Abstract
We aimed to examine longitudinal associations between family dinner and disordered eating behaviors among adolescents. We studied 7535 females and 5913 males, 9 to 14 years of age in 1996. We performed multivariable logistic regression to assess the associations of previous year family dinner with 1-year incidence of each of 3 outcomes: purging, binge eating, and frequent dieting. Compared to those who ate family dinner “never or some days,” female adolescents who ate family dinner at least most days were less likely to initiate purging, binge eating, and frequent dieting. Estimates of association among males were similar in direction and magnitude, although lower frequency of the outcomes resulted in less precise estimates and fewer statistically significant results.
INTRODUCTION
Disordered eating behaviors, including vomiting, laxative use, binge eating, and frequent dieting are prevalent among adolescent females (D. M. Ackard, Neumark-Sztainer, Story, & Perry, 2003; Eaton, et al., 2006). These behaviors are of public health concern due to their association with adverse physical and psychological outcomes, including depressive symptoms (Johnson, Cohen, Kasen, & Brook, 2002), and the onset of obesity (Field, et al., 2003; Neumark-Sztainer, et al., 2006; Stice, Presnell, Shaw, & Rohde, 2005) and eating disorders (G. C. Patton, Selzer, Coffey, Carlin, & Wolfe, 1999; Santonastaso, Friederici, & Favaro, 1999).
Results from retrospective (D. Ackard & Neumark-Sztainer, 2001) and cross-sectional studies (Fulkerson, et al., 2006; Neumark-Sztainer, Wall, Story, & Fulkerson, 2004) suggest that adolescents who report more frequent family meals may be less likely to engage in disordered eating behaviors. However, the retrospective study may be limited by differential recall of frequency of family meals between adolescents with and without disordered eating behavior, and the cross-sectional studies cannot rule out reverse causality, i.e., that disordered eating behavior could lead to less frequent family dinners.
A single prospective study has examined the association between family meals and disordered eating. Among 2516 adolescents residing in Minnesota, Neumark-Sztainer et al. (Neumark-Sztainer, Eisenberg, Fulkerson, Story, & Larson, 2008) found that regular family meals were associated with lower prevalences of disordered eating among females. Among males, regular family meals were associated with higher prevalences of disordered eating behaviors, which was unanticipated. The authors suggested that further exploration of the association between family meals and disordered eating behaviors, particularly among males, is warranted.
An additional gap in our understanding is whether the associations between family meals and disordered eating behaviors are moderated by familial weight-related norms or behaviors. Previous studies examining the association between family meals and disordered eating have adjusted for family-level variables, such as parental connectedness and parental encouragement to diet (Neumark-Sztainer, et al., 2008), but none have examined how the association may be moderated by these family-level variables. Given the evidence showing that parental behaviors, such as parental role modeling of disordered eating (Field, et al., 2008; Hill, Weaver, & Blundell, 1990; Levine, Smolak, Moodey, Shuman, & Hessen, 1994) and parental comments to the child about their weight (Schreiber, et al., 1996; Smolak, Levine, & Schermer, 1999), have a strong influence on disordered eating risk among adolescents, it is possible that, among families in which parents are dieting, or the adolescent’s thinness is extremely important to parents, or the parents make negative comments to the child about their weight, more frequent family meals may be too weak an influence to overcome the parents’ attitude or behaviors.
Our primary aim was to examine the longitudinal associations between frequency of family dinners and disordered eating behaviors in a nationwide sample of over 13,000 male and female adolescents. We hypothesized that more frequent family dinners would be inversely associated with the onset of purging, binge eating, and dieting behaviors among both female and male adolescents. Although the previous longitudinal study found that more frequent family meals were associated with increased prevalence of disordered eating behaviors among males, this finding was unanticipated and the authors were unable to explain why the findings were counter to their hypothesis (Neumark-Sztainer, et al., 2008). It is possible this finding may have been due to chance, thus we hypothesized that family meals would be inversely associated with the onset of disordered eating behaviors among males.
Our secondary aims were to explore the extent to which the longitudinal associations between family dinner frequency and disordered eating behaviors are moderated by adolescent perceptions of a) importance of adolescent’s thinness to parents, b) frequency of parental comments to child about their weight (parental weight teasing), or c) maternal dieting behaviors. Based on the evidence suggesting the strong influence that parental weight-related behaviors and concerns have on adolescent disordered eating risk (e.g., (Field, et al., 2008; Smolak, et al., 1999)), we hypothesized that family dinners would have a weaker protective effect among adolescents who report that it is important to their parents that the adolescent be thin, who report a high level of parental weight teasing, or who report that their mothers frequently diet.
METHODS
Participants
The Growing Up Today Study (GUTS) is a longitudinal cohort study of adolescent girls and males residing throughout the United States. Participants are offspring of women taking part in the Nurses’ Health Study II, a prospective cohort of more than 116,000 female registered nurses. GUTS was designed to assess prospectively determinants of adolescent dietary intake, physical activity, inactivity, weight concerns and disordered eating behaviors. All data were collected by means of mailed self-administered questionnaires.
Details of initial recruitment are available elsewhere (Gillman, et al., 2001). The baseline 1996 sample included 8843 girls and 7696 males, age 9–14 years. At baseline in 1996, the mean (SD) age of participants was 11.9 (1.6) years and the mean (SD) BMI was 19.1 (3.5) kg/m2. The cohort was 93% non-Hispanic white, reflecting the race/ethnicity representation of their mothers, who are participants of the Nurses’ Health Study II. In 1997, 1998, and 1999, participants were mailed follow-up questionnaires. For the current analyses, we excluded 515 females and 798 males who did not return at least one follow-up questionnaire. We excluded 793 females and 985 males who were missing family dinner data or follow-up data on outcome behaviors (i.e., purging, binge eating, and frequent dieting). Thus, our final sample size was 7535 females and 5913 males. There were no substantial differences in exposure or outcome between excluded participants and the final sample. The Human Subjects Committee at Brigham and Women’s Hospital approved this study.
Instruments
Family dinner
Our exposure variable of interest was family dinner. On each GUTS questionnaire from 1996 through 1998, we asked the question, “How often do you sit down with other members of your family to eat dinner or supper?” Response categories to this question, which formed our exposure variables, were “never, some days, most days, and every day.” Because of the very low proportion (1%) of participants answering “never,” we grouped these participants with those reporting “some days” for our analyses.
Disordered eating behaviors
Our outcome variables of interest were purging behaviors, binge eating, and frequent dieting. We assessed these disordered eating behaviors on each GUTS questionnaire from 1996 to 1999 with questions adapted from the Youth Risk Behavior Surveillance System questionnaire (Kann, et al., 1996). We assessed purging with two questions, “During the past year, how often did you make yourself throw up to keep from gaining weight?” and “During the past year, how often did you take laxatives to keep from gaining weight?” We classified respondents as engaging in purging behavior if they reported doing either of these behaviors at least monthly.
We assessed binge eating with a two-part question. Participants first reported the frequency during the past year of eating “so much food in a short period of time that you would be embarrassed if others saw you (binge-eating or gorging).” Respondents who reported at least occasional episodes of overeating were directed to a follow-up question that asked whether “you felt out of control during these episodes, like you could not stop eating even if you wanted to stop.” We defined binge eating as eating a very large amount of food in a short amount of time at least monthly and feeling out of control during the eating episode. For these bulimic behaviors, binge eating and purging, we used a cut-off of monthly to define these behaviors as disordered based on previous research which has shown that subthreshold eating disorder cases who engage in these behaviors at least monthly are similar to full criteria cases in terms of eating disorder psychopathology and history of treatment seeking (Striegel-Moore, et al., 2000).
We assessed dieting with the question: “During the past year, how often did you diet to lose weight or to keep from gaining weight?” We categorized respondents as frequent dieters if they reported that they had dieted to lose or maintain weight at least weekly. This frequency of dieting behaviors has been shown to be associated with increased risk of disordered eating among adolescents (G C Patton, Johnson-Sabine, Wood, Mann, & Wakeling, 1990). All three disordered eating items, binge eating, purging, and dieting, have been validated in previous studies (Brener, Collins, Kann, Warren, & Williams, 1995; Field, Taylor, Celio, & Colditz, 2004).
Weight concern
We assessed weight concern using 3 items from the McKnight Risk Factor Survey (MRFS) (Shisslak, et al., 1999). Males are more likely than females to focus on wanting to increase muscle tone, rather than being thin (McCabe, Ricciardelli, & Finemore, 2002), thus, to make the MRFS questions appropriate for males, we replaced the questions on thinness with questions inquiring about the importance of not being fat or desiring not to be fat in the surveys sent to male participants.
Importance of thinness to parents
We considered adolescents’ thinness (females) or lack of fatness (males) to be important to parents if the adolescents reported that the degree of perceived importance to their mothers and/or fathers was “a lot” or “totally” in the past year on a 5-point scale ranging from “not at all” to “totally.”
Frequency of parental comments to child about their weight (parental weight teasing)
We considered parental weight teasing to be frequent if the adolescents reported that their mothers and/or fathers made comments about their weight or eating that made them feel bad “a lot” or “always” in the past year.
Maternal dieting
We considered mothers to be frequent dieters if the adolescents reported that their mothers had tried to lose weight “a lot” or “always” in the past year.
Body Mass Index (BMI)
Participants self-reported their height and weight, and we calculated BMI with the formula weight in kilograms divided by squared height in meters. Previous studies reported high validity for self-reported heights and weights in preadolescents (Shannon, Smiciklas-Wright, & Wang, 1991) and adolescents (Strauss, 1999). We calculated age- and gender-specific BMI z-scores based on 2000 Centers for Disease Control and Prevention standards (Kuczmarski, et al., 2000).
Other covariates
Participants reported their Tanner maturation stage in five categories of pubic hair development using a validated self-rating measure (Morris & Udry, 1980), and females reported whether/when their menstrual periods began. We calculated each child’s age from his or her birthdate and the date each questionnaire was returned.
Analyses
To study the effect of family dinner frequency in the past year (our predictor variable of interest) on incident disordered eating behaviors (Aim 1), we related the past year frequency of family dinner reported in 1996 to incident disordered eating behaviors from 1996 to 1997, family dinner frequency reported in 1997 to incident disordered eating from 1997 to 1998, and family dinner frequency reported in 1998 to incident disordered eating from 1998 to 1999. Thus, our effect estimates are pooled 1-year estimates. Because each participant could contribute up to three observations, the assumption of independent observations required by ordinary least squares (OLS) regression was not met, so we used logistic regression models with estimation by generalized estimating equations (GEE) and adjusted for clustered, non-independent observations among participants (Zeger & Liang, 1986). To ensure that we evaluated only incident, not prevalent cases, we excluded participants who reported engaging in the relevant outcome behavior (i.e., purging, binge eating, and frequent dieting) in previous years, i.e., if a participant reported purging at baseline in 1996 s/he was excluded from all analyses, if a participant reported purging in 1997, s/he was excluded from the 1997 to 1998 analyses and the 1998 to 1999 analyses, and if a participant reported purging in 1998 s/he was excluded from the 1998 to 1999 analyses.
All models were stratified by sex. In the final multivariable models, we included covariates that may be related to both frequency of family dinner and incidence of disordered eating behaviors, including age, Tanner maturation stage, BMI z-score, weight concerns, and for females, menstrual status. These multivariable models were used to estimate the odds of initiating each disordered eating behavior among those who ate dinner with their family on “most days” or “everyday” as compared to the referent group, who ate dinner with their family “never/some days.” We also calculated p for trend across family dinner categories using continuous family dinner coded as 1, 2, and 3.
To explore whether associations between frequency of family dinner and the onset of disordered eating behaviors were moderated, i.e., whether effect modification was present, by importance of thinness to parents, parental weight teasing, and maternal dieting (Aim 2), we ran multivariable models stratified on each of these variables as well as models with the following interaction terms: a) family dinner × importance of thinness to parents, b) family dinner × parental weight teasing, and c) and family dinner × maternal dieting. We also explored whether associations between frequency of family dinner and onset of disordered eating were moderated by age (<13 years vs. ≥13 years in 1996) and weight status (BMI <85th percentile vs. ≥85th percentile for age and gender), based on previous analyses with this cohort that show that estimates of association for various predictors of disordered eating may differ by these factors (Field, et al., 2008). We performed all analyses using SAS version 9.1 (SAS Institute, Cary, NC).
RESULTS
Family dinner
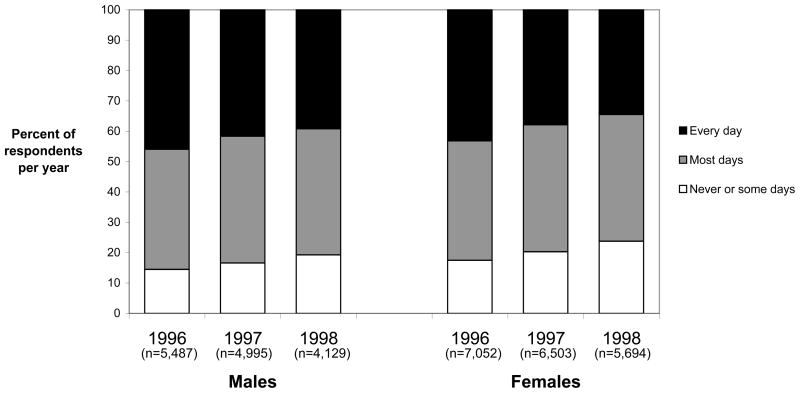
At baseline in 1996, 17.5% of females and 14.5% of males ate dinner with members of their family “never or some days,” 39.4% of females and 39.6% of males ate dinner with their family on “most days,” and 43.2% of females and 46.0% of males ate dinner with their family “every day.” Frequency of eating family dinner was lower in later years (Figure 1). In 1998, 34.5% of females and 39.2% of males reported eating family dinner “every day.”
Figure 1.
Frequency of family dinner consumption among Growing Up Today Study participants, by year and sex
Family dinner and purging
During the three years of follow-up (1997–1999), 1.3% (n = 224) of females and 0.3% (n = 43) of males started to purge. As shown in Table 2, among females, more frequent family meals in the previous year were associated with lower 1-year incidence of purging behavior. Compared with females who ate family dinner “never or some days,” the multivariable adjusted OR for females who ate family dinner on “most days” was 0.67 (95% CI, 0.48, 0.93), and it was 0.70 (95% CI, 0.50, 1.00) for females who ate family dinner “every day.”
Table 2.
ORs (95% CI) of one-year incidence of disordered eating behaviors associated with past year frequency of eating family dinner in the Growing Up Today Study (33,860 observations for 13,448 participants*)
| Purging | Binge Eating | Frequent Dieting | ||||
|---|---|---|---|---|---|---|
| Model 1† | Model 2†† | Model 1† | Model 2†† | Model 1† | Model 2†† | |
| FEMALES | ||||||
| OR (95%CI) | ||||||
| Never or some days | 1.0 (ref) | 1.0 (ref) | 1.0 (ref) | 1.0 (ref) | 1.0 (ref) | 1.0 (ref) |
| Most days | 0.53 (0.39, 0.73) | 0.67 (0.48, 0.93) | 0.70 (0.59, 0.85) | 0.82 (0.68, 0.99) | 0.72 (0.61, 0.84) | 0.87 (0.73, 1.03) |
| Every day | 0.44 (0.32,0.62) | 0.70 (0.50, 1.00) | 0.58 (0.48, 0.70) | 0.73 (0.59, 0.89) | 0.58 (0.49, 0.68) | 0.76 (0.64, 0.92) |
| Trend p | <0.01 | 0.06 | <0.01 | <0.01 | <0.01 | <0.01 |
| MALES | ||||||
| OR (95%CI) | ||||||
| Never or some days | 1.0 (ref) | 1.0 (ref) | 1.0 (ref) | 1.0 (ref) | 1.0 (ref) | 1.0 (ref) |
| Most days | 0.47 (0.22, 1.01) | 0.55 (0.26, 1.18) | 0.55 (0.38, 0.79) | 0.66 (0.45, 0.97) | 0.63 (0.47, 0.83) | 0.76 (0.56, 1.04) |
| Every day | 0.53 (0.25, 1.12) | 0.56 (0.25, 1.24) | 0.57 (0.40, 0.81) | 0.71 (0.48, 1.03) | 0.62 (0.47, 0.81) | 0.81 (0.60, 1.10) |
| Trend p | 0.21 | 0.22 | 0.01 | 0.16 | <0.01 | 0.31 |
Numbers differ slightly for each model
Model 1 Unadjusted
Model 2 includes age, Tanner stage, menarchal status for females only, BMI z-score, weight concerns
We found that the direction and magnitude of the estimates of association between family meal frequency and purging behaviors were similar among males, although the smaller number of outcomes led to wider CI’s and results that were not statistically significant (Table 2).
Family dinner and binge eating
From 1997 to 1999, 4.4% (n= 760) of females and 1.5% (n= 203) of males started to binge eat. As with purging, among females, we found that more frequent family meals in the previous year were associated with lower 1-year incidence of binge eating. Compared with females who ate family dinner “never or some days,” the multivariable adjusted OR for females who ate family dinner on “most days” was 0.82 (95% CI 0.68, 0.99), and it was 0.73 (95% CI 0.59, 0.89) for females who ate family dinner “every day.”
Among males, we also found that more frequent family meals in the previous year were associated with lower 1-year incidence of binge eating. Compared with males who ate family dinner “never or some days,” the multivariable adjusted OR for males who ate family dinner on “most days” was 0.66 (95% CI 0.45, 0.97), and it was 0.71 (95% CI 0.48, 1.03) for males who ate family dinner “every day” (Table 2).
Family dinner and frequent dieting
From 1997 to 1999, 6.5% (n = 1051) of females and 2.8% (n = 357) of males began to diet frequently. As with the previous disordered eating behaviors examined, we found that more frequent family dinner was associated with lower 1-year incidence of dieting. Compared with females who ate family dinner “never or some days,” the multivariable adjusted OR for females who ate family dinner on “most days” was 0.87 (95% CI 0.73, 1.03), and it was 0.76 (95% CI 0.64, 0.92) for females who ate family dinner “every day.”
We found that the direction and magnitude of the estimates of association between family meal frequency and dieting were similar among males, although the smaller number of outcomes led to wider CI’s and results that were not statistically significant (Table 2).
Effect modification by age, weight status, and parental factors
Among female adolescents, we found some evidence of effect modification by age for the association between family dinners and binge eating. Among females 8–12 years of age we found that, compared to their similarly-aged peers who ate family dinner “never or some days,” the multivariable adjusted OR for females who ate family dinner on “most days” was 0.81 (95% CI 0.63,1.05) and it was 0.63 (95% CI 0.48, 0.82) among those who ate family dinner “every day.” Among females who were 13 years of age and older, we found that, compared to females who ate dinner “never or some days,” the adjusted OR for females who ate family dinner on “most days” was 0.72 (95% CI 0.53., 0.99) and it was 0.90 (95% CI 0.65, 1.24) among those that ate family dinner “every day” (p for test for interaction = 0.03). We did not find evidence of effect modification by age for the association between family dinner and purging and frequent dieting among females. Among males, we did not find evidence of effect modification by age for any of the associations explored.
Among males, we found some evidence of effect modification by weight status for the association between family dinner and frequent dieting. Among males with a BMI <85th percentile for age and gender, we found that, compared to those who ate family dinner “never or some days,” the multivariable adjusted OR for males who ate family dinner “most days” was 0.73 (95% CI 0.45, 1.20) and it was 0.55 (95% CI 0.33, 0.93) among those who ate family dinner “every day.” Among males with a BMI ≥85th percentile for age and gender, we found that, compared to those who ate family dinner “never or some days,” the adjusted OR was 0.74 (95% CI 0.49, 1.10) and it was 0.98 (95% CI, 0.66, 1.45) among those who ate family dinner “every day” (p for test for interaction = 0.03).
Overall, we did not find any strong evidence that the associations were modified by the three parental variables we explored: importance of adolescent’s thinness to parents, frequency of parental comments to child about their weight, and maternal dieting behaviors. We also re-ran our multivariable regression models to include these parental variables as covariates and found that our results were essentially unchanged (results not shown).
DISCUSSION
In this prospective study of over 13,000 preadolescents and adolescents, we found that female youth who ate dinner with members of their family most days or every day of the week were less likely to initiate purging behaviors, binge eating, and frequent dieting in the following year. These associations were independent of age, Tanner maturation stage, BMI z-score, weight concerns, and menstrual status. Estimates of association among male youth were similar in direction and magnitude, although the lower frequency of the outcomes resulted in less precise estimates that were not statistically significant.
One way that eating family dinner may protect against disordered eating behaviors is that eating family dinner together may encourage more regular meal consumption, which may prevent disordered eating behaviors, in particular binge eating (Masheb & Grilo, 2006). Another possible explanation is that eating meals together may help enhance the quality of parent-child relationships, in particular parent-child communication and cohesion, which may reduce risk for engaging in these disordered behaviors (Bailey, 1991). Confounding may also explain our findings: it is possible that an unmeasured variable associated with both higher frequency of family dinner and lower incidence of disordered eating behavior accounts for the associations we found. Our effect estimates were attenuated with the addition of individual-level factors, such as weight concern and body mass, into the model suggesting that residual confounding by these variables is also possible.
Our results are in agreement with previous cross-sectional (Fulkerson, et al., 2006; Neumark-Sztainer, et al., 2004) and longitudinal (Neumark-Sztainer, et al., 2008) research which found an inverse association between family meals and disordered eating among adolescent females. Our finding of a potential protective influence of family meals among males is contrary to Neumark-Sztainer and colleagues’ (Neumark-Sztainer, et al., 2008) finding that regular family meals were associated with higher prevalences of disordered eating behaviors, such as fasting. Neumark-Sztainer et al., also found non-significant positive associations between regular family meals and binge eating and frequent dieting among males. One potential explanation for this variation is the different ages of the populations studied. The participants in the Neumark-Sztainer study were older than those included in our study (mean age 14.8 vs. 11.9 years). It is possible that family meals may offer benefit to preadolescent and early adolescent males, but that this protective influence does not hold among males in later adolescence. Additionally, the follow-up period in the Neumark-Sztainer study was substantially longer than in the present study (5 years vs. 1 year). Family meals may have a more proximal effect on disordered eating behaviors among males than would be detected with a 5-year follow-up.
Contrary to our hypotheses, we did not find that associations between family meals and disordered eating behaviors were moderated by the parental variables we explored. This finding may suggest that family dinners are protective for disordered eating behaviors among all adolescents, regardless of the weight-related norms and behaviors in their families. It is also possible that the association between family meals and disordered eating may be moderated by other important family-level variables, such as family functioning or parent-child communication, that were not assessed in this study.
One strength of the current analyses is the prospective study design, which allowed us to examine changes over time in family dinner frequency and disordered eating behaviors. Additionally, this study was sufficiently large to assess associations between family dinner and disordered eating behaviors separately for males and females stratified by various individual and family-level factors.
This study also had several limitations. Although the participants in this study reside throughout the United States, our cohort is not a representative sample of U.S. adolescents. Participants are children of registered nurses and the cohort is >90% white, which may reduce the generalizability of our findings. A second limitation was our inability to explore how the general family context, of the participants, e.g., family functioning and parent-child communication, influenced the association between family meals and disordered eating. While previous research has included variables, such as family connectedness, as covariates in analyses exploring these associations (Neumark-Sztainer, et al., 2008), additional research is needed to examine how the general family context may moderate the association between family meals and disordered eating. A third limitation was the necessity of collecting data on youth by self-report on mailed questionnaires. However, all three self-report outcome measures and the exposure have been previously validated (Brener, et al., 1995; Field, et al., 2004) and the resulting measurement error should be random. A final limitation of this study is that family meal frequency in GUTS was assessed from 1996–1998 only. However, more recent studies of family dinners or disordered eating behaviors have found similar prevalence rates for both family dinner (Videon & Manning, 2003; (Neumark-Sztainer, et al., 2008) and disordered eating behaviors (Eaton, et al., 2006), suggesting that the findings from this study may be generalizable to similar adolescent populations a decade later.
In summary, we found that youth who ate more frequent family meals were less likely to initiate disordered eating behaviors. Future research efforts in this area should focus on the mechanisms by which eating dinner with one’s family may protect against the initiation of disordered eating behaviors. Additionally, results from experimental research, such as family-based trials that can test if increasing family meals results in decreased disordered eating behaviors over time, are needed to provide stronger evidence of causality than can be achieved with prospective observational studies. Based on the results of this study, health professionals and community leaders working with families may support the efforts of family members to eat together as a means for preventing youth from engaging in disordered eating behaviors. Methods of support may include helping families plan their schedules to increase the frequency of family meals, identifying easy-to-prepare, healthful menu options for family meals, and advocating for adolescent activities to be held at times that do not conflict with the evening family meal.
Table 1.
Baseline characteristics in 1996 of preadolescents and adolescents in the Growing Up Today Study by sex
| Females (N=7052)* | Males (N=5487)* | |
|---|---|---|
| Mean (SD), n (%) | Mean (SD), n (%) | |
| Mean age, years (SD) | 11.9 (1.6) | 11.8 (1.5) |
| Mean body mass index, kg/m2 (SD) | 19.1 (3.6) | 19.2 (3.5) |
| Mean body mass index z score (unit) | 0.10 (1.0) | 0.25 (1.1) |
| Mean weight concern (SD) | 2.1 (1.1) | 1.6 (0.8) |
| Tanner stage (%)† | ||
| Stage 1 | 1466 (21.2%) | 1394 (26.2%) |
| Stage 2 | 1503 (21.7%) | 1561 (29.3%) |
| Stage 3 | 1188 (17.2%) | 1026 (19.3%) |
| Stage 4 | 1640 (23.7%) | 986 (18.5%) |
| Stage 5 | 1115 (16.1%) | 355 (6.7%) |
| Menstral status (% yes) | 2270 (32.4%) | NA |
total n differs slightly for each variable
Tanner stage of pubic hair development
NA, not applicable
SD, standard deviation
Acknowledgments
This study was supported by grants from the National Institutes of Health (DK46834, DK59570), the Kellogg Company, and the Canadian Institutes of Health Research (200510MFE-154556-10955).
References
- Ackard D, Neumark-Sztainer D. Family mealtime while growing up: Associations with symptoms of bulimia nervosa. Eating Disorders: The Journal of Treatment and Prevention. 2001;9:239–249. doi: 10.1080/10640260127551. [DOI] [PubMed] [Google Scholar]
- Ackard DM, Neumark-Sztainer D, Story M, Perry C. Overeating among adolescents: Prevalence and associations with weight-related characteristics and psychological health. Pediatrics. 2003;111(1):67–74. doi: 10.1542/peds.111.1.67. [DOI] [PubMed] [Google Scholar]
- Bailey CA. Family Structure and Eating Disorders: The Family Environment Scale and Bulimic-Like Symptoms. Youth and Society. 1991;23(2):251–272. [Google Scholar]
- Brener ND, Collins JL, Kann L, Warren CW, Williams BI. Reliability of the Youth Risk Behavior Survey Questionnaire. Am J Epidemiol. 1995;141(6):575–580. doi: 10.1093/oxfordjournals.aje.a117473. [DOI] [PubMed] [Google Scholar]
- Eaton DK, Kann L, Kinchen S, Ross J, Hawkins J, Harris WA, et al. Youth risk behavior surveillance--United States, 2005. MMWR Surveill Summ. 2006;55(5):1–108. [PubMed] [Google Scholar]
- Field AE, Austin SB, Taylor CB, Malspeis S, Rosner B, Rockett HR, et al. Relation between dieting and weight change among preadolescents and adolescents. Pediatrics. 2003;112(4):900–906. doi: 10.1542/peds.112.4.900. [DOI] [PubMed] [Google Scholar]
- Field AE, Javaras KM, Aneja P, Kitos N, Camargo CA, Jr, Taylor CB, et al. Family, peer, and media predictors of becoming eating disordered. Arch Pediatr Adolesc Med. 2008;162(6):574–579. doi: 10.1001/archpedi.162.6.574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field AE, Taylor CB, Celio A, Colditz GA. Comparison of self-report to interview assessment of bulimic behaviors among preadolescent and adolescent girls and boys. Int J Eat Disord. 2004;35(1):86–92. doi: 10.1002/eat.10220. [DOI] [PubMed] [Google Scholar]
- Fulkerson JA, Story M, Mellin A, Leffert N, Neumark-Sztainer D, French SA. Family dinner meal frequency and adolescent development: relationships with developmental assets and high-risk behaviors. J Adolesc Health. 2006;39(3):337–345. doi: 10.1016/j.jadohealth.2005.12.026. [DOI] [PubMed] [Google Scholar]
- Gillman MW, Rifas-Shiman SL, Camargo CA, Jr, Berkey CS, Frazier AL, Rockett HR, et al. Risk of overweight among adolescents who were breastfed as infants. Jama. 2001;285(19):2461–2467. doi: 10.1001/jama.285.19.2461. [DOI] [PubMed] [Google Scholar]
- Hill AJ, Weaver C, Blundell JE. Dieting concerns of 10-year-old girls and their mothers. British Journal of Clinical Psychology. 1990;29:346–348. doi: 10.1111/j.2044-8260.1990.tb00894.x. [DOI] [PubMed] [Google Scholar]
- Johnson JG, Cohen P, Kasen S, Brook JS. Childhood adversities associated with risk for eating disorders or weight problems during adolescence or early adulthood. Am J Psychiatry. 2002;159(3):394–400. doi: 10.1176/appi.ajp.159.3.394. [DOI] [PubMed] [Google Scholar]
- Kann L, Warren CW, Harris WA, Collins JL, Williams BI, Ross JG, et al. Youth Risk Behavior Surveillance--United States, 1995. Morbidity and Mortality Weekly Report. CDC Surveillance Summaries. 1996;45(4):1–84. [PubMed] [Google Scholar]
- Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, Flegal KM, Guo SS, Wei R, et al. CDC Growth Charts: United States. Advance Data, June. 2000;8(314):1–27. [PubMed] [Google Scholar]
- Levine MP, Smolak L, Moodey AF, Shuman MD, Hessen LD. Normative developmental challenges and dieting and eating disturbances in middle school girls. International Journal of Eating Disorders. 1994;15(1):11–20. doi: 10.1002/1098-108x(199401)15:1<11::aid-eat2260150103>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- Masheb RM, Grilo CM. Eating patterns and breakfast consumption in obese patients with binge eating disorder. Behav Res Ther. 2006;44(11):1545–1553. doi: 10.1016/j.brat.2005.10.013. [DOI] [PubMed] [Google Scholar]
- McCabe MP, Ricciardelli LA, Finemore J. The role of puberty, media and popularity with peers on strategies to increase weight, decrease weight and increase muscle tone among adolescent boys and girls. J Psychosom Res. 2002;52(3):145–153. doi: 10.1016/s0022-3999(01)00272-0. [DOI] [PubMed] [Google Scholar]
- Morris N, Udry J. Validation of a self-administered instrument to assess stage of adolescent development. Journal of Youth and Adolescence. 1980;9:271–280. doi: 10.1007/BF02088471. [DOI] [PubMed] [Google Scholar]
- Neumark-Sztainer D, Eisenberg ME, Fulkerson JA, Story M, Larson NI. Family meals and disordered eating in adolescents: longitudinal findings from project EAT. Arch Pediatr Adolesc Med. 2008;162(1):17–22. doi: 10.1001/archpediatrics.2007.9. [DOI] [PubMed] [Google Scholar]
- Neumark-Sztainer D, Wall M, Guo J, Story M, Haines J, Eisenberg M. Obesity, disordered eating, and eating disorders in a longitudinal study of adolescents: how do dieters fare 5 years later? J Am Diet Assoc. 2006;106(4):559–568. doi: 10.1016/j.jada.2006.01.003. [DOI] [PubMed] [Google Scholar]
- Neumark-Sztainer D, Wall M, Story M, Fulkerson JA. Are family meal patterns associated with disordered eating behaviors among adolescents? J Adolesc Health. 2004;35(5):350–359. doi: 10.1016/j.jadohealth.2004.01.004. [DOI] [PubMed] [Google Scholar]
- Patton GC, Johnson-Sabine E, Wood K, Mann AH, Wakeling A. Abnormal eating attitudes in London schoolgirls a prospective epidemiological study: Outcome at twelve-month follow-up. Psychological Medicine. 1990;20(2):383–394. doi: 10.1017/s0033291700017700. [DOI] [PubMed] [Google Scholar]
- Patton GC, Selzer R, Coffey C, Carlin JB, Wolfe R. Onset of adolescent eating disorders: population based cohort study over 3 years. BMJ. 1999;318(7186):765–768. doi: 10.1136/bmj.318.7186.765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santonastaso P, Friederici S, Favaro A. Full and partial syndromes in eating disorders: A 1-year prospective study of risk factors among female students. Psychopathology. 1999;32:50–56. doi: 10.1159/000029067. [DOI] [PubMed] [Google Scholar]
- Schreiber G, Robins M, Striegel-Moore R, Obarzanek E, Morrison J, Wright D. Weight modification efforts reported by Black and White preadolescent girls: National heart, lung, and blood institute growth and health study. Pediatrics. 1996;98:63–70. [PubMed] [Google Scholar]
- Shannon B, Smiciklas-Wright H, Wang MQ. Inaccuracies in self-reported weights and heights of a sample of sixth-grade children. J Am Diet Assoc. 1991;91(6):675–678. [PubMed] [Google Scholar]
- Shisslak CM, Renger R, Sharpe T, Crago M, McKnight KM, Gray N, et al. Development and evaluation of the McKnight Risk Factor Survey for assessing potential risk and protective factors for disordered eating in preadolescent and adolescent girls. Int J Eat Disord. 1999;25(2):195–214. doi: 10.1002/(sici)1098-108x(199903)25:2<195::aid-eat9>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- Smolak L, Levine MP, Schermer F. Parental input and weight concerns among elementary school children. International Journal of Eating Disorders. 1999;25:263–271. doi: 10.1002/(sici)1098-108x(199904)25:3<263::aid-eat3>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- Stice E, Presnell K, Shaw H, Rohde P. Psychological and behavioral risk factors for obesity onset in adolescent girls: a prospective study. J Consult Clin Psychol. 2005;73(2):195–202. doi: 10.1037/0022-006X.73.2.195. [DOI] [PubMed] [Google Scholar]
- Strauss RS. Comparison of measured and self-reported weight and height in a cross-sectional sample of young adolescents. Int J Obes Relat Metab Disord. 1999;23(8):904–908. doi: 10.1038/sj.ijo.0800971. [DOI] [PubMed] [Google Scholar]
- Striegel-Moore RH, Dohm FA, Solomon EE, Fairburn CG, Pike KM, Wilfley DE. Subthreshold binge eating disorder. Int J Eat Disord. 2000;27(3):270–278. doi: 10.1002/(sici)1098-108x(200004)27:3<270::aid-eat3>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42(1):121–130. [PubMed] [Google Scholar]