Abstract
This study was conducted to determine the psychometric properties of a measure of social support, the Community Assessment Inventory (CAI), and to examine the role of social support in recovery. The CAI and the Addiction Severity Index (ASI) were administered to 196 opioid-dependent adults in (n = 135) or out of methadone treatment (n = 61) in Baltimore, Maryland between 2004 and 2006. Baseline CAI scale scores indicated a generally high level of internal consistency (α scores). Pearson correlations showed that the scales were stable and had good discriminant validity with the ASI composite scores. One-way analysis of variance indicated that in-treatment participants reported significantly more support at baseline than out-of-treatment participants. This study's findings indicate the CAI may be a useful measure of social support and that such support is an important factor in treatment entry.
Keywords: Opioid addiction, social support, methadone maintenance, heroin addiction, treatment entry, treatment engagement
Introduction
Social support is considered important in the recovery of drug-addicted individuals, yet little is known regarding how such factors may influence treatment entry and engagement (1,2,3). Spouses, family members, peers, and neighborhood factors have been shown to play key roles in both an individual's addiction and also in his or her recovery (4,1,2,3). In spite of this finding, traditional drug treatment interventions have been criticized for focusing on the individual without taking into account the individual's environmental situation that may support or permit continued drug use (1). Thus, a key component of substance-abuse treatment should involve strengthening the individual's place in the community as a productive worker, family member, and community member (2,5,6).
Previous research has established that effective drug treatment may depend on the quality of an individual's interpersonal relationships (4,1,2,7). Individuals who report supportive and cohesive family relationships at treatment entry have reported fewer drug, family, and psychological problems three months after beginning treatment (8,2). Support from a relative or significant other at treatment entry has specifically been associated with lower heroin and alcohol use (9). Additional research has shown family support to be related to positive treatment outcomes (10,11), and that such support can influence recovery through motivation to change (12,13,14). Individuals may also experience fewer and less serious episodes of relapse when family is involved in treatment (2,3).
Peer relationships at treatment entry have also been found to be related to the course of drug treatment and recovery. The link between involvement with delinquent peer groups and engaging in delinquency has been consistently reported in previous research (15,16,17). In comparison with individuals who report fewer relationships with deviant peers, individuals who report more ties with deviant peers have been shown to have poorer treatment outcomes, especially if those peers are also drug users and less supportive of treatment (4,1,18). Although participants entering treatment are sometimes successful in severing ties with deviant peers, they often subsequently establish ties with new drug-using peers (19).
Finally, the level of neighborhood deviance may influence individuals' perceptions of how supportive their communities are of drug treatment and recovery (20). Communities that are characterized by higher rates of deviance – such as drug use and crime – often lack the informal social control structures that are essential for maintaining public order (21,22). Members of communities who may initially have an interest in maintaining social order may fear retribution from individuals engaging in and benefiting from criminal activity (i.e. selling drugs), and so are less willing to take a stand against drugs and violence in their community. These communities invite further drug use and criminal activity, as individuals perceive the residents of the communities as being indifferent to what takes place in the neighborhood (23,24,25).
In order to contribute to an understanding of the roles that social supports play in drug abuse treatment entry and engagement, this article examines perceived levels of support for opioid-addicted individuals both in and out of outpatient drug abuse treatment. The Community Assessment Inventory (CAI) (1) was administered to opioid-addicted individuals in Baltimore, Maryland to measure perceptions of support within their households, friends, families, and communities. Analyses focused on six research questions: 1) What are the relationships among the CAI scales at baseline in the total sample?; 2) What are the relationships between CAI scales at baseline and CAI scales at the 3-month assessment for the in-treatment group?; 3) What are the relationships between baseline CAI scales and baseline Addiction Severity Index (ASI) (26) composite scores in the total sample?; 4) Are there significant differences in levels of support at baseline between in- and out-of-treatment opioid-addicted individuals?; 5) What are the relationships between CAI scales at baseline and drug use and illegal activity at the 3-month follow-up for the in-treatment group?; and 6) Are there significant changes over time in perceived levels of support by individuals in treatment?
Methods
Participants
The sample consisted of 196 opioid-addicted individuals, including 135 participants newly enrolled in methadone treatment in Baltimore City and County and 61 participants neither enrolled in drug abuse treatment nor seeking such treatment. Eligibility for study entry for both groups required that participants were 18 years of age or older and met the criteria for methadone maintenance treatment at recruitment (i.e., at least one year of continuous opioid dependence). Furthermore, participants in the out-of-treatment group were only eligible for recruitment if they had not been in any type of drug treatment during the 12-month period preceding recruitment and were not interested in seeking treatment at time of recruitment.
Procedures
In-treatment participants were recruited from one of six Baltimore area methadone maintenance treatment programs and completed a baseline interview within one week following admission. Participants in the in-treatment group were interviewed again three months following treatment entry, regardless of whether they were still attending treatment.
Out-of-treatment participants were recruited from one of twelve street locations in Baltimore City chosen through targeted sampling methods (27,28,29,30). A screening form, created by study ethnographers, was administered to potential out-of-treatment participants to ensure that eligibility requirements for participation were met. There was no scheduled 3-month follow-up interview with the out-of-treatment sample. All participants provided informed consent in keeping with the Friends Research Institute's Institutional Review Board approval of this study.
Measures
Community Assessment Inventory (1)
The CAI measures individuals' perceptions of level of support in four domains: household members, which may include spouse or partner and/or adult relatives; family outside the home; friends; and community (1). Each scale includes 6 to 13 four-point Likert-type questions: “strongly agree”; “agree”; “disagree”; or “strongly disagree”. Because some sources of support were not available to all participants in the study, participants were instructed to skip questions relating to any inapplicable domain.
Items in each of the four areas of social support were summed to create the four scale scores, with lower scores indicating less support and higher scores indicating greater support. Scoring for analysis in this study was consistent with scoring in the original study conducted by the CAI developers (1), with one exception: items that inquired about current participation in drug treatment were omitted from the construction of scales for this study for analyses that included both the in- and out-of-treatment samples, as they were not applicable to and were not asked of out-of-treatment participants.
Addiction Severity Index (ASI.) (26)
The ASI measures current and lifetime functioning in seven different domains: alcohol use; drug use; medical; psychiatric; family/social; employment; and legal. Selected ASI items, based on the last 30 days only, are combined within each domain to create composite scores ranging from 0 (no problem) to 1 (extreme problem) (31,26). The instrument has been used extensively in substance-abuse studies and has been found to be valid and reliable (32,33,34).
In addition to ASI composite scores measured at baseline, several ASI items measured at three months post-study entry were included in the analyses. For example, the number of days that in-treatment participants used heroin, used cocaine, and engaged in illegal activity during the 30 days prior to the 3-month assessment were included as continuous variables.
Statistical Analyses
What are the relationships among the CAI scales at baseline in the total sample?
The psychometric properties of the CAI scales were investigated for the total sample. In order to measure the reliability of the four scales, coefficient α (35) was computed for each of the four baseline CAI scales. In addition, simple Pearson product-moment correlations among the four baseline CAI scale scores were calculated to examine their interrelationships in order to ascertain their degree of overlap.
What are the relationships between CAI scales at baseline and CAI scales at the 3-month assessment for the in-treatment group?
Simple Pearson product-moment correlations between CAI scale scores at baseline and CAI scale scores at the 3-month assessment were calculated for the in-treatment group in order to assess the stability of the CAI scales.
What are the relationships between baseline CAI scales and baseline Addiction Severity Index composite scores in the total sample?
Although we did not expect a relationship between these two measures, as a way to establish the discriminant validity of the CAI scales, we examined the relationships between each of the four CAI scales and the seven ASI composite scores. Simple Pearson product-moment correlations were calculated to assess the degree of overlap between the CAI scales and the ASI composite scores. Results should indicate modest relationships between the four CAI scales and the seven ASI composite scores in order to show good discriminant validity for the CAI scales.
Are there significant differences in levels of support at baseline between in- and out-of-treatment opioid-addicted individuals?
In addition to examining the measurement properties of the CAI scales, mean levels of baseline support were compared between in- and out-of-treatment groups. Any significant differences in support would contribute to an understanding of why individuals do or do not enter treatment. One-way analysis of variance (ANOVA) was used to determine differences in means on each of the four CAI scale scores between the in- and out-of-treatment groups.
What are the relationships between CAI scales at baseline and drug use and illegal activity at the 3-month follow-up for the in-treatment group?
To understand whether there is a relationship between early evidence of behavior change and perceptions of social support, simple Pearson correlations were calculated to determine the association between the four CAI scales at baseline and heroin use, cocaine use, and illegal activity at the 3-month assessment for the in-treatment group.
Are there significant changes over time in perceived levels of support by individuals in treatment?
To assess whether there are changes in perceptions of support over time, paired-sample t tests were utilized with CAI scale scores at baseline and 3-month follow-up for the in-treatment group.
Results
Sample Characteristics
Of the overall sample of 196 opioid-addicted individuals, 69% were in treatment and 31% were out of treatment at the baseline assessment (see Table 1). Sixty percent of the total sample was male, 74% was African American, and the mean age was 41 years old. Just over half the total sample had been employed at least part-time during most of the three years prior to the baseline interview. Regarding drug use, the mean number of lifetime years of heroin use was about 12½ years for the total sample, and 11 years of cocaine use for the 151 participants who had had any lifetime years of cocaine use. No significant differences were found on any demographic variables between the in- and out-of-treatment groups (all ps >.05).
Table 1.
Sample demographics
| Demographics | Total | In Treatment | Out of Treatment |
|---|---|---|---|
| N | 196 | 135 | 61 |
| Male % | 60 | 61 | 59 |
| Ethnicity % | |||
| African American | 74 | 72.6 | 77.0 |
| Caucasian | 25.5 | 26.7 | 23.0 |
| Native American | .5 | .7 | 0 |
| Mean age (SD) | 41.3 (8.0) | 41.0 (8.0) | 42.0 (7.9) |
| Heroin use (Lifetime) | |||
| N | 196 | 135 | 61 |
| Mean number of years (SD) | 12.6 (7.6) | 12.1 (7.3) | 13.7 (8.1) |
| Cocaine use (Lifetime) | |||
| N | 151 | 95 | 56 |
| Mean number of years for those who used (SD) | 11.08 (7.0) | 10.5 (6.6) | 12.1 (7.5) |
| Employment pattern past 3 years | |||
| Employed % | 51 | 49 | 51 |
Findings with regard to research questions
What are the relationships among the CAI scales at baseline in the total sample?
Similar to findings from the original study (1), internal consistency αs for the Household Members, Family, and Community scales ranged from.75 to.87, all within the acceptable range (see Table 2). The scale that assesses participants' perceptions of support from Friends, however, yielded a lower α at baseline (.56), compared with the α in the original study (.79). Correlations among the scales ranged from.16 to.56 (all ps <.05). However, these relationships were not so strong as to indicate major overlap between scales with the largest simple correlation of.56 between Friends and Family. As in the original study, the strongest relationships were found among the Household Members and Family and Friends scales, with weaker relationships found between the Community scale and the Household Members, Family, and Friends scales.
Table 2.
Descriptive statistics, internal consistency reliabilities (αs), and simple Pearson product-moment correlations between CAI scales at baseline in total sample
| Scales | Household (6 items) |
Family (8 items) |
Friends (7 items) |
Community (13 items) |
|---|---|---|---|---|
| Household | α=.87 (N=150) |
|||
| Family | .446** (N=131) |
α=.75 (N=166) |
||
| Friends | .322** (N=105) |
.557* (N=121) |
α=.56 (N=140) |
|
| Community | .169* (N=150) |
.156* (N=166) |
.202* (N=140) |
α=.77 (N=196) |
| Mean | 17.4 | 22.2 | 20.1 | 31.0 |
| SD | 4.2 | 4.2 | 3.0 | 5.8 |
p <.05.
p <.01.
What are the relationships between CAI scales at baseline and CAI scales at the 3-month assessment for the in-treatment group?
Simple Pearson product-moment correlations between each CAI scale score at baseline and its respective counterpart at three months were significant, as expected (see Table 3). Between-scale correlations across time were not significant, with two exceptions. The baseline Household Members and Friends scales significantly correlated with the 3-month Family scale (both ps <.01).
Table 3.
Simple Pearson product-moment correlations between CAI at baseline and CAI at 3-month follow-up for the in-treatment group
| Baseline CAI scales | ||||
|---|---|---|---|---|
| 3-Month CAI Scales | Household | Family | Friends | Community |
| Household | .308** (N=71) |
.164 (N=68) |
.193 (N=61) |
-.151 (N=78) |
| Family | .337** (N=73) |
.451** (N=78) |
.326** (N=64) |
-.076 (N=87) |
| Friends | .052 (N=62) |
.066 (N=68) |
.278* (N=66) |
-.021 (N=80) |
| Community | .044 (N=80) |
.051 (N=85) |
-.042 (N=76) |
.313** (N=101) |
p <.05.
p <.01.
What are the relationships between baseline CAI scales and baseline Addiction Severity Index composite scores in the total sample?
The baseline Household Members CAI scale correlated negatively and significantly with Alcohol, and positively and significantly with Medical composite scores. In addition, a small but significant negative relationship was found between the baseline Community scale and the ASI Alcohol composite score, as well as between the Community scale and the ASI Employment and Legal composite scores. Scales for Family and Friends showed no significant correlations with any of the ASI composite scores.
Are there significant differences in levels of support at baseline between in- and out-of-treatment opioid-addicted individuals?
Findings indicate that the in-treatment group perceives significantly (all ps <.005) more support at baseline than does the out-of-treatment group on all four CAI scales (see Figure 1). The largest difference between the two groups was found for the Community scale, with the in-treatment group showing a mean score of 32.4 (SD = 5.87) and the out-of-treatment group showing a mean score of 27.9 (SD = 4.13). The smallest difference between the two groups at baseline was found for the Friends scale, with the in-treatment group having a mean of 20.6 (SD = 2.88), and the out-of-treatment group having a mean of 19.1 (SD = 3.11).
Figure 1.
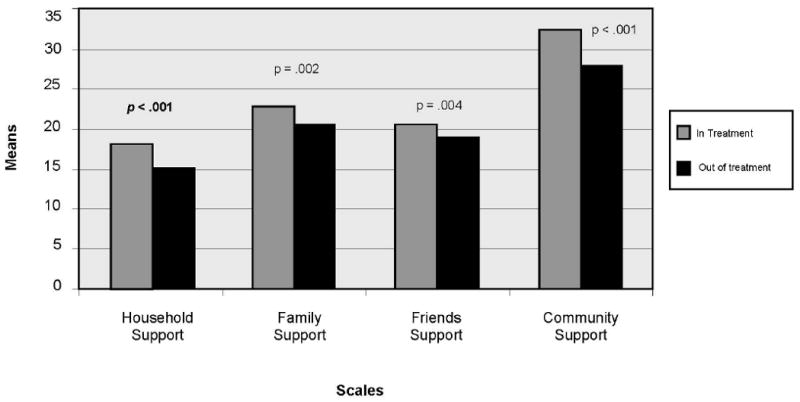
CAI scale means for in-treatment group vs. out-of-treatment group at baseline
What are the relationships between CAI scales at baseline and drug use and illegal activity at the 3-month follow-up for the in-treatment group?
Simple Pearson product-moment correlations indicated that the CAI baseline scales were negatively related to 3-month drug use and illegal activity for the in-treatment group (see Table 5), though none of these associations were significant (all ps >.05).
Table 5.
Simple Pearson product-moment correlations between baseline CAI scales and 3-month drug use and illegal activity in the in-treatment group
| Drug use and illegal activity | Household (N=80) |
Family (N=85) |
Friends (N=76) |
Community (N=101) |
|---|---|---|---|---|
| Days used (past 30 days) heroin at 3 months | -.138 | -.017 | -.102 | -.001 |
| Days used (past 30 days) cocaine at 3 months | -.042 | .040 | -.136 | -.030 |
| Whether used heroin (past 30 days) at 3 months | -.202 | -.106 | .-.014 | -.016 |
| Whether used cocaine (past 30 days) at 3 months | -.114 | -.099 | -.128 | -.114 |
| Days did illegal activity (past 30 days) at 3 months | -.084 | .020 | -.159 | -.048 |
Are there significant changes over time in perceived levels of support for individuals in treatment?
Analyses revealed that there were no significant changes in perceived support from baseline to 3-month follow-up for in-treatment participants (see Table 6), although there was a tendency toward increased support for the Friends scale (p =.089).
Table 6.
Paired samples t-tests comparing baseline CAI scales with 3-month CAI scales in the in-treatment sample
| Scales | n | Mean | SD | Mean difference | t | p | |
|---|---|---|---|---|---|---|---|
| Household | Baseline | 71 | 18.7 | 3.5 | .13 | .28 | .78 |
| 3-month | 71 | 18.6 | 3.0 | ||||
| Family | Baseline | 78 | 28.4 | 5.0 | -.60 | -1.07 | .29 |
| 3-month | 78 | 29.0 | 4.6 | ||||
| Friends | Baseline | 66 | 23.5 | 3.1 | -.71 | -1.73 | .09 |
| 3-month | 66 | 24.2 | 2.5 | ||||
| Community | Baseline | 101 | 32.2 | 5.5 | .12 | .20 | .85 |
| 3-month | 101 | 32.1 | 5.2 |
Discussion
Social factors have been found to be important in influencing entry into drug-addiction treatment, as well as for retention in treatment and ultimate recovery (1,2,3). Given these findings, Brown et al. (1) developed the Community Assessment Inventory, a 37-item self-report instrument that measures four potential sources of social support. The instrument was previously found to be both valid and reliable in a sample of 241 patients in a drug-free outpatient clinic in Baltimore. The current study of 196 opioid-addicted individuals both in and out of treatment in Baltimore provides further data on the CAI's psychometric properties, and also on its ability to distinguish between in- and out-of-treatment populations. This study also measures changes over time in perceived social support in a sample of methadone treatment patients.
In terms of its psychometric properties, three of the CAI's four scales showed acceptable internal consistency reliabilities. These findings are consistent with the results reported in the original study (1). However, the comparatively low α for the Friends support scale is not consistent with findings from the Brown et al. study. The moderate correlations among all four CAI scales show the scales to have good concurrent validity and that each scale measures a different source of support. Again, these findings are consistent with those found by researchers in the original study.
The modest correlations found between CAI scales and ASI composite scores suggest that the CAI scales have good discriminant validity. Few significant associations were found between CAI scale scores and ASI composite scores, all of which were small in magnitude. This finding suggests that the four constructs measured by the CAI scales are distinct from the seven constructs underlying the ASI composite scores. Moreover, results indicate that Household Members' support is significantly associated with less severe alcohol use, and Community support is significantly associated with less severe alcohol problems, employment problems, and legal issues. Thus, the more likely the home and neighborhood are seen as supportive of prosocial behaviors, the more likely individuals will be concerned with, and capable of maintaining those behaviors. Alternatively, it can be argued that as individuals adopt prosocial behaviors, they come to view the home and neighborhood as providing support for those behaviors. In either event, the perception of support from others can be seen as an important factor in the effort to encourage prosocial functioning.
An important finding in this study was that individuals who were in treatment, as compared with those who were out of treatment, perceived significantly greater support from their partners or family with whom they lived, family members outside the home, friends, and their communities at treatment entry. This finding is consistent with previous research illustrating that greater levels of support from family and friends are associated with treatment motivation (12,4,36,13,37,14). Further, 31% of all out-of-treatment participants responded that they lived with someone who used drugs even once in a while, versus only 19% of all in-treatment participants, and nearly half of out-of-treatment participants responded that they had at least one friend who used drugs, compared with a little over a third of in-treatment participants. Given that drug-using family and peers are less likely to be supportive of an individual's efforts to stop using drugs (4,18), it is not surprising that out-of-treatment participants would perceive less support from these individuals.
While relationships were observed between baseline perceptions of social support and reductions in drug use and criminal activity at 3 months, it is probably not surprising that those relationships did not achieve significance. Findings from the Treatment Outcome Prospective Study (TOPS) suggested that retention in methadone maintenance treatment for a minimum of six months was necessary to obtain reliable evidence of behavior change (38), while findings from the Drug Abuse Treatment Outcome Study (DATOS) suggested that a minimum of one year in methadone maintenance treatment was associated with sustained treatment (39). The lack of significant findings may be due to the fact that participants were still in the beginning stages of treatment.
Finally, results revealed stability in perceived levels of support from baseline to the 3-month follow-up. It is, perhaps, not unexpected that since usual treatment programming puts little emphasis on building and/or strengthening social supports for abstinence that no change is seen in measures of the perceived levels of those supports. That is, treatment programming is typically concerned with increasing the individuals' self-understanding, and emphasizes skills-building to cope with internal and social cues to drug use and relapse. There is, then, a concern with the individuals and with developing their strengths to achieve and maintain abstinence with relatively little concern for developing supports within the community to encourage or sustain that process, or of changing the way in which those potential supports may be viewed.
A limitation to both the present study and the previous research with the CAI by Brown and colleagues is these studies are limited largely to urban African Americans. Thus, determination of the instrument's psychometric properties for other populations is beyond the scope of these studies. Another limitation is these studies were conducted primarily with opioid-dependent patients, and so it is not known whether these findings are generalizeable to other drug- or alcohol-using populations. Further analysis is needed to examine the CAI's reliability and validity in diverse populations.
Despite these limitations, this study's findings indicate the importance of working with drug users located in the community (e.g., through street outreach or work in correctional and health care settings) with regard to their perceptions of social supports and/or the development of those supports for treatment entry. For drug treatment to make a substantial public health impact, it is necessary that a higher percentage of drug-addicted individuals enter treatment (40). Thus, the recognition that increasing the motivation of new entrants to treatment is the first task of treatment can be seen as having its counterpart in the need to increase interest in treatment entry for the many drug users remaining in the community. Beliefs about social supports appear capable of playing a significant role in that effort. In addition, perceptions of social support appear to have potential for increasing levels of engagement for individuals entering drug treatment, and appears to be an important issue for further exploration.
Table 4.
Simple correlations between baseline CAI scales and ASI composite scores in total sample
| ASI Composite Scores | |||||||
|---|---|---|---|---|---|---|---|
| CAI Scales | Medical | Employment | Alcohol | Drug | Legal | Family/Social | Psychiatric |
| Household (N=150) | .207* | -.022 | -.173* | -.023 | -.145 | .012 | .008 |
| Family (N=166) | -.037 | -.015 | -.038 | -.104 | .003 | -.122 | -.003 |
| Friends (N=140) | .098 | -.044 | -.068 | -.035 | -.142 | .026 | -.053 |
| Community (N=196) | .069 | -.183* | -.179* | -.055 | -.185** | .088 | -.010 |
| M | .098 | .858 | .104 | .310 | .248 | .058 | .056 |
| SD | .255 | .213 | .149 | .098 | .235 | .115 | .134 |
p <.05.
p <.01.
Acknowledgments
This study was supported by the National Institute on Drug Abuse Entry and Engagement in Methadone Maintenance Treatment (R01 DA015842, Robert P. Schwartz, PI). The authors wish to express their appreciation to the research participants; research assistants Terrence Hudson, Warren Lee, Donnette Randolph, and Sheree Roles; staff at Man Alive Research, Glenwood Life Counseling Center, Daybreak Rehabilitation Center, Awakenings Counseling Programs, REACH Mobile Health Services, and Turning Point Clinic; and Ms. Melissa Harris, for expert assistance in preparing the manuscript.
Contributor Information
Sharon M. Kelly, Friends Research Institute, Inc. 1040 Park Avenue, Suite 103, Baltimore, MD 21201.
Kevin E. O'Grady, University of Maryland, College Park, MD 20742
Robert P. Schwartz, Friends Research Institute, Inc. 1040 Park Avenue, Suite 103, Baltimore, MD 21201
James A. Peterson, Friends Research Institute, Inc. 1040 Park Avenue, Suite 103, Baltimore, MD 21201
Dr. Monique E. Wilson, Friends Research Institute, Inc. 1040 Park Avenue, Suite 103, Baltimore, MD 21201
Barry S. Brown, University of North Carolina at Wilmington, Wilmington, NC 228403 and Friends Research Institute, Inc 1040 Park Avenue, Suite 103, Baltimore, MD 21201
References
- 1.Brown BS, O'Grady KE, Battjes RJ, Katz EC. The Community Assessment Inventory–Client views of supports to drug abuse treatment. JSAT. 2004;27:241–251. doi: 10.1016/j.jsat.2004.08.002. [DOI] [PubMed] [Google Scholar]
- 2.Gruber KJ, Fleetwood TW. In-home continuing care services for substance use affected families. Subst Use Misuse. 2004;39:1379–1403. doi: 10.1081/ja-120039395. [DOI] [PubMed] [Google Scholar]
- 3.O'Farrell TJ, Feehan M. Alcoholism treatment and the family: Do family and individual treatments for alcoholic adults have preventive effects for children? J Stud Alcohol. 1999 13:125–129. doi: 10.15288/jsas.1999.s13.125. [DOI] [PubMed] [Google Scholar]
- 4.Broome KM, Knight DK, Knight K, Hiller ML, Simpson DD. Peer, family, and motivational influences on drug treatment process and recidivism for probationers. J Clin Psychol. 1999;53:387–397. doi: 10.1002/(sici)1097-4679(199706)53:4<387::aid-jclp12>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- 5.McCrady BS, Epstein EE. Theoretical bases of family approaches to substance abuse treatment. In: Rotger F, Kekker DS, Morganstern J, editors. Treating Substance Abuse: Theory and Technique. New York: Guilford Press; 1999. [Google Scholar]
- 6.Wynne RD, McCrady BS, Kahler CW, Liddle HA, Palmer RB, Horberg LK, et al. When addictions affect the family. In: Harway M, editor. Treating the Changing Family. New York: John Wiley & Sons; 1996. [Google Scholar]
- 7.Moore J, Finkelstein N. Parenting services for families affected by substance abuse. Child Welfare. 2001;80:221–238. [PubMed] [Google Scholar]
- 8.Constantini MF, Wermuth L, Sorensen JL, Lyons JS. Family functioning as a predictor of progress in substance abuse treatment. JSAT. 1992;9:331–335. doi: 10.1016/0740-5472(92)90027-l. [DOI] [PubMed] [Google Scholar]
- 9.Tucker MB. U.S. ethnic minorities and drug abuse: An assessment of the science and practice. In J Addict. 1985;20:1021–1048. doi: 10.3109/10826088509047763. [DOI] [PubMed] [Google Scholar]
- 10.Broome KM, Simpson DD, Joe GW. The role of social support following short-term inpatient treatment. American Journal on Addictions. 2002;11:57–65. doi: 10.1080/10550490252801648. [DOI] [PubMed] [Google Scholar]
- 11.Hanlon TE, Nurco DN, Bateman RW, O'Grady KE. The response of drug abuser parolees to a combination of treatment and intensive supervision. The Prison Journal. 1998;78:31–44. [Google Scholar]
- 12.Battjes RJ, Onken LS, Delany PJ. Drug abuse treatment entry and engagement: Report of a meeting on treatment readiness. J Clin Psychol. 1999;55:643–657. doi: 10.1002/(sici)1097-4679(199905)55:5<643::aid-jclp11>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 13.Joe GW, Simpson DD, Broome KM. Retention and patient engagement models for different modalities in DATOS. Drug Alcohol Depend. 1999;57:113–125. doi: 10.1016/s0376-8716(99)00088-5. [DOI] [PubMed] [Google Scholar]
- 14.Strauss S, Falkin G. Social support systems of women offenders who use drugs: A focus on the mother-daughter relationship. Am J Drug Alcohol Abuse. 2001;27:65–89. doi: 10.1081/ada-100103119. [DOI] [PubMed] [Google Scholar]
- 15.Elliott DS, Huizinga D, Ageton SS. Explaining Delinquency and Drug Use. Newbury Park, CA: Sage Publications, Inc.; 1985. [Google Scholar]
- 16.Thornberry TP, Lizotte AJ, Krohn MD, Farnworth M, Jang SJ. Delinquent peers, beliefs, and delinquent behavior: A longitudinal test of interactional theory. Criminology. 1994;32:47–83. [Google Scholar]
- 17.Warr M, Stafford MC. The influence of delinquent peers: What they think or what they do? Criminology. 1991;29:851–66. [Google Scholar]
- 18.Gandhi DH, Kavanaugh GJ, Jaffe JH. Young heroin users in Baltimore: A qualitative study. Am J Drug Alcohol Abuse. 2006;32:177–188. doi: 10.1080/00952990500479290. [DOI] [PubMed] [Google Scholar]
- 19.Hawkins JD, Fraser MW. The social networks of drug abusers before and after treatment. Int J Addict. 1987;22:343–355. doi: 10.3109/10826088709027434. [DOI] [PubMed] [Google Scholar]
- 20.Nurco DN, Kinlock TW, O'Grady KE, Hanlon TE. Early family adversity as a precursor to narcotic addiction. Drug Alcohol Depend. 1996;43:103–113. doi: 10.1016/s0376-8716(96)01299-9. [DOI] [PubMed] [Google Scholar]
- 21.Kelly SM. Dissertation Abstracts International. Vol. 67. 2005. Holistic reentry: A multidimensional analysis of the revolving prison door; p. 175. UMI No. 3207287. [Google Scholar]
- 22.Sampson RJ, Raudenbush SW, Earls F. Neighborhoods and violent crime: A multilevel study of collective efficacy. Science. 1997;277:918–924. doi: 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- 23.Kelling G, Coles C. Fixing Broken Windows: Restoring Order and Reducing Crime in our Communities. New York: Free Press; 1996. [Google Scholar]
- 24.Skogan W. Disorder and Decline: Crime and the Spiral of Decay in American Cities. Berkeley: University of California Press; 1990. [Google Scholar]
- 25.Wilson JQ, Kelling G. The police and neighborhood safety: Broken windows. Atlantic. 1982;127:29–38. [Google Scholar]
- 26.McLellan AT, Kushner H, Metzger D, Peters R, Smith I, Grissom G, et al. The fifth edition of the Addiction Severity Index: Historical critique and normative data. JSAT. 1992;9:199–213. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- 27.Booth RE, Corsi KF, Mikulich SK. Improving entry to methadone maintenance among out-of-treatment injection drug users. JSAT. 2002;24:305–311. doi: 10.1016/s0740-5472(03)00038-2. [DOI] [PubMed] [Google Scholar]
- 28.Carlson R, Wang J, Siegal H, Falck R, Guo J. An ethnographic approach to targeted sampling: Problems and solutions in AIDS prevention research among injection drug and crack-cocaine users. Human Organization. 1994;53:279–286. [Google Scholar]
- 29.Peterson J, Schacht-Reisinger HS, Schwartz RP, Mitchell SG, Kelly SM, Brown BS, et al. Targeted sampling in drug abuse research: A review and case study. Journal of Field Methods. in press. [Google Scholar]
- 30.Watters JK, Biernacki P. Targeted sampling: Options for the study of hidden populations. Social Problems. 1989;36:416–430. [Google Scholar]
- 31.McLellan AT, Luborsky L, O'Brien CP, Woody GE. An improved diagnostic evaluation instrument for substance abuse patients: The Addiction Severity Index. J Nerv Ment Dis. 1980;168:26–33. doi: 10.1097/00005053-198001000-00006. [DOI] [PubMed] [Google Scholar]
- 32.Hendricks VM, Kaplan CD, van Limbeek J, Geerlings P. The Addiction Severity Index: Reliability and validity in a Dutch addict sample. JSAT. 1989;6:133–141. doi: 10.1016/0740-5472(89)90041-x. [DOI] [PubMed] [Google Scholar]
- 33.Kosten T, Rounsaville BJ, Kleber HD. Concurrent validity of the Addiction Severity Index. J Nerv Ment Dis. 1983;171:606–610. doi: 10.1097/00005053-198310000-00003. [DOI] [PubMed] [Google Scholar]
- 34.McLellan AT, Luborsky L, Cacciola JS, Griffith J, Evans F, Barr HL. New data from the ASI: Reliability and validity in three centers. J Nerv Ment Dis. 1985;173:412–423. doi: 10.1097/00005053-198507000-00005. [DOI] [PubMed] [Google Scholar]
- 35.Cronbach LJ. Essentials of Psychological Testing. 3rd. New York: Harper & Row; 1970. [Google Scholar]
- 36.Grella CE, Joshi V. Gender differences in drug treatment careers among clients in the national drug abuse treatment outcome study. Am J Drug Alcohol Abuse. 1999;25:385–406. doi: 10.1081/ada-100101868. [DOI] [PubMed] [Google Scholar]
- 37.Knight DK, Cross DR, Giles-Sims J, Simpson DD. Psychosocial functioning among adult drug users: The role of parental absence, support and conflict. Int J Addict. 1995;30:1271–1288. doi: 10.3109/10826089509105133. [DOI] [PubMed] [Google Scholar]
- 38.Hubbard RL, Marsden ME, Rachel JV, Harwood HJ, Cavanaugh ER, Ginzburg HM. Drug Abuse Treatment: A National Study of Effectiveness. Chapel Hill: University of North Carolina Press; 1989. [Google Scholar]
- 39.Simpson DD, Joe GW, Brown BS. Treatment retention and follow-up outcomes in the Drug Abuse Treatment Outcome Study (DATOS) Psychol Addict Behav. 1997;11:294–307. [Google Scholar]
- 40.Friedman SR, Tempalski B, Cooper H, Perlis T, Keem M, Friedman R, et al. Estimating numbers of injecting drug users in metropolitan areas for structural analyses of community vulnerability and for assessing relative degree of service provision for injecting drug users. Journal of Urban Health. 2004;81:377–400. doi: 10.1093/jurban/jth125. [DOI] [PMC free article] [PubMed] [Google Scholar]


