Abstract
Psychological distress has been inconsistently associated with sexual risk behavior in youth, suggesting additional factors, such as substance use, may explain this relationship. The mediating or moderating role of substance use on the relationship between psychological distress and sexual risk behaviors was prospectively examined over the four high school years in a sample of urban youth (N=850; 80% African American; 50% female). Growth curve modeling was used to estimate changes in sexual risk across adolescence and to test its association to psychological distress symptoms and frequency of substance use. Substance use was associated with psychological distress. Greater psychological distress was associated with increased sexual intercourse frequency, decreased condom use, and increased number of partners. Substance use fully mediated the relationship between psychological distress and intercourse frequency and condom use, and partially mediated the relationship between psychological distress and number of partners. We found no differences in mediation by sex or race/ethnicity and no evidence to support moderation of psychological distress and substance use on sexual risk. Findings suggest that psychological distress is associated with sexual risk because youth with greater psychological distress are also more likely to use substances. Practical implications for adolescent HIV/STI prevention are discussed.
Keywords: High risk youth, psychological distress, anxiety, depression, substance use, HIV/STI Risk
Psychological Distress, Substance Use, and HIV/STI Risk Behaviors among Youth
HIV and other sexually transmitted infections (STIs) remain a serious public health problem for youth in the US. While the onset of sexual activity is a developmental milestone of adolescence or young adulthood, youth's risk of acquiring HIV/STIs is larger than the overall population (Centers for Disease Control and Prevention [CDC], 2008a). Among sexually active high school youth, approximately 40% reported unprotected sex at their last sexual encounter; close to 25% used drugs or alcohol at last sexual encounter, and 15% reported sexual intercourse with four or more partners in their lifetime (CDC, 2008b). Recent estimates also suggest sex and racial/ethnic differences in high-risk sexual behaviors among youth, with males and African American and Hispanic youths reporting higher rates of sexual activity and risk (CDC, 2008b). Parallel to these behaviors, STI rates are increasing rapidly among youth (CDC, 2008a), with a notable disparity evidenced across sex and race. In 2007, females ages 15 to 19 years-old had the highest incidence of Chlamydia and African Americans in the same age group were almost 40 times more likely to report gonorrhea than their White counterparts (CDC, 2008b). In order to decrease the health-related effects of sexual risk behaviors and to intervene effectively as these youth transition from adolescence into young adulthood, we must understand the factors that increase these behaviors (Bauermeister, Zimmerman, Gee, Caldwell, & Xue, 2009). In this study, we examined the contribution of psychological distress and substance use on youth's sexual risk trajectories across adolescence in a sample of urban youth.
Psychological Distress and HIV/STI Sexual Risk Behavior
A growing body of literature has examined the potential causes and correlates of adolescent sexual risk behavior, including the effect of mental health problems on sexual risk behaviors among adolescents (Brown, Danovsky, Lourie, DiClemente, Ralph, & Ponton, 1997; Donenberg & Pao, 2000; Smith, 2001). Mental health difficulties and substance use increase rapidly during adolescence and young adulthood (Kessler, Avenevoli, & Merikangas, 2001; Kessler, 2004), and depression and anxiety are among the most common mental health difficulties faced by youth (Birmaher, et al., 1996; Pine, Cohen, Cohen, & Brook, 1999). Psychological distress (i.e. symptoms of depression and anxiety) is associated with sexual risk behaviors in diverse adolescent populations (e.g., high school students, youth in psychiatric treatment, and youth involved in the juvenile justices system), both in cross-sectional and longitudinal studies (Brown et al., 2006; Lehrer, Shrier, Gortmaker, & Buka, 2006; Rubin, Gold, & Primack, in press; Tolou-Shams, Brown, Houck, & Lescano, 2008).
The association between sexual risk and psychological distress among youth may be related to an attempt to regulate distressful affective states through sexual or intimate behaviors (Brown et al., 2006; Donenber & Pao, 2005). The desire for intimacy and love, for example, has been linked to sexual activity (Marston & King, 2006; Ott, Millstein, & Halpern-Felsher, 2004; Sanderson & Canter, 1995) and identified as a prominent reason for sexual debut among adolescents (Rogers, 1996). Psychological distress has also been associated with low self-efficacy to negotiate consistent condom use and low perceived relationship control among youth (Salazar et al., 2004), which may diminish an adolescent's condom use. Low motivation or feelings of hopelessness and helplessness consistent with depression, for example, may make it more difficult for an individual to adopt and maintain safer sexual practices (Brooks-Gunn & Paikoff, 1997; Brown et al., 2006). Alternatively, an individual may become depressed or anxious because of engaging in risky sexual behavior or contracting an STI (Shrier et al., 2002; Brown et al., 2006). Several researchers, however, have not found a relationship between symptoms of psychological distress and sexual risk behaviors (Bachanas, Morris, Lewis-Gess, Sarett-Cuasay, Sirl, Ries, et al., 2002; Donenberg, Emerson, Bryant, Wilson, & Weber-Shifrin, 2001; Tolou-Shams, Paikoff, McKirnan, & Holmbeck, 2007), suggesting additional factors may be involved.
Substance Use, Psychological Distress and HIV/STI Sexual Risk Behavior
Substance use and mental health problems frequently co-occur in adolescence (Angold, Costello & Erkanli, 1999; Armstrong & Costello, 2002; Kandel et al., 1997), and substance use is particularly common among youth with psychological distress (i.e. depression and anxiety) (Armstrong & Costello, 2002; Brook, Brook, Zhang, Cohen, & Whiteman, 2002). Youth may use substances as a way to self-medicate or alleviate these symptoms (Deykin, Levy, & Wells, 1987; Kelder et al., 2001; Lewishohn, Gotlib, & Seeley, 1995). Substances have also been shown to precede or exacerbate onset of psychiatric disorders such as major depression (Brook, Brook, Zhang, Cohen, & Whiteman, 2002; Brook, Cohen, & Brook, 1998). In the context of HIV/STI risk behaviors, the potential mediating or moderating role of substance use may account for the mixed findings in the literature between psychological distress and sexual risk behavior.
Substance use has been associated with high rates of sexual risk behavior in adolescents (Collins, Ellickson, Orlando, & Klein, 2005; Cook et al., 2006; Graves & Leigh, 1995; Guo et al., 2002; Tapert, Aarons, Sedlar, & Brown 2001). The exact association between substance use and sexual risk is likely multifaceted. Risk appears to be highest among youth who use substances frequently, who use substances before or during sex, and who use more serious substances (e.g., cocaine) (Collins et al., 2005; Graves & Leigh, 1995). Substance use impairs decision making ability, reduces risk perception and judgment, and may heighten arousal, reducing the likelihood of using condoms and negotiating safer sex practices (Dausey & Desai, 2003; Logan, Cole, & Leukefeld, 2002; McKinnon, 1996). In adolescence, substance use may also indirectly increase HIV/STI risk via exposing the youth to deviant peers or social groups and risky sexual partners (Houck et al., 2006), and by straining the resiliency effects associated with having protective ties with family and positive peers (Fergus & Zimmerman, 2005). In some high risk samples, such as homeless or runaway youth, youth may also engage in sex exchange practices in order to support a substance addiction (Greene, Ennett, & Ringwalt, 1999). Thus, in adolescents, substance use, psychological distress and risky sexual behavior frequently co-occur, yet the exact nature of this relationship is not well understood.
Study Objectives and Hypotheses
Given that substance use has been strongly associated with both psychological distress and sexual risk behavior, it may account for the inconsistent findings in the literature regarding the association between psychological distress and sexual risk. Yet, most researchers who have found an association between psychological distress and HIV/STI sexual risk have not taken into account the effects of substance use. The use of substances may serve to moderate the association of psychological distress and sexual risk (i.e., greater substance use exacerbates the effect of psychological distress on sexual risk). Conversely, substance use may mediate the association between psychological distress and sexual risk (i.e., the effect of psychological distress on sexual risk behavior occurs via youth's substance use). The existing literature justifies investigation of both hypotheses.
1) Substance use may moderate the relationship between psychological distress and HIV/STI sexual risk behaviors
Substance use may moderate the relationship between psychological distress and sexual risk, serving to exacerbate psychological symptoms and increase the negative effects of psychological distress on sexual risk behavior. Ramrakha and colleagues (Ramrakha, Caspi, Dickson, Moffitt, & Paul, 2000), for example, found that, although depressive and anxiety disorders were related to sexual risk behaviors in a sample of youth, youth who reported comorbid depressive and substance use disorders were even more likely to engage in risk behaviors. Similarly, Teplin and colleagues (2005) found that the association between sexual risk behaviors and major mental disorders (MMD; e.g., depression, manic episode or psychosis) among detained youth was less robust when compared to those youth who reported comorbid MMD and substance use disorders (SUD). Yet, the additive effect of comorbid MMD and SUD on risk behavior diminished as these detained youth grew older (Elkington et al., 2008). Both of these studies examined psychiatric disorder, and, as such, these results may not apply to youth who experience psychological distress but do not reach the threshold for a clinical diagnosis. Consequently, as a contribution to this literature, we examined whether the combined effect of psychological distress and substance use (i.e., interaction effect) was associated to sexual risk behaviors across adolescence.
2) Substance use may mediate the relationship between psychological distress and HIV/STI sexual risk behaviors
As an alternative explanation of these relationships, substance use may mediate the relationship between psychological distress and sexual risk. Given the robust association between substance use and sexual risk, it may be the use of substances by youth with psychological distress that places them at increased risk for engaging in risky sexual behaviors (Chen, Stiffman, Cheng, & Dore, 1997; Shrier et al., 2001). In a cross-sectional study of school-aged youth, Shrier and colleagues (2001) found that the association between symptoms of depression and prior history of STI was mediated by alcohol and marijuana use. This association, however, was noted only for males. In a sample of youth seeking services (i.e., child welfare, primary health care, juvenile justice, and education), Chen et al., (1997) found that the positive association between depressive symptoms and sexual risk behaviors disappeared after accounting for substance abuse and conduct disorder symptoms. Taken together, findings from these two studies suggest that the association between psychological distress and HIV/STI risk behaviors identified in prior studies may have been confounded by substance use. Yet, whether the mediating effect of substance use changes as youth age or differs by race/ethnicity and sex is not clear.
A longitudinal study that disentangles the association between psychological distress, substance use and sexual risk behavior is needed. Youth in urban settings are at substantial risk for HIV and other poor health outcomes in adulthood. Understanding the role of key factors in HIV/STI sexual risk behaviors can help identify those youth at greatest risk for HIV/STIs and, in turn, inform the design of effective HIV/STI prevention interventions that focus on the mental health and substance use needs as youth transition into adulthood. Given the exploratory nature of this study, we sought to extend the literature by examining both the mediation and moderation hypotheses. In order to do so, we first determined a basic association between psychological distress and HIV/STI sexual risk behaviors across adolescence. We then, examined whether substance use plays a mediating and/or moderating role in this relationship. Finally, we examined whether race/ethnicity or sex moderate either the basic association between psychological distress and HIV/STI sexual risk behavior or the mediating/moderating role of substance use.
Methods
Sample
This study is based on an eight-year longitudinal study of youth from mid-adolescence to the transition into young adulthood. Data were collected from 850 adolescents beginning their ninth grade (Wave 1: 1994) in one of four public high schools in a Flint, Michigan. To be eligible for the study, participants had a grade point of 3.0 or lower at the end of the eighth grade, were not diagnosed by the school as having emotional or developmental impairments, and were identified as African American, White, or Bi-racial (African American and White). Of the 979 youth who met criteria, 52 had left the public school system; 67 were consistently absent from school after several attempts to interview them; and nine participants were refused participation by parents and one refused to participate. The final sample, n=850, represents 92% of the eligible youth. Waves 1 through 4 and correspond to the participants' high school years (1994-1997). Waves 5 through 8 correspond to the transition to young adulthood years (2000-2004). Data for this report focuses on the first four Waves (e.g., the high school years). A more detailed description of our methods is published elsewhere (Bauermeister, Zimmerman, Barnett & Caldwell, 2007; Ramirez-Valles, Zimmerman, & Newcomb, 1998).
Fifty percent of the original sample was female. Adolescents self-reporting as African American constituted 80% percent of the sample in Wave 1 (n = 679); 17% were White (n = 145); and, three percent were biracial (n = 26). The mean age at Wave 1 for participants was 14.55 years (SD=.66).
Procedures
Participants in Waves 1–4 (i.e., 9th to 12th grades) were interviewed at one-year intervals, whether they were in or out of school. Structured, close-ended, face-to-face interviews were conducted with students in school or in a community setting if the participants could not be found in school. Before each interview, the participant read and signed the study's consent forms and asked any questions regarding the confidentiality procedures. On average, each interview lasted 50-60 minutes. After the interview portion of the protocol, participants completed a self-administered paper and pencil questionnaire about alcohol and substance use, sexual behavior and other sensitive information. The study had a 90% response rate by Wave 4. Participants were given an incentive ($15 for Wave 1, $20 for Wave 2, $25 for Waves 3 and 4, respectively) as remuneration for taking time to participate in the study. The University of Michigan's Institutional Review Board approved the study design and procedures (UM-IRB#H03-0001309).
Measures
Time-Varying Covariates
We include the unstandardized mean and standard deviation for study variables across the four Waves in Table 1. Below, we note the intraclass correlation coefficient for these time-varying covariates, as well as Cronbach's alpha coefficients for multi-item scales.
Table 1.
Descriptive Statistics for Study Variables across Waves 1 thru 4
| Wave 1 | Wave 2 | Wave 3 | Wave 4 | |||||
|---|---|---|---|---|---|---|---|---|
| Mean(SD) | α | Mean(SD) | α | Mean(SD) | α | Mean(SD) | α | |
| Condom use | 4.49(1.06) | --- | 4.45(1.08) | --- | 4.30(1.17) | --- | 4.05(1.29) | --- |
| Sex Frequency | 1.75(1.84) | --- | 2.02(1.84) | --- | 2.32(1.96) | --- | 2.85(2.03) | --- |
| Number of Partners | 2.10(3.21) | --- | 1.89(2.70) | --- | 2.02(2.94) | --- | 1.85(2.26) | --- |
| Depression | 2.05(.64) | .70 | 2.20(.77) | .73 | 2.13(.73) | .72 | 2.11(.79) | .77 |
| Anxiety | 1.60(.62) | .78 | 1.76(.82) | .84 | 1.69(.77) | .83 | 1.71(.87) | .88 |
| Alcohol Use | 1.01(1.45) | --- | 1.24(1.57) | --- | 1.33(1.76) | --- | 1.56(1.80) | --- |
| Marijuana Use | 0.96(1.67) | --- | 1.57(2.07) | --- | 1.64(2.19) | --- | 1.74(2.27) | --- |
Frequency of Sexual Intercourse
Participants self-reported their frequency of sexual intercourse in the previous year (“How many times have you had sex in the last year?”). Participants could respond using the following categories: 0 = None, 1 = 1 or 2 times, 2 = 3 to 5 times, 3 = 6 to 8 times, 4 = 9 to 11 times, and 5 = 12 or more times. Participants reporting never having sex or not having had sex in the previous year were coded as zero. The intraclass correlation for frequency of sexual intercourse over the 4 waves was α = .81.
Consistent Condom Use
Across all Waves, participants self-reported their condom use over the previous year (“How often have you used a condom when having sex in the last year?”). Participants could respond with one of the following categories: 1=Almost never, 2=Not very often, 3=Half of the time, 4=Most of the time, and 5=Always. The intraclass correlation for condom use over the 4 waves was α = .52.
Number of sex partners
Participants reported the number of sex partners in lifetime using an open-ended question format at Wave 1 (“How many partners have you had?”). For all other Waves, participants self-reported the number of sex partners in the past year by answering an open-ended question (“How many sex partners have you had in the last year?”). The intraclass correlation for number of partners over the 4 waves was α = .69.
Psychological distress
Two indicators of psychological distress, depression (6 items) and anxiety (6 items), were measured using the Brief Symptom Inventory (Derogatis & Spencer, 1982). Participants answered these items using a 5-point scale ranging from 1=never to 5=very often. We created a standardized psychological well-being composite score for each Wave based on participants' mean standardized values for depression and anxiety symptoms, respectively. The reliability for the depression scale ranged between .70 and .77 across the four years. The reliability for the anxiety scale ranged between .78 and .88 across the four years. The intraclass correlation for psychological well-being over the 4 waves was α = .66.
Substance use
Alcohol and marijuana use were measured with the same questions employed by the Monitoring the Future Study. Questions included frequency of alcohol and marijuana use, respectively, over the past year on a 7-point Likert scale (0 = 0 times; 6 = 40+ times). We created a standardized drug use composite score per each Wave based on the mean standardized value of participants' frequency reports for both alcohol and marijuana use. The intraclass correlation for alcohol and marijuana use over the 4 waves was α = .85.
Individual characteristics
We used Wave 1 baseline data to assess youth's demographic characteristics.
Demographic characteristics
Participants were asked to report their month and year of birth, race, and sex. Age was computed for each Wave by subtracting the interview date to their month and year of birth. Participant's race was collapsed into a dichotomous variable; Whites served as the referent group. Biracial participants were included within the African American category, as there were too few cases (N=26) to include them as a separate group and their exclusion from the African American category did not change our results (data not shown). Males served as the referent group for the sex variable. Forty percent of the youth reported living with both parents. Youth also reported the highest level of education for each parent: 35% of youth's parents had completed high school; 35% had completed some college; and 20% had a college degree. In addition, participants reported the occupations of both parents as a measure of socioeconomic status (SES). Occupations were assigned a prestige score using Nakao and Treas' (1994) classification and rating scheme. The highest occupational group received a score of 64.38 (professional), and the lowest group received a score of 27.84 (private household worker). If scores were available for both parents, the higher prestige score was used for analysis. Parents of youth were mostly blue-collar workers from the local factories. The mean prestige score was 39.92 (SD = 9.77).
Data Analytic Strategy
First, we prepared the data using SPSS 17.0 before estimating the multilevel model. Longitudinal data preparation consisted of exploratory analyses on all variables, recoding of user-reported missing data (i.e., Refusal, Don't know) as system missing, and restructuring of study variables for growth curve analyses. We then used HLM 6.08 (SSI, 2009) to test the association between sex risk and the time-varying covariates across the four high school years. While a repeated measures regression performs list-wise deletion for cases with missing values in one or more data points, HLM maximizes all available data because its algorithms do not require information across all Waves in order to compute growth estimates for all participants (Raudenbush & Bryk, 2002). Similar to repeated measures regressions, multilevel modeling allows the total variance to be divided into within-individual variation (Level One Model; i.e., change in sex behavior over time) and between-individual variation (Level Two Model; i.e., person-centered characteristics such as sex and race).
The level-1 model assumes the within-person variation for participant i's outcome (Yti) at each wave can be modeled by estimating his/her initial mean score on the outcome (π0i), the growth parameters (πpi), and his/her associated within-individual random error term (eti), where t is the wave of each observation, i is the individual, and p is a particular growth parameter for each wave. The initial mean score for our growth curve models were centered on age 14, with the time growth parameter accounting for the linear change in the outcome for every additional year of age during adolescence. We also included the quadratic term of this growth parameter when the outcome had a curvilinear shape. A quadratic piecewise growth estimate approximates the mean acceleration or deceleration of the outcome over time. We then examined whether the mean initial score (π0i) and growth term parameters (πpi) differed by sex and race by inspecting the random effects table in the HLM output (p < .05). If a term's random effects were nonsignificant, we kept each term as a fixed covariate in the level-1 model. We dropped nonsignificant predictors from the level-1 and level-2 models.
We carried out several analyses to test our study hypotheses. Following a traditional mediational analysis, we first modeled psychological distress and tested its association to youth's alcohol and marijuana use across adolescence (see Table 2). We then examined whether psychological distress was correlated with sex risk across adolescence (see Table 3; Model 1). If the association between psychological distress and sexual risk was significant, we included youth's alcohol and marijuana use in a subsequent model (see Table 3; Model 2). To test our mediation hypothesis, we then used Sobel's test to examine whether psychological distress had an indirect effect on the sex risk outcomes through alcohol and marijuana use, after controlling for the direct effects of mental health on sex risk (Krull & MacKinnon, 1999; MacKinnon, Warsi, & Dwyer, 1995a; 1995b). Finally, to test for the moderation of substance use and psychological distress on sex risk behaviors over time, we created a time-varying interaction estimate and included this term alongside the main effects of substance use and psychological distress in each model.
Table 2.
Growth Curve of Psychological Distress across Adolescence
| b | SE | p | |
|---|---|---|---|
| Mean Score at Age 14, π00i a | 0.34 | 0.2 | 0.1 |
| Female, β01 | 0.07 | 0.11 | Ns |
| African American, β02 | 0.24 | 0.14 | 0.1 |
| Mean Linear Change, π10i | 0.98 | 0.09 | 0.001 |
| Female, β11 | -0.11 | 0.04 | 0.01 |
| African American, β12 | -0.34 | 0.06 | 0.001 |
| Mean Quadratic Change, π20i | -0.07 | 0.01 | 0.001 |
| Alcohol and Marijuana Use, π30i | 0.20 | 0.04 | 0.001 |
Mean score at age 14 coefficient (π00i) refers to overall score at baseline (i.e. Wave 1) for white youth
Table 3.
Growth Curve Models for Youth Sexual Risk Behaviors Across Adolescence
| Model 1 | Model 2 | |||||
|---|---|---|---|---|---|---|
| b | SE | p | b | SE | P | |
| Sexual Intercourse Frequency | ||||||
| Mean Score at Age 14, π00i | 1.42 | 0.24 | 0.001 | 1.63 | 0.23 | 0.001 |
| male, β01 | -0.68 | 0.14 | 0.001 | -0.67 | 0.13 | 0.001 |
| African American, β02 | 1.16 | 0.17 | 0.001 | 1.09 | 0.16 | 0.001 |
| Mean Linear Change, π10i | 0.32 | 0.09 | 0.001 | 0.11 | 0.09 | ns |
| Female, β11 | 0.22 | 0.05 | 0.001 | 0.24 | 0.05 | 0.001 |
| African American, β12 | -0.32 | 0.06 | 0.001 | -0.2 | 0.06 | 0.001 |
| Psychological Distress, π20i | 0.09 | 0.05 | 0.05 | 0.02 | 0.05 | ns |
| Alcohol and Marijuana Use, π30i | 0.34 | 0.02 | 0.001 | |||
| Sobel Test | 4.80 | 0.001 | ||||
| Consistent Condom Use | ||||||
| Mean Score at Age 14, π00i | 4.47 | 0.18 | 0.001 | 4.38 | 0.18 | 0.001 |
| Female, β01 | 0.21 | 0.09 | 0.05 | 0.2 | 0.09 | 0.05 |
| African American, β02 | -0.25 | 0.11 | 0.05 | -0.23 | 0.11 | 0.01 |
| Mean Linear Change, π10i | 0.15 | 0.08 | 0.1 | 0.25 | 0.09 | 0.01 |
| Female, β11 | -0.21 | 0.03 | 0.001 | -0.22 | 0.03 | 0.001 |
| African American, β12 | 0.13 | 0.05 | 0.01 | 0.1 | 0.05 | 0.05 |
| Mean Quadratic Change, π20i | -0.02 | 0.01 | 0.05 | -0.03 | 0.01 | 0.05 |
| Psychological Distress, π30i | -0.06 | 0.03 | 0.05 | -0.04 | 0.03 | ns |
| Alcohol and Marijuana Use, π40i | -0.11 | 0.01 | 0.001 | |||
| Sobel Test | -4.55 | 0.0001 | ||||
| Number of Partners | ||||||
| Mean Score at Age 14, π00i | 3.01 | 0.4 | 0.01 | 3.18 | 0.4 | 0.001 |
| Female, β01 | -1.54 | 0.24 | 0.01 | -1.54 | 0.25 | 0.001 |
| African American, β02 | 1.63 | 0.23 | 0.01 | 1.5 | 0.23 | 0.001 |
| Mean Linear Change, π10i | 0.00004 | 0.13 | ns | -0.09 | 0.12 | ns |
| Female, β11 | 0.16 | 0.07 | 0.05 | 0.17 | 0.07 | 0.05 |
| African American, β12 | -0.29 | 0.07 | 0.001 | -0.24 | 0.07 | 0.001 |
| Psychological Distress, π20i | 0.18 | 0.08 | 0.05 | 0.15 | 0.07 | 0.05 |
| Alcohol and Marijuana Use, π30i | 0.18 | 0.05 | 0.001 | |||
| Sobel Test | 2.92 | 0.01 | ||||
In subsequent sensitivity analyses, we examined and found no support to suggest that our results would differ if we had entered the mental health (e.g., depression and anxiety) and substance use (e.g., alcohol and marijuana use) indicators into the growth curves (i.e., instead of the composite scores). To facilitate brevity, we provide full statistical statements only for those outcomes that achieved statistical significance.
Results
Psychological Distress and Substance Use
Psychological distress across adolescence
At baseline (age 14), African American youth had greater psychological distress (b = .24, SE = .14; p ≤ .10) than their White counterparts (b = .34, SE = .02; p ≤ .10). We found no sex differences in youth's mean mental health score at baseline. After accounting for these baseline differences, we modeled the growth curve for psychological distress and found a non-linear quadratic model was appropriate (see Figure 1). Youth's psychological distress increased over time (b = .98, SE = .09, p ≤ .001), but the quadratic term indicated that the linear change decreased across adolescence (b = -.07, SE = .01; p ≤ .001). We found differences by race and sex in youth's linear growth term. On average, African American and female youth reported greater decreases in psychological symptoms across adolescence than their White (b = -.34, SE = .06; p ≤ .001) and male counterparts (b = -.11, SE = .04; p ≤ .01), respectively. We found no differences by race or sex in youth's quadratic growth term.
Figure 1. Change in Psychological Distress across Adolescence by Sex and Race.
Note Across the adolescent years, White males and females reported greater increases in mental health symptomatology than their African American counterparts.
Substance use across adolescence
Use of alcohol and/or marijuana was associated with more psychological distress across adolescence (b = .20, SE = .04, p ≤ .001). Youth were more likely to report greater psychological distress over time with every unit increase in substance use. We found no differences by race or sex in the association between substance use and psychological distress.
Sexual Risk Behaviors
Sex frequency across adolescence
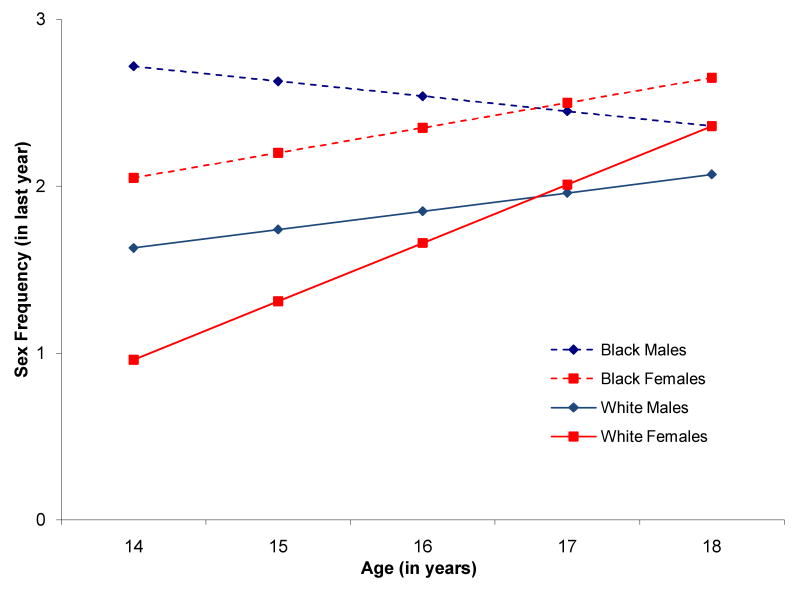
At age 14, youth reported having had sexual intercourse on several occasions (b = 1.63, SE = .23; p < .001). This initial mean score, however, varied by sex and race. Females reported less sexual intercourse at age 14 (b = -.67, SE = .13; p < .001) than males, and African American youth reported greater sexual intercourse frequency than White youth (b = 1.09, SE = .16; p < .001). Sexual intercourse frequency was modeled best with a linear growth term across adolescence, yet the growth rates differed by sex and race (see Figure 2). Compared to males, for example, females reported greater sexual intercourse frequency across adolescence (b = .22, SE = .05; p < .001). African American youth, on the other hand, reported less sexual intercourse frequency over time than their White counterparts (b = -.32, SE = .06, p < .001).
Figure 2. Change in Sexual Intercourse Frequency across Adolescence by Sex and Race.
Note Across the adolescent years, African American youth reported greater sexual intercourse frequency than their White counterparts. Female youth reported steeper increases in sexual activity than their male counterparts. (Y-axis scalar: 0 = None, 1 = 1 or 2 times, 2 = 3 to 5 times, 3 = 6 to 8 times)
Determining an association between psychological distress and sexual frequency
When we entered psychological distress as a time-varying covariate, we found greater psychological distress was associated with increased sexual intercourse frequency across adolescence (Model 1: b = .09, SE = .05; p < .05).
Mediation of substance use
We then entered substance use as a time-varying covariate in the model and found substance use was associated with increased sexual intercourse frequency across adolescence (b = .34, SE = .02; p < .001). Consistent with the mediation argument, we found substance use fully mediated the relationship between psychological distress and sexual intercourse frequency (Sobel = 4.80; p < .0001; see Model 2 in Table 3); that is, the association between psychological distress and sexual intercourse frequency became non-significant once substance use was included in the model.
Moderation of substance use
We entered the interaction term for psychological distress and substance use on sexual intercourse frequency to test a moderation model; however, we found no support for the moderation argument.
Moderation of sex and race/ethnicity
We found no differences by sex or race in the association between sexual intercourse frequency and the main effects of psychological distress or substance use, respectively, nor on their interaction effect.
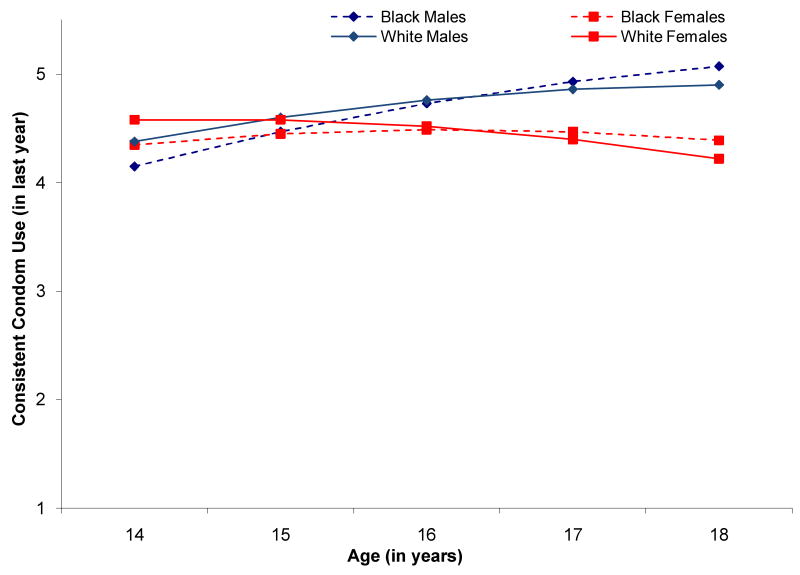
Condom use across adolescence
Sexually active youth reported frequent condom use at baseline (b = 4.47, SE = .18; p ≤ .001). At age 14, sexually active females (b = .21, SE = .09; p ≤ .05) reported greater condom use than males and African American youth reported less condom use that White youth (b = -.25, SE = .11; p ≤ .05). These sex and race differences reversed, however, as youth grew older. As shown in Figure 3, we found condom use was modeled best with a linear and quadratic term. The linear change, however, was found to vary by sex and race. Females reported less frequent condom use over time (b = -.22, SE = .03; p ≤ .001) than males. African American youth reported more frequent condom use over time (b =.10, SE = .05; p ≤ .05) than White youth. The linear change in youth's condom use decreased as youth grew older, as noted by the quadratic growth term (b = -.03, SE = .01; p < .05), yet this deceleration did not vary across sex or race.
Figure 3. Change in Consistent Condom Use across Adolescence by Sex and Race.
Note Across the adolescent years, African American and White youth reported high condom use. Female youth, however, reported steeper decreases in condom use than their male counterparts as they grew older. (Y-axis scalar: 1=Almost never, 2=Not very often, 3=Half of the time, 4=Most of the time, and 5=Always).
Determining an association between psychological distress and condom use
When we included psychological distress as a time-varying covariate into the model, we found greater psychological distress over time decreased condom use across adolescence (Model 1: b = -.06, SE = .03; p < .05).
Mediation of substance use
We then entered substance use as a time-varying covariate in the model and found it decreased consistent condom use across adolescence (b = -.11, SE = .01; p < .001). Furthermore, we found substance use fully mediated the relationship between psychological distress and condom use across adolescence (Sobel = -4.55; p < .0001; see Model 2 in Table 3); that is, the association between psychological distress and condom use became non-significant after accounting for substance use.
Moderation of substance use
To test for moderation, we entered the interaction term for psychological distress and substance use on condom use, yet we found no support for the moderation argument.
Moderation of sex and race/ethnicity
We found no differences by sex or race in the association between condom use and the main effects of psychological distress or substance use, respectively, nor on their interaction effect.
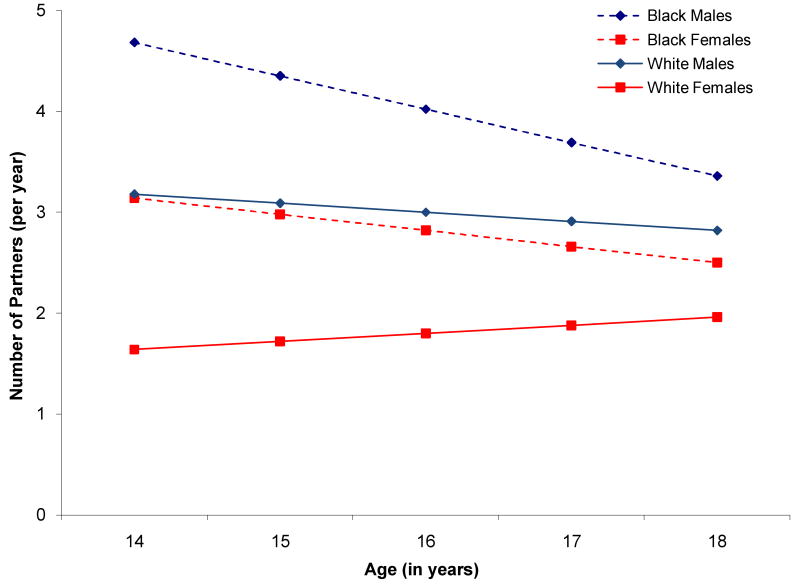
Number of partners across adolescence
Sexually active participants reported multiple partners at age 14 (b = 3.18, SE = .04; p < .001), yet the mean initial score differed by sex and race. Females reported fewer partners than males (b= -1.54, SE = .24; p < .01), and African American youth reported more partners than White youth (b = 1.63, SE = .23; p < .01). Number of partners was modeled best with a linear growth term, yet the change over time differed by sex and race (see Figure 4). Females reported a greater number of partners across adolescence than males (b = .17, SE = .07; p < .05). African American youth, on the other hand, reported fewer sexual partners across adolescence than White youth (b = -.24, SE = .07; p < .001).
Figure 4. Change in Number of Partners across Adolescence by Sex and Race.
Note Number of sexual partners decreased across the adolescent years. Black youth reported greater number of partners than their White counterparts. Females reported fewer sexual partners than males over time, yet males had steeper decreases in their number of partners across adolescence.
Determining an association between psychological distress and number of partners
When we entered psychological distress as a time-varying covariate, we found more psychological distress over time was associated with an increase in the number of partners reported across adolescence (Model 1: b = .18, SE = .08; p < .05).
Mediation of substance use
The association between psychological distress and number of partners remained statistically significant (b = .15, SE = .07; p < .05), even after adjusting for substance use as a time-varying covariate in the model (b = .18, SE = .05; p < .001). We found substance use partially mediated the relationship between psychological distress and sexual intercourse frequency (Sobel = 2.92; p < .01; see Model 2 in Table 3).
Moderation of substance use
When we entered the interaction term for psychological distress and substance use on number of partners, we found no support for the moderation argument.
Moderation of sex and race/ethnicity
We found no differences by sex or race in the association between condom use and the main effects of psychological distress or substance use, respectively, nor on their interaction effect.
Discussion
Our study extends the literature by examining the effect of both psychological distress and substance use on sexual risk over time, and testing whether substance use mediates or moderates the relationship between the psychological distress and HIV/STI sexual risk behaviors. Overall, mirroring national trends, we found that sexual risk behaviors increased across adolescence in our sample; specific findings by race/ethnicity and gender with respect to these national trends were also observed. The increase in sex risk behaviors across adolescence is concerning given that frequent and unprotected sex is the most prevalent route of HIV/STI transmission for adolescents in the US (CDC, 2008c). Consistent with prior studies, our data also indicate that psychological distress and substance use increased as youth aged (Kandel, Yamaguchi, & Chen, 1992; Kessler et al., 2001; Kessler, 2004), and were each associated with increased sexual risk behaviors across adolescence (Guo et al., 2002, Stiffman et al., 1992, Tubman, Windle & Windle, 1996). Few prospective studies, however, have disentangled the association among psychological distress, substance use and HIV/STI risk behavior across adolescence.
As expected, we found that substance use was associated with psychological distress across adolescence, and adolescents who used more substances more frequently reported greater psychological distress. One plausible explanation for this finding is that youth may use substances to self-medicate and manage the experience of psychological distress (Lewishohn et al., 1995; Deykin et al., 1987; Kelder et al., 2001); however, it is also plausible that using substances, such as alcohol, which is a central nervous system depressant, contributes to the onset of depression and anxiety (Brook et al., 2002). We are unable to determine causality without examining the onset of both psychological distress and substance use, but these results suggest that these factors covary over time. Nevertheless, either interpretation is worrisome in the context of HIV/STI prevention.
We found no evidence of a moderation effect for any of the sexual risk behaviors when we examined whether substance use enhanced the relationship between psychological distress and youth's HIV/STI sexual risk across adolescence. This suggests that youth with symptoms of psychological distress are not put at increased risk due to co-occurring substance use. For example, an adolescent's need to reduce painful affective states through physical intimacy is not increased by heightened sexual desire and decreased inhibition related to substance use. These findings are consistent with those of Shrier et al., (2001) but inconsistent with prior studies of psychiatric disorders (Ramrakha et al., 2000; Teplin et al., 2005). Our findings may differ from these studies of disorders, however, because of differences in operationalization of psychological distress and samples. In the current study of urban youth, we examined symptoms across adolescence whereas other research studies focused on the presence of one or more psychiatric disorders at one point in time. The effect of more severe experiences of mental illness on sexual risk may well be exacerbated by more serious substance use. Oshri and colleagues (2008) found that, for example, in a sample of youth in alcohol and drug abuse treatment (i.e. youth likely with a substance use disorder), those with moderate to high mental illness symptom severity were more likely to engage in HIV/STI sexual risk behavior compared to those with low symptom severity.
We found support for a mediation model. Although psychological distress is associated with HIV/STI sexual risk behaviors across adolescence, substance use may be a more proximal factor of sexual risk. Substance use fully mediated the association between psychological distress and both sexual frequency and condom use. Notably, we did not find any differences by type of substance used (i.e. alcohol or marijuana), nor did the mediation effect of substance use on these sexual behaviors differ by sex or race. These findings indicate that, in an urban sample of White and African-American youth, psychological distress is associated with sexual risk through its effect on substance use. Thus, psychological distress appears to be a more distal or indirect factor of sexual risk in our sample while substance use has a more proximal or direct effect. These results suggest that efforts to address urban adolescents' psychological distress or improve their psychological well-being may have the benefit of both helping to reduce substance use and therefore sexual risk behavior.
One mechanism in which adolescents experiencing psychological distress may also use substances is through their affiliation with other high-risk peer groups who use substances and engage in sexual risk behaviors (Brown et al., 1997; Donenberg, Emerson, Bryant, Wilson, & Weber-Shifrin, 2001; McFarlane, Bellissimo, & Norman, 1995). Thus, the youth's likelihood of engaging in sexual risk behavior increases (Bauermeister, Elkington, Brackis-Cott, Dolezal, & Mellins, 2009; Doljanac & Zimmerman, 1998; Elkington, Bauermeister, Brackis-Cott, Dolezal, & Mellins, 2009). Given the role social norms may play in the onset and enactment of risky behaviors among youth, future research examining the role of youth's social networks (e.g., prevalence of substance use and psychological distress among youth and his/her family and peers) would be useful. Alternatively, studies have also found that substance use, alcohol in particular, is related to sexual risk-taking depending on how the individual user expects it to be related (Gordon, Carey, & Carey, 1997; LaBrie, Earlywine, Schiffman, Pedersen, & Marriot, 2005). Thus, people who believe that drinking alcohol has positive effects on their sexual experience perceive fewer risks associated with unprotected sex and are more likely to engage in risky sexual behaviors compared to those who do not hold such expectations or beliefs (Dermen, Cooper, & Agocha, 1998; O'Hare, 2005) Future work examining the role of alcohol and other drugs in sexual situations, i.e. social lubrication (Stoner, George, Peters & Norris, 2007), for youth experiencing psychological distress and their expectancies of its effects on their sexual behavior would further extend our understanding of the mediating role of substance use on the relationship between psychological distress and sexual risk.
Interestingly, substance use only partially mediated the association between psychological risk and number of partners over time. Independent of substance use, mental distress may leave youth feeling alienated and isolated from family and peers (Donenberg & Pao, 2005; Hamilton, Asarnow, & Tompson, 1999), who then seek comfort in sexual partners as a method to reduce feelings of isolation and increase self-worth (Bachanas, Morris, Lewis-Gess, Sarett-Cuasay, Flores, et al., 2002). Potential reliance on partners to improve painful affect is concerning as the desire to avoid isolation and rejection by partners may result in risky sexual behavior as a way to maintain relationships (Donenberg & Pao, 2005; Lehrer et al., 2006). While the current study is a first step in understanding the association between psychological distress, substance use and sexual risk, future research is necessary to better understand the mechanisms through which substance use increases sexual risk among youth experiencing psychological distress.
While not a main focus of the study, we found some demographic differences. We saw overall growth in sexual risk behavior and psychological distress across adolescence in our sample, consistent with national trends; however, some specific findings differed. African Americans demonstrated a slower increase in sexual risk behaviors and females a slower increase in symptoms of psychological distress across adolescence compared to their White and male counterparts, respectively. These findings, while not consistent with prior literature or national trends (CDC, 2008b), may reflect the fact that African American and female youth reported higher rates of sexual risk behaviors and psychological distress, respectively, at baseline. In addition, our data suggest that trends in behaviors and mental health problems may differ by context (e.g. neighborhood or location). Flint, Michigan, the location of the current study, is a city that has experienced economic change following the collapse of the auto industry. The role of poverty in Flint likely differs from the role of poverty in other contexts (e.g. inner-city settings with predominantly ethnic minority youth) as the widespread economic decline in Flint affected African American and White youth alike. This finding thus underscores the importance of examining the role of neighborhood disadvantage within specific communities, and its potential relationship to patterns of risk behavior that may differ from national datasets and point toward tailored community interventions (Blankenship, Friedman, Dworkin & Mantell, 2006; Dworkin, Pinto, Hunter, Rabkin & Remien, 2008).
Several limitations of this study should be noted. First, the study's findings may be generalizable only to youth who reside in economically-disadvantaged urban centers. The fact that our results are consistent with past research of co-occurring mental health problems and substance use (Armstrong & Costello, 2002; Kandel et al., 1997), psychological distress, substance use and HIV risk (Guo et al., 2002, Stiffman et al., 1992, Tubman et al., 1996) as well as studies of mediation (Shrier et al, 2001), however, suggests the bias that may have been introduced by our sample may not be problematic. Second, we were unable to account for other factors that may influence sexual risk behavior. Low self-efficacy, including social self-efficacy and self-efficacy to refuse heavy drinking, has been associated with substance use, depression and increased sexual risk behaviors (Rosenthal, Moore, & Flynn, 1991; Seal, Minichiello, & Omodei, 1997). Adolescents with psychological distress also demonstrate externalizing symptoms (e.g., aggression, delinquency, and impulsivity) that have been found to be more closely associated with sexual risk behaviors and substance use than internalizing symptoms (e.g., depression and anxiety) (Donenberg et al., 2001). Given that these risk factors may co-occur and increase HIV risk among youth (Houck et al., 2006), future research examining the role of substance use, psychological distress, and externalizing symptoms on sex risk across adolescence is warranted.
These limitations notwithstanding, this study builds on our knowledge about the effects of psychological distress and substance use on HIV/STI sexual risk behaviors across adolescence in a unique sample of youth by examining these issues longitudinally and in a diverse sample. The results also have several prevention implications for both clinical and non-clinical settings. First, our data suggest that youth experiencing psychological distress and using substances are engaging in high rates of sexual risk behavior. Treatment providers are thus well positioned to reduce HIV/STI risk behaviors among youth in their care (Donenberg & Pao, 2005), and sexual risk reduction should be incorporated into these programs wherever possible (Mellins et al., 2009; Elkington, et al., 2008). Second, although most of our results indicate that the effects of psychological distress on sexual risk are indirect, and operate through substance use, they suggest that screening for and treating psychological distress and substance use in various non-clinical settings (e.g., schools, juvenile justice system) may be warranted because early detection may indirectly decrease HIV/STI risk behavior (Ellickson, McCaffrey, & Klein, 2009), by identifying those youth who might otherwise go untreated. Notably, our results suggest that programs that focus on youth in the first or second years of high school may be most beneficial because they are more likely to catch youth prior to or at the early stages of developing psychological distress and increasing substance use and sexual risk behaviors. Given the context of the study, youth development programs implemented during this time may delay the onset of substance use and risky sexual behavior while also providing assets for positive development in a resource constrained setting. Finally, despite the strong association between mental health problems, substance use and sexual risk behaviors, HIV/STI prevention programming for youth has typically not focused on mental health problems and substance use while also addressing sexual risk. Thus, our findings also suggest programs that address both psychological distress and substance use prevention may be most effective for HIV/STI prevention as well (Donenberg & Pao, 2005). Programs that identify triggers for engaging in both sex and substance use risk behaviors while also promoting mental health are necessary to address the comprehensive needs of youth at greater risk for HIV/STI infection.
Acknowledgments
This work was supported by two National Institute of Drug Abuse grants (5R01DA007484-11; “A longitudinal study of school dropout and substance use”, and 1R03AA017240-01; “Protective factors for alcohol use among urban adolescents”) awarded to Dr. Zimmerman. Dr. Elkington is supported by the Center Grant P30 MH43520 to the HIV Center for Clinical and Behavioral Studies, Anke A. Ehrhardt, PhD, Principal Investigator, from the National Institute of Mental Health. All authors have nothing to disclose.
References
- Angold A, Costello EJ, Erkanli A. Comorbidity. Journal of Child Psychology and Psychiatry. 1999;40:57–87. [PubMed] [Google Scholar]
- Armstrong TD, Costello EJ. Community Studies of Adolescent Substance Use, Abuse or Dependence and Psychiatric Comorbidity. Journal of Consulting and Clinical Psychology. 2002;70:1224–1239. doi: 10.1037//0022-006x.70.6.1224. [DOI] [PubMed] [Google Scholar]
- Bachanas P, Morris M, Lewis-Gess J, Sarett-Cuasay EJ, Flores AL, Sirl K, et al. Psychological adjustment, substance use, HIV knowledge, and risky sexual behavior in at-risk minority females: Developmental differences during adolescence. Journal of Pediatric Psychology. 2002;27(4):373–384. doi: 10.1093/jpepsy/27.4.373. [DOI] [PubMed] [Google Scholar]
- Bachanas P, Morris M, Lewis-Gess J, Sarett-Cuasay EJ, Sirl K, Ries JK, et al. Predictors of risky sexual behavior in African-American girls: Implications for prevention interventions. Journal of Pediatric Psychology. 2002;27(6):519–530. doi: 10.1093/jpepsy/27.6.519. [DOI] [PubMed] [Google Scholar]
- Bauermeister JA, Elkington KS, Brackis-Cott E, Dolezal C, Mellins C. Sexual behavior and perceived peer norms: Comparing perinatally infected and affected youth. Journal of Youth and Adolescence. 2009;38(8):1110–22. doi: 10.1007/s10964-008-9315-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauermeister JA, Zimmerman M, Gee G, Caldwell C, Xue Y. Work and Sexual Trajectories among African American youth. Journal of Sex Research. 2009;46(4):290–300. doi: 10.1080/00224490802666241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauermeister JA, Zimmerman M, Barnett TE, Caldwell C. Working in High School and Adaptation in the Transition to Young Adulthood among African American Youth. Journal of Youth and Adolescence. 2007;36:877–890. [Google Scholar]
- Blankenship K, Friedman S, Dworkin S, Mantell J. Structural interventions: Concepts, challenges and opportunities for research. Journal of Urban Health. 2006;83(1):59–72. doi: 10.1007/s11524-005-9007-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birmaher B, Ryan N, Williamson D, Brent DA, Kaufman J, Dahl RE, et al. Childhood and adolescent depression: A review of the past 10 years, part I. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35:1427–1439. doi: 10.1097/00004583-199611000-00011. [DOI] [PubMed] [Google Scholar]
- Brook DW, Brook JS, Zhang C, Cohen P, Whiteman M. Drug Use and the Risk of Major Depressive Disorder, Alcohol Dependence, and Substance Use Disorders. Archives of General Psychiatry. 2002;59:1039–1044. doi: 10.1001/archpsyc.59.11.1039. [DOI] [PubMed] [Google Scholar]
- Brook JS, Cohen P, Brook DW. Longitudinal Study of co-occurring psychiatric disorders and substance use. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37:322–330. doi: 10.1097/00004583-199803000-00018. [DOI] [PubMed] [Google Scholar]
- Brooks-Gunn J, Paikoff R. Sexuality and developmental transitions during adolescence. In: Schulenberg J, Maggs J, Hurrelmann K, editors. Health Risks and Developmental Transactions During Adolescence. New York, NY: Cambridge University Press; 1997. pp. 190–219. [Google Scholar]
- Brown LK, Danovsky MB, Lourie KJ, DiClemente RJ, Ralph J, Ponton LE. Adolescents with psychiatric disorders and the risk of HIV. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36(11):1609–1617. doi: 10.1016/S0890-8567(09)66573-4. [DOI] [PubMed] [Google Scholar]
- Brown LK, Tolou-Shams M, Lescano C, Houck C, Zeidman J, Pugatch D, et al. Depressive symptoms as a predictor of sexual risk among African American adolescents and young adults. Journal of Adolescent Health. 2006;39(3):444.e1–444.e8. doi: 10.1016/j.jadohealth.2006.01.015. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. HIV/AIDS among Youth. 2008c Retrieved August 26, 2009 from http://www.cdc.gov/hiv/resources/factsheets/youth.htm.
- Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance 2007. 2008a Retrieved July 20, 2009 from http://www.cdc.gov/std/stats07/toc.htm.
- Centers for Disease Control and Prevention. Youth risk surveillance–United States 2007. MMWR. 2008b;57(SS-4) Retrieved July 9, 2009, from http://www.cdc.gov/HealthyYouth/yrbs/pdf/yrbss07_mmwr.pdf.
- Chen Y, Stiffman AR, Cheng L, Dore P. Mental health, social environment and sexual risk behaviors of adolescent service users: A gender comparison. Journal of Child and Family Studies. 1997;6(1):9–25. [Google Scholar]
- Collins RL, Ellickson PL, Orlando M, Klein DJ. Isolating the nexus of substance use, violence and sexual risk for HIV infection among young adults in the United States. AIDS and Behavior. 2005;9(1):73–87. doi: 10.1007/s10461-005-1683-2. [DOI] [PubMed] [Google Scholar]
- Cook RL, Comer DM, Wisenfeld HC, Chang C, Tarter R, Lave JR, Clark DB. Alcohol and drug use and related disorders: An underrecognized health issue among adolescents and young adults attending sexually transmitted disease clinics. Sexually Transmitted Diseases. 2006;33(9):565–570. doi: 10.1097/01.olq.0000206422.40319.54. [DOI] [PubMed] [Google Scholar]
- Dausey DJ, Desai RA. Psychiatric comorbidity and the prevalence of HIV infection in a sample of patients in treatment for substance abuse. The Journal of Nervous and Mental Disease. 2003;191(1):10–17. doi: 10.1097/00005053-200301000-00003. [DOI] [PubMed] [Google Scholar]
- Dermen KH, Cooper ML, Agocha VB. Sex-related alcohol expectancies as moderators of the relationship between alcohol use and risky sex in adolescents. Journal of Studies on Alcohol. 1998;59(1):71–77. doi: 10.15288/jsa.1998.59.71. [DOI] [PubMed] [Google Scholar]
- Deykin EY, Levy JC, Wells V. Adolescent depression, alcohol and drug abuse. American Journal of Public Health. 1987;77(2):178–182. doi: 10.2105/ajph.77.2.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doljanac RF, Zimmerman MA. Psychosocial factors and high risk sexual behavior: Race differences among urban adolescents. Journal of Behavioral Medicine. 1998;21:451–467. doi: 10.1023/a:1018784326191. [DOI] [PubMed] [Google Scholar]
- Donenberg GR, Emerson E, Bryant FB, Wilson H, Weber-Shifrin E. Understanding AIDS-risk behavior among adolescents in psychiatric care: Links to psychopathology and peer relationships. Journal of the American Academy of Child Adolescent Psychiatry. 2001;40(6):642–653. doi: 10.1097/00004583-200106000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donenberg GR, Pao M. Youths and HIV/AIDS: Psychiatry's role in a changing epidemic. Journal of the American Academy of Child Adolescent Psychiatry. 2005;44(8):728–747. doi: 10.1097/01.chi.0000166381.68392.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dworkin S, Pinto RM, Hunter J, Rapkin B, Remien R. Keeping the spirit of community partnerships alive in the scale up of HIV/AIDS prevention: Critical reflections on the roll-out of DEBI (Diffusion of Effective Behavioral Interventions) American Journal of Community Psychology. 2008;42(1-2):51–59. doi: 10.1007/s10464-008-9183-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton DK, Kann L, Kinchen S, Ross J, Hawkins J, Harris WA, et al. Youth risk behavior surveillance—United States, 2005. Journal of School Health. 2006;76(7):353–62. doi: 10.1111/j.1746-1561.2006.00127.x. [DOI] [PubMed] [Google Scholar]
- Elkington KS, Bauermeister JA, Brackis-Cott E, Dolezal C, Mellins CA. Substance use and sexual risk behaviors in perinatally human immunodeficiency virus-exposed youth: The role of caregivers, peers and HIV Status. Journal of Adolescent Health. 2009;45(2):133–1. doi: 10.1016/j.jadohealth.2009.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elkington KS, Teplin LA, Mericle AA, Welty LJ, Romero EG, Abram KM. HIV/STI risk behaviors in delinquent youth with psychiatric disorders: A longitudinal study. Journal of the American Academy of Child and Adolescent Psychiatry. 2008;47(8):901–911. doi: 10.1097/CHI.0b013e318179962b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellickson PL, McCaffrey DF, Klein DJ. Long-term effects of drug prevention of risky sexual behavior among young adults. Journal of Adolescent Health. 2009;45:111–117. doi: 10.1016/j.jadohealth.2008.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fergus S, Zimmerman MA. Adolescent resilience: A framework for understanding healthy development in the face of risk. Annual Review of Public Health. 2005;26:399–419. doi: 10.1146/annurev.publhealth.26.021304.144357. [DOI] [PubMed] [Google Scholar]
- Gordon CM, Carey MP, Carey KB. Effects of a drinking event on behavioral skills and condom attitudes in men: Implications for HIV risk from a controlled experiment. Health Psychology. 1997;16:490–495. doi: 10.1037//0278-6133.16.5.490. [DOI] [PubMed] [Google Scholar]
- Gotlib I, Lewinsohn P, Seeley J. Symptoms versus a diagnosis of depression: Differences in psychosocial functioning. Journal of Consulting and Clinical Psychology. 1995;63(1):90–100. doi: 10.1037//0022-006x.63.1.90. [DOI] [PubMed] [Google Scholar]
- Graves KL, Leigh BC. The relationship of substance use to sexual activity among young adults in the United States. Family Planning Perspectives. 1995;27(1):18–22. [PubMed] [Google Scholar]
- Greene JM, Ennett ST, Ringwalt CL. Prevalence and correlates of survival sex among runaway and homeless youth. American Journal of Public Health. 1999;89(9):1406–1409. doi: 10.2105/ajph.89.9.1406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo J, Chung IJ, Hill KG, Hawkins JD, Catalano RF, Abbott RD. Developmental relationships between adolescent substance use and risky sexual behavior in young adulthood. Journal of Adolescent Health. 2002;31(4):354–362. doi: 10.1016/s1054-139x(02)00402-0. [DOI] [PubMed] [Google Scholar]
- Hamilton EB, Asarnow JR, Tompson MC. Family interaction styles of children with depressive disorders, schizophrenia-spectrum disorders, and normal controls. Family Process. 1999;38(4):463–476. doi: 10.1111/j.1545-5300.1999.00463.x. [DOI] [PubMed] [Google Scholar]
- Houck CD, Lescano CM, Brown LK, Tolou-Shams M, Thompson J, DiClemente R, et al. “Islands of risk”: Subgroups of adolescents at risk for HIV. Journal of Pediatric Psychology. 2006;31(6):619–629. doi: 10.1093/jpepsy/jsj067. [DOI] [PubMed] [Google Scholar]
- Jessor R. Risk behavior in adolescence: a psychosocial framework for action. Journal of Adolescent Health. 1991;12(8):597–605. doi: 10.1016/1054-139x(91)90007-k. [DOI] [PubMed] [Google Scholar]
- Kandel DB, Johnson JG, Bird HR, Canino G, Goodman SH, Lahey BB, et al. Psychiatric disorders associated with substance use among children and adolescents: Findings from the methods for the epidemiology of child and adolescent mental disorders (MECA) study. Journal of Abnormal Child Psychiatry. 1997;25(2):121–132. doi: 10.1023/a:1025779412167. [DOI] [PubMed] [Google Scholar]
- Kandel DB, Yamaguchi K, Chen K. Stages of progression in drug involvement from adolescence to adulthood: Further evidence for the gateway theory. Journal of Studies on Alcohol. 1992;53(5):447–457. doi: 10.15288/jsa.1992.53.447. [DOI] [PubMed] [Google Scholar]
- Kelder SH, Murray NG, Orpinas P, Prokhorov A, McReynolds L, Zhang Q, et al. Depression and substance use in minority middle-school students. American Journal of Public Health. 2001;91(5):761–766. doi: 10.2105/ajph.91.5.761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC. The Epidemiology of Dual Diagnosis. Biological Psychiatry. 2004;56(10):730–737. doi: 10.1016/j.biopsych.2004.06.034. [DOI] [PubMed] [Google Scholar]
- Kessler R, Avenevoli S, Merikangas K. Mood disorders in children and adolescents: An epidemiologic perspective. Biological Psychiatry. 2001;49(12):1002–1014. doi: 10.1016/s0006-3223(01)01129-5. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, et al. The epidemiology of major depressive disorder. Journal of the American Medical Association. 2003;289(3):3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- Krull JL, MacKinnon DP. Multilevel mediation modeling in group-based intervention studies. Evaluation Review. 1999;23(4):418–444. doi: 10.1177/0193841X9902300404. [DOI] [PubMed] [Google Scholar]
- LaBrie J, Earlywine M, Schiffman J, Pedersen E, Marriot C. Effects of alcohol, expectancies, and partner type on condom use in college males: Event-level analyses. Journal of Sex Research. 2005;42:259–266. doi: 10.1080/00224490509552280. [DOI] [PubMed] [Google Scholar]
- Lehrer JA, Shrier LA, Gortmaker S, Buka S. Depressive Symptoms as a longitudinal predictor of sexual risk behaviors among US middle and high school students. Pediatrics. 2006;118(1):189–200. doi: 10.1542/peds.2005-1320. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Gotlib IH, Seeley JR. Adolescent psychopathology, IV: Specificity of psychosocial risk factors for depression and substance abuse in older adolescents. Journal of the American Academy of Child Adolescent Psychiatry. 1995;34(9):1221–1229. doi: 10.1097/00004583-199509000-00021. [DOI] [PubMed] [Google Scholar]
- Lewinsohn P, Solomon A, Seeley J, Zeiss A. Clinical implications of “subthreshold” depressive symptoms. Journal of Abnormal Psychology. 2000;109(2):345–351. [PubMed] [Google Scholar]
- Locke TF, Newcomb MD. Alcohol involvement and dysphoria: A longitudinal examination of gender differences from late adolescence to adulthood. Psychology of Addictive Behaviors. 2001;15:227–236. [PubMed] [Google Scholar]
- Logan TK, Cole J, Leukefeld C. Women, sex, and HIV: Social and contextual factors, meta-analysis of published interventions, and implications for practice and research. Psychological Bulletin. 2002;128(6):851–885. doi: 10.1037/0033-2909.128.6.851. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Warsi G, Dwyer JH. A simulation study of mediated effect measures. Multivariate Behavioral Research. 1995a;30:41–62. doi: 10.1207/s15327906mbr3001_3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Warsi G, Dwyer JH. A simulation study of mediated effect measures: Erratum. Multivariate Behavioral Research. 1995b;30(3):ii. doi: 10.1207/s15327906mbr3001_3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McFarlane AH, Bellissimo A, Norman GR. The role of family and peers in social efficacy: links to depression in adolescence. American Journal of Orthopsychiatry. 1995;63:402–410. doi: 10.1037/h0079655. [DOI] [PubMed] [Google Scholar]
- McKinnon K. Sexual and Drug-Use Risk Behavior. In: Cournos F, Bakalar N, editors. AIDS and People with Severe Mental Illness: A Handbook for Mental Health Professionals. New Haven, CT: Yale University Press; 1996. pp. 17–46. [Google Scholar]
- Marston C, King E. Factors that shape young people's sexual behavior: A systematic review. Lancet. 2006;368:1581–1586. doi: 10.1016/S0140-6736(06)69662-1. [DOI] [PubMed] [Google Scholar]
- Mellins CA, Elkington KS, Bauermeister JA, Brackis-Cott E, Dolezal C, McKay M, et al. Sexual and drug use behavior in perinatally-HIV-infected youth: Mental health and family influences. Journal of the American Academy of Child and Adolescent Psychiatry. 2009;48(8):810–819. doi: 10.1097/CHI.0b013e3181a81346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakao K, Treas J. Updating occupational prestige and socioeconomic scores: How the new measures measure up. Sociological Methodology. 1994;24:1–72. [Google Scholar]
- O'Hare T. Risky sex and drinking contexts in freshman first offenders. Addictive Behaviors. 2005;30(3):585–588. doi: 10.1016/j.addbeh.2004.07.002. [DOI] [PubMed] [Google Scholar]
- Oshri A, Tubman JG, Wagner EF, Leon-Morris S, Snyders J. Psychiatric symptom patterns, proximal risk factors, and sexual risk behaviors among youth in outpatient substance abuse treatment. American Journal of Orthopsychiatry. 2008;78(4):430–441. doi: 10.1037/a0014326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ott M, Millstein S, Halpern-Felsher B. Positive Motivations for Sex among Male and Female Teens. Paper presented at the Annual Meeting of the Society for Adolescent Medicine; St. Louis, MO. 2004. [Google Scholar]
- Petersen AC, Compas BE, Brooks-Gunn J, Stemmler M, Ey S, Grant KE. Depression in adolescence. American Psychologist. 1993;48(2):155–178. doi: 10.1037//0003-066x.48.2.155. [DOI] [PubMed] [Google Scholar]
- Pine D, Cohen E, Cohen P, Brook J. Adolescent depressive symptoms as predictors of adult depression: Moodiness or mood disorder? American Journal of Psychiatry. 1999;156:133–135. doi: 10.1176/ajp.156.1.133. [DOI] [PubMed] [Google Scholar]
- Ramirez-Valles J, Zimmerman MA, Newcomb MD. Sexual risk behavior among youth: Modeling the influence of prosocial activities and socioeconomic factors. Journal of Health and Social Behavior. 1998;39:237–253. [PubMed] [Google Scholar]
- Ramrakha S, Caspi A, Dickson N, Moffitt TE, Paul C. Psychiatric disorders and risky sexual behaviour in young adulthood: Cross sectional study in birth cohort. British Medical Journal. 2000;321:263–266. doi: 10.1136/bmj.321.7256.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raudenbush S, Bryk A. Hierarchical Linear Models: Applications and data analysis methods. Second. Thousand Oaks, California: Sage Publications; 2002. [Google Scholar]
- Rogers JL. Sexual transitions in adolescence. In: Graber JA, Brooks-Gunn J, Peterson AC, editors. Transitions Through Adolescence: Interpersonal Domains and Context. Mahwah, NJ: Erlbaum; 1996. pp. 85–110. [Google Scholar]
- Rosenthal D, Moore S, Flynn I. Adolescent self-efficacy, self-esteem, and sexual risk-taking. Journal of Community and Applied Social Psychology. 1991;1(2):77–88. [Google Scholar]
- Rubin AG, Gold DO, Primack BA. Associations between depressive symptoms and sexual risk behavior in a diverse sample of female adolescents. Journal of Pediatric and Adolescent Gynocology. doi: 10.1016/j.jpag.2008.12.011. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salazar LF, DiClemente RJ, Wingood GM, Crosby RA, Harrington K, Davies S, Hook EW, Oh MK. Self-concept and adolescents' refusal of unprotected sex: A test of mediating mechanisms among African American girls. Prevention Science. 2004;5(3):137–149. doi: 10.1023/b:prev.0000037638.20810.01. [DOI] [PubMed] [Google Scholar]
- Sanderson C, Cantor N. Social dating goals in late adolescence: Implications for safer sexual activity. Journal of Personality and Social Psychology. 1995;68:1121–1134. doi: 10.1037//0022-3514.68.6.1121. [DOI] [PubMed] [Google Scholar]
- Scientific Software International. Hierarchical Linear Models. Chicago, IL: SSI Inc; 2009. [Google Scholar]
- Seal A, Minichiello V, Omodei M. Young women's sexual risk taking behaviour: Revisiting the influences of sexual self-efficacy and sexual self-esteem. International Journal of STD & AIDS. 1997;8:159–165. doi: 10.1258/0956462971919822. [DOI] [PubMed] [Google Scholar]
- Shrier L, Harris S, Beardslee W. Temporal associations between depressive symptoms and self-reported sexually transmitted disease among adolescents. Archives of Pediatric and Adolescent Medicine. 2002;156(6):599–606. doi: 10.1001/archpedi.156.6.599. [DOI] [PubMed] [Google Scholar]
- Shrier LA, Harris SK, Sternberg M, Beardslee WR. Associations of depression, self-esteem, and substance use with sexual risk among adolescents. Preventative Medicine. 2001;33(3):179–89. doi: 10.1006/pmed.2001.0869. [DOI] [PubMed] [Google Scholar]
- Smith MD. HIV Risk in Adolescents with Severe Mental Illness: Literature Review. Journal of Adolescent Health. 2001;29:320–329. doi: 10.1016/s1054-139x(01)00265-8. [DOI] [PubMed] [Google Scholar]
- Stiffman AR, Dore P, Earls F, Cunningham R. The influence of mental health problems on AIDS-related risk behaviors in young adults. Journal of Nervous and Mental Disease. 1992;180(5):314–320. doi: 10.1097/00005053-199205000-00005. [DOI] [PubMed] [Google Scholar]
- Stoner SA, George WH, Peters LM, Norris J. Liquid Courage: Alcohol Fosters Risky Sexual Decision-Making in Individuals with Sexual Fears. AIDS and Behavior. 2007;11:227–237. doi: 10.1007/s10461-006-9137-z. [DOI] [PubMed] [Google Scholar]
- Tapert SF, Aarons GA, Sedlar GR, Brown SA. Adolescent Substance Use and Sexual Risk-Taking Behavior. Journal of Adolescent Health. 2001;28(3):181–189. doi: 10.1016/s1054-139x(00)00169-5. [DOI] [PubMed] [Google Scholar]
- Teplin LA, Elkington KS, McClelland GM, Abram KM, Mericle AA, Washburn JJ. Major mental disorders, substance use disorders, comorbidity, and HIV-AIDS risk behaviors in juvenile detainees. Psychiatric Services. 2005;56:823–828. doi: 10.1176/appi.ps.56.7.823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tolou-Shams M, Brown LK, Houck C, Lescano CM. The association between depressive symptoms, substance use, and HIV risk among youth with an arrest history. Journal of Studies on Alcohol and Drugs. 2008;69(1):58–64. doi: 10.15288/jsad.2008.69.58. [DOI] [PubMed] [Google Scholar]
- Tolou-Shams M, Paikoff RL, McKirnan DJ, Holmbeck GN. Mental health and HIV risk among African American adolescents: the role of parenting. Social Work in Mental Health. 2007;5(1-2):27–58. [Google Scholar]
- Tubman J, Windle M, Windle R. The onset and cross-temporal patterning of sexual intercourse in middle adolescence: Prospective relations with behavioral and emotional problems. Child Development. 1996;67(2):327–343. [PubMed] [Google Scholar]