Abstract
Objectives
To implement and assess a 4-week advanced pharmacy practice experience in transitional care.
Design
Students participated in the transitional care planning of patients being discharged from 4 general medicine services. Students interviewed patients; assessed discharge medications; reconciled preadmission and discharge medications; provided medication counseling; and conducted postdischarge follow-up by phone to assist patients with medication-related problems and identify additional concerns.
Assessment
Student involvement increased the number of patients who could be assessed and interviewed by the pharmacist preceptor from 10 patients/day to 15 to 20 patients/day. Students strengthened their provider-patient and provider-provider communication skills and developed skills in identifying and resolving barriers to medication adherence.
Conclusion
This transitional care APPE provided students an opportunity to gain experience and self-confidence in the application of pharmaceutical care skills in a transitional care setting, while also providing valuable patient care services to the hospital.
Keywords: advanced pharmacy practice experience, transitional care, pharmacy student, medication reconciliation
Transitional care has been defined as “a set of actions designed to ensure the coordination and continuity of health care as patients transfer between different locations or different levels of care in the same location.”1 It involves logistical arrangements for the patient, education of the patient and family to prepare them for their roles in the next setting of care, and coordination among health care professionals involved in the transition to ensure continuity of care.
Care transitions are complex and as patients transition from the hospital setting to home, they are particularly vulnerable to medical error, especially to adverse medication events (ADEs).2 Nearly two-thirds of post-discharge adverse events are medication related.3 Twenty-nine percent of these ADEs are serious or life threatening, sometimes resulting in emergency department visits and unscheduled hospital admissions. However, as many as 60% of post-discharge ADEs could be prevented or ameliorated with intervention by health professionals at or shortly after discharge.4-10
Health care regulatory agencies and others are advocating the redesign of the discharge process, incorporating activities such as medication reconciliation, discharge medication counseling, and post-discharge patient monitoring. The Joint Commission's National Patient Safety Goals, for example, require health care organizations to “accurately and completely reconcile medications across the continuum of care.”11 These activities provide opportunities for practitioners to identify and resolve potential medication-related problems and reduce the incidence of post-discharge ADEs and their associated costs.4,5,10
Pharmacists are well suited to identify and resolve medication-related problems related to transitional care and provide medication education to patients and their families to prepare them to manage medication therapy following discharge. Such activities are fundamental to pharmaceutical care and are embodied in the 2015 goals of the American Society of Health-System Pharmacists.12 Redesigned discharge processes that incorporate pharmacists to address transitional care needs have been piloted by various institutions and suggest that pharmacist-specific interventions such as medication reconciliation, patient counseling, follow-up telephone calls, and the specific role of pharmacist transition coordinators can result in identification and resolution of medication discrepancies, reduce the incidence of preventable ADEs after discharge, and decrease the number of return visits to the emergency department.5,6,9 Preventable ADEs resulting in hospital admissions are estimated to increase the cost of care to the health system by $3.8 million per year, with nonadherence being the main cause for ADE admissions.13 Although few studies have measured the economic benefits of pharmacist interventions at discharge, health systems may accrue financial benefits through reduced 30-day readmissions and emergency department visits.6-8
The ability of pharmacy students to identify and resolve drug-related problems and to contribute meaningfully to patient care in a variety of practice settings is well documented.14-19 Incorporation of pharmacy students into transitional care activities is a relatively new concept. In one study, pharmacy students provided medication reconciliation upon patient admission to a 300-bed community hospital.20 Specifically, students conducted medication histories and made interventions (under preceptor supervision) to improve medication documentation and pharmaceutical care, thus adding value to the services provided by the pharmacists. Another study demonstrated that pharmacy students could perform accurate, thorough admission medication histories and identify and, under the supervision of the pharmacist preceptor, correct important omissions, thereby improving the completeness and accuracy of more than 67% of patient medication records.21 Pharmacy students have also conducted medication reconciliation activities with patients admitted to an emergency department, finding one or more medications missing from the medication lists recorded at triage for nearly 50% of patients.22 Although these studies illustrate that pharmacy students can be effective in conducting these activities while maximizing preceptor time, experiences involving students in transitional care at hospital discharge are lacking.
The Accreditation Council for Pharmacy Education (ACPE) Standards state that all pharmacy students must complete at least 1 advanced pharmacy practice experience (APPE) in acute care general medicine.23 However, in designing and implementing these experiences, preceptors often struggle with the balance between the responsibilities of clinical teaching and their professional duties to the patients and healthcare system they serve. An ideal solution is to promote development of student experiences that provide actual patient care opportunities with real patients, which would benefit the practice settings while providing a high-quality learning experience. The practice area of transitional care was chosen as a new APPE site because of its potential ability to serve these functions. The purpose of this paper is to describe an APPE in transitional care and demonstrate effects on the quality of patient care.
DESIGN
Expected Outcomes
In the 2007-2008 academic year, a new APPE in transitional care was introduced that emphasized skill development in 4 main areas: patient interview and assessment, patient counseling, medication reconciliation, and post-discharge monitoring. Students conducted these tasks simultaneously and repeatedly throughout the APPE. Communication skills were practiced via interaction with the interdisciplinary health care team and by presenting cases and in-services for pharmacy, medical, and/or other allied health staff members. Students’ clinical therapeutic skills were also honed during patient case discussions with the preceptor and occasional attendance at medical staff teaching rounds. Upon completion of the APPE, students were expected to be able to do the following: describe the potential impact of medication reconciliation and patient counseling on health outcomes; describe the potential role of the pharmacist in facilitating the discharge process; reconcile medication regimens at discharge; identify barriers to medication adherence and compose and implement strategies to overcome non-adherence; screen for, implement appropriate intervention for, and prevent adverse drug events in patients being discharged from the hospital; demonstrate appropriate patient counseling and education skills; and assess patients for post-discharge medication-related problems.
APPE Setting
University Hospital of the University of Michigan is a 550-bed tertiary care academic teaching hospital. The clinical pharmacist preceptor and students participated in the transitional care planning of patients discharged from 4 general medicine services (2 faculty hospitalist teams and 2 traditional medical resident-staffed services). The maximum census for the resident services and the faculty hospitalist teams were 16 patients and 12 patients, respectively, and the average daily discharge volume was 3-5 patients per medical service or team. Pharmacist coverage alternated between the hospitalist teams (maximum 32 patients/day) one month and the resident-staffed services (maximum 24 patients/day) the next.
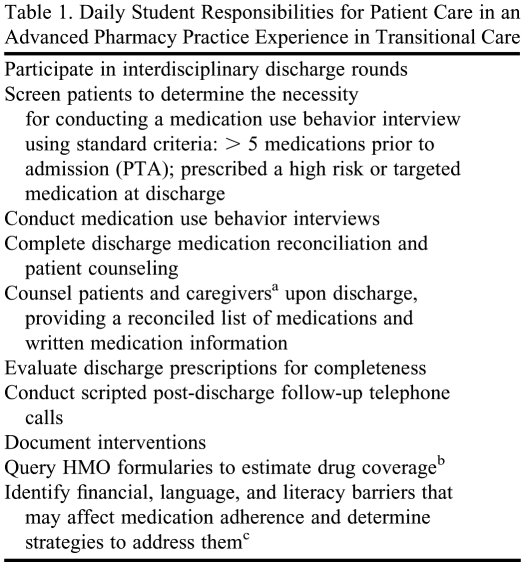
The pharmacist and students attended interdisciplinary team discharge rounds to discuss the clinical and social aspects of each patient's care in preparation for transition from the hospital to home or an alternate care facility; to identify patients scheduled for discharge who were likely to benefit from pharmacist intervention; and to gather information needed to make appropriate pharmacotherapeutic recommendations regarding patients’ discharge medications. Specific activities performed by the pharmacist preceptor and the students during this APPE are shown in Table 1. A pharmacist was regularly assigned to provide transitional care for patients discharged from the targeted medical services and was responsible for any patient follow-up required after the students completed their APPE experience. Patient care activities were documented in the patients’ electronic medical records or in Pharmdoc.net, an internal pharmacy workload documentation and clinical intervention/patient monitoring database.24
Table 1.
Daily Student Responsibilities for Patient Care in an Advanced Pharmacy Practice Experience in Transitional Care
a Caregivers, which are often family members, may be responsible for medication-related activities and reinforcing appropriate behaviors after discharge.
b Majority of queries were conducted using Epocrates Online (https://online.epocrates.com/)
c Strategies might include consulting a social work or interpreter, using visual counseling tools, providing information on drug discount programs, or creating personalized, patient-friendly written medication information.
Instructional Methods and Content
To build and reinforce core skills, each student was assigned to at least 1 of 4 medical teams and made responsible for the daily tasks listed in Table 1. In contrast to the traditional acute care APPE in which there was a significant focus on utilizing objective patient information for therapeutic review, the transitional care APPE emphasized the importance of taking patient personality and behavior into account, as well as evidence-based medicine, when designing therapeutic plans.
During the first week of the APPE, the student shadowed the preceptor; was introduced to the healthcare team; and read assigned literature describing the complexity of the discharge process, rates of post-discharge medication adverse events, and the role of the pharmacist in transitional care. The student was then assigned 1 medical team to follow and, during the second week, assumed greater responsibility for carrying out the associated clinical activities. All tasks were performed under supervision of the preceptor who provided follow-up critique. In a progressive manner throughout the 4-week APPE, students were given more responsibility, including the opportunity to interview and counsel patients in the absence of the preceptor, although the students' work was subsequently reviewed. They generally conducted 8 to 10 patient interviews per day and actively participated in daily interdisciplinary rounds. Medication reconciliation and discharge counseling sessions (1 or 2 patients per day) continued to be directly supervised into the third week, after which the reconciliation results and resolutions were reviewed with the preceptor prior to the student independently counseling the patient upon discharge. Students made post-discharge phone calls to the patients they had assisted. Phone calls were always directly supervised due to the unpredictable nature of problems and questions that might arise; students conducted, on average, 1 or 2 calls per day.
Each week the student spent a minimum of 5 hours in discussion with the preceptor. Topics of discussion included patient cases, therapeutics, pharmacist involvement in transitional care, and barriers to medication adherence. Students were assigned supplemental readings prior to these discussions and were expected to relate the readings in conversation.
During the APPE, the student was expected to respond to drug information questions posed by the interdisciplinary team and patients. Students presented patient case discussions, developed and provided nursing in-services on relevant topics, attended relevant journal clubs, and participated in retrospective chart reviews focused on documenting the impact of the pharmacist in transitional care.
EVALUATION AND ASSESSMENT
The APPE was evaluated from 3 perspectives: student evaluation of the experience, preceptor evaluation of student learning, and the impact of student participation on the productivity of the site.
Student Evaluation of the Experience
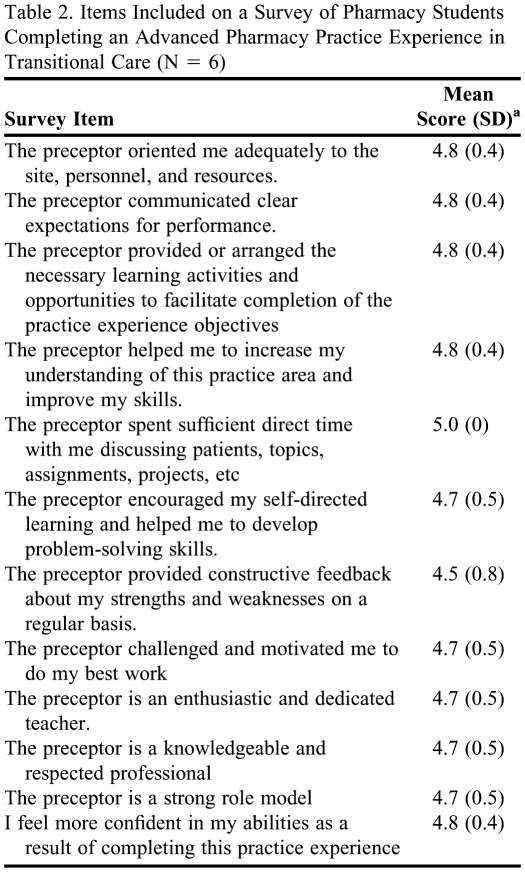
Six fourth-year pharmacy students completed the APPE during the 2007-2008 academic year. These students were randomly selected for participation by the Coordinator of Experiential Training from the cohort of P4 students eligible to enroll in APPEs. Upon completion of the APPE, students were asked to complete a survey instrument regarding the experience (Table 2), rating each statement using a Likert scale of 1 = strongly disagree to 5 = strongly agree. Additionally, students were asked to comment on the strengths and weaknesses of the experience.
Table 2.
Items Included on a Survey of Pharmacy Students Completing an Advanced Pharmacy Practice Experience in Transitional Care (N = 6)
a Rating scale: 1= strongly disagree, 2 = disagree, 3 = neither agree nor disagree, 4 = agree, 5 = strongly agree.
The mean Likert-scale ratings for these statements with regard to the transitional care experience ranged from 4.7 to 5.0. In each case, these ratings either matched or exceeded the mean student rating of each statement for all APPEs in the program for the 2007-2008 academic year. The following student's comment is representative of the feedback received:
The one thing that distinguishes this rotation from other clinical ones is the extensive contact the pharmacy student has with patients.…[The pharmacist] has to interact with a lot of other healthcare workers in order to do her job successfully (thus I had to, too). I really liked feeling I was a part of a ‘team.' Through this rotation, I finally realized that pharmacists can play a very crucial role in catching medication errors that are often overlooked by other health professionals…
Suggestions for improvement included encouraging students to attend morning medical rounds and the suggestion that this experience might be better classified as an ambulatory care experience rather than an inpatient medicine experience.
Preceptor Evaluation of Student Learning
Student learning and performance were evaluated and students were provided written and verbal feedback on their performance at the APPE midpoint and again at culmination. Preceptor evaluation occurred through direct observation of student activities and during case/topic discussions. Students were expected to show professionalism and improved confidence when engaging in provider-to-provider communication exercises. Students were also expected to develop proficiency in provider-to-patient communication skills; students were required to obtain medication information from patients using appropriate prompting, discuss complex medical ideas in lay terminology, and express appropriate empathy.
Preceptors felt that students met or exceeded performance expectations in all assessed areas and indicated that students became active contributors to interdisciplinary rounds. Preceptors observed that students’ interview and counseling skills improved and that by the end of the experience, they demonstrated the ability to appropriately prompt interviewees and redirect conversations. Preceptors felt that the students’ proposed solutions to adherence barriers, based largely on patient interviews, made valuable contributions to the overall care plan.
Impact on Site Productivity
The presence of a pharmacy student substantially increased the number of patients initially assessed and interviewed from 31%-42% of eligible patients (10 per day) by the pharmacist alone to as much as 63% to 83% of eligible patients (ie, 15-20 patients per day), depending on the medical services being covered. The variation reflects differences in skill levels between students, changes in the abilities of individual students over the course of the APPE, differences in patient complexity and its impact on workload, and fluctuation in the daily patient census.
Students screened patients using predefined criteria (see Table 1) to identify patients at risk for medication-related problems after discharge and patients who were most likely to benefit from medication-use behavior interviews. This aided the preceptor in prioritizing patients who were in most need of transitional pharmaceutical care and helped to improve the health system's compliance with the Joint Commission's requirements for medication reconciliation across the continuum of care.
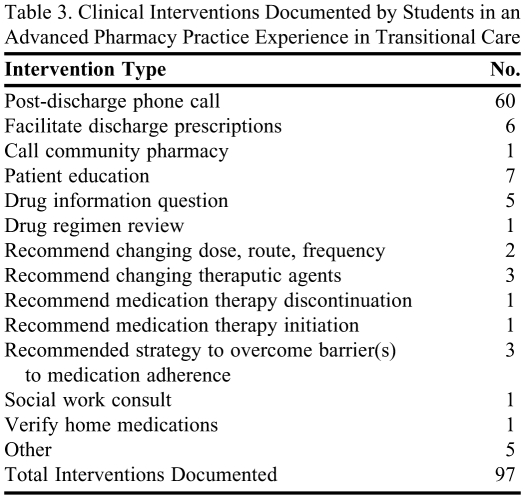
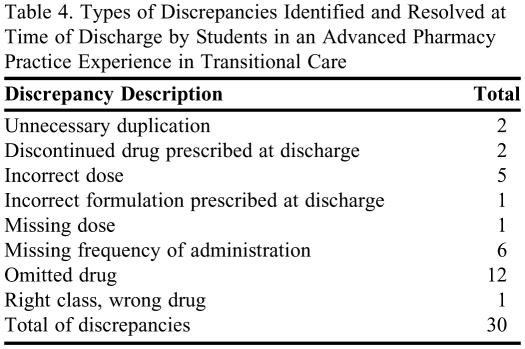
During their 6 months on the service, students documented 97 specific clinical interventions and 30 discharge medication discrepancies in 62 patients (Table 3 and Table 4). All discrepancies were clarified with prescribers and appropriately resolved by the prescribers or the pharmacist prior to patient discharge. Sixty postdischarge follow-up phone calls were completed by the students, monitored by a preceptor.
Table 3.
Clinical Interventions Documented by Students in an Advanced Pharmacy Practice Experience in Transitional Care
Table 4.
Types of Discrepancies Identified and Resolved at Time of Discharge by Students in an Advanced Pharmacy Practice Experience in Transitional Care
DISCUSSION
Transitional care, including medication reconciliation, presents a tremendous opportunity for pharmacists to decrease medication errors and improve overall patient outcomes. A role for pharmacists in transitional care has been described; thus, pharmacy education should provide opportunities for students to gain the necessary skills to participate in this important care process. These skills can be discussed in didactic courses, but actual practice and implementation are essential to true mastery. However, APPEs designed to prepare pharmacy students to participate in transitional care have not been described previously.
We found that the transitional care process provided a rich training experience for pharmacy students. The students who participated in this APPE effectively conducted medication-related transitional care activities at discharge. By performing medication reconciliation at discharge, medication use behavior assessments, patient counseling, post-discharge telephone follow-up, and other activities; students honed their practice skills, developed an appreciation for the role of the pharmacist in transitional care, and also provided a valuable service to the practice site.
Because our report describes the first year of the transitional care service APPE, no comparator data are available. Our sample size was small, with only 6 students completing the APPE in its first year, which may limit the generalizability of our results to other settings. Although in this study we did not attempt to assess the economic benefits of having a student on the service to assist with the workload, other studies of pharmacy students’ contributions have shown economic benefit to the health system through reduced patient readmissions and emergency department visits.6-8
SUMMARY
This transitional care APPE provided students an opportunity to gain experience and self-confidence in the application of pharmaceutical care skills in a transitional care setting while also providing valuable patient care services to the hospital.
REFERENCES
- 1.Coleman EA, Boult C. Improving the quality of transitional care for persons with complex care needs. J Am Geriatr Soc. 2003;51(4):556–567. doi: 10.1046/j.1532-5415.2003.51186.x. [DOI] [PubMed] [Google Scholar]
- 2.Coleman EA. Falling through the cracks: challenges and opportunities for improving transitional care for persons with continuous complex care needs. J Am Geriatr Soc. 2003;51(4):549–555. doi: 10.1046/j.1532-5415.2003.51185.x. [DOI] [PubMed] [Google Scholar]
- 3.Forster AJ, Murff HJ, Peterson JF, Gandhi TK, Bates DW. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003;138(3):161–167. doi: 10.7326/0003-4819-138-3-200302040-00007. [DOI] [PubMed] [Google Scholar]
- 4.Forster AJ, Murff HJ, Peterson JF, Gandhi TK, Bates DW. Adverse drug events occurring following hospital discharge. J Gen Intern Med. 2005;20(4):317–323. doi: 10.1111/j.1525-1497.2005.30390.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Halasymani L, Kripalani S, Coleman E, et al. Transition of care for hospitalized elderly patients – development of a discharge checklist for hospitalists. J Hosp Med. 2006;1(6):354–360. doi: 10.1002/jhm.129. [DOI] [PubMed] [Google Scholar]
- 6.Schnipper JL, Kirwin JL, Cotugno MC, et al. Role of pharmacist counseling in preventing adverse drug events after hospitalization. Arch Intern Med. 2006;166(5):565–571. doi: 10.1001/archinte.166.5.565. [DOI] [PubMed] [Google Scholar]
- 7.Crotty M, Rowett ID, Spurling L, Giles LC, Phillips PA. Does the addition of a pharmacist transition coordinator improve evidence-based medication management and health outcomes in older adults moving from the hospital to a long-term care facility? Results of a randomized controlled trial. Am J Geriatr Pharmacother. 2004;2(4):257–264. doi: 10.1016/j.amjopharm.2005.01.001. [DOI] [PubMed] [Google Scholar]
- 8.Dudas V, Bookwalter T, Kerr KM, Pantilat SZ. The impact of follow-up telephone calls to patients after hospitalization. Am J Med. 2001;111(9B):26S–30S. doi: 10.1016/s0002-9343(01)00966-4. [DOI] [PubMed] [Google Scholar]
- 9.Boockvar KS, Carlson LaCorte H, Giambanco V, Fridman B, Siu A. Medication reconciliation for reducing drug-discrepancy adverse events. Am J Geriatr Pharmacother. 2006;4(3):236–43. doi: 10.1016/j.amjopharm.2006.09.003. [DOI] [PubMed] [Google Scholar]
- 10. Burniske GM, et al. http://www.hospitalmedicine.org/AM/Template.cfm?Section=Abstracts1&Template=/CM/ContentDisplay.cfm&ContentID=5701. Accessed January 26, 2010.
- 11. 2009 National Patient Safety Goals. http://www.jointcommission.org/PatientSafety/NationalPatientSafetyGoals/. Accessed January 26, 2010.
- 12. American Society of Health-System Pharmacists. 2015 Health-System Pharmacy Initiative. http://www.ashp.org/2015.
- 13.Senst BL, Achusim LE, Genest RP, et al. Practical approach to determining costs and frequency of adverse drug events in a health care network. Am J Health-Syst Pharm. 2001;58(12):1126–1132. doi: 10.1093/ajhp/58.12.1126. [DOI] [PubMed] [Google Scholar]
- 14.Donihi AC, Weber RJ, Sirio CA, Mark SM, Meyer SM. An advanced pharmacy practice experience in inpatient medication education. Am J Pharm Educ. 2009;73(1) doi: 10.5688/aj730111. Article 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bock LM, Duong M, Williams JS. Enhancing clinical services by using pharmacy students during advanced experiential rotations. Am J Health-Syst Pharm. 2008;65(6):566–569. doi: 10.2146/ajhp070336. [DOI] [PubMed] [Google Scholar]
- 16.Patterson BY. An advanced pharmacy practice experience in public health. Am J Pharm Educ. 2008;72(5) doi: 10.5688/aj7205125. Article 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ambrose PJ. An advanced pharmacy practice experience in sports medicine. Am J Pharm Educ. 2008;72(1) doi: 10.5688/aj720119. Article 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chisholm MA. A renal transplantation advanced pharmacy practice experience. Am J Pharm Educ. 2006;70(1) doi: 10.5688/aj700103. Article 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Slaughter RL, Erickson SR, Thomson PA. Clinical interventions provided by doctor of pharmacy students. Ann Pharmacother. 1994;28(5):665–670. doi: 10.1177/106002809402800519. [DOI] [PubMed] [Google Scholar]
- 20.Padiyara RS. Student pharmacists and medication reconciliation upon hospital admission: Proposing a way to meet ASHP 2015 objective 1.1. J Am Pharm Assoc. 2008;48(6):701. doi: 10.1331/japha.2008.08106. [DOI] [PubMed] [Google Scholar]
- 21.Mersfelder TL, Bickel RJ. Inpatient medication history verification by pharmacy students. Am J Health-Syst Pharm. 2008;65(23):2273–2275. doi: 10.2146/ajhp080013. [DOI] [PubMed] [Google Scholar]
- 22.Shepherd G, Schwartz RB. Frequency of incomplete medication histories obtained at triage. Am J Health-Syst Pharm. 2009;66(1):65–69. doi: 10.2146/ajhp080171. [DOI] [PubMed] [Google Scholar]
- 23. Accreditation Council for Pharmacy Education. Accreditation standards and guidelines for the professional program in pharmacy leading to the doctor of pharmacy degree. 2006. Available at: http://www.acpe-accredit.org/standards/default.asp. Accessed January 26, 2010.
- 24.McCreadie SR, Callahan BL, Collins CD, Walker PC. Improving information flow and documentation for clinical pharmacy services. Am J Health-Syst Pharm. 2004;61(1):46–49. doi: 10.1093/ajhp/61.1.46. [DOI] [PubMed] [Google Scholar]