Abstract
Permeability-glycoprotein (P-gp), an efflux transporter in several organs, acts at the blood-brain barrier to protect the brain from exogenous toxins. P-gp almost completely blocks brain entry of the positron emission tomographic (PET) radiotracer 11C-N-desmethyl-loperamide (11C-dLop). We examined the ability of 11C-dLop to quantify P-gp function in humans after increasing doses of tariquidar, an inhibitor of P-gp.
Methods
Seventeen healthy volunteers had a total of twenty-three PET scans with 11C-dLop at baseline and after increasing doses of tariquidar (2, 4, and 6 mg/kg i.v.). A subset of subjects received PET imaging with 15O-H2O to measure cerebral blood flow. Brain uptake of 11C-dLop was quantified in two ways. Without blood data, uptake was measured as area under the time-activity curve in brain from 10 to 30 min (AUC10-30). With arterial blood data, brain uptake was quantified with compartmental modeling to estimate the rates of entry into (K1) and efflux from (k2) brain.
Results
Brain uptake of radioactivity was negligible at baseline and increased only slightly (∼30%) after 2 mg/kg tariquidar. In contrast, 4 and 6 mg/kg tariquidar increased brain uptake 2- and 4-fold, respectively. Greater brain uptake reflected greater brain entry (K1), since efflux (k2) and cerebral blood flow did not differ between tariquidar-treated and untreated subjects. In the subjects that received the highest dose of tariquidar (and had the highest brain uptake), regional values of K1 correlated linearly with absolute cerebral blood flow, consistent with high single pass-extraction of 11C-dLop. AUC10-30 correlated linearly with K1.
Conclusion
P-gp function at the blood-brain barrier in humans can be quantified using PET and 11C-dLop. A simple measure of brain uptake (AUC10-30) may be used as a surrogate of the fully-quantified rate constant for brain entry (K1) and thereby avoids arterial sampling. However, to dissect the function of P-gp itself, both brain uptake and the influx rate constant must be corrected for radiotracer delivery (blood flow).
Keywords: P-glycoprotein, positron emission tomography, N-desmethyl-loperamide
Introduction
ATP binding cassette (ABC) transporters are a group of transmembrane proteins that maintain chemical homeostasis by selectively effluxing compounds from the cytoplasm to the extracellular milieu. One of the most extensively studied ABC transporters is ABCB1, which is the product of the multidrug resistance gene (MDR1), which is more commonly referred to as Permeability-glycoprotein (P-gp) (1). P-gp is present at several sites in the body, including the blood-brain barrier, where P-gp prevents potentially toxic material from entering the brain (2). However, several therapeutic drugs are also substrates for P-gp, and their efflux by P-gp is a potential mechanism of drug-resistance in schizophrenia (3), epilepsy (4), and several types of tumors (1, 5).
The function of P-gp has been measured with positron emission tomography (PET) using radiolabeled substrates, including 99m/94mTc-Sestamibi (6, 7), 11C-verapamil (8), and 18F-paclitaxel (9). Each of these agents has at least one limitation, including difficulty in synthesis, significant contamination by radiometabolites, or only modest increase in brain uptake after inhibition of P-gp (see (10) for review).
In the search for an improved radiotracer to measure P-gp function, we evaluated 11C-loperamide and 11C-desmethyl loperamide (dLop). Loperamide is a potent opiate agonist that is available over the counter and used to treat diarrhea. Loperamide lacks effects on the central nervous system because P-gp avidly blocks its entry into brain (11, 12). Although 11C-loperamide can monitor the function of P-gp at the blood-brain barrier, quantitation with this radiotracer is impaired, since its prominent metabolite, 11C-dLop, is also a substrate for P-gp (13). 11C-dLop is an ideal radiotracer to measure the function of P-gp because its further metabolism generates radiometabolites with minimal entry into brain (13, 14). In addition, using cell cultures with transfected human genes, we found that dLop is selective for P-gp (ABCB1) among the three most common ABC transporters at the blood-brain barrier (ABCB1, ABCC1, and ABCG2) (unpublished data).
We previously showed that [11C]dLop can quantify P-gp function at the blood-brain barrier in monkey (15). However, to separately measure the effect of P-gp on entry vs. delivery, brain uptake must be corrected for regional cerebral blood because of the high single pass extraction (>30%) of this radiotracer. We then extended 11C-dLop to healthy humans and found virtually no uptake in brain (16), consistent with P-gp acting quickly and with high capacity to block the uptake of 11C-dLop. The purpose of this study was to determine whether 11C-dLop can quantify P-gp function in humans and whether measurement of cerebral blood flow is required to correct for differential delivery to regions of the brain. To have measureable uptake of radiotracer, we inhibited P-gp with tariquidar (also called XR9576). Tariquidar was previously tested as an adjuvant to cancer chemotherapy with the goal of increasing uptake of anticancer drugs in tumors that had become resistant by over-expressing P-gp (17). Tariquidar (tested at 2 mg/kg i.v.) was generally ineffective in multi-drug resistant cancer (18). Based upon our studies in monkeys (and the negative clinical trials in human cancer), we suspected that higher doses of tariquidar would be required to significantly increase brain uptake of 11C-dLop. Thus, we tested three doses of tariquidar: 2, 4, and 6 mg/kg i.v.
Materials and Methods
Subject selection
Five healthy human volunteers (age 35 ± 10 years, 3 male, weight 90.2 ± 27.8 kg) participated in the initial PET imaging with 11C-dLop, but without arterial blood sampling. Each subject had two PET scans: at baseline and after administration of tariquidar (2 mg/kg i.v. up to a maximal dose of 150 mg) Because of low brain uptake in the initial study, 12 additional healthy volunteers were studied with arterial blood sampling. These 12 subjects had a total of 13 PET scans: six at baseline (age 31 ± 7, 2 male, 79.3 ± 17.4 kg), four after tariquidar 4 mg/kg (age 38 ± 11, 4 male, 78.8 ± 13.4 kg), and three after tariquidar 6 mg/kg (age 33 ± 7, 1 male, 79.4 ± 16.9 kg). One subject had PET imaging both at baseline and after 6 mg/kg tariquidar (see Supplemental Table for demographic and PET scan information for each subject).
All subjects underwent history, physical examination, routine blood and urine laboratory testing (including chemistries, complete blood count, liver function tests, and urinalysis) and electrocardiogram to exclude serious medical conditions, psychiatric illness, and abuse of illicit substances. Subjects were free of any medication (including non-prescription medications, herbals, and supplements) for at least three days before and after administration of tariquidar, except female subjects of child-bearing potential who were allowed to continue taking oral contraceptives. Subjects younger than 18 years or older than 50 years of age were excluded from study.
Radiotracer preparation
11C-dLop was prepared by the methylation of its primary amide precursor with 11C-iodomethane, as described previously (13). The preparations were conducted according to our investigational new drug application (101,092), submitted to the U.S. Food and Drug Administration (http://pdsp.med.unc.edu/snidd/). The radiotracer was obtained in high radiochemical purity (100%) and with a specific activity of 90 ± 46 GBq/μmol (n = 23 batches) at the time of injection.
Tariquidar preparation and administration
Tariquidar solution was supplied by AzaTrius Pharmaceuticals (London, U.K.). Each mL of solution contained 7.5 mg of tariquidar base as the dimesylate salt in a sterile solution of 20% ethanol / 80% propylene glycol, with a small amount of hydrochloric acid added. Tariquidar solution was stored refrigerated (2 – 8 °C) and protected from light, and allowed to warm to ambient temperature before dilution. The stock solution was filtered and then diluted in 5% dextrose solution at a concentration of 0.6 mg/mL for intravenous administration. The infusion bag and tubing was protected from light at all times.
Tariquidar was infused intravenously via the antecubital vein at a rate of 375 mL/h. Injection of 11C-dLop took place within one hour of the completion of the tariquidar infusion. The one hour delay was required to complete the 15O-H2O scans between completion of tariquidar administration and injection of 11C-dLop.
Safety monitoring
Subjects were monitored for changes in blood pressure, temperature, heart rate, and respiration rate before and after tariquidar infusion. In addition, these parameters, as well as electrocardiogram tracing, were monitored after injection of 11C-dLop. Blood and urine laboratory tests were repeated within 24 hours after completion of the study.
11C-dLop PET imaging
Five subjects underwent PET imaging without arterial sampling. In these subjects, 3D images were acquired on GE Advance (GE Healthcare, Waukesha, WI) in dynamic mode with increasing frame duration for a total scan time of 60 min. An eight-min 68Ge transmission scan was performed before injection of radiotracer for attenuation correction. A fixed injection duration of 20 seconds was used for these subjects. 11C-dLop was injected via a computer-controlled Harvard programmable pump (Harvard Apparatus, Holliston, MA). The injection rate was calculated using DOSE program (NIH PET Department) after inputting the syringe size, desired dose of radioactivity, and injection duration. Subjects had the PET scan repeated under identical conditions on the same day (n = 2), or on a following day (n = 3), after administration of tariquidar (2 mg/kg i.v. or maximum dose of 150 mg).
A total of 12 additional subjects underwent PET imaging with arterial sampling. In these subjects, 3D images were acquired on High Resolution Research Tomograph (Siemens Medical Solution, Knoxville, TN) over a scan time of 60 min. A six-min transmission scan using a 137Cs point source was performed before injection of radiotracer for attenuation correction. A fixed injection duration of one minute was used for these subjects, however one baseline subject had 11C-dLop injected over 20 seconds. The radiotracer injection method was otherwise identical to that described above. Arterial blood was manually sampled at 15 s intervals for first 2 min, then at 3, 5, 10, 20, 30, 45, and 60 min. Plasma 11C-dLop was quantified using radio–high-performance liquid chromatography (radio-HPLC). The plasma concentration of parent radiotracer was separated from radiolabeled metabolites. Due to time constraints, a small number of alternating plasma samples from the early time points were not analyzed using radio–HPLC. Instead the percent composition of parent radiotracer for these time points was estimated by interpolating the measured values. Radio-HPLC was used to determine the concentration of parent radiotracer for the 60 min time point for each subject. Free fraction of 11C-dLop in plasma was measured by ultrafiltration, as previously described (13).
Injected doses of radioactivity from 11C-dLop administration were as follows: 695 ± 69 MBq (baseline), 621 ± 91 MBq (tariquidar, 2 mg/kg), 722 ± 13 MBq (tariquidar, 4 mg/kg), and 707 ± 44 MBq (tariquidar, 6 mg/kg).
15O-water Imaging
Two baseline subjects, and all subjects receiving tariquidar at 4 or 6 mg/kg i.v., also received one to three PET scans with 15O-H2O before injection of 11C-dLop. For each scan, 444 MBq of 15O-H2O were administered, followed by a one-min acquisition. To allow adequate decay of radioactivity, at least 15 min was allowed between injections of 15O-H2O, and between the terminal injection of 15O-H2O and injection of 11C-dLop. Continuous arterial blood sampling was performed during each 15O-H2O scan using an automated blood counter.
Image Analysis
For the HRRT scans, reconstructed images were realigned using Statistical Parametric Mapping 5 (SPM5; Wellcome Department of Cognitive Neurology) and normalized to stereotaxic space. The Montreal Neurological Institute template was used to define regions of interest (frontal, temporal, occipital, parietal, and cerebellar cortex) with pixelwise modeling software 3.95 (PMOD Technologies, Zurich, Switzerland). Regions were inspected and manually adjusted when necessary. An additional region was manually drawn over the choroid plexus in the lateral ventricles.
Concentration of radioactivity was corrected for subject body weight and injected dose of radioactivity and expressed as standardized uptake value (SUV): %SUV = (% injected activity per cm3 brain) × (g body weight). The area under the time-activity curve from 10 to 30 min (AUC10-30) for each brain region was calculated using the trapezoidal method and compared between each group of subjects.
To compare results from images acquired on the GE camera (tariquidar 2 mg/kg, no arterial sampling) to those acquired on the Siemens camera, a 30 cm3 region of cerebellar gray matter was manually drawn. The AUC10-30 of this region was pooled to compare the concentration of radioactivity in the cerebellum at baseline and after administration of tariquidar at 2, 4, and 6 mg/kg.
For baseline and tariquidar scans of 4 and 6 mg/kg, brain and metabolite-corrected plasma data were used to calculate rate constants and total distribution volume (VT) using standard one- and two-tissue compartment models (19). VT is equal to the ratio, at equilibrium, of the concentration of total radioactivity in the brain to the concentration of parent radioligand in plasma, and is the quotient of K1 (the rate constant for brain entry) and k2 (the rate constant for brain efflux) when using the one-tissue compartment model. The total concentration of radioactivity in whole blood was used for vascular correction, assuming that blood constitutes 5% brain volume. The identifiability of the rate constants were obtained from the diagonal of the covariance matrix and expressed as the standard error (SE).
The 15O-H2O scans were also normalized to stereotaxic space and the same regions used for 11C-dLop analysis were applied. Absolute blood flow was calculated using the autoradiographic method (20). In subjects who received more than one 15O-H2O scan, outlier blood flow values were discarded and remaining values were averaged for each region. With absolute blood flow (F) and K1, we further calculated the extraction fraction (E) using the following equation:
| (Eq. 1) |
where
| (Eq. 2) |
and PS is the permeability–surface-area product.
Group data are expressed as mean ± SD.
Results
Safety analysis
11C-dLop was well-tolerated by all subjects. No subjective complaints were attributed to radiotracer injection. Heart rate, blood pressure, respiratory rate, temperature, and ECG were unchanged after injection of 11C-dLop.
Tariquidar was well-tolerated in all but one subject. This subject received 6 mg/kg (total dose = 367 mg). Thirty minutes after initiating the tariquidar infusion, the subject complained of a metallic taste in her mouth and mild nausea. The subject denied any other complaints, including headache, change in vision, weakness, dizziness, or abdominal pain. Heart rate, blood pressure, respiration rate, and temperature did not significantly change during tariquidar administration. Out of concern for possible toxicity, we terminated further accrual into the study. All subjects who received the higher dose of tariquidar (6 mg/kg) returned for repeat blood and urine laboratory tests between 3 and 7 days after receiving tariquidar. No subject had any significant change in blood chemistries (including liver function tests, blood urea nitrogen, and creatinine concentrations), complete blood count, or urinalysis.
Brain uptake of 11C-dLop
Since results from monkey studies using 11C-dLop demonstrated that the AUC could be used as a surrogate measure of K1 (15), we performed the initial 11C-dLop analysis without the use of the arterial input function. At baseline, concentration of radioactivity was low (∼15 %SUV). After P-gp blockade, concentration of radioactivity increased by 28%, however this difference was not statistically significant. Brain uptake (SUV • min) was 211 ± 42 at baseline and 271 ± 54 after 2 mg/kg tariquidar (p = 0.0502, paired t-test, n = 5).
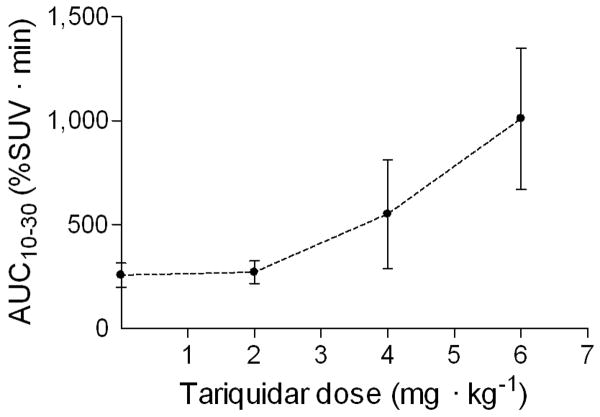
To achieve greater inhibition of P-gp, we administered higher doses of tariquidar. Brain uptake increased in a dose-dependent manner at 2, 4, and 6 mg/kg tariquidar (Figs 1 and 2). Tariquidar at 4 and 6 mg/kg increased brain uptake about 2- and 4-fold, respectively, compared to baseline values (Fig 3). Similar to that in the baseline scans, the time-activity curves show that tariquidar-treated subjects had a rapid peak uptake followed by minimal washout of radioactivity.
Figure 1.
Uptake of radioactivity in brain after injection of 11C-dLop as a function of the dose of tariquidar. Brain uptake was measured as the area under the time-activity curve from 10 to 30 min (AUC10-30) in cerebellum (30 cm3). In addition to the baseline scan (dose of 0 mg/kg), tariquidar was administered at 2, 4, or 6 mg/kg i.v. Symbols and error bars represent mean values ± SD.
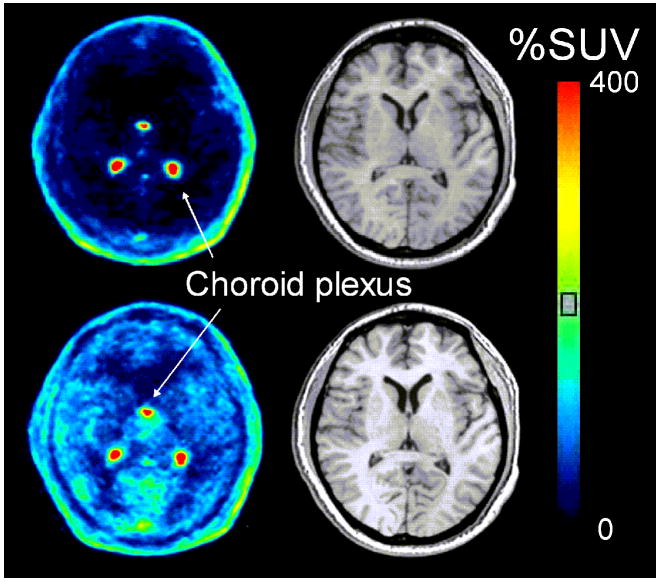
Figure 2.
PET images of 11C-dLop in human brain and corresponding MR image at baseline and after administration of tariquidar (6 mg/kg i.v.). PET images were summed from 0 to 60 min, and pixel values represent mean concentration of radioactivity (%SUV). Arrows point to choroid plexus on the medial surfaces of the lateral ventricles and the roof of the third ventricle.
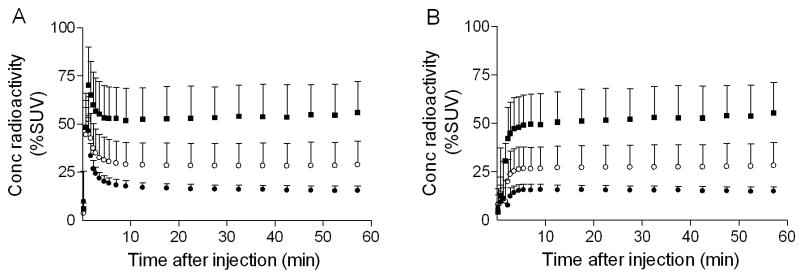
Figure 3.
(A) Concentration of radioactivity in brain, without vascular correction, at baseline (●) and after administration of tariquidar 4 mg/kg i.v. (○) and 6 mg/kg i.v. (■). Symbols and error bars represent mean ± SD. (B) Concentration of radioactivity in the same subjects, with vascular correction.
After injection of 11C-dLop, the choroid plexus had high (∼300 – 400% SUV) and sustained uptake of radioactivity in both baseline and P-gp-blocked scans (Fig 2). P-gp inhibition did not significantly change the peak uptake in the choroid plexus, even after correcting for spill in from adjacent brain regions.
Kinetic analysis
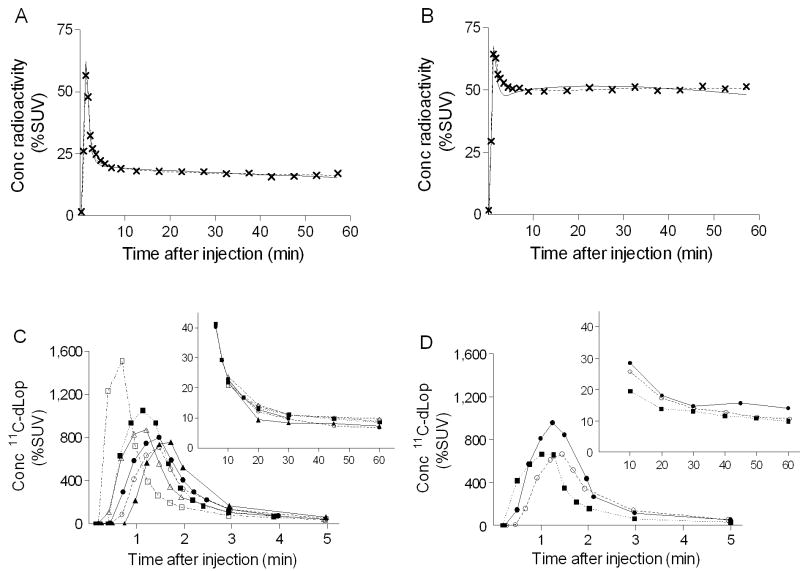
Overall, the unconstrained two-tissue compartment model did not provide significantly better fit than the one-tissue compartment model (Fig 4A, B). Although a subset of brain regions demonstrated significantly better fit using the two-tissue compartment model in certain subjects (F-test, p < 0.01), these regional differences were not consistent among all subjects. Moreover, the two-tissue compartment model estimated the kinetic parameters with poor identifiability (e.g., SE > 100%). In comparison, the one-tissue compartment model estimated K1, k2, and VT with much better identifiability (SE < 12%). P-gp blockade using tariquidar at concentrations of 4 mg/kg and 6 mg/kg resulted in 2- and 4-fold higher values for VT, respectively. These increases were mainly due to higher values of K1, since k2 was similar for baseline and P-gp-blocked scans, regardless of the concentration of tariquidar (Table 1).
Figure 4.
(A, B) Representative time-activity curves and compartmental fitting of radioactivity in the occipital cortex (X) in a single subject at baseline and after administration of tariquidar 6 mg/kg i.v. Solid and dashed lines represent one- and two-compartment model fitting, respectively. (C, D) Concentration of parent 11C-dLop in plasma from six subjects at baseline and three subjects after administration of tariquidar 6 mg/kg i.v. Each symbol represents a different subject. Duration of 11C-dLop injection was 60 s for each subject except one baseline subject (□), who had 11C-dLop injected over 20 s.
Table 1.
Rate constants from one-tissue compartmental modeling of 11C-dLop scans, at baseline and after pharmacolocal inhibition of P-gp with tariquidar (4 or 6 mg / kg i.v.).
| K1 (mL • cm-3 • min-1) | k2 (min-1) | |||||
|---|---|---|---|---|---|---|
| Region | Baseline (n = 6) | 4 mg / kg (n = 4) | 6 mg / kg (n = 3) | Baseline (n = 6) | 4 mg / kg (n = 4) | 6 mg / kg (n = 3) |
| Frontal Cortex | 0.013 ± 0.002 | 0.024 ± 0.008 | 0.044 ± 0.008 | 0.010 ± 0.002 | 0.009 ± 0.001 | 0.012 ± 0.000 |
| Parietal Cortex | 0.014 ± 0.001 | 0.027 ± 0.009 | 0.046 ± 0.007 | 0.012 ± 0.001 | 0.010 ± 0.001 | 0.011 ± 0.001 |
| Occipital Cortex | 0.015 ± 0.004 | 0.031 ± 0.010 | 0.055 ± 0.008 | 0.011 ± 0.004 | 0.011 ± 0.001 | 0.012 ± 0.001 |
| Temporal Cortex | 0.012 ± 0.002 | 0.025 ± 0.008 | 0.040 ± 0.007 | 0.011 ± 0.001 | 0.010 ± 0.001 | 0.011 ± 0.001 |
| Cerebellum | 0.015 ± 0.004 | 0.029 ± 0.010 | 0.052 ± 0.006 | 0.015 ± 0.006 | 0.012 ± 0.003 | 0.014 ± 0.001 |
Increases in brain uptake were not due to increased plasma concentrations of 11C-dLop in the subjects who received tariquidar, since peak plasma concentration was slightly lower on average after maximal blockade of P-gp (Fig 4C, D). In addition, plasma free fraction of parent radiotracer was not significantly different between groups, being 14.6 ± 1.7% at baseline, and 17.4 ± 5.4% and 16.0 ± 4.0% after 4 mg/kg and 6 mg/kg tariquidar, respectively.
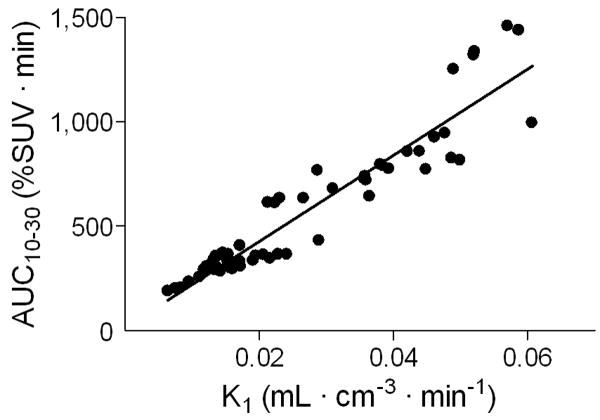
Regional AUC10-30 correlated well with K1 values among the twelve subjects who underwent PET imaging with arterial sampling (Fig 5). Time stability analysis indicates that VT values calculated from less than 50 min of scanning were within 10% difference of that from the entire 60 min scan, but continued to increase because of the slow washout of 11C-dLop. However, K1 values were stable (within 10% of terminal value) after only 20 minutes of scan time (Supplemental Figure).
Figure 5.
Linear correlation between K1 and area under the time-activity curve in brain from 10 to 30 min (AUC10-30). K1 was calculated using the arterial input function, for five brain regions in subjects at baseline (n = 6), and after administration of tariquidar at 4 (n = 4) and 6 mg/kg i.v. (n = 3). Correlation coefficient (r) = 0.94, p < 0.0001.
For the choroid plexus, K1 values were much higher than those for cortical regions. Values for K1 (mL • cm-3 • min-1) were similar among subjects at baseline (0.25) and those who received tariquidar at 4 mg/kg (0.23) and 6 mg/kg (0.28).
Parent radiotracer represented an unusually high percent of total radioactivity throughout the duration of the 11C-dLop scan. After combining the 4 and 6 mg/kg groups, the percentage of total radioactivity composed of parent radiotracer at 60 min was not significantly different between subjects at baseline (90.2 ± 5.5%) and after tariquidar (75.7 ± 15.8%) (p = 0.08, two-tailed t-test).
Blood flow
Tariquidar increased brain uptake of radioactivity but did not do so by increasing delivery of 11C-dLop to brain, as measured by regional cerebral blood flow. For example, in the occipital cortex, a brain region with high blood flow, CBF values (mL • cm-3 • min-1) were 0.348 ± 0.023 in the baseline group, and 0.385 ± 0.060 and 0.393 ± 0.110 in the 4 and 6 mg/kg tariquidar groups. The 13% difference in CBF between the baseline and 6 mg/kg blocked conditions was much less than the 300% difference in brain uptake of radioactivity.
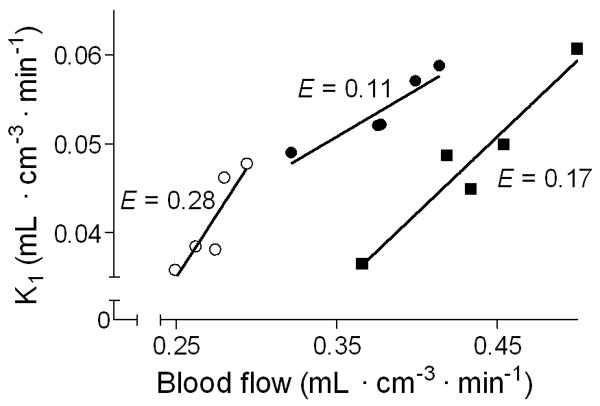
In the subjects that received the highest concentration of tariquidar, K1 correlated linearly with absolute blood flow (Fig 6). Using absolute blood flow values, we calculated extraction fraction and permeability-surface fraction for 5 brain regions in each subject. At baseline, E was low (3.5%), and was 2 and 4–fold higher in the 4 mg/kg and 6 mg/kg tariquidar groups, respectively (Table 2). PS values increased proportionately with increasing dose of tariquidar.
Figure 6.
Relationship between K1 (rate constant of brain entry) and blood flow in the three subjects who received tariquidar 6 mg/kg i.v. K1 and blood flow showed positive correlation, with correlation coefficient (r) > 0.88 and p < 0.05 for each subject. Five brain regions are shown for each subject. The extraction fraction (E) was calculated from the slope of each line.
Table 2.
Extraction fraction and permeability surface product of 11C-dLop at baseline and after pharmacological inhibition of P-gp with tariquidar (4 and 6 mg / kg i.v.).
| Extraction fraction | Permeability surface product (mL • min-1 • mL-1) | |||||
|---|---|---|---|---|---|---|
| Region | Baseline (n = 2) | 4 mg / kg (n = 4) | 6 mg / kg (n = 6) | Baseline (n = 2) | 4 mg / kg (n = 4) | 6 mg / kg (n = 6) |
| Frontal Cortex | 0.032 (0.013) | 0.067 (0.019) | 0.120 (0.018) | 0.011 (0.003) | 0.025 (0.009) | 0.048 (0.007) |
| Parietal Cortex | 0.044 (0.003) | 0.074 (0.016) | 0.132 (0.012) | 0.014 (0.000) | 0.028 (0.009) | 0.050 (0.007) |
| Occipital Cortex | 0.032 (0.020) | 0.077 (0.012) | 0.133 (0.028) | 0.011 (0.007) | 0.032 (0.010) | 0.059 (0.007) |
| Temporal Cortex | 0.031 (0.008) | 0.070 (0.015) | 0.126 (0.022) | 0.010 (0.002) | 0.026 (0.008) | 0.043 (0.008) |
| Cerebellum | 0.035 (0.023) | 0.080 (0.025) | 0.134 (0.026) | 0.012 (0.006) | 0.030 (0.011) | 0.056 (0.006) |
Discussion
The results from this study confirm that 11C-dLop is a substrate for P-gp at the human blood-brain barrier and that the function of P-gp is inversely related to brain uptake of radioactivity. Similar to results in monkeys, the function of P-gp can be quantified from either a simple measure of brain uptake (AUC10-30) or the rate constant of brain entry (K1), and both are strongly correlated. However, the single pass extraction fraction (E) of 11C-dLop is sufficiently high that both AUC10-30 and K1 should be corrected for regional cerebral blood flow to separately measure the effects of permeability from those of drug delivery. Finally, our results suggest that the human blood-brain barrier expresses P-gp with such high capacity that a large degree of inhibition, via high doses of tariquidar, is required to overcome its efflux activity. Based on the limited data size in this study, we cannot make a definitive recommendation on which measure, AUC10-30 or K1, is superior for future studies with 11C-dLop.
Tariquidar increased brain uptake of 11C-dLop by increasing its entry (K1) rather than by decreasing its efflux (k2). These results support the notion that P-gp captures the substrate while in transit through the membrane, thereby preventing entry into brain (21). K1 is the product of flow and extraction (Eq. 1), and extraction itself is also a function of flow (Eq. 2). Among the variables listed in equations 1 and 2, the primary effect of P-gp is to decrease permeability P. Thus, to measure the direct effect of P-gp, permeability (or some surrogate) must be calculated that corrects for the effect of blood flow. Although both K1 and E are dependent on flow, K1 shows the greater effect for physiological values of flow. Thus, we recommend that either K1 (or its surrogate AUC10-30) be corrected (i.e., divided by) flow to more directly measure the function of P-gp.
Unlike the brain, uptake in the choroid plexus was not affected by inhibition of P-gp, even after correcting for spill in of activity from surrounding brain. These results suggest that P-gp does not play a role in the accumulation of 11C-dLop in the choroid plexus. However, both brain and choroid plexus showed prolonged and unexplained retention of radioactivity. The retention is not caused by the radiotracer binding to opiate receptors, since naloxone is not able to displace uptake in monkey brain (13).
P-gp activity is only slightly inhibited by tariquidar at the dose of 2 mg/kg i.v. This dose was used in clinical studies of tariquidar as an adjuvant to chemotherapy in patients with multi-drug resistant tumors (17, 18). The largely negative results of these studies have led most to conclude that P-gp inhibition is not an effective method of improving delivery of chemotherapy to tumor cells. However, if multi-drug resistant tumors have the same large capacity of P-gp as that at the blood-brain barrier, the dose of tariquidar may have simply been too low.
Although tariquidar has been well tolerated at 2 mg/kg in moderately large trials of cancer chemotherapy, one of our patients at 6 mg/kg experienced a metallic taste in the mouth and mild nausea. Both symptoms abated shortly after the infusion was stopped. Although both symptoms were mild and are fairly common from intravenous medications, we halted the study to explore whether they were side effects of tariquidar or of the compounds (propylene glycol and ethanol) used to dissolve the drug. We do not know the answer to this question. However, oral administration of tariquidar has been used in phase I studies (22), and may result in more stable amounts of P-gp inhibition while avoiding potential toxicity from propylene glycol.
PET imaging with 11C-dLop has numerous clinical applications, such as predicting drug resistance in patients suffering from cancer (1), epilepsy (4), and treatment-resistant psychiatric illness (3). Results from imaging with 11C-dLop might inform clinicians of the potential benefit or futility of available medications. In addition, imaging with 11C-dLop could aid in determining the influence of P-gp dysfunction in a number of neurodegenerative disorders, such as Alzheimer's disease, that have been associated with decreased P-gp function. Since several medications are known to be inducers of P-gp function (23-25), pairing 11C-dLop imaging with directed treatment could slow the progression of these diseases.
Conclusion
P-gp function in humans can be quantified using PET and 11C-dLop. After pharmacological inhibition of P-gp, 11C-dLop has a sufficiently large extraction fraction to require that brain uptake be corrected for radiotracer delivery (i.e., cerebral blood flow) to accurately measure the function of P-gp. Thus, in future clinical application we recommend blood flow be measured to correct uptake of 11C-dLop for any group or regional differences in delivery of radiotracer.
Supplementary Material
Figure. Time-stability of VT (A) and K1 (B) in the three subjects who received tariquidar 6 mg/kg i.v. using the occipital cortex (●) and temporal cortex (○).VT continuously increased during the entire 60-min scan, but K1 tended to asymptote and was within 10% of the terminal value after only 20 min. Symbols and error bars represent mean ± SD.
Supplemental Table. PET scans performed with 11C-dLop.
Acknowledgments
We thank AzaTrius Pharmaceuticals for supplying tariquidar; Judith Starling, George Grimes, and Gerald Overman for formulating tariquidar; Jinsoo Hong and Yi Zhang for assistance in the production of radiotracer; and Maria D. Ferraris-Araneta, Barbara Scepura, Gerald Hodges, Leah Dickstein, Robert Gladding, and the NIH PET Department for successfully completing the PET studies. A patent application has been filed on behalf of the U.S. government for PET imaging of P-gp function; Sami Zoghbi, Victor Pike, and Robert Innis could personally benefit from this patent. This research was supported by the Intramural Research Program of NIMH (project # Z01-MH-002852-04).
Financial support: This research was supported by the Intramural Research Program of NIMH (project # Z01-MH-002852-04).
Footnotes
11C-dLop quantifies P-gp function in man
Publisher's Disclaimer: Disclaimer: A patent application has been filed on behalf of the U.S. government for PET imaging of P-gp function; Sami Zoghbi, Victor Pike, and Robert Innis could personally benefit from this patent.
References
- 1.Gottesman MM. Mechanisms of cancer drug resistance. Annu Rev Med. 2002;53:615–627. doi: 10.1146/annurev.med.53.082901.103929. [DOI] [PubMed] [Google Scholar]
- 2.Fromm MF. Importance of P-glycoprotein at blood-tissue barriers. Trends Pharmacol Sci. 2004;25:423–429. doi: 10.1016/j.tips.2004.06.002. [DOI] [PubMed] [Google Scholar]
- 3.Wang JS, Zhu HJ, Donovan JL, et al. Aripiprazole brain concentration is altered in P-glycoprotein deficient mice. Schizophr Res. 2009;110:90–94. doi: 10.1016/j.schres.2009.01.011. [DOI] [PubMed] [Google Scholar]
- 4.Luna-Tortos C, Fedrowitz M, Loscher W. Several major antiepileptic drugs are substrates for human P-glycoprotein. Neuropharmacology. 2008;55:1364–1375. doi: 10.1016/j.neuropharm.2008.08.032. [DOI] [PubMed] [Google Scholar]
- 5.Jamroziak K, Robak T. Pharmacogenomics of MDR1/ABCB1 gene: the influence on risk and clinical outcome of haematological malignancies. Hematology. 2004;9:91–105. doi: 10.1080/10245330310001638974. [DOI] [PubMed] [Google Scholar]
- 6.Piwnica-Worms D, Chiu ML, Budding M, Kronauge JF, Kramer RA, Croop JM. Functional imaging of multidrug-resistant P-glycoprotein with an organotechnetium complex. Cancer Res. 1993;53:977–984. [PubMed] [Google Scholar]
- 7.Bigott HM, Prior JL, Piwnica-Worms DR, Welch MJ. Imaging multidrug resistance P-glycoprotein transport function using microPET with technetium-94m-sestamibi. Mol Imaging. 2005;4:30–39. doi: 10.1162/15353500200504166. [DOI] [PubMed] [Google Scholar]
- 8.Takano A, Kusuhara H, Suhara T, et al. Evaluation of in vivo P-glycoprotein function at the blood-brain barrier among MDR1 gene polymorphisms by using 11C-verapamil. J Nucl Med. 2006;47:1427–1433. [PubMed] [Google Scholar]
- 9.Kurdziel KA, Kiesewetter DO, Carson RE, Eckelman WC, Herscovitch P. Biodistribution, radiation dose estimates, and in vivo Pgp modulation studies of 18F-paclitaxel in nonhuman primates. J Nucl Med. 2003;44:1330–1339. [PubMed] [Google Scholar]
- 10.Kannan P, John C, Zoghbi SS, et al. Imaging the function of P-glycoprotein with radiotracers: pharmacokinetics and in vivo applications. Clin Pharmacol Ther. 2009;86:368–377. doi: 10.1038/clpt.2009.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sadeque AJ, Wandel C, He H, Shah S, Wood AJ. Increased drug delivery to the brain by P-glycoprotein inhibition. Clin Pharmacol Ther. 2000;68:231–237. doi: 10.1067/mcp.2000.109156. [DOI] [PubMed] [Google Scholar]
- 12.Schinkel AH, Wagenaar E, Mol CA, van Deemter L. P-glycoprotein in the blood-brain barrier of mice influences the brain penetration and pharmacological activity of many drugs. J Clin Invest. 1996;97:2517–2524. doi: 10.1172/JCI118699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lazarova N, Zoghbi SS, Hong J, et al. Synthesis and evaluation of [N-methyl-11C-N]-desmethyl-loperamide as a new and improved PET radiotracer for imaging P-gp function. J Med Chem. 2008;51:6034–6043. doi: 10.1021/jm800510m. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zoghbi SS, Liow JS, Yasuno F, et al. 11C-loperamide and its N-desmethyl radiometabolite are avid substrates for brain permeability-glycoprotein efflux. J Nucl Med. 2008;49:649–656. doi: 10.2967/jnumed.107.047308. [DOI] [PubMed] [Google Scholar]
- 15.Liow JS, Kreisl W, Zoghbi SS, et al. P-glycoprotein function at the blood-brain barrier imaged using 11C-N-desmethyl-loperamide in monkeys. J Nucl Med. 2009;50:108–115. doi: 10.2967/jnumed.108.056226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Seneca N, Zoghbi SS, Liow JS, et al. Human brain imaging and radiation dosimetry of 11C-N-desmethyl-loperamide, a PET radiotracer to measure the function of P-glycoprotein. J Nucl Med. 2009;50:807–813. doi: 10.2967/jnumed.108.058453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pusztai L, Wagner P, Ibrahim N, et al. Phase II study of tariquidar, a selective P-glycoprotein inhibitor, in patients with chemotherapy-resistant, advanced breast carcinoma. Cancer. 2005;104:682–691. doi: 10.1002/cncr.21227. [DOI] [PubMed] [Google Scholar]
- 18.Abraham J, Edgerly M, Wilson R, et al. A phase I study of the P-glycoprotein antagonist tariquidar in combination with vinorelbine. Clin Cancer Res. 2009;15:3574–3582. doi: 10.1158/1078-0432.CCR-08-0938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Innis RB, Cunningham VJ, Delforge J, et al. Consensus nomenclature for in vivo imaging of reversibly binding radiotracers. J Cereb Blood Flow Metab. 2007;27:1533–1539. doi: 10.1038/sj.jcbfm.9600493. [DOI] [PubMed] [Google Scholar]
- 20.Herscovitch P, Markham J, Raichle ME. Brain blood flow measured with intravenous H215O. I. Theory and error analysis. J Nucl Med. 1983;24:782–789. [PubMed] [Google Scholar]
- 21.Stewart PA, Beliveau R, Rogers KA. Cellular localization of P-glycoprotein in brain versus gonadal capillaries. J Histochem Cytochem. 1996;44:679–685. doi: 10.1177/44.7.8675989. [DOI] [PubMed] [Google Scholar]
- 22.Stewart A, Steiner J, Mellows G, Laguda B, Norris D, Bevan P. Phase I trial of XR9576 in healthy volunteers demonstrates modulation of P-glycoprotein in CD56+ lymphocytes after oral and intravenous administration. Clin Cancer Res. 2000;6:4186–4191. [PubMed] [Google Scholar]
- 23.Narang VS, Fraga C, Kumar N, et al. Dexamethasone increases expression and activity of multidrug resistance transporters at the rat blood-brain barrier. Am J Physiol Cell Physiol. 2008;295:C440–450. doi: 10.1152/ajpcell.00491.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zong J, Pollack GM. Modulation of P-glycoprotein transport activity in the mouse blood-brain barrier by rifampin. J Pharmacol Exp Ther. 2003;306:556–562. doi: 10.1124/jpet.103.049452. [DOI] [PubMed] [Google Scholar]
- 25.Zhou SF, Lai X. An update on clinical drug interactions with the herbal antidepressant St. John's wort. Curr Drug Metab. 2008;9:394–409. doi: 10.2174/138920008784746391. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure. Time-stability of VT (A) and K1 (B) in the three subjects who received tariquidar 6 mg/kg i.v. using the occipital cortex (●) and temporal cortex (○).VT continuously increased during the entire 60-min scan, but K1 tended to asymptote and was within 10% of the terminal value after only 20 min. Symbols and error bars represent mean ± SD.
Supplemental Table. PET scans performed with 11C-dLop.