Abstract
Objective
To design and implement an advanced cardiac life support (ACLS) workshop featuring a human patient simulator (HPS) for third-year pharmacy students.
Design
The ACLS workshop consisted of a pre-session lecture, a calculation exercise, and a 40-minute ACLS session using an HPS. Twenty-four 5-member teams of students were assigned roles on a code team and participated in a ventricular fibrillation/pulseless ventricular tachycardia case.
Assessment
Students completed an anonymous postactivity survey instrument and knowledge quiz. Most students who completed the ACLS workshop agreed they would like to participate in additional simulation activities and that the HPS experience enhanced their understanding of ACLS and the pharmacist responsibilities during an ACLS event (99.2% and 98.3%, respectively). However, the median score on the knowledge-based questions was 25%.
Conclusion
Pharmacy students agreed HPS enhanced their learning experience; however, their retention of the knowledge learned was not consistent with the perceived benefits of HPS to education.
Keywords: advanced cardiac life support, simulation, pharmacotherapy, ventricular fibrillation
INTRODUCTION
Advanced cardiovascular life support (ACLS) is a complex, team-based set of treatment strategies essential for the survival of patients experiencing a life-threatening cardiac event. As members of the ACLS team, pharmacists prepare medications at the bedside, provide pharmacotherapy consultations, and document medication administration.1 Pharmacist participation on a resuscitation team in United States hospitals is a core clinical pharmacy service, as their participation decreases adverse drug reactions and hospital mortality.2,3 From an educational standpoint, ACLS represents an ideal integration of patient assessment skills, drug preparation skills, and pharmacotherapeutic knowledge into a process that requires immediacy and accuracy. The Accreditation Council for Pharmacy Education (ACPE) recommends the integration of ACLS into the doctor of pharmacy (PharmD) curriculum.4 However, the best methods for incorporating ACLS knowledge and skill competencies into the curriculum have not been established.
Patient care simulators have been used with increasing acceptance by schools of medicine, nursing, and pharmacy to train students for a variety of clinical scenarios.5 One example is high-fidelity simulation, a unique way to introduce students to ACLS while creating an activity that allows students to apply ACLS pharmacotherapeutic knowledge and skill sets. Simulations are typically case studies of a physical reality in which participants assume a role and address problems that arise during the simulation.6 The fidelity of the simulations refers to the degree to which the simulation reflects reality and can be further characterized by environmental, equipment, psychological, and factual accuracy.7 Human patient simulators (HPSs) are a type of high-fidelity simulator that uses a mannequin integrated with a computer to produce dynamic physiologic outputs such as respiratory movement and electrocardiogram (ECG) monitor readings. Human patient simulators use software that allows the physiologic parameters to change in response to interventions.8
Human patient simulators may be more useful than a didactic lecture and/or paper-based cases in the introduction of ACLS skills because HPSs may help illustrate how clinical, communication, and teamwork skills must be integrated to manage a patient's therapy. For example, a paper-based case may allow students to use their pharmacotherapeutic knowledge to select ACLS medications and develop a monitoring plan. However, it would not recreate the immediacy in which that knowledge would have to be applied, nor would it illustrate the environment in which nonpharmacologic interventions are occurring simultaneously with the pharmacologic interventions. The HPS activity provides firsthand experience, allowing students to gather patient data actively, make real-time decisions, learn about the roles of other health care providers, and implement concurrent interventions such as cardiopulmonary resuscitation. The ACPE recognizes simulation as a method to help develop critical-thinking and problem-solving skills that should be incorporated in PharmD curricula.4 Human patient simulation has been used in pharmacy education to evaluate blood pressure assessment techniques and assess students’ mastery of pharmacotherapeutic coursework. 9-12 The use of HPS for teaching pharmacy students ACLS content has not been reported, but its use has been documented in other health disciplines.13-15
At the University of Kentucky College of Pharmacy, an ACLS laboratory was developed as part of a patient care laboratory course sequence. In 2008, an ACLS laboratory was redesigned as a HPS-based workshop to introduce third-year pharmacy students to the pharmacist's role in ACLS. This paper describes the design and implementation of an HPS-based ACLS workshop for third-year pharmacy students. The investigation was conducted to evaluate student knowledge and perception after the activity.
DESIGN
Patient Care Laboratory VI is the last course in a required 6-semester laboratory sequence in the college's PharmD curriculum. Prior to student participation in the ACLS workshop in the spring semester of the third year, students completed a majority of the pharmacotherapeutics coursework in cardiovascular and pulmonary disease and critical care management. Earlier in the curriculum, students had completed coursework in physical assessment and preparation of sterile products.
Previous iterations of the ACLS workshop consisted of 3 to 4 hours of lecture, design of a patient care plan, introduction to the code cart, and preparation of common medications used in ACLS algorithms. These station-based activities were disconnected and focused on specific individual aspects of ACLS. For example, a small group of students would spend 15 minutes being oriented to a code cart (cardiac arrest cart), then 15 minutes working through a paper cardiac arrest case, then 15 minutes preparing a norepinephrine drip. The result was an exercise that illustrated skills a pharmacist must master to provide ACLS, but the activity failed to demonstrate how these skills must be integrated to provide fast, efficient, and correct care to a patient.
The intent of the revised ACLS workshop was to introduce an advanced area of pharmacy practice to pharmacy students while integrating patient assessment skills, sterile product preparation, and application of knowledge of critical care and cardiovascular pharmacotherapeutics. The incorporation of HPS technology into an ACLS workshop allowed for the simulation of the immediacy that is required to apply these skills and knowledge. Although students were required to maintain basic life support certification while enrolled in the PharmD program, the workshop did not meet the criteria for and was not intended to substitute for ACLS certification.
The ACLS workshop consisted of a pre-session lecture, a pre-session ACLS calculation exercise, and a 40-minute ACLS HPS session. Objectives of the ACLS workshop included preparation of medications for administration in a code situation, calculation and recommendation of appropriate administration rates for ACLS medications, and assessment of a patient's clinical status to anticipate possible therapeutic interventions. To accomplish these objectives, students attended a 2-hour prelaboratory lecture that identified the role of the pharmacist during ACLS, reviewed common pharmacologic agents used in ACLS protocols, and reviewed preparation and calculation of intravenous infusion rates. Students were also provided an ACLS cardiac arrest algorithm and were asked to review the document prior to attending the HPS session.16 Students were divided into 24 groups of 5 students and assigned to a session time. Each group was given a pre-session activity consisting of 3 ACLS-based scenarios that allowed students to review basic concentration and infusion rate calculations.
The HPS sessions were scheduled on 4 different days and held at the University of Kentucky Clinical Skills Training and Assessment Center between February 2008 and April 2008. Six-40 minute sessions were scheduled for each day. The sessions were spaced over a 3-month period because of class schedules and availability of the HPS suite. This activity required approximately 19 hours of instruction to provide all lectures and to have 24 groups of students complete the HPS session. This was a marked increase in instruction time compared to a previous iteration of the activity, which had taken 11 hours. The availability of only 1 HPS was the primary reason for the increase in time. This activity required students to attend 3 hours and 40 minutes of instruction with an estimated 1 to 2 hours of outside preparation for the HPS session.
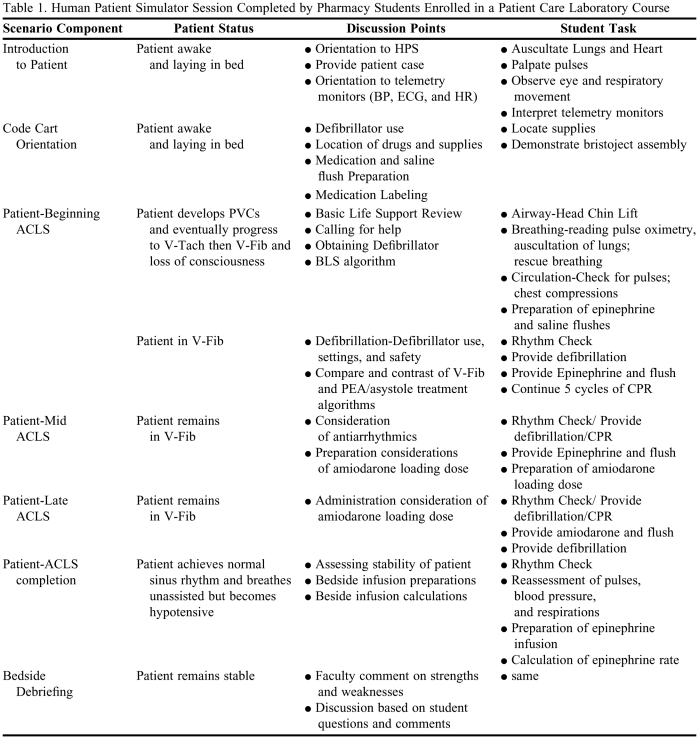
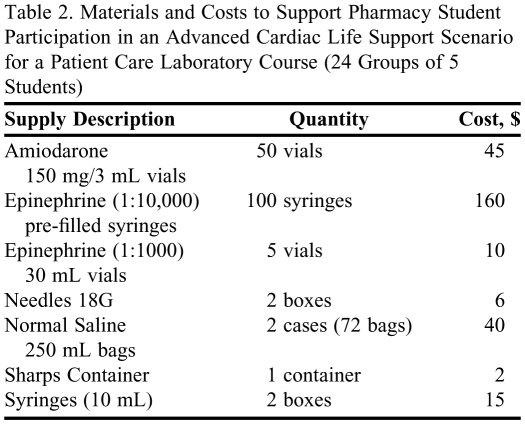
The HPS session was designed around a simulated ventricular fibrillation/pulseless ventricular tachycardia ACLS case. The METI Human Patient Simulator (METI, Sarasota, FL) was used for this simulation. This simulator was specifically designed for training in anesthesia, respiratory, and critical care medicine.17 The simulator had multiple features including palpable pulses, reactive eyes, and the ability to respond physiologically to medication administration based on type, dose, and timing of administration. The simulator also had a complete monitoring system that mirrored standard monitoring systems available in intensive care units. The monitoring system allowed students to view the ECG, oxygen saturation, blood pressure, and heart rate of the patient in real time. A ventricular fibrillation/pulseless ventricular tachycardia scenario was programmed into the HPS, allowing the instructors to pause the scenario to discuss teaching points and then advance the scenario as appropriate. Given the introductory nature of this activity, the course instructor and resident utilized this pause feature to provide immediate feedback and cover specific discussion points throughout the scenario. Additionally, this structure allowed them to standardize information being provided to the students. This format differed from traditional simulation exercises in which students work independently and receive feedback after the completion of the scenario. Table 1 outlines the discussion points covered during the session. In addition to the HPS, a code cart stocked with a defibrillator and typical ACLS medications and materials was utilized during the workshop (Table 2). The Clinical Skills Training and Assessment Center, a division of the University of Kentucky College of Medicine, managed the HPS.
Table 1.
Human Patient Simulator Session Completed by Pharmacy Students Enrolled in a Patient Care Laboratory Course
Abbreviations: HPS = Human Patient Simulator; BP = Blood Pressure; ECG = Electrocardiograph; HR = Heart Rate; PVCs = Premature Ventricular Contractions; V-Tach = Ventricular Tachycardia; V-Fib = Ventricular Fibrillation PEA = pulseless electrical activity; BLS = Basic Life Support; CPR = Cardiopulmonary Resuscitation
Table 2.
Materials and Costs to Support Pharmacy Student Participation in an Advanced Cardiac Life Support Scenario for a Patient Care Laboratory Course (24 Groups of 5 Students)
The ACLS workshop was led by the course instructor and a postgraduate year 2 critical care pharmacy resident. Students were oriented to the available monitoring devices (ECG, pulse oximetry, blood pressure, respiratory rate, and heart rate) and the HPS. Students were asked to palpate the different pulses and auscultate the lungs and heart. Next, the group was oriented to the code cart, location of materials and medications, and use of the defibrillator. After the orientation period, the 5 members were assigned roles on the code team including serving as the code leader, administering respirations, performing chest compressions, preparing medications, and operating the defibrillator or administering medications. Following code team assignments, the patient began to develop premature ventricular contractions (PVCs) and progress to ventricular fibrillation or pulseless ventricular tachycardia. Each group performed basic life support measures, demonstrated mock defibrillation, administered vasoactive and antiarrhythmic medications according to ACLS algorithms, and prepared an epinephrine drip for vasoactive support following return of spontaneous circulation (ie, successful cardiopulmonary resuscitation). During each HPS session, an instructor was present and provided real-time supervision and coached all group members in each of their roles. After completion of the scenarios, the instructors summarized areas of difficulty and responded to student questions.
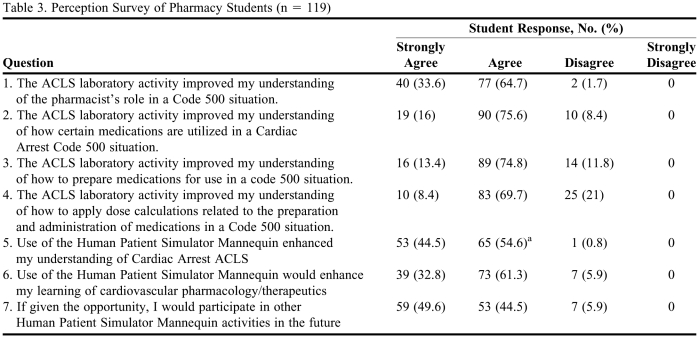
The entire ACLS laboratory was worth 25 points toward the final course grade. Ten of the 25 points could be earned from the preworkshop activity, 10 points could be earned for appropriate participation in the workshop, and the remaining 5 points could be earned from completing an anonymous postactivity survey instrument and knowledge quiz at the end of the spring semester during an unrelated laboratory activity. Anonymity was preserved by instructing students to refrain from writing any identifiers on the survey instrument and knowledge quiz. Students were then asked to sign their name on a log after they completed and turned in their survey instrument and quiz. Students were not permitted to use any resources other than a 4-function calculator. The perception survey (Table 3) evaluated the students’ perception of the ACLS workshop and the HPS. The survey instrument consisted of 7 questions and used a 4-point Likert scale (1 = strongly agree, 2 = agree, 3 = disagree, 4 = strongly disagree). The knowledge quiz consisted of 2 K-type questions and 2 multiple-choice questions to assess knowledge gained during the HPS patient care workshop and prior didactic lectures. The questions addressed ACLS protocols for asystole, pulseless electrical activity (PEA), ventricular tachycardia, and concentration and rate calculations for an epinephrine intravenous infusion (assessment materials are available upon request). The survey and quiz results were quantified and compared using means and medians where appropriate. This assessment was covered by the exempt Institutional Review Board application of the College of Pharmacy Office of Education, which allows faculty members to collect data related to the curriculum for the purposes of assessment and accreditation.
Table 3.
Perception Survey of Pharmacy Students (n = 119)
a One student scored Question 5 as a 2.5.
EVALUATION AND ASSESSMENT
One hundred twenty students completed the ACLS workshop and 119 students completed the postworkshop survey and quiz. Almost all students agreed or strongly agreed the HPS experience enhanced their understanding of ACLS and the pharmacist responsibilities during an ACLS event (99.2% and 98.3%, respectively; Table 3). The survey questions regarding medication utilization, preparation, and administration received the most varied responses from the students. Some students did not agree that the simulation experience helped them understand how to prepare medications (n=14) or apply dosing calculations to the preparation of medications during an ACLS event (n=25). However, the majority of students responded they would participate with an HPS again if given the opportunity and would like to see this type of experiential learning incorporated into other areas of their pharmacy curriculum.
The median score on the knowledge-based portion of the survey instrument was 25%. Ninety-five percent of students answered 2 or fewer questions correctly. Questions regarding asystole/PEA and ventricular tachycardia were answered correctly by 21.8% and 11.8%, respectively. Approximately 20% of answers for the concentration calculation were correct and 78% of the rate calculations were correct.
DISCUSSION
Simulation has consistently been an important tool for the education of health care professionals.18 Simulation learning is highly valued by students training in the healthcare professions. Fourth-year medical students who underwent trauma management simulation training felt they were more clinically competent to handle trauma situations in the hospital.19 Also, fourth-year medical students who were taught how to handle medical emergencies through HPS perceived improvement in both teamwork skills and their understanding of approaching a problem in a systematic way.20 Third- and fourth-year medical students felt that critically ill patient simulation scenarios promoted critical thinking and active learning and allowed them to integrate basic and clinical sciences in order to practice for residency. The medical educators overseeing these students recognized opportunities for integration of basic clinical teaching with advanced problem solving in the scenarios.21
Use of HPS in pharmacy education has been described in 3 studies conducted by Seybert et al in which second-year pharmacy students were trained using HPS as part of 2 courses: Pharmacotherapy of Cardiovascular Disease and Introduction to Critical Care.10-12 Simulation provided the students enrolled in the Pharmacotherapy of Cardiovascular Disease course an opportunity to apply classroom knowledge in a realistic setting to measuring blood pressures and dysrhythmia and myocardial infarction management.10,11 Students were given a pre- and post-activity satisfaction survey and written examination. After simulation-based learning, the authors found a significant improvement in students’ knowledge, confidence when performing physical assessment, and ability to interpret patient data.
The application of basic critical care concepts was introduced through simulation in the Introduction to Critical Care course.12 Not only did the majority of students feel the simulation session allowed them to utilize knowledge learned in the course, 78% believed the experience stimulated their overall interest in critical care. When HPS was used to teach management of hypertensive emergency as part of a Patient Care Laboratory with second-year pharmacy students, 90% of the students felt their clinical patient care learning improved with HPS compared to standard lectures.9 Eighteen percent of the students did not feel the simulation should be a graded experience in order to reduce the stress caused by having to perform. In all of these studies, student were in favor of continued use of HPS throughout the curriculum.9-12
Our study's perception results regarding HPS are similar to other reported perceptions of this type of interactive training with the exception of one objective to this workshop. Twenty-one percent of the students did not perceive an improvement in applying pharmaceutical calculations to the preparation and administration of medications in an ACLS situation. The individual roles of each student participant may have hindered improvements in the application of calculations during this activity. Although the facilitators guided the entire group throughout, only 1 student in each group actually performed the calculations. The remaining group members may not have been adequately exposed to the preparation of medications due to involvement in other ACLS activities during the scenario.
Students performed poorly on the knowledge questions, with 95% of students answering no more than half of the questions correctly. However, reports have documented higher scores on knowledge assessments administered after participating in HPS activities. The performance of students in our study may have been a reflection of how the assessments were conducted and the frequency and duration of use of the HPS.11 Repeated use of HPS may better orient students to this unique learning style and ultimately lead to greater improvements in knowledge, for example, an HPS-based ACLS certification course that offered over 20 contact hours resulted in a 98.9% rate of success leading to certification.22 Our HPS exercise only allowed for 30 minutes of exposure to the mannequin. Learning experiences lacking repetition may not achieve long-term learning, a finding confirmed in this study.23,24
Student preparation is an important factor in their success on assessments. Students may have chosen not to prepare for the workshop since the workshop had little impact on their course grade. However, the amount of time students spent preparing for the workshop was not collected. Students may have performed better if the knowledge assessment was given as a scheduled activity and had a larger impact on the workshop and/or course grade. A scheduled, higher stakes assessment may have increased student motivation to review ACLS material prior to the workshop and prior to the assessment. Another factor to consider in the poor student performance on the knowledge quiz is that the survey instrument and knowledge quiz were not pretested in a focus group setting to determine whether questions or wording were unclear.
The most effective learning strategies when using HPS include providing feedback, repetitive practice, curriculum integration, multiple learning strategies, and a controlled environment 25 Additionally, HPS requires significant investment of time and financial resources to implement successfully, causing some colleges to limit the incorporation of HPS. A limited use of HPS can be counterproductive as it may interfere with learning due to students’ lack of comfort with the simulation enivornment.12 Optimal use of HPS should include repeated exposure to the simulation environment before conducting assessments. Proper orientation and practice may facilitate student acclimation to this interactive method and enhance knowledge gains.
The postlaboratory results of the perception and knowledge assessments lacked comparator prelaboratory assessments. Without knowing the students’ baseline acceptance or knowledge of ACLS training, it was difficult to determine whether this innovative learning technique was better or worse than the previous ACLS curriculum. However, the students’ overall acceptance of this initial attempt of HPS learning encouraged the course instructor to continue using HPS in the ACLS curriculum. The authors acknowledge the need for improvement in the workshop activities and made the following changes. To further enhance the students’ learning during the activity, the course instructor increased the workshop time from 40 minutes to 50 minutes, allowing more time for the students to complete the session tasks. To address the problems with knowledge retention, the instructor scheduled an additional hour of lecture in order to provide expanded material and several case examples to help the students better prepare for the HPS sessions and assessment activities. Finally, knowledge assessments count towards the ACLS workshop grade, which may improve student motivation to prepare for the HPS and assessments. At this time, increasing the use of HPS-based ACLS activities is not possible because of scheduling constraints. However, the course instructor is investigating ways to use HPS for other workshop activities that will improve student familiarity with HPS technology. HPS is being discussed at the university level as a method to provide multidisciplinary instruction to students of the various health professions colleges at the University of Kentucky.
SUMMARY
The introduction of an HPS-based ACLS workshop helped to integrate ACPE curricular standards related to ACLS and active-learning in a format that was positively embraced by students. In our investigation, pharmacy students in their third year agreed that HPS enhanced their learning experience. However, their retention of knowledge gained during the HPS activity was not consistent with the perceived educational benefits of using HPS. Students performed poorly on a post-quiz designed to assess ACLS competencies. The limited HPS exposure and use of a non-graded assessment tool administered months after the experience may have contributed to students’ poor retention of knowledge. Educators should be proactive to ensure appropriate conditions when implementing this interactive technology to enhance student learning.
REFERENCES
- 1.Draper HM, Eppert JA. Association of pharmacist presence on compliance with advanced cardiac life support guidelines during in-hospital cardiac arrest. Ann Pharmacother. 2008;42:469–474. doi: 10.1345/aph.1K475. [DOI] [PubMed] [Google Scholar]
- 2.Bond CA, Raehl CL. Clinical pharmacy services, pharmacy staffing, and adverse drug reactions in United States hospitals. Pharmacotherapy. 2006;26(6):735–747. doi: 10.1592/phco.26.6.735. [DOI] [PubMed] [Google Scholar]
- 3.Bond CA, Raehl CL. Clinical pharmacy services, pharmacy staffing, and hospital mortality rates. Pharmacotherapy. 2007;27(4):481–493. doi: 10.1592/phco.27.4.481. [DOI] [PubMed] [Google Scholar]
- 4. ACPE. Accreditation Standards and Guidelines for the Professional Program in Pharmacy Leading to the Doctor of pharmacy degree. Appendix B. Chicago, Ill: 2006. http://www.acpe-accredit.org/pdf/ACPE_Revised_PharmD_Standards_Adopted_Jan152006.pdf. Accessed on February 5, 2010.
- 5.Henneman EA, Cunningham H, Roche JP, Curnin ME. Human patient simulation: teaching students to provide safe care. Nurse Educactor. 2007;32(5):212–217. doi: 10.1097/01.NNE.0000289379.83512.fc. [DOI] [PubMed] [Google Scholar]
- 6.Gredler ME. Games and simulation and their relationships to learning. In: Jonassen DH, editor. Handbook of Research on Educational Communications and Technology. 2nd ed. Mahwah, NJ: Lawrence Erlbaum Associates; 2004. pp. 571–581. [Google Scholar]
- 7.Beaubien JM, Baker DP. The use of simulation for training teamwork skills in health care: How low can you go? Quality Safety Health Care. 2004;13(Suppl 1):i51–i56. doi: 10.1136/qshc.2004.009845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bradley P. The history of simulation in medical education and possible future directions. Med Educ. 2006;40(3):254–262. doi: 10.1111/j.1365-2929.2006.02394.x. [DOI] [PubMed] [Google Scholar]
- 9.Fernandez R, Parker D, Kalus J, Miller D, Compton S. Using a human patient simulation mannequin to teach interdisciplinary teams skills to pharmacy students. Am J Pharm Educ. 2007;71(3) doi: 10.5688/aj710351. Article 51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Seybert AL, Barton CM. Siumlation-based learning to teach blood pressure assessment to doctor of pharmacy students. Am J Pharm Educ. 2007;71(3) doi: 10.5688/aj710348. Article 48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Seybert AL, Kobulinsky LR, McKaveney TP. Human patient simulation in a pharmacotherapy course. Am J Pharm Educ. 2008;72(2) doi: 10.5688/aj720237. Article 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Seybert AL, Laughlin KK, Benedict NJ, Barton CM, Rea RS. Pharmacy student response to patient-simulation mannequins to teach performance-based pharmacotherapeutics. Am J Pharm Educ. 2006;70(3) doi: 10.5688/aj700348. Article 48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hravnak M, Beach M, Tuite P. Simulator technology as a tool for education in critical care. J Cardiovasc Nurs. 2007;22(1):16–24. doi: 10.1097/00005082-200701000-00003. [DOI] [PubMed] [Google Scholar]
- 14.Perkins GD. Simulation in resuscitation training. Resuscitation. 2007;73(2):202–211. doi: 10.1016/j.resuscitation.2007.01.005. [DOI] [PubMed] [Google Scholar]
- 15.Wayne DB, Didwania A, Feinglass J, et al. Simulation-based education improves quality of care during cardiac arrest team responses at an academic teaching hospital: a case-control study. Chest. 2008;133(1):56–61. doi: 10.1378/chest.07-0131. [DOI] [PubMed] [Google Scholar]
- 16.2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2005;112(24 Suppl):IV1–203. doi: 10.1161/CIRCULATIONAHA.105.166550. [DOI] [PubMed] [Google Scholar]
- 17. HPS…Unmatched Realism With Objective Performance Assessment [brochure] Sarasota, FL: Medical Education Technologies, Inc; 2008. [Google Scholar]
- 18.Steadman RH, Coates WC, Huang YM, et al. Simulation-based training is superior to problem-based learning for the acquisition of critical assessment and management skills. Crit Care Med. 2006;34(1):151–157. doi: 10.1097/01.ccm.0000190619.42013.94. [DOI] [PubMed] [Google Scholar]
- 19.Gilbart MK, Hutchison CR, Cusimano MD, Regehr G. A computer-based trauma simulator for teaching trauma management skills. Am J Surg. 2000;179(3):223–228. doi: 10.1016/s0002-9610(00)00302-0. [DOI] [PubMed] [Google Scholar]
- 20.Weller JM. Simulation in undergraduate medical education: bridging the gap between theory and practice. Med Educ. 2004;38(1):32–38. doi: 10.1111/j.1365-2923.2004.01739.x. [DOI] [PubMed] [Google Scholar]
- 21.Gordon JA, Wilkerson WM. Williamson Shaffer D, Armstrong EG. “Practicing” medicine without risks: students’ and educators’ responses to high-fidelity patient simulation. Acad Med. 2001;76(5):469–472. doi: 10.1097/00001888-200105000-00019. [DOI] [PubMed] [Google Scholar]
- 22.Tafreshi MJ, Huxtable LM. Advanced cardiac life support (ACLS) certification: an innovative course for pharmacy students. Am J Pharm Educ. 2004;68(1) Article 01. [Google Scholar]
- 23.Boonmak P, Boonmak S, Srichaipanha S, Poomsawat S. Knowledge and skill after brief ACLS training. J Med Assoc Thai. 2004;87(11):1311–1314. [PubMed] [Google Scholar]
- 24.Wayne DB, Butter J, Siddall VJ, et al. Simulation-based training of internal medicine residents in advanced cardiac life support protocols: a randomized trial. Teach Learn Med. 2005;17(3):210–216. doi: 10.1207/s15328015tlm1703_3. [DOI] [PubMed] [Google Scholar]
- 25.Issenberg SB, McGaghie WC, Petrusa ER, Gordon DL, Scalese RJ. Features and uses of high-fidelity medical simulations that lead to effective learning: A BEME systematic review. Med Teach. 2005;27(1):10–28. doi: 10.1080/01421590500046924. [DOI] [PubMed] [Google Scholar]