Abstract
Objective
To evaluate 17-alpha hydroxyprogesterone caproate (17P) for prevention of preterm birth (PTB) in women with prior spontaneous PTB (SPTB) and cervical length (CL) <25mm.
Study Design
Planned secondary analysis of the NICHD-sponsored randomized trial evaluating cerclage for women with singleton gestations, prior SPTB (17-33 6/7weeks), and CL<25mm between 16-22 6/7weeks. Women were stratified at randomization to intent to use or not use 17P. The effect of 17P was analyzed separately for cerclage and no cerclage groups. Primary outcome was PTB<35weeks.
Results
In 300 women, 17P had no effect on PTB<35weeks in either cerclage (p=0.64) or no cerclage (p=0.51) groups. Only PTB<24weeks (OR=0.08) and perinatal death (OR=0.14) were significantly lower for those with 17P in the no cerclage group.
Conclusions
17P had no additional benefit for prevention of PTB in women who have prior spontaneous PTB and get ultrasound-indicated cerclage for CL<25mm. In women who do not get cerclage, 17P reduced previable birth and perinatal mortality.
Keywords: progesterone, short cervical length, cerclage, preterm birth
Background and Objective
A short cervical length (CL) on second trimester transvaginal ultrasound (TVU) is currently the best method to predict spontaneous preterm birth (SPTB). (1) Prior SPTB is perhaps the strongest historic risk factor for recurrent SPTB (2). Cerclage (3-8) and progesterone (9,10) supplementation have been the two interventions proposed most often to prevent PTB once the short TVU CL has been detected or in women with prior SPTB.
It has now been shown in a large randomized trial that cerclage reduces the incidence of recurrent PTB <24 and <37 weeks, as well as perinatal mortality, in women with both a prior spontaneous PTB 17-33 6/7 weeks and also a short CL < 25 mm, identified between 16-22 6/7 weeks (3). This confirmed results from a meta-analysis (8) of prior trials (4-7). In one trial (9) and one systematic review and meta-analysis (10), 17 alpha-hydroxyprogesterone caproate (17P) has been associated with a reduction of recurrent SPTB. It is unclear if the effects of 17P (for prior SPTB) and cerclage (for short CL) are additive in women with both risk factors. Moreover, it is unclear if 17P is beneficial in women with a prior PTB and a short CL who do not undergo ultrasound-indicated cerclage.
Our objective was to estimate the effect of 17P for the prevention of PTB in women with prior SPTB, and a short CL, with and without ultrasound-indicated cerclage.
Materials and Methods
This is a planned secondary analysis of the NICHD-sponsored randomized trial evaluating cerclage for women with singleton gestations, prior SPTB (17-33 6/7 wks), and short CL < 25 mm measured between 16 and 22 6/7 weeks. This randomized controlled trial was performed by 15 U.S. Clinical Centers between January, 2003 and November, 2007. (3) Each center obtained Institutional Review Board approval. Exclusion criteria were fetal anomaly, planned history-indicated cerclage, and clinically significant maternal-fetal complications (3). Gestational age was always confirmed by standard sonographic biometric measurements at less than 20 weeks’ gestation. Sonologists underwent a uniform certification process by a single investigator (J.O.) to ensure uniformity in sonographic measurements of TVU CL screening. (3,11).
Women with prior SPTB were screened with TVU CL starting at 16 0/7 – 21 6/7 weeks, then every 2 weeks until 22 6/7 weeks unless the CL was observed to be 25-29 mm, after which the scan frequency was increased to every week. Women who were detected by TVU screening to have a short CL <25mm at 16-22 6/7 weeks were randomized after informed consent to cerclage or no cerclage.
Very early in the trial (May, 2003), after the first 10 women were randomized, the results of a randomized trial of 17P became available (9). In response to this report the steering committee and an independent data and safety monitoring board recommended that women eligible for the cerclage trial be counseled regarding the use of progesterone for preterm birth prevention, and an additional randomization stratum, reflecting the patient’s stated intent to use progesterone, was added. The suggested 17P dose was 250mg IM starting at 16 weeks and continued weekly until 36 weeks. Subsequent use of 17P was recorded and actual use was utilized for these analyses.
Study nurses contacted patients weekly to record medication use. To determine if the reported use on the study data forms reflected actual use of 17P, medical records were reviewed for study patients at the center with the largest number of recruited study patients. Of the 23 patients at this center with a reported dose, 20 (91%) received at least one recorded dose of 17P. There was 85% agreement between the reported 17P and the administered 17P (kappa=0.85). Therefore we concluded that the reported 17P on the study data forms was an accurate reflection of actual 17P use. We then defined actual use of 17P for our analyses as at least one reported dose on the study data forms.
The effect of 17P use was analyzed separately for the cerclage and no cerclage groups. Randomization to cerclage/no-cerclage (intent to treat) was used in the primary analysis. (3) We also planned to analyze data by actual cerclage/no-cerclage placement groups. In this latter analysis, women were allocated to the cerclage group if they actually received a cerclage, and to the ‘no cerclage’ group if they did not receive cerclage.
The primary outcome of this secondary analysis as well as that of the primary analysis (3) was PTB < 35 weeks. Secondary outcomes included birth < 7 days from randomization, PTB < 24, < 28, < 32, and < 37 weeks, and perinatal death. Perinatal death was defined as either a stillbirth or a post natal death prior to hospital discharge. Maternal age, race, smoking, drug use, shortest CL, gestational age of the qualifying preterm birth, prior induced abortion, number of sonograms, and gestational age at randomization were considered as possible confounders.
The primary study outcome and other categorical variables were compared with chi-square tests and, where appropriate, Fisher’s exact test. Continuous variables were analyzed using the t-test and Wilcoxon rank-sum test where appropriate. Differences in time to birth were assessed with Kaplan-Meier curves and the log-rank test. Multivariable logistic regression and Cox proportional hazard models considered possible confounders for the outcomes of preterm birth < 35 weeks and time to birth respectively. We selected an alpha level of < 0.05 to represent statistical significance.
Results
Of 1014 women with prior SPTB who were screened with TVU CL at 16-22 6/7 weeks, 318 had a CL <25mm, of which 302 agreed to randomization. Of these, 300 were available for this analysis, because one woman was lost to follow up and one woman was excluded because she received vaginal progesterone, not 17P. Of these 300, 148 were randomized to cerclage and 152 were randomized to no-cerclage.
Of the 148 women with a prior SPTB, a short CL<25mm, and who were randomized to receive cerclage, characteristics were similar except for race/ethnicity (p < 0.01), smoking (p = 0.036), and total number of vaginal sonograms (p = 0.03) between the 47 women who used progesterone, and the 101 who did not use 17P (table 1). 17P had no effect on PTB < 35 weeks (p=0.64), or on other outcomes (table 2).
Table 1.
Baseline characteristics by actual progesterone use for 148 women with prior SPTB, short CL <25mm at 16-22 6/7weeks, and randomized to cerclage placement.
| 17P (n = 47) |
No 17P (n = 101) |
P value | |
|---|---|---|---|
| Maternal age (y) | 26.9 (6.3) | 26.1 (5.1) | 0.38 |
| Race/ethnicity* Black (non-Hispanic) White (non-Hispanic) Hispanic Other |
26 (55) 13 (28) 2 (4.3) 6 (13) |
54 (53) 12 (12) 25 (25) 10 (10) |
<0.01 |
| Cigarette use | 12 (26) | 12 (12) | 0.036 |
| Any drug abuse | 3 (6) | 2 (2) | 0.33** |
| One or more prior induced abortion | 7 (15) | 18 (18) | 0.66 |
| Years of education | 12.5 (2.1) | 11.8 (3.0) | 0.15 |
| Gestational age of qualifying birth (weeks) | 23.2 (4.8) | 24.7 (4.8) | 0.08 |
| Gestational age at randomization (weeks) | 18.9 (1.9) | 19.6 (1.9) | 0.054 |
| Cervical length at randomization (mm) | 19.0 (5.5) | 18.5 (6.6) | 0.64 |
| Total number of vaginal sonograms | 2 (1, 4)† | 2 (1, 4)† | 0.03 |
Data presented as mean± 1 SD, or n (%).
Race and ethnic group are self-reported
Fisher’s exact test
Median and interdecile range
Table 2.
Perinatal outcomes and actual progesterone use for 148 women randomized to cerclage.
| 17P (n = 47) |
No 17P (n = 101) |
P value |
OR (95% CI) | |
|---|---|---|---|---|
| Preterm birth < 35 weeks | 14 (30) | 34 (34) | 0.64 | 0.84 (0.40, 1.77) |
| Birth < 7 days from randomization | 0 (0) | 4 (4) | 0.31* | 0.23 (0.01, 4.32) |
| Previable birth < 24 weeks | 2 (4) | 7 (7) | 0.72* | 0.60 (0.12, 2.99) |
| Preterm birth < 28 weeks | 4 (9) | 17 (17) | 0.18 | 0.46 (0.16, 1.45) |
| Preterm birth < 32 weeks | 8 (17) | 25 (25) | 0.29 | 0.62 (0.26, 1.51) |
| Preterm birth < 37 weeks | 23 (49) | 43 (43) | 0.47 | 1.29 (0.65, 2.59) |
| Perinatal death | 3 (6) | 10 (10) | 0.76* | 0.62 (0.16, 2.37) |
Data presented as n (%).
Fisher’s exact test
Of the 152 women with a prior SPTB, a short CL<25mm, and who were randomized to not receive cerclage, significant disparities were found only for prior induced abortion (p = 0.003) and years of education (p = 0.001) between the 52 women who used, and the 100 did not use 17P (table 3). While 17P had no effect on PTB < 35 weeks (p=0.51), the odds of PTB <24 weeks (OR=0.08, p=0.0022) and perinatal death (OR=0.14, p=0.0029) were significantly lower for those with 17P in the no cerclage group (table 4).
Table 3.
Baseline characteristics by actual progesterone use for 152 women with prior SPTB, short CL <25mm at 16-22 6/7 weeks, randomized to no cerclage.
| 17P (n = 52) |
N0 17P (n = 100) |
P value | |
|---|---|---|---|
| Maternal age (y) | 26.3 (4.5) | 26.8 (5.3) | 0.56 |
| Race/ethnicity* Black (non-Hispanic) White (non-Hispanic) Hispanic Other |
32 (62) 13 (25) 4 (7.7) 3 (5.8) |
60 (60) 15 (15) 13 (13) 12 (12) |
0.25 |
| Cigarette use | 12 (23) | 17 (17) | 0.37 |
| Any drug abuse | 6 (11.5) | 4 (4) | 0.09** |
| One or more prior induced abortion | 15 (29) | 10 (10) | 0.0029 |
| Years of education | 12.8 (1.8) | 11.5 (2.6) | 0.0011 |
| Gestational age of qualifying birth (weeks) | 24.0 (5.0) | 24.7 (4.6) | 0.36 |
| Gestational at randomization (weeks) | 19.6 (2.0) | 19.4 (2.1) | 0.56 |
| Cervical length at randomization (mm) | 19.5 (5.0) | 19.4 (5.5) | 0.87 |
| Total number of vaginal sonograms | 3 (1, 4)† | 2 (1, 4)† | 0.21 |
Data presented as mean± 1 SD, or n (%).
Race and ethnic group are self-reported
Fisher’s exact test
Median and interdecile range
Table 4.
Perinatal outcomes by actual progesterone use for 152 women randomized to no cerclage.
| 17P (n = 52) |
No 17P (n = 100) |
P value |
OR (95% CI) | |
|---|---|---|---|---|
| Preterm birth < 35 weeks | 20 (39) | 44 (44) | 0.51 | 0.80 (0.40, 1.58) |
| Birth < 7 days from randomization | 0 (0) | 3 (3) | 0.55* | 0.27 (0.01, 5.23) |
| Previable birth < 24 weeks | 1 (2) | 20 (20) | 0.0022 | 0.08 (0.01, 0.60) |
| Preterm birth < 28 weeks | 8 (15) | 25 (25) | 0.17 | 0.55 (0.23, 1.31) |
| Preterm birth < 32 weeks | 11 (21) | 34 (34) | 0.10 | 0.52 (0.23, 1.14) |
| Preterm birth < 37 weeks | 31 (60) | 59 (59) | 0.94 | 1.03 (0.52, 2.03) |
| Perinatal death | 2 (4) | 23 (23) | 0.0029 | 0.14 (0.03, 0.61) |
Data presented as n (%).
Fisher’s exact test
In multivariable logistic regression models, the odds of PTB < 35 weeks were lower for increasing CL at randomization (OR = 0.91; 95% CI: 0.85 – 0.98; p = 0.012) for women randomized to cerclage. For women randomized to no-cerclage, the odds of PTB < 35 weeks were higher for black women (OR = 4.23; 95% CI: 1.31 - 13.62; p = 0.016) and lower for longer CL at randomization (OR = 0.39; 95% CI: 0.77 - 0.92; p < 0.0001). Similar results of shortest CL were seen in Cox models for time to delivery, where women randomized to cerclage (HR = 0.94; 95% CI: 0.90 – 0.97; p = 0.0003) and women randomized to no cerclage (HR = 0.97; 95% CI: 0.94 – 1.00; p = 0.077) were less likely to deliver for larger values of CL at randomization.
The shortest CL was a significant predictor in both the cerclage and no cerclage multiple logistic regression models for PTB < 35 weeks. Therefore, we considered the effect of 17P among those women with CL <15 mm at randomization versus those with CL 15-24 mm at randomization. (12, 13) Analyses of the interaction between CL sub-groups and 17P use were not significant for any outcome when stratified by cerclage randomization groups. However, after considering all randomized women and controlling for randomization group, we found that progesterone use did have a statistically significant effect on reducing the odds of both previable birth (OR = 0.11; 95% CI: 0.15 - 0.88; p = 0.0371) and perinatal death (OR = 0.18; 95% CI: 0.04 - 0.81; p = 0.026) for those women with CL 15-24 mm. These effects were not significant for the women with CL < 15 mm. In the Cox proportional hazards models stratified by randomization group there was no effect of 17P use on time to delivery for either group of women.
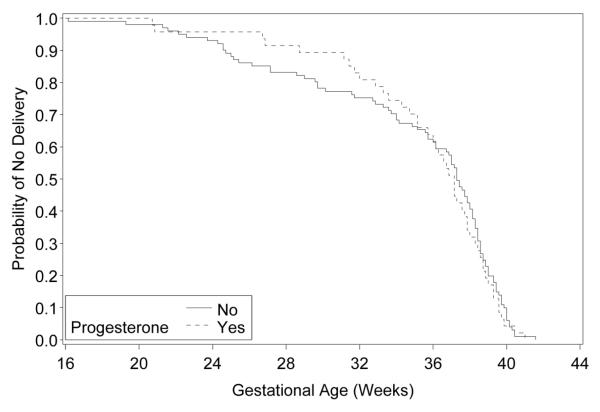
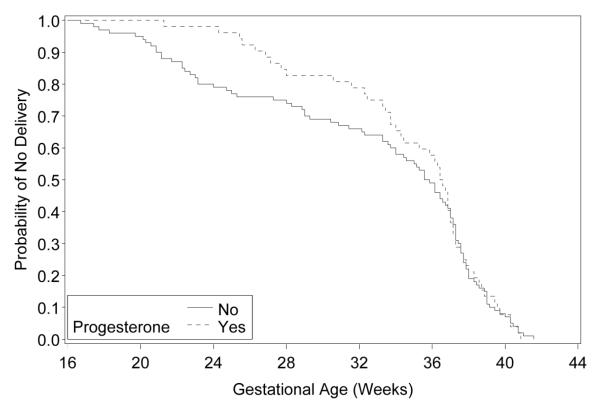
Differences in the time-to-delivery for women who did and did not use 17P were assessed with Kaplan-Meier curves. We again considered women assigned to cerclage (n=148) and to nocerclage (n=152) separately. We found no statistically significant difference in time-to-delivery between 17P use and non-use for any cerclage subpopulation. The significance levels are: randomized to cerclage, p=0.639 (figure 1); randomized to no-cerclage, p=0.694 (figure 2). Note that we did see a large separation between the 17P users and non-users at early gestational age for women assigned to no-cerclage and women who received cerclage. Notably, at 24 weeks the proportion of women yet to deliver is much higher for those taking progesterone than for those not taking progesterone in the no-cerclage group (figure 2).
Figure 1.
Time to delivery for women with and without progesterone use, randomized to cerclage (p=0.639).
Figure 2.
Time to delivery for women with and without progesterone use, randomized to no cerclage (p=0.694)
Of the 148 women assigned to receive cerclage, 10 did not undergo surgery. Of the 152 women assigned to the no-cerclage group, 14 received a post-randomization stitch. Thus, 152 women actually received cerclage and 148 did not. We observed similar results when considering actual cerclage placement and non-placement (data not shown). For example, 17P was associated with a non significant OR of 0.70 (95% CI 0.23, 2.09) for perinatal death in the cerclage group.
Comment
17P in women with a prior SPTB and a cerclage for short CL < 25 mm at 16-22 6/7 weeks was not associated with an effect on PTB < 35 weeks. Several trials (9,10) have demonstrated that 17P prevents SPTB in women with prior PTB, and this is now recommended (14). A meta-analysis (8) of randomized trials, and individual trial (5) and, more importantly, one large individual trial (3) have shown that cerclage prevents SPTB in women with a prior SPTB if they develop a short CL<25mm. Our data do not support the hypothesis that these two interventions (17P and cerclage) are cumulative in their benefit in this highly selected patient population.
In the absence of cerclage, 17P was associated with a reduction in previable birth and perinatal mortality in women with a prior SPTB and a CL <25 mm. Our results are in agreement with the benefit shown of 17P in women with prior SPTB in general (9). The effect of 17P for asymptomatic women with a short CL has not yet been reported, but is under much current investigation. Vaginal progesterone has also been associated with prevention of preterm birth in women with a short CL (13,15), but the effect of cerclage was not evaluated in these two trials.
The possible relationship between 17P and ultrasound-indicated cerclage has not been studied before, so this is a strength of our study. A prior study (16) reported the effect of 17P in women with cerclage, but could not distinguish between cerclage placed for history- or ultrasound- or even physical exam-indications. Another strength is the use of 17P was actually confirmed with measure of compliance. While the clinical trial was not powered for this secondary analysis, we did plan for it near the inception of the primary study. Because the sample size was predetermined by the results of the clinical trial, this study may have had insufficient power to detect a clinically significant effect of 17P at other preterm gestational age cutoffs. 17P was associated with lower incidences of the primary and secondary outcomes, but rarely were the analyses significant. If one examines Tables 2 and 4, the rates of early PTB at 28 and 32 weeks show that for women with no cerclage and no 17P, the rates of PTB are 25% and 34%, respectively; if one performs cerclage those rates drop to 17% and 25%; if one does not perform cerclage but starts 17P the rates also drop and are similar at 15% and 21%; and then finally if one does both cerclage and 17-OHP the rates appear the lowest at 9% and 17%. The OR for benefit from 17P is about 0.5 for both sets of patients with and without cerclage. It’s true that the OR for these effects were not statistically significant, with upper limits of the OR varying between 1.14 and 1.51, but this may be due to Beta error. Post-hoc analysis reveals that, to detect a change in the rate of PTB<35weeks from 34% to 30%, 2134 women are needed in each 17P and non-17P group (for the cerclage arm) to have 80% power. Similarly, for 80% power, to detect a change in the rate of PTB<32weeks from 25% to 17%, 406 women are needed in each arm, and for a difference in the rate of PTB<28weeks from 17% to 9%, 276 women are needed in each arm. In a larger study, these observed effects may be significant; the observed OR effects are consistent in both groups and are therefore suggestive of possible benefit of both therapies together. A more definitive study of this would be a 4-armed randomized factorial trial of placebo-no-cerclage, cerclage-no-17P, 17P-no-cerclage, and cerclage plus 17P.
Only one trial has compared the effect on SPTB of ultrasound-indicated cerclage versus 17P in women with a short CL<25mm (17). The cumulative effect of cerclage with 17P could therefore not be evaluated. No differences in effect were noted between 17P and cerclage groups, but the trial did not recruit the planned sample size because it was felt ‘impractical, unethical and unreasonable’ to withhold 17P from women (in the cerclage group) with prior SPTB. Cerclage was more effective at preventing SPTB compared to 17P in women with CL<15mm. This is in agreement with our results, showing that 17P is effective at 15-24mm, but may not be as effective at shorter cervical lengths.
It is yet unclear if progesterone prevents a cervix from shortening. In asymptomatic women with prior PTB, 17P prophylaxis was not associated with an effect on cervical length shortening in one study (18), while in another, it was associated with significant preservation of cervical length (19). In women with preterm labor, 17P injections instead prevented further cervical shortening (20). If 17P prevented cervical shortening from occurring, then women who responded best to 17P may never have developed a CL < 25mm and therefore this study may have inadvertently “selected” for women who are not “responders” to 17P. In them, this would obviate the need for ultrasound-indicated cerclage, and justify using both approaches (17P for prior SPTB, and cerclage for short CL) for prevention of preterm birth in women with a prior SPTB.
Several questions remain for use of progesterone and cerclage for prevention of preterm birth. Many factors may dictate management, such as prior obstetrical/gynecological history and risk factor for preterm birth, number of fetuses, degree of cervical shortening and gestational age at detection, etc. For example, cerclage may be better for shorter CL (3, 17), while progesterone may be more efficacious for women with lesser degrees of cervical shortening. (13) It is important to highlight that in our study women were screened serially by ultrasound for a short CL, and studies who screen only once may have different results. Better understanding of the mechanisms of 17P and of cerclage will help the clinician understand further how these two interventions are best employed. The fact that cerclage may have more of a mechanical mechanism while 17P may work more by its anti-inflammatory properties might make their effect cumulative. The role of inflammation (21), infection, genetic markers, enzymes (e.g. sialidases, collagenases), FFN, and other factors will play a larger role in selection of these therapies for the woman with a short CL in the near future. (22, 23) More research is also needed to look at interactions of several possible therapies for short CL, such as cerclage, progesterone, indomethacin, antibiotics, and others. Several trials and studies are currently ongoing and will soon provide more evidence to be able to answer these questions and guide clinical care.
Acknowledgements
Other members of the VUCT consortium: Robert S. Egerman, MD; Mark Tomlinson, MD; Richard Silver MD; Susan M. Ramin, MD; Michael Gordon MD; Helen Y. How, MD; Eric J. Knudtson, MD; Suzanne Cliver, MSPH; John C. Hauth, MD
Funding: The Eunice Kennedy Shriver National Institute of Child Health and Development provided funding via grant U01 HD039939
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Reprints will not be available Accepted in abstract format for an oral presentation on Feb. 4th, 2010 at the 30th Annual Meeting of the Society for Maternal-Fetal Medicine, in Chicago, IL.
References
- 1.Iams JD, Goldenberg RL, Meis PJ, Mercer BM, Moawad A, Das A, et al. The length of the cervix and the risk of spontaneous premature delivery. NEJM. 1996;334(9):567–72. doi: 10.1056/NEJM199602293340904. [DOI] [PubMed] [Google Scholar]
- 2.Mercer BM, Goldenberg RL, Moawad AH, Meis PJ, Iams JD, das AF, et al. The preterm prediction study: effect of gestational age and cause of preterm birth on subsequent obstetric outcome. Am J Obstet Gynecol. 1999;181:1216–21. doi: 10.1016/s0002-9378(99)70111-0. [DOI] [PubMed] [Google Scholar]
- 3.Owen J, Hankins G, Iams JD, Berghella V, Sheffield JS, Perez-Delboy A, et al. Multicenter randomized trial of cerclage for preterm birth prevention in high-risk women with shortened midtrimester cervical length. Am J Obstet Gynecol. 2009;201:375.e1–8. doi: 10.1016/j.ajog.2009.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rust OA, Atlas RO, Reed J, van Gaalen J, Balducci J. Revisiting the short cervix detected by transvaginal ultrasound in the second trimester: Why cerclage therapy may not help. Am J Obstet Gynecol. 2001;185:1098–105. doi: 10.1067/mob.2001.118163. [DOI] [PubMed] [Google Scholar]
- 5.Althuisius SM, Dekker GA, Hummel P, Bekedam DJ, van Geijn HP. Final results of the cervical incompetence prevention randomized cerclage trial (CIPRACT): Therapeutic cerclage with bed rest versus bed rest alone. Am J Obstet Gynecol. 2001;185:1106–12. doi: 10.1067/mob.2001.118655. [DOI] [PubMed] [Google Scholar]
- 6.To MS, Alfirevic Z, Heath VCF, Cacho AM, Williamson PR, Nicolaides KH. Cervical cerclage for prevention of preterm delivery in women with short cervix: randomized controlled trial. Lancet. 2004;363:1849–53. doi: 10.1016/S0140-6736(04)16351-4. [DOI] [PubMed] [Google Scholar]
- 7.Berghella V, Odibo AO, Tolosa JE. Cerclage for prevention of preterm birth in women with a short cervix found on transvaginal ultrasound examination: A randomized trial. Am J Obstet Gynecol. 2004;191:1311–7. doi: 10.1016/j.ajog.2004.06.054. [DOI] [PubMed] [Google Scholar]
- 8.Berghella V, Odibo AO, To MS, Rust OA, Althuisius SM. Cerclage for short cervix on ultrasonography: Meta-analysis of trials using individual patient-level data. Obstet Gynecol. 2005;106:181–9. doi: 10.1097/01.AOG.0000168435.17200.53. [DOI] [PubMed] [Google Scholar]
- 9.Meis PJ, Klebanoff M, Thom E, Dombrowski MP, Sibai B, Moawad AH, et al. Prevention of recurrent preterm delivery by 17 alpha-hydroxyprogesterone caproate. N Engl J Med. 2003;348:2379–85. doi: 10.1056/NEJMoa035140. [DOI] [PubMed] [Google Scholar]
- 10.MacKenzie R, Walker M, Armson A, Hannah ME. Progesterone for the prevention of preterm birth among women at increase risk: a systematic review and meta-analysis of randomized controlled trials. Am J Obstet Gynecol. 2006;194:1234–42. doi: 10.1016/j.ajog.2005.06.049. [DOI] [PubMed] [Google Scholar]
- 11.Owen J, Yost N, Berghella V, Thom E, Swain M, Dildy GA, et al. Mid-trimester endovaginal sonography in women at high risk for spontaneous preterm birth. JAMA. 2001;286:1340–8. doi: 10.1001/jama.286.11.1340. [DOI] [PubMed] [Google Scholar]
- 12.To MS, Alfirevic Z, Heath VCF, et al. Cervical cerclage for prevention of preterm delivery in women with short cervix: randomized controlled trial. Lancet. 2004;363:1849–1853. doi: 10.1016/S0140-6736(04)16351-4. [DOI] [PubMed] [Google Scholar]
- 13.Fonseca E, Celik E, Parra M, Singh M, Nicolaides KH. Progesterone and the risk of preterm birth among women with a short cervix. N Eng J Med. 2007;357:462–469. doi: 10.1056/NEJMoa067815. [DOI] [PubMed] [Google Scholar]
- 14.American College of Obstetricians and Gynecologists Use of progesterone to reduce preterm birth. ACOG Committee Opinion No.419. Obstet Gynecol. 2008;112:963–5. doi: 10.1097/AOG.0b013e31818b1ff6. [DOI] [PubMed] [Google Scholar]
- 15.DeFranco EA, O’Brien JM, Adair CD, Lewis DF, Hall DR, Fusey S, et al. Vaginal progesterone is associated with a decrease in risk for early preterm birth and improved neonatal outcome in women with a short cervix: a secondary analysis from a randomized, double-blind, placebo-controlled trial. Ultrasound Obstet Gynecol. 2007;30:697–705. doi: 10.1002/uog.5159. [DOI] [PubMed] [Google Scholar]
- 16.Rebarber A, Cleary-Goldman J, Istwan NB, Rhea DJ, Desch C, Russo-Stieglitz K, Saltzman DH. The use of 17 alpha-hydroxyprogesterone caproate (17P) in women with cervical cerclage. Am J Perinatol. 2008;25:271–5. doi: 10.1055/s-2008-1064935. [DOI] [PubMed] [Google Scholar]
- 17.Keeler SM, Kiefer D, Rochon M, Quinones JN, Novetsky AP, Rust O. A randomized trial of cerclage vs. 17 α-hydroxyprogesterone caproate for treatment of short cervix. J Perinat Med. 2009;37:473–9. doi: 10.1515/JPM.2009.083. [DOI] [PubMed] [Google Scholar]
- 18.Durnwald CP, Lynch CD, Walker H, Iams JD. The effect of treatment with 17 alpha-hydroxyprogesterone caproate on changes in cervical length over time. Am J Obstet Gynecol. 2009;201:410.e1–5. doi: 10.1016/j.ajog.2009.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.O’Brien JM, DeFranco EA, Adair CD, Lewis DF, Hall DR, How H, et al. effect of progesterone on cervical shortening in women at risk for preterm birth: secondary analysis from a multinational, randomized, double-blind, placebo-controlled trial. Ultrasound Obstet Gynecol. 2009;34:653–9. doi: 10.1002/uog.7338. [DOI] [PubMed] [Google Scholar]
- 20.Facchinetti F, Paganelli S, Comitini G, Dante G, Volpe A. Cervical length changes during preterm cervical ripening: Effects of 17 alpha hydroxyprogesterone caproate. Am J Obstet Gynecol. 2007;453:e1–4. doi: 10.1016/j.ajog.2006.09.009. [DOI] [PubMed] [Google Scholar]
- 21.Kiefer DG, Keeler SM, Rust OA, Waycock CP, Vintzileos AM, Hanna N. Is midtrimester short cervix a sign of intraamniotic inflammation? Am J Obstet Gynecol. 2009;200:374.e1–374.e5. doi: 10.1016/j.ajog.2009.01.047. [DOI] [PubMed] [Google Scholar]
- 22.Romero R, Espinosa J, Erez O, Hassan S. The role of cervical cerclage in obstetric practice: can the patient who could benefit from this procedure be identified? Am J Obstet Gynecol. 2006;194:1–9. doi: 10.1016/j.ajog.2005.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sakai M, Shiozaki A, Tabata M, Sasaki Y, Yoneda S, Arai T, et al. Evaluation of effectiveness of prophylactic cerclage of a short cervix according to interleukin-8 in cervical mucus. Am J Obstet Gynecol. 2006;194:14–9. doi: 10.1016/j.ajog.2005.06.014. [DOI] [PubMed] [Google Scholar]