Abstract
Objectives
To assess the impact on learning of adding a pediatric human patient simulation to a pharmacy course.
Design
Pharmacy students enrolled in a pediatric elective participated in 1 inpatient and 1 outpatient scenario using a pediatric patient simulator. Immediately following each case, reflective debriefing occurred.
Assessment
Forty-two students participated in the simulation activity over 2 academic years. A pretest and posttest study design was used, with average scores 4.1 ± 1.2 out of 9 on pretest and average 7.0 ± 1.5 out of 9 on posttest (p < 0.0001). Ninety-five percent (40/42) of students' scores improved. Students felt the learning experiences were positive and realistic.
Conclusions
Pharmacy students' knowledge and application skills improved through use of pediatric simulation exercises.
Keywords: simulation, adult learning, pediatric
INTRODUCTION
Accreditation Council for Pharmacy Education standards require colleges and schools of pharmacy to foster students' development of critical thinking and problem-solving skills through application of instructional technologies, laboratory experiences, case studies, guided group discussions, and simulations.1 The offering of elective courses, such as the pediatrics elective highlighted in this study, is also encouraged. Furthermore, the American College of Clinical Pharmacy advocates that pediatric pharmacy be a significant component of pharmacy school education.2 However, this requirement may be difficult given the shortage/lack of pediatric pharmacy education resources. Simulation centers with a pediatric focus might allow expansion of application activities, which could augment a pediatric didactic curriculum.
Patient simulation activities offer one method of building application skills. Simulation involves either actors who portray patients and healthcare professionals, or high-fidelity full-body human patient simulators (HPS). Although HPS use is increasing in many health care disciplines, it has been used in pharmacy education only for teaching clinical and team skills and application of pharmacotherapeutic knowledge.3-6 The utilization of HPS in a pharmacy course that focuses on pediatrics has not been reported.
In 2000, a pediatrics pharmacy elective course at the Samford University McWhorter School of Pharmacy was redesigned to incorporate problem-based learning as the primary pedagogical format. Initial goals for improvement of the course included providing students experience in identifying and solving pharmacy-related problems in infants and children and increasing student motivation for learning. To achieve these goals, the course content was taught primarily through progressive disclosure patient cases. In general, course changes resulted in an increase in student perception of their skills and knowledge related to pediatric pharmacy problems. In particular, there was an increase in students' estimation of their capabilities to calculate pediatric drug dosages, an important skill for pharmacists to have if they are to reduce the rate of medication errors.
Despite improvements in student problem-solving skills, additional emphasis was needed on building students' abilities to provide patient-centered care. In 2007, after acquisition of a simulation center at The Children's Hospital of Alabama (TCHA) where the course instructors practiced, use of a pediatric HPS experience to aid in the development of students' patient care skills was considered. In particular, the learning exercise might help students achieve the following Center for the Advancement of Pharmaceutical Education (CAPE) pharmacy practice supplemental outcomes: (1) formulate a patient-centered pharmaceutical care plan (new or revised) in collaboration with other health care professionals, patients, and/or their caregivers; and (4) communicate and collaborate with prescribers, patients, caregivers and other involved health care providers to engender a team approach to patient care.7
DESIGN
The 2-credit-hour pediatrics pharmacy elective was offered each fall semester to third-year students. The subject material for the class was divided into three 4-week periods: (1) neonatal; (2) infancy and early childhood; and (3) older childhood and adolescence. Each period began with 2 weeks of case-oriented learning, followed by a week of lecture/discussion to reinforce case material, and concluded with a week of student presentations related to the subject matter in the periods. Although the cases did not involve actual patients, the instructors relied heavily on their real life experiences as clinical practitioners for pediatric patients and utilized aspects of real patient situations during case development.
The HPS experience was scheduled to occur after the students had participated in the infancy and early childhood period of the course as the scenarios developed utilized patient cases from these age groups. Also, at this point of the course, students were expected to have sufficient experience learning in a case-based format to be prepared for the simulation encounter. For the exercise, groups of 4 students were exposed to two 30-minute simulation exercises, one similar to what might be encountered by a pharmacist in an outpatient setting and one similar to an inpatient setting. The learning objectives for both scenarios were designed to assess several levels of Bloom's taxonomy of learning.8
The outpatient scenario involved a 15-month old child and his parents who present to a pharmacy with prescriptions for albuterol and fluticasone inhalers and a spacer with mask. While in the pharmacy, the patient develops acute respiratory distress. The infant simulator made audible grunting sounds, had wheezing audible with a stethoscope and had an increased respiratory rate. The simulator also had an increased heart rate which could be determined either by assessing the pulses of the simulator or listening to the chest. There was an actual spacer and albuterol metered-dose inhaler that needed to be dispensed correctly to the infant patient simulator. The students were expected to: (1) know the uses and pharmacologic effects of albuterol and fluticasone; (2) know and comprehend the signs of pediatric respiratory distress; (3) apply their knowledge of albuterol and spacer with mask administration to correctly administer therapy; and (4) analyze the severity of the patient's distress and provide referral care. While assessing the patient, the students had to console the frightened parents. The human dimension and caring were important aspects of the exercise as noted in Fink's taxonomy of significant learning.9
The inpatient scenario was an infant who presented to the emergency department with supraventricular tachycardia (SVT). The infant was attached to a cardiopulmonary monitor that displayed the simulator's heart rate and rhythm, saturations, respiratory rate, and blood pressure. An electrocardiogram was available to the students if requested. Also, the students were able to feel the simulator's very fast heart rate as well as auscultate the heart. Also, adenosine had to be drawn from an actual vial filed with saline and administered correctly, taking into account its extremely short half-life Students were expected to: (1) know and comprehend the dysrhythmia; (2) know recommended treatments for SVT; and (3) apply their knowledge of SVT and its treatment to prepare and administer the recommended dose of adenosine. Students were also asked questions regarding the correct administration of adenosine by the nurse to assess their abilities to communicate and collaborate with other health professionals.
All simulation activities were led by the same 4 instructors. One instructor ran all of the simulator programs, decreasing the variability of the students' experiences. Each simulation was run from the same preprogrammed scenario. Another instructor served as the mother of the child in the outpatient scenario and as the physician in the inpatient scenario. Following each simulation, debriefing was led by the 2 instructors involved in the simulations and assisted by the 2 instructors who taught the course. All simulation sessions occurred at the Pediatric Simulation Center at TCHA using the Simbaby (Laerdal Corporation, Stavanger, Norway) HPS mannequin.
The TCHA Simulation Center has extensive experience, having conducted pediatric simulation training with more than 3000 participants ranging from students to advanced learners. Because the center works exclusively with adult learners, their learning exercises rely heavily on the 6 core andragogy principles introduced by Malcolm Knowles: (1) adults need to know why they need to learn something before learning it; (2) adults want to be self-directing in their learning; (3) adults have rich past experiences which shape their current learning; (4) learning needs to be temporally related to real-world application; (5) orientation to learning needs to be task-centered not subject-centered; and (6) internal motivators are important for adult learners.10 The center also focuses on the debriefing aspects of exercises as part of their learning philosophy relates to the belief that effective simulation activities naturally follow the experiential learning cycle as presented by David Kolb and Kurt Lewin.11 This cycle begins with an experience (either actual patient encounter or simulation), followed by reflective observation, abstract conceptualization, and finally, active experimentation. These principles and concepts were both utilized in the pharmacy student exercises.
To assess the effectiveness of the simulation exercises, a preintervention and postintervention test were used. All students who participated in the simulation experience were in their last 2 academic years when the elective was offered. Each student received a unique identifying number that allowed for anonymous testing but subsequent comparison of preintervention and postintervention scores. Responses to pre- and posttest questions were compared using chi-square analysis, and overall scores for the pretest and posttest were compared using a paired t test. All statistical analyses were conducted using SPSS, Version 11.5 (SPSS, Inc., Chicago, IL). A p value of < 0.05 was considered significant. This study was approved by the Institutional Review Boards at both the University of Alabama at Birmingham and Samford University.
EVALUATION AND ASSESSMENT
A 9-question examination was administered 1-2 weeks prior to students participating in the simulation session. The pretest included fill-in-the-blank questions on signs and symptoms of respiratory distress in an infant, comparing and contrasting stridor and wheezing, the anterior fontanelle and its importance in pediatrics, pediatric dysrhythmias and their treatment, and the use of albuterol inhalers and spacers for acute respiratory symptoms in pediatric patients. Following the simulation session, the students were administered a posttest that included the same 9 questions as in the pretest, plus 3 additional questions to assess the perceived quality of the experience: (1) What did you like best about the simulation center experience?; (2) What did you like least about the experience?; (3) How can the simulation activity be improved? In the first academic year, there were 2 weeks between the pretest and posttest; in the second academic year the posttest was completed immediately following the simulation.
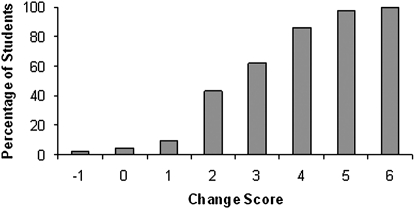
Forty-two students participated in both the simulation activity and lecture in the 2 academic years studied. All 17 (100%) students in the initial year of the study and 25 of 28 (89%) students in the second year participated in all study components. The average score on the pretest was 4.1 ± 1.2 and the average score on the posttest was 7.0 ± 1.5 out of 9 (p < 0.0001). The average change score (pretest minus posttest) was 3.0 ± 1.5. Ninety-five percent (40/42) of students improved their score from pretest to posttest (Figure 1).
Figure 1.
Summary of change scores (posttest minus pretest). Key: the change score represents the difference between the pretest and posttest scores. The maximal score was 9. Forty out of 42 students scored higher on the posttest examination than on the pretest.
The knowledge portion of the assessment contained 3 components. The first component asked students to list signs and symptoms of pediatric respiratory distress. For this question, there was no significant change in the number of signs and symptoms listed. The second component tested students' knowledge of pertinent definitions. Again, there was no significant improvement. The third section was composed of questions on how to treat conditions and how to administer medications. The scores on all questions in this section improved significantly. For example, student response to a question on naming, treating, and drug administration for a pediatric dysrhythmia improved significantly from pretest to posttest. Naming improved from 0% correct to 76% correct; treating improved from 6% correct to 100% correct; and drug administering improved from 0% correct to 88% correct (p < 0.0001 for each of the 3 components).
Additional posttest questions revealed students commenting on enjoying the “realism of the experience” (n = 15), “putting knowledge to practice” (n = 5), “reflecting upon the teaching experience” (n = 3) and “seeing the patient respond” (n = 3). Suggestions for improving the experience included having “more time” (n=5), “more preparation” (n=10), and a “better understanding of what we can do in simulation” (n=3).
DISCUSSION
The use of HPS to augment learning in a pediatric pharmacy elective for third-year pharmacy students was successful. It improved students' abilities to formulate a pediatric pharmacy care plan in conjunction with other health professionals or caregivers. The students enjoyed the realism of the scenarios as they were able to take knowledge acquired in didactic courses and use it in clinical care decisions. They also benefited from their reflections on the experience. We found the greatest improvement in learning as assessed by pretest and posttest was in application of knowledge. This was consistent with our expectations as simulation focuses on Bloom's higher order learning objectives, such as application and analysis.8 As determined anecdotally, through conversations with students in the year following the simulation exercises, knowledge content from the case scenarios was retained. This was in agreement with the findings of Dale who reported that lectures and other passive forms of teaching have only a 10%-20% retention rate after 3 days, whereas simulation activities, such as role-playing and practice, improve retention rates to as high as 70%.12
We did not formally examine the students' skills in communicating and collaborating with other health professionals or caregivers, but we believe the simulation exercises also were successful in giving students the opportunities to practice these abilities. The outpatient scenario required the students to demonstrate the appropriate use of a spacer with a mask to a toddler and counsel anxious parents. Many students had never actually given a dose of albuterol through a spacer before. During the inpatient SVT scenario, the student was required to interact with the nurse and physician caring for the infant. The integration of these human aspects into the scenarios made the scenarios more realistic. Although the “patients” were actually plastic mannequins, the sophistication of the simulators and the actors' authentic portrayal of the infant's parents provided students with a realistic patient care experience. The realism allowed them to suspend disbelief and interact and react as they would have in an actual patient care setting, thus enhancing the learning that occurred during the simulation.12 The realism of the simulation was especially evident as we observed the pharmacy students interact in genuine, caring, and professional ways with the parents and health professionals in the 2 scenarios.
Our findings were consistent with those reported in previous pharmacy HPS experiences including improving students' clinical skills in evaluating blood pressure and pharmacotherapy knowledge of hypertension,3 helping students apply knowledge and practice problem-solving skills in a pharmacotherapy-related course,4,5 teaching interpretation of electrocardiograms and anticipation of antiarrhythmic agents and their pharmacology, and developing interdisciplinary team skills.6 While these previously reported simulation experiences used adult HPS, our affiliation with a simulation center with infant and child simulators allowed us to focus on aspects unique to pediatric patients and demonstrate the application of HPS to pharmacy scenarios involving a special population.
Like other studies with pharmacy students, the simulation learning activities in this report were well received and complemented the other forms of instruction in the elective course. The students had weekly classroom sessions that involved case-based discussions, which may have increased student learning with the simulation and added to their experience. Another positive aspect of the simulations was the debriefing time that followed each session, which augmented student learning by allowing instructors the opportunity to point out right and wrong actions and further explain concepts experienced in the simulation. This active and purposeful debriefing constitutes reflection in David Kolb's experiential learning cycle.11 The post-simulation assessment in this study showed that many students enjoyed the debriefings and recognized that this process furthered their understanding of the scenarios. Since the simulations and the debriefings involve active learning and are learner centered by nature, this contributes to their appeal as an educational method.
Simulations may be a successful approach to teaching pharmacy students because these student have a specific learning style and learn best when a variety of teaching settings and methods (both active and ability-based learning) are used. Both learners who are doers (goal orientated, active, and opportunistic) and learners who are reflectors (people oriented and organized) 12 can benefit from simulators since a thorough simulation exercise involves components of both doing and reflecting and can maximize learning in pharmacists and pharmacy students.
Even though the simulation exercises met the desired student and course outcomes, the course instructors are constantly striving to improve the simulation experience based on the student responses on the posttests. Results from the first academic year showed that students were frustrated with not knowing what to expect and understanding the capabilities of the simulator. Thus, for the second year of implementation, the course instructors offered an introduction to simulation focusing on what to expect at their simulation visit, including the actual preparation and administration of medications. In addition, to introducing the school's administrators to this simulation, the school's dean was extended an invitation to experience this with the students — an event he later described as “positive” and vital to include in all future course offerings. Involving administrators in unique learning experiences like simulation exercises is important because it gives them the opportunity to better understand the educational value of these innovative approaches to teaching and may make them more amenable to procuring continued or additional funding for the program.
The study also has limitations. First, it is difficult to show significant long-term retention with only a single teaching session. In further studies, we plan to do a follow-up knowledge test, and if possible, a follow-up simulation to assess long-term retention. Second, the ability of this educational intervention to change learning was limited due to the small amount of time spent in the simulator center. This is mainly because of the heavy resource requirement of instructors and mannequins involved during simulation activities. The students and educators alike desired more simulated experiences involving other possible pharmacy scenarios. A third limitation is lack of interdisciplinary student involvement. Although the instructors for the simulation were of different health disciplines, the only learners were pharmacy students. In real patient encounters, especially inpatient settings, rarely would a pharmacist act alone. We have done other courses that included doctors, nurses, and pharmacists, and as a result, the breadth and depth of discussion was improved.
SUMMARY
Pediatric patient simulators can improve pharmacy students' knowledge, especially in application of material. This learner-centered approach focusing both on the simulation case and reflective practice was well received by pharmacy students. Although simulation requires significant resources, it offers a great technique to improve pharmacy students' critical thinking and application skills.
REFERENCES
- 1. Accreditation Council for Pharmacy Education: Accreditation Standards and Guidelines for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree. http://www.acpe-accredit.org/pdf/ACPE_Revised_PharmD_Standards_Adopted_Jan152006.pdf. Accessed January 26, 2010.
- 2.Aucoin RG, Buck ML, Dupuis LL, Dominguez KD, Smith KP. Pediatric pharmacotherapeutic education: current status and recommendations to fill the growing need. Pharmacotherapy. 2005;25(9):1277–1282. doi: 10.1592/phco.2005.25.9.1277. [DOI] [PubMed] [Google Scholar]
- 3.Seybert AL, Barton CM. Simulation-based learning to teach blood pressure assessment to doctor of pharmacy students. Am J Pharm Educ. 2007;71(3) doi: 10.5688/aj710348. Article 48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Seybert AL, Kobulinsky LR, McKaveney TP. Human patient simulation in a pharmacotherapy course. Am J Pharm Educ. 2008;72(2) doi: 10.5688/aj720237. Article 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Seybert AL, Laughlin KK, Benedict NJ, Barton CM, Rea RS. Pharmacy student response to patient-simulation mannequins to teach performance-based pharmacotherapeutics. Am J Pharm Educ. 2006;70(3) doi: 10.5688/aj700348. Article 48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fernandez R, Parker D, Kalus JS, MMiller D, Compton S. Using a human patient simulation mannequin to teach interdisciplinary team skills to pharmacy students. Am J Pharm Educ. 2007;71(3) doi: 10.5688/aj710351. Article 51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. American Association of Colleges of Pharmacy Center for the Advancement of Pharmaceutical Education: Educational Outcomes 2004. http://aacp.org/resources/education/Documents/PharmacyPracticeDEC006.pdf Assessed February 8, 2010.
- 8.Bloom BS, editor. Taxonomy of Educational Objectives. The Classification of Educational Goals. Handbook I: Cognitive Domain. New York, NY: McKay; 1956. [Google Scholar]
- 9.Fink LD. Creating Significant Learning Experiences. An Integrated Approach to Designing College Courses. San Francisco, CA: Jossey-Bass; 2003. [Google Scholar]
- 10.Knowles MS, Holton EF, Swanson RA. The Adult Learner. 5th ed. Woburn, MA: Butterworth-Heinemann; 1998. [Google Scholar]
- 11.Kolb DA. Experiential Learning. Englewood Cliffs, NJ: PrenticeHall; 1984. [Google Scholar]
- 12.Austin Z. Development and validation of the pharmacists' inventory of learning styles (PILS) Am J Pharm Educ. 2004;68(2) Article 37. [Google Scholar]