Participant F maintained moderate to high G. vaginalis levels throughout the period sampled. There were transient increases in concentrations of some BV-associated bacteria after eradication on Day 5, but they resolved by Day 15. However, an elevation of G. vaginalis, A. vaginae and Leptotrichia/Sneathia spp. quantities were observed during menses. Participant F was subsequently diagnosed with BV at her 1-month clinic visit. Participant F was never colonized with L. crispatus or L. jensenii throughout the period sampled.
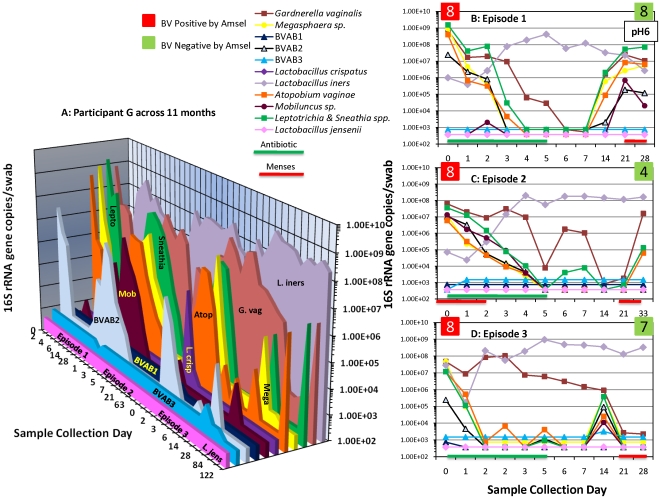
Variability of bacteria in women with recurrent BV
Three women (37.5%) in this study had at least ≥2 episodes of BV. Figure 4 shows recurrent BV in a representative participant with three episodes of BV. Participant G harbored several BV-associated bacteria and had a clinical diagnosis of BV at study entry (Episode 1, Figure 4B). With treatment, quantities of BV-associated bacteria declined below detection thresholds (except G. vaginalis). Subsequently, levels of BV-associated bacteria trended upwards reaching maximal levels during menses. At the 1-month clinic visit, Participant G was negative for BV by Amsel's criteria (pH 6, <20% clue cells, negative whiff test, normal discharge) and was not treated. Participant G returned to clinic 3 months later and was diagnosed with BV (Episode 2, Figure 4C). With metronidazole treatment, levels of BV-associated bacteria declined below detection thresholds and the participant was clinically BV negative at 1 month. However, she returned again in 3 months and was diagnosed with the third episode of BV (Episode 3, Figure 4D). With her third course of metronidazole, participant G had a similar response as previously observed, wherein there was initial decline of BV-associated bacteria and the participant was clinically negative for BV at 1 month. However, two months later quantities of G. vaginalis, Leptotrichia/Sneathia spp. and A. vaginae increased but she did not return to clinic for further examination. In all three episodes studied, L. iners had an inverse relationship with the BV-associated bacteria. Participant G was never colonized with L. jensenii and was briefly colonized with L. crispatus through the sampling period.
Figure 4. Bacterial fluctuations in a participant with recurrent BV.
Figure 4A depicts dynamic patterns of BV bacteria in Participant G across a period spanning 11 months. She was diagnosed with BV by Amsel's and Nugent's criteria at entry (Episode 1, 4B), and was responsive initially to treatment. However, she had two more episodes subsequently (4C and 4D) and each time she responded to metronidazole treatment but had a return of BV-associated bacteria and went on to develop BV.
Discussion
In our study of frequent sampling of the vaginal microbiota, we found that the bacterial community is dynamic and changes rapidly. We sought to study changes in the levels of bacteria in the human vagina and assess their relationship with the common condition, bacterial vaginosis. Our first goal was to determine how stable the microbial community is in healthy women. As noted in previous cultivation-based studies, healthy women tended to be colonized with several Lactobacillus species, though G. vaginalis was also frequently detected, including in 70% of women without BV using PCR methods [12]. G. vaginalis concentrations increased substantially with menses in 81% of monitored menstrual cycles, and levels decreased with the end of menstruation. During these surges of G. vaginalis, L. iners levels also trended upwards while levels of the other two lactobacilli decreased. Schwebke et al. [14] have similarly reported increases in Gardnerella/Bacteroides morphotypes by Gram stain and reduced quantities of lactobacilli during menses. Our study enhances the observations made by these authors by measuring levels of specific bacterial species and provides the ability to distinguish among Lactobacillus species. In our study, all subjects (n = 14) classified as negative for BV by the Amsel diagnostic criteria on Day 0 had at least a low level of G. vaginalis on one of the days sampled. A longitudinal cultivation study reported the isolation of G. vaginalis in at least one time point in the menstrual cycle in all subjects, though the number of subjects examined was small (n = 7) [15]. These findings raise the question of the role of the normal fluctuations of G. vaginalis in the development of abnormal flora associated with BV.
The growth of G. vaginalis may be tied to the availability of iron. Iron is an essential growth factor for most bacteria and the acquisition of iron enhances the replication of many pathogens [16], [17], [18]. There is limited free iron in the human body as much of it is sequestered in compounds such as hemoglobin, the iron-containing metalloprotein in erythrocytes, and lactoferrin, present in mucosal tissues. One mechanism for acquiring iron is to lyse host cells such as erythrocytes with a cytolysin thereby liberating intracellular iron stores. G. vaginalis produces a toxin, vaginolysin, a member of the cholesterol-dependent cytolysin family of toxins [19], [20]. Experiments examining the growth of G. vaginalis have shown that this bacterium cannot grow in iron-limiting conditions, but can use iron sources such as hemoglobin for growth and can produce siderophores suggesting a well adapted ability to harvest iron from the environment [21]. Our observation that surges in G. vaginalis coincide with menses (and therefore vaginal blood) is consistent with this hypothesis. As to the role of G. vaginalis in BV, we hypothesize that G. vaginalis may function as a facilitator to enhance acquisition of other BV-associated bacteria that are also characteristic of this condition.
In healthy women, concentrations of L. iners, when present, tended to increase along with levels of G. vaginalis during menses (Figures 1 & 2). It is noteworthy that both G. vaginalis and L. iners are easily cultivated on blood agar medium. As noted with Participant G on multiple occasions, concentrations of L. iners tended to increase with antibiotic treatment for BV, suggesting that this bacterium may fill the niche vacated by the loss of BV-associated bacteria.
Our second goal was to determine if BV-associated bacteria were eradicated with antibiotic treatment in women with recurrent BV, and to assess the time to eradication. We found that quantities of BV-associated bacteria decreased rapidly with intravaginal metronidazole, evidencing multi-log declines on a daily basis, though the slope of this decline varied (Figures 3 & 4). This observation supports the hypothesis that recurrent BV is not a result of initial antibiotic failure, but rather is associated with the reappearance of BV-associated bacteria after completion of antibiotic therapy. We are able to detect as few as 2.5 gene copies per qPCR reaction translating to 375 16S rRNA copies per swab. Hence, if the bacteria were present below these concentrations, we could not have detected them. Understanding how women with recurrent BV reacquire the BV bacteria is critical for prevention efforts.
This study has some limitations. First, there were a small number of subjects in this study. Longitudinal studies collecting many samples require highly motivated participants. Some investigators have taken the approach of processing limited numbers of samples from many women [9], [22], [23], [24], [25]. Our approach was to process large numbers of samples from a relatively small number of women in order to better explore vaginal bacterial dynamics. Second, we applied 11 bacterial assays; but this does not represent all bacterial taxa associated with the vagina. Complementary molecular technologies such as broad-range PCR, cloning and sequencing, or pyrosequencing may help overcome this limitation, though these approaches are not quantitative. Third, although daily qPCR data were obtained from the subjects, this was not correlated with daily clinical data such as exams since the swabs were mostly self-collected. Fourth, all subjects were from a single clinic and may not be broadly representative of reproductive age women with and without BV. Fifth, patterns of bacterial fluctuations were statistically examined in retrospect; hence p-values and 95% CIs arise from exploratory analyses and serve as a basis for future hypothesis-driven research.
In conclusion, the vagina is a dynamic microbial ecosystem supporting a changing and diverse bacterial population, both in healthy women and women with BV. Lactobacilli predominantly occur in healthy women, although their Lactobacillus species profiles vary. Subjects with BV have many fastidious BV-associated bacteria that respond well to the 5-day metronidazole treatment regimen, suggesting that these bacteria are susceptible to metronidazole or are dependent on other bacteria that are eradicated with antibiotic treatment. Recurrence of BV is associated with reappearance of BV-associated bacteria suggesting re-infection or resurgence from an endogenous reservoir. The rate of decrease of the BV bacteria with antibiotic treatment varies, suggesting that longer antibiotic treatments may be warranted in some women.
Acknowledgments
We are grateful to Dwyn Dithmer and Kathleen Ringwood for their clinical contributions and data management efforts.
Footnotes
Competing Interests: D. N. Fredricks and T. L. Fiedler have developed intellectual property related to the use of PCR for the diagnosis of BV. Refer to US patent 7625704 on use of PCR for diagnosis of BV. No products to report. This does not alter the authors' adherence to all the PLoS ONE policies on sharing data and materials.
Funding: This project was funded with a grant (R01 AI061628) to Dr. Fredricks from the National Institute of Allergy and Infectious Diseases (NIAID) (www3.niaid.nih.gov), division of National Institutes of Health (NIH). Dr. Mitchell received salary support from a Women's Reproductive Health grant (HD-01-264) from the National Institute of Child Health and Human Development (NICHD) (www.nichd.nih.gov), division of the NIH. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Koumans EH, Sternberg M, Bruce C, McQuillan G, Kendrick J, et al. The prevalence of bacterial vaginosis in the United States, 2001–2004; associations with symptoms, sexual behaviors, and reproductive health. Sex Transm Dis. 2007;34:864–869. doi: 10.1097/OLQ.0b013e318074e565. [DOI] [PubMed] [Google Scholar]
- 2.Hillier SL, Nugent RP, Eschenbach DA, Krohn MA, Gibbs RS, et al. Association between bacterial vaginosis and preterm delivery of a low-birth-weight infant. The Vaginal Infections and Prematurity Study Group. N Engl J Med. 1995;333:1737–1742. doi: 10.1056/NEJM199512283332604. [DOI] [PubMed] [Google Scholar]
- 3.Taha TE, Hoover DR, Dallabetta GA, Kumwenda NI, Mtimavalye LA, et al. Bacterial vaginosis and disturbances of vaginal flora: association with increased acquisition of HIV. AIDS. 1998;12:1699–1706. doi: 10.1097/00002030-199813000-00019. [DOI] [PubMed] [Google Scholar]
- 4.Haggerty CL, Hillier SL, Bass DC, Ness RB. Bacterial vaginosis and anaerobic bacteria are associated with endometritis. Clin Infec Dis. 2004;39:990–995. doi: 10.1086/423963. [DOI] [PubMed] [Google Scholar]
- 5.Hillier S, Marrazzo JM, Holmes KK. Bacterial vaginosis. In: Holmes KK, Sparling P-A, editors. Sexually Transmitted Diseases. New York: McGraw-Hill; 2008. pp. 737–768. [Google Scholar]
- 6.Kalra A, Palcu CT, Sobel JD, Akins RA. Bacterial vaginosis: culture- and PCR-based characterizations of a complex polymicrobial disease's pathobiology. Curr Infect Dis Rep. 2007;9:485–500. doi: 10.1007/s11908-007-0074-4. [DOI] [PubMed] [Google Scholar]
- 7.Srinivasan S, Fredricks DN. The human vaginal bacterial biota and bacterial vaginosis. Interdiscip Perspect Infect Dis. 2008;2008:750479. doi: 10.1155/2008/750479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bradshaw CS, Morton AN, Hocking J, Garland SM, Morris MB, et al. High recurrence rates of bacterial vaginosis over the course of 12 months after oral metronidazole therapy and factors associated with recurrence. J Infect Dis. 2006;193:1478–1486. doi: 10.1086/503780. [DOI] [PubMed] [Google Scholar]
- 9.Fredricks DN, Fiedler TL, Thomas KK, Mitchell CM, Marrazzo JM. Changes in vaginal bacterial concentrations with intravaginal metronidazole therapy for bacterial vaginosis as assessed by quantitative PCR. J Clin Microbiol. 2009;47:721–726. doi: 10.1128/JCM.01384-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Amsel R TP, Spiegel CA, Chen KC, Eschenbach D, Holmes KK. Nonspecific vaginitis: diagnostic criteria and microbial and epidemiologic associations. Am J Med. 1983;74:14–22. doi: 10.1016/0002-9343(83)91112-9. [DOI] [PubMed] [Google Scholar]
- 11.Nugent RP, Krohn MA, Hillier SL. Reliability of diagnosing bacterial vaginosis is improved by a standardized method of Gram stain interpretation. J Clin Microbiol. 1991;29:297–301. doi: 10.1128/jcm.29.2.297-301.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fredricks DN, Fiedler TL, Thomas KK, Oakley BB, Marrazzo JM. Targeted PCR for detection of vaginal bacteria associated with bacterial vaginosis. J Clin Microbiol. 2007;45:3270–3276. doi: 10.1128/JCM.01272-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Khot PD, Ko DL, Hackman RC, Fredricks DN. Development and optimization of quantitative PCR for the diagnosis of invasive aspergillosis with bronchoalveolar lavage fluid. BMC Infect Dis. 2008;8:73. doi: 10.1186/1471-2334-8-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schwebke JR, Morgan SC, Weiss HL. The use of sequential self-obtained vaginal smears for detecting changes in the vaginal flora. Sex Transm Dis. 1997;24:236–239. doi: 10.1097/00007435-199704000-00009. [DOI] [PubMed] [Google Scholar]
- 15.Sautter RL, Brown WJ. Sequential vaginal cultures from normal young women. J Clin Microbiol. 1980;11:479–484. doi: 10.1128/jcm.11.5.479-484.1980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Litwin CM, Calderwood SB. Role of iron in regulation of virulence genes. Clin Microbiol Rev. 1993;6:137–149. doi: 10.1128/cmr.6.2.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Miethke M, Marahiel MA. Siderophore-based iron acquisition and pathogen control. Microbiol Mol Biol Rev. 2007;71:413–451. doi: 10.1128/MMBR.00012-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Weinberg ED. Iron availability and infection. Biochim Biophys Acta. 2009;1790:600–605. doi: 10.1016/j.bbagen.2008.07.002. [DOI] [PubMed] [Google Scholar]
- 19.Gelber SE, Aguilar JL, Lewis KL, Ratner AJ. Functional and phylogenetic characterization of Vaginolysin, the human-specific cytolysin from Gardnerella vaginalis. J Bacteriol. 2008;190:3896–3903. doi: 10.1128/JB.01965-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Randis TM, Kulkarni R, Aguilar JL, Ratner AJ. Antibody-based detection and inhibition of vaginolysin, the Gardnerella vaginalis cytolysin. PLoS One. 2009;4:e5207. doi: 10.1371/journal.pone.0005207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jarosik GP, Land CB, Duhon P, Chandler R, Jr, Mercer T. Acquisition of iron by Gardnerella vaginalis. Infect Immun. 1998;66:5041–5047. doi: 10.1128/iai.66.10.5041-5047.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.De Backer E, Verhelst R, Verstraelen H, Alqumber MA, Burton JP, et al. Quantitative determination by real-time PCR of four vaginal Lactobacillus species, Gardnerella vaginalis and Atopobium vaginae indicates an inverse relationship between L. gasseri and L. iners. BMC Microbiol. 2007;7:115. doi: 10.1186/1471-2180-7-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Menard JP, Fenollar F, Henry M, Bretelle F, Raoult D. Molecular quantification of Gardnerella vaginalis and Atopobium vaginae loads to predict bacterial vaginosis. Clin Infect Dis. 2008;47:33–43. doi: 10.1086/588661. [DOI] [PubMed] [Google Scholar]
- 24.Mitchell CM, Hitti JE, Agnew KJ, Fredricks DN. Comparison of oral and vaginal metronidazole for treatment of bacterial vaginosis in pregnancy: impact on fastidious bacteria. BMC Infect Dis. 2009;9:89. doi: 10.1186/1471-2334-9-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zozaya-Hinchliffe M, Martin DH, Ferris MJ. Prevalence and abundance of uncultivated Megasphaera-like bacteria in the human vaginal environment. Appl Environ Microbiol. 2008;74:1656–1659. doi: 10.1128/AEM.02127-07. [DOI] [PMC free article] [PubMed] [Google Scholar]