Abstract
Context
The gene that codes for cannabinoid receptor 1 (CNR1) represents an important target for investigations designed to elucidate individual differences in the etiology of alcohol dependence.
Objective
To achieve a better understanding of the role of the CNR1 gene in the etiology and treatment of alcohol dependence.
Design
The present investigation spans multiple levels of analysis, including receptor binding in postmortem brain tissue, neuroimaging, human laboratory models, and analyses of treatment outcome data.
Results
Findings indicate that the C allele of rs2023239 is associated with greater CB1 binding in the prefrontal cortex, greater alcohol cue–elicited brain activation in the midbrain and prefrontal cortex, greater subjective reward when consuming alcohol, and more positive outcomes after treatment with a medication that targets the mesocorticolimbic neurocircuitry. In addition, there were strong correlations between cue-elicited brain activation and alcohol consumption measures in individuals with the C allele.
Conclusion
Individuals with the C allele may be more susceptible to changes in the mesocorticolimbic neurocircuitry that is involved in the attribution of incentive salience after repeated exposure to alcohol.
There is growing recognition that cannabinoid receptor type 1 (CB1) plays a major role in alcohol and other drug addictions.1–6 Much of this work has focused on the interaction between the cannabinoid system and neuronal substrates that underlie drug-seeking behavior (Kalivas and Volkow7 provide a review of the neurobiologic mechanisms). The CB1 receptor is the most prevalent G protein–coupled receptor in the brain, and the CB1 receptor is densely localized to the same structures that underlie drug-seeking behavior (eg, the ventral tegmental area [VTA], nucleus accumbens [NAcc], prefrontal cortex [PFC], basolateral amygdala, and hippocampus). On a mechanistic level, the cannabinoid system regulates the release of dopamine, γ-aminobutyric acid (GABA), and glutamate. The CB1 receptors located on GABA interneurons suppress GABA release, which disinhibits dopaminergic projections to the accumbens and increases dopaminergic activation (Maldonado et al5 and De Vries and Schoffelmeer6 provide reviews). The CB1 receptors also regulate glutamatergic projections from the basolateral amygdala and hippocampus by inhibiting the release ofGABA and GABAergic projections from the accumbens to the VTA, indirectly activating the VTA.5,6
With respect to alcohol, the CB1 receptor mediates the effects of alcohol on the neuronal circuitry that underlies reward and the attribution of incentive salience. Recent studies have demonstrated that CB1 antagonists (eg, rimonabant) block the ability of alcohol to initiate the release of dopamine in the accumbens,3 decrease alcohol intake in alcohol- preferring8–12 and normal13 rats, and prevent the ability of cues associated with alcohol and other drugs to reinstate consumption. 6,14–16 In addition, CB1 agonists increase alcohol intake in rats.17 Moreover, CB1 knockout mice consume less alcohol, 3,18–20 show deficits in cue-initiated reinstatement and place preference,20,21 and do not demonstrate alcohol withdrawal symptoms22 or alcohol-induced increases in dopamine release in the accumbens. 3,19 Furthermore, alcohol-preferring animals have greater levels of CB1 messenger RNA in the structures that underlie drug-seeking behavior.23 Thus, the evidence is clear about the importance of the CB1 receptor and the gene that codes for this receptor (CNR1 [OMIM 114610]).3
Despite findings from the animal literature, similar studies in the human literature are almost nonexistent. Although a CB1 antagonist has been tested with nicotine dependence, to our knowledge, there have been no published trials with alcohol dependence. Regarding the gene that codes for the CB1 receptor, several studies24–26 found an association between CNR1 genetic variants and alcohol dependence, and 2 others27,28 did not. Contradictory results are not surprising given the many variables that affect the development of alcohol dependence, the potential error in the assignment of the diagnosis, and the dichotomous nature of a variable that reflects a spectrum disorder. Thus, the use of alcohol dependence as the sole phenotypic end point is a limitation. One of these studies25 noted that several single-nucleotide polymorphisms (SNPs) were associated with messenger RNA changes, and these same SNPs also overlap with SNPs associated with a reward-related neuroimaging phenotype.29
The present investigation encompassed multiple approaches, including receptor binding in postmortem brain tissue, functional magnetic resonance imaging, human laboratory models, and analyses of treatment outcome data. Specifically, this investigation was designed to test the effect of a specific CNR1 SNP (rs2023239) associated with substance dependence and CNR1 messenger RNA changes25 and linked to loci associated with a neuroimaging phenotype. 29 Three hypotheses were tested: (1) rs2023239 may be associated with differential CB1 binding in the PFC based on previous evidence suggesting a link with messenger RNA levels25; (2) rs2023239 may be associated with differences in brain activation during the presentation of alcohol cues using a neuroimaging paradigm and may be associated with the rewarding effects of alcohol based on previous evidence suggesting an association with neuroimaging phenotypes and the extensive literature on the importance of the CB1 receptor in alcohol reward; and (3) rs2023239 may be associated with the effects of a medication on the incentive salience of alcohol and drinking behavior in a treatment outcome trial based on the notion that the medication is effective because it dampens mesocorticolimbic activity.
METHODS
Each of the multiple approaches used in this investigation is described in the following subsections. All the studies were approved by the University of Colorado human research committee.
CB1 BINDING ASSAY IN HUMAN POSTMORTEM BRAIN TISSUE
From 25 to 50 mg of recently collected postmortem tissue (from Brodmann areas 9 and 10) from 20 individuals (10 male white alcoholics and 10 matched controls) was received on dry ice from the Australian Brain Donor Program New South Wales Tissue Resource Centre, University of Sydney, and was immediately stored in a −70°C freezer.
To prepare crude particulate fractions, samples were thawed, suspended in 0.1X buffer (buffer consists of NAcc, 140mM; potassium chloride, 1.5mM; calcium chloride, 2.0mM; magnesium sulfate, 1.0mM; and N-[2-hydroxyethyl]piperazine-N′-[2-ethanesulfonic acid], 25mM; pH, 7.5), homogenized using a motor-driven pestle, and centrifuged at 15 000g for 20 minutes. The supernatants were discarded, and the pellets were resuspended in fresh 0.1X buffer and again centrifuged. The resuspension/ centrifugation cycle was repeated 3 times. After the fourth centrifugation, the supernatant was discarded, fresh hypotonic buffer was added, and the samples were stored frozen as pellets until assay for tritium-labeled CP55,940 binding.
Tritium-labeled CP55,940 binding was measured as described previously30,31 using a 96-well cell harvester (Inotech Biosystems, Rockville, Maryland) with the following modifications. The total volume of the binding reactions was 210 µL. Immediately before filtration, volumes were increased to 1 mL with 0.1% bovine serum albumin and filtration was performed using 0.1% bovine serum albumin as wash solution. The tritium-labeled CP55,940 concentration was 1.2nM, and nonspecific binding was determined in the presence of CP55,940, 10µM. Samples were counted using a liquid scintillation counter (MicroBeta TriLux; Perkin Elmer, Wellesley, Massachusetts) after the addition of scintillant. Binding levels were determined using the method of Lowry et al.32
GENOMIC DNA EXTRACTION AND SNP GENOTYPING
Genomic DNA was collected from buccal cells (cheek swabs) following published procedures.33,34 For the brain samples, genomic DNA was extracted from 5 to 10 mg of the PFC using a commercially available product (DNeasy Mini Kit; Qiagen, Valencia, California) according to the manufacturer’s recommendations. The purity and quantity of DNA were determined by means of spectrophotometric analysis and then adjusted to a concentration of 20 ng/µL. The SNP rs2023239 was assayed using a premade TaqMan genotyping assay (hcv11600616; Applied Biosystems, Foster City, California). The SNP assays were performed using a reaction volume of 15 µL, which consisted of 7.5 µL of TaqMan 2X universal master mix (Applied Biosystems), 0.38 µL of 20X TaqMan predesigned SNP genotyping assay, 6.14 µL of nuclease-free water, and 1 µL of genomic DNA. After polymerase chain reaction amplification per the manufacturer’s recommendations, SNP genotypes were determined by allelic discrimination using a sequence detector instrument (ABI-7500; Applied Biosystems). At least 10% of the samples were repeated, and no error was detected when comparing those samples with the previous samples.
NEUROIMAGING ANALYSES
Blood oxygenation level–dependent functional magnetic resonance images were collected for 34 individuals during exposure to alcohol cues.35 For inclusion, individuals had to report drinking twice per week and at least 5 drinks per occasion (4 drinks for women). Participants also completed alcohol use disorder and craving measures (the Alcohol Use Disorders Identification Test [AUDIT]36 and the Alcohol Urge Questionnaire [AUQ]37).
Details on the procedure are presented elsewhere.35 Participants were presented with 2 echoplanar imaging (EPI) runs consisting of subject-relevant alcohol vs control taste cues (litchi juice). Each EPI consisted of 12 pseudorandom trials of the alcohol and control taste cues. A single trial was composed of a continuous 24-second taste delivery period (total liquid delivered, 1 mL) accompanied by visual instructions. This was followed by a 16-second washout wherein the word rest was visually presented.
Blood oxygenation level–dependent images were collected using a 3-T scanner (Signa; GE Healthcare, Milwaukee, Wisconsin) using a gradient-echo, echoplanar sequence (repetition time, 2000 milliseconds; echo time, 30 milliseconds; flip angle, 90°; field of view, 24 cm; matrix size, 64 × 64; slice thickness, 5 mm; and number of slices, 29). For 2-stage registration of the EPIs, a high-resolution, T1-weighted, 3-dimensional magnetic resonance image (40 axial slices of part of the head; matrix, 512 × 512) acquired using the same slice angles, thickness, and gap as the EPIs and a high-resolution structural image using the inversion-recovery, spoiled, gradient-echo recalled sequence (inversion time, 500 milliseconds; flip angle, 7°; slice thickness, 1.5 mm; matrix, 256 × 256; field of view, 200 × 200 mm; bandwidth, 15.6 kHz; and number of slices, 124) were collected close to EPI acquisition. The tastes were delivered via fluorocarbon resin tubing using a computer-controlled pump system (Custom Infinity Controller; J-Kem Scientific, St Louis, Missouri) that was synchronized with visual instructions programmed in E-Prime38 and presented using a goggle system.
Imaging data analyses were conducted through FEAT (FMRI Expert Analysis Tool) version 5.43, part of FSL (FMRIB Software Library). Standard preprocessing was applied, including nonbrain removal using the Brain Extraction Tool method,39 spatial smoothing using a gaussian kernel of full width at half maximum of 8-mm, mean-based intensity normalization of all volumes by the same factor and high-pass temporal filtering (σ = 50.0 seconds). Time series statistical analysis was performed using FMRIB’s Improved Linear Model with local autocorrelation correction.40 Regressors were created by convolving the stimulus timing files with a double γ-variate hemodynamic response function. A multiple linear regression analysis was performed to estimate the hemodynamic parameters for different explanatory variables (ie, alcohol taste period, control taste period, and baseline period), and a corresponding t statistic indicated the significance of the activation of the stimulus. The primary contrast was the alcohol vs control taste period. For comparisons between genotype groups, these contrast maps were then registered to a high-resolution image using FMRIB’s Linear Image Registration Tool. A priori region-of-interest anatomical masks were created using previously described methods35 for the NAcc/ventral striatum, the VTA, the orbitofrontal cortex (OFC), and the ventromedial PFC (VMPFC). Group-level analysis was performed using FLAME (FMRIB’s Local Analysis of Mixed Effects) stage 1 only (ie, without the final Markov Chain Monte Carlo–based stage).41,42 Z (gaussianized T/F) statistical images were thresholded using gaussian random field theory–based maximum height thresholding with a significance of P = .05.43
To determine the relationship between brain activation in response to cues and subjective craving, Pearson product moment correlations were performed between region-of-interest (NAcc, VTA, left and right OFC, or VMPFC) peak percentage signal change values and AUDIT and AUQ scores. For these analyses, more restricted region-of-interest masks for the smaller regions, such as the NAcc (x, 8 to 16; y, 14 to 6; z, −4 to −12) and the VTA (x, −8 to −4; y, −10 to −18; z, −8 to −16), were used for better localization. Group differences were investigated by converting the correlation coefficients to z scores and dividing the difference by the standard error. Larger masks were used in the main analyses to avoid missing significant findings. The regions of interest for the correlation analysis were restricted to a smaller size to focus the correlations on the peak activity in the theoretically meaningful voxels.
SHORT-TERM RESPONSES TO ALCOHOL
Study 1
Volunteers (n = 74) provided informed consent before participating. Participants were compensated $100 for study completion. Moderate to heavy drinkers aged 18 to 25 years were recruited from the Denver or Boulder, Colorado, metropolitan area.
Participants were scheduled for 2 sessions, 1 week apart. Consistent with previous studies,35 participants consumed 3 standard drinks with equivalent alcohol content during 1 session and 3 placebo drinks in the other session, for which the order was randomized. Laboratory sessions were scheduled between noon and 6 PM. After each drink, participants completed measures of reward and positive affect. During the baseline session, participants completed a battery of self-report tobacco use assessments. A demographic questionnaire collected information on age, sex, marital status, socioeconomic status, occupation, annual income, educational level, and race. An alcohol history questionnaire collected information on frequency and quantity of alcohol use. At the beginning of the following (experimental) session, participants underwent breathalyzer testing to ensure that they had not been drinking before the session. The rewarding effects of alcohol were measured using the Alcohol Rating Scale, which included the following items: How satisfying was the drink? How enjoyable was the drink? How much did you like the drink? The elation scale from the Profile of Mood States was used to measure positive affect.44 Analyses involved a 2 (genotype: TT vs CT) × 3 (drink: 1 vs 2 vs 3) analysis of variance (ANOVA). The difference scores (alcohol session minus placebo session) for reward and positive affect were the dependent variables in the ANOVA.
Study 2
To provide further replication, data from a previously published study (n = 67) were reanalyzed with rs2023239.34 The methods differed considerably because the present study did not include a placebo alcohol condition and was designed to examine the effects of active and control medications on responses to alcohol. The dependent variables were subjective high and reward (as described previously).
TREATMENT STUDY
To examine the treatment implications of rs2023239, we reanalyzed data from a previous clinical trial (N = 69) that involved a medication that targets the mesocorticolimbic neurocircuitry. The methods of this study are described briefly; they are described in detail elsewhere.34
Participants were selected based on DSM-IV criteria for alcohol dependence and the consumption of 14 drinks (women) or 21 drinks (men) on average per week for 4 consecutive weeks. Participants had to be within 21 days of their last drink to be included. Patients were excluded if they met the criteria for specific psychiatric diagnoses (bipolar disorder, schizophrenia, bulimia, or anorexia nervosa), reported a psychological disorder requiring pharmacotherapy, endorsed current use of illicit drugs other than marijuana, or tested positive for illicit drugs other than marijuana.
The analyses included 69 participants randomized to a 12- week trial of olanzapine (5 mg) or placebo. Participants completed baseline measures of demographics, personality, alcohol use, alcohol-related problems, and motivation for change. At 2 weeks, these participants completed a cue reactivity assessment that involved comparing reactivity between controls (eg, a nonalcoholic beverage such as Gatorade) and alcohol-related cues (eg, the preferred alcoholic beverage). During the control cue exposure, participants were asked to lift and sniff Gatorade without tasting it for 3 minutes. Participants completed measures of mood and craving before and after exposure. After a 5-minute relaxation period, participants repeated the cue exposure with their preferred alcoholic beverage and completed the same craving and mood measures. All the participants received 2 sessions of a brief, psychosocial intervention. These sessions occurred at the end of the baseline and cue reactivity sessions.
With respect to cue reactivity, the AUQ was used to measure craving during the cue reactivity assessment. The AUQ consists of 8 items rated on a 7-point Likert scale anchored by “strongly disagree” and “strongly agree.” The AUQ has demonstrated high reliability in assessing urge to drink.37
Consistent with previous studies,45–47 the primary outcomes were drinks per drinking day measured at baseline and at 4, 8, and 12 weeks using a timeline follow-back procedure. 48 Of the 69 participants, 46 had the TT genotype, 22 had the CT genotype, and 1 had the CC genotype. For the analyses, the individual with the CC genotype was included in the CT group. The baseline data suggested that the groups did not differ on sex, ethnicity, or tobacco use.
RESULTS
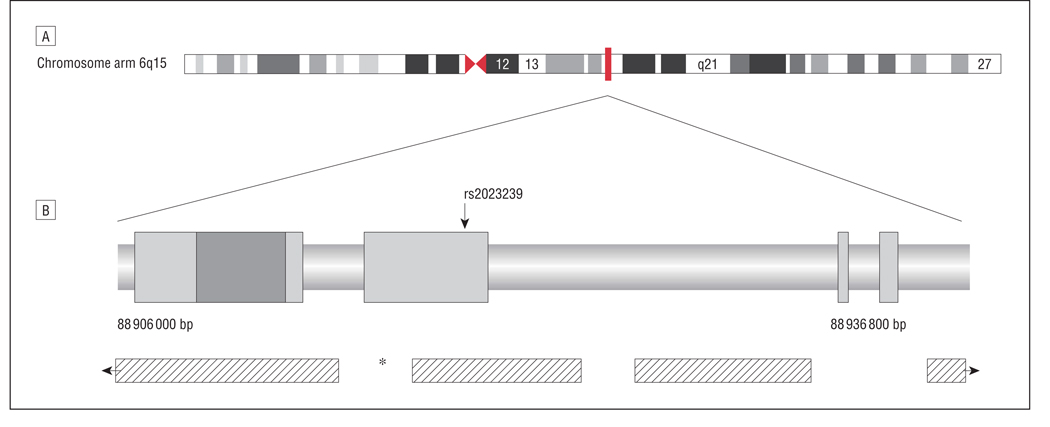
Figure 1 depicts the regulatory and coding regions of CNR1 based on the study by Zhang et al25 and the National Center for Biotechnology Information. Analyses were focused on rs2023239 found in the region upstream of exon 3, which has been described as an alternative promoter.25 Each approach described in the “Methods” section has a corresponding result subsection.
Figure 1.
Depiction of the cannabinoid receptor type 1 gene (CNR1) genomic region, the location of rs2023239, and linkage disequilibrium (LD) throughout the region. A, The location of the CNR1 gene on chromosome arm 6q15. B, The location of the coding region (box indicated by the arrow), potential noncoding exons, and the untranslated region as depicted by Zhang et al.25 The regions of significant LD are depicted by the hashed rectangles. The asterisk shows the location of a predicted recombination hotspot. bp indicates base pair.
CB1 BINDING LEVELS IN POSTMORTEM PFC
To test the association between rs2023239 and CB1 receptor levels, CB1 binding was quantified in postmortem human PFC and the relationship between rs2023239 and CB1 binding was assessed. Ten samples were genotyped as TT and 10 as CT. The ANOVA revealed that individuals with the CT genotype for rs2023239 demonstrated significantly greater CB1 binding in Brodmann areas 9 and 10 compared with individuals with the TT genotype (F1,16 = 9.62, P < .01) (Figure 2).
Figure 2.
Cannabinoid receptor type 1 (CB1) receptor levels by genotype. Tritium-labeled CP55,940 binding in postmortem prefrontal cortex, Brodmann areas 9 (BA 9) and 10 (BA 10), comparing individuals with the TT genotype with those with the CT genotype for rs2023239. Those with the CT genotype have significantly greater CB1 receptor binding (*P < .01). Error bars represent SE.
CUE-ELICITED CRAVING AND BRAIN ACTIVATION
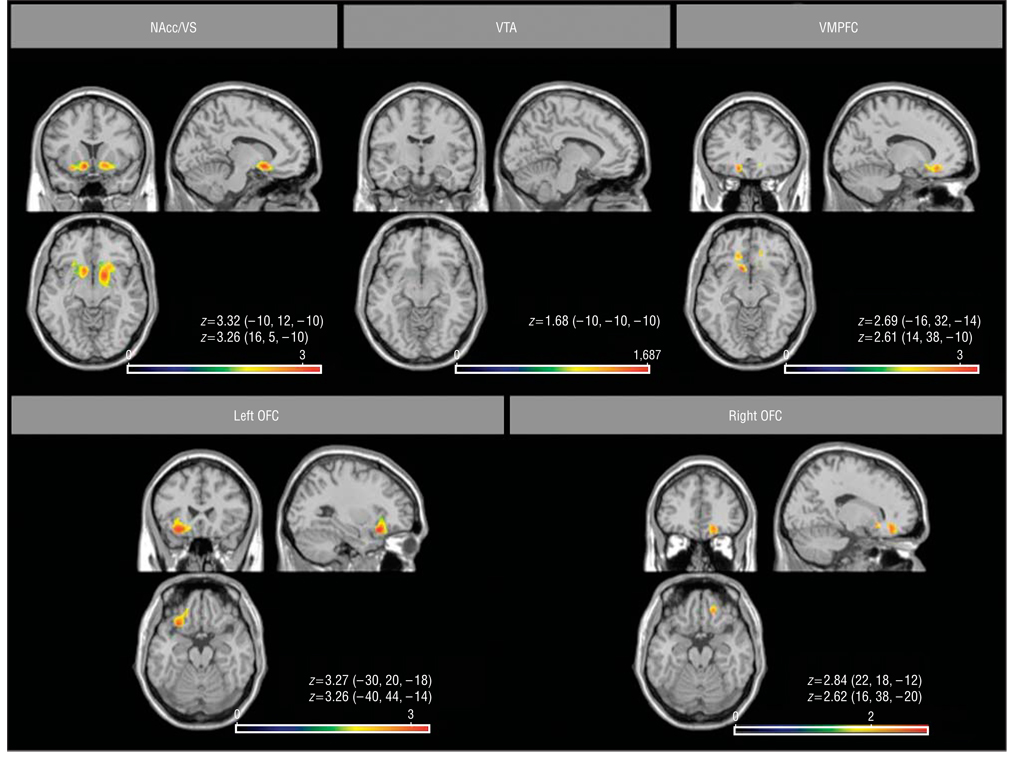
Because CNR1 receptors modulate the mesocorticolimbic neurocircuitry that underlies drug-seeking behavior in animals,5,6 it was expected that the genetic variation that alters CB1 receptor levels would also be associated with the differential activation of these structures during exposure to alcohol cues. To explore the functional significance of rs2023239, data from a recent neuroimaging study35 were reanalyzed. Participants were 34 heavy drinkers who were right-handed and had no history of psychiatric or neurologic disorders. Two participants had the CC genotype and 8 had the CT genotype. Individuals with at least 1 copy of C (n=10; mean [SD] age, 21.5 [0.71] years; 7 men; all white participants) were age matched with 24 participants who had the TT genotype (mean [SD] age, 22.5 [1.59] years; 17 men; 21 white, 1 Asian, and 2 Latin American participants).
The CT group demonstrated greater activation when alcohol was contrasted with inactive (ie, rest) and active (ie, litchi juice) appetitive controls in the NAcc, VMPFC, VTA, and OFC compared with the TT group (P < .05) (Figure 3). Pearson product moment correlations between peak activity in these regions and subjective measures indicated several significant findings. In the CT group, the alcohol use disorder score, measured using the AUDIT, was significantly correlated with activation of the NAcc (r = 0.83, P = .003) and the VMPFC (r = 0.68, P = .03) using the alcohol vs active control contrast. In addition, the urge to consume alcohol in the CT group, as measured using the total AUQ score, was also significantly correlated with the VMPFC (r = 0.67, P = .03), the left OFC (r = 0.80, P = .005), and the right OFC (r = 0.62, P = .06). The only correlations that were significant in the TT group were the correlations between the left and right OFC and the AUDIT score (r = 0.42, P < .05 and r = 0.51, P = .01) (Table).
Figure 3.
Functional magnetic resonance imaging differences between cannabinoid receptor type 1 gene (CNR1) genotype groups. Greater activity is seen in the CT group compared with the TT group during the alcohol vs control condition. The peak loci of activation in each region are listed below each corresponding contrast map in terms of z scores and Talairach coordinates corresponding to the voxel with the maximum signal intensity. Significance was determined at P < .05. The color scale represents z scores. Left hemispheric activations are depicted on the left side of the images. NAcc/VS indicates nucleus accumbens/ventral striatum; OFC, orbitofrontal cortex; VMPFC, ventromedial prefrontal cortex; and VTA, ventral tegmental area.
Table.
Correlations Between Brain Activation in Response to Alcohol Cues and Alcohol Use Problem Severity and Subjective Craving
| CT Genotype Groupa | TT Genotype Groupa | |||||||
|---|---|---|---|---|---|---|---|---|
| AUDIT | AUQ | AUDIT | AUQ | |||||
| r Value | P Value | r Value | P Value | r Value | P Value | r Value | P Value | |
| NAcc | 0.83 | .003 | 0.25 | .48 | 0.36 | .10 | 0.003 | .99 |
| VTA | 0.53 | .12 | 0.50 | .14 | 0.07 | .74 | 0.15 | .48 |
| VMPFC | 0.68 | .03 | 0.67b | .03 | 0.37 | .08 | −0.17 | .43 |
| OFC | ||||||||
| Left | 0.48 | .16 | 0.80b | .005 | 0.42 | .045 | −0.11 | .60 |
| Right | 0.33 | .35 | 0.62b | .06 | 0.50 | .01 | −0.08 | .71 |
Abbreviations: AUDIT, Alcohol Use Disorder Identification Test; AUQ, Alcohol Urge Questionnaire; NAcc, nucleus accumbens; OFC, orbitofrontal cortex; VMPFC, ventromedial prefrontal cortex; VTA, ventral tegmental area.
Results of Pearson product moment correlations between peak percentage signal change within the a priori regions of interest for the alcohol taste greater than control taste contrast and self-reported craving as measured using the AUDIT and the AUQ are shown.
SHORT-TERM EFFECTS OF ALCOHOL ON SUBJECTIVE REWARD
A human laboratory study was conducted to determine whether rs2023239 was associated with the rewarding effects of alcohol. Fifty-six individuals had the TT genotype, 15 had the CT genotype, and 3 had the CC genotype for rs2023239. The individuals with the CC and CT genotypes were combined into 1 group to facilitate analyses. The first set of analyses tested for differences between the TT and CT groups on demographics and alcohol/ other drug use variables. There were no differences in self-reported ancestry. There was 1 individual with African American ancestry in the TT group; the CT group included 1 Latin American, 1 Asian, and 1 African American individual. Of the TT group, 50% smoked tobacco, and of the CT group, 54% smoked tobacco. There were no significant differences (P > .05) between the TT and CT groups in mean (SD) age (21.6 [3] years vs 22.4 [3] years), sex (66% vs 79% male), or mean (SD) past-month quantity of alcohol use measured using a 30-day timeline follow-back method (72 [50] vs 72 [41] standard drinks). Mean breath alcohol levels after each of the 3 drinks were 0.018%, 0.038%, and 0.055% and did not differ by genotype. To ensure that population stratification was not a confounding factor, analyses were repeated with only the white individuals. No differences emerged.
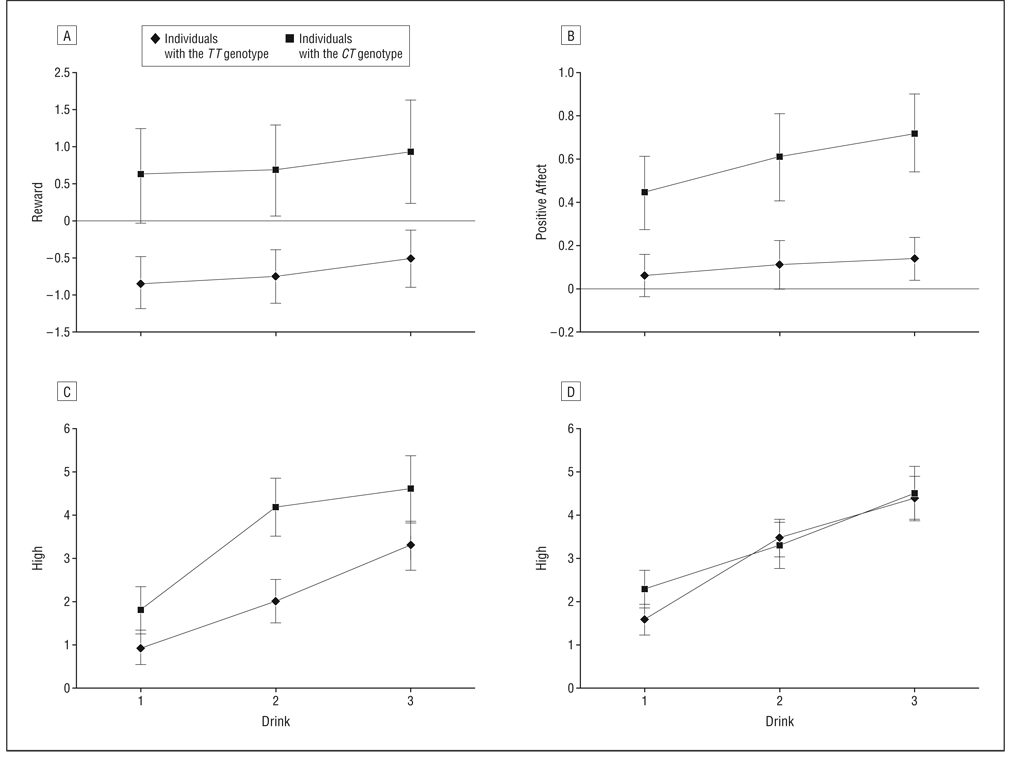
The primary analyses focused on the reward and positive affect scales of the Profile of Mood States. The analyses involved a 2 (genotype: TT vs CT or CC) × 3 (drink: 1 vs 2 vs 3) repeated-measures ANOVA. The dependent variable was the difference between the alcohol and placebo beverage scores for each drink. Analyses revealed a significant main effect for genotype (F1,69 = 4.27, P <.05) such that individuals with the CT genotype reported significantly greater reward and positive affect after drinking (F1,69 = 6.27, P < .05) (Figure 4A and B).
Figure 4.
Short-term effects of alcohol on subjective reward for each genotype group. Individuals with the CT genotype demonstrated significantly greater mean subjective reward (A) and positive affect (B) after alcohol consumption. In a replication and extension of this work, genotype was a significant moderator of the effect of medication on subjective high such that individuals with the CT genotype reported subjective high in the cyproheptadine hydrochloride (control) condition (C) but not in the olanzapine condition (D). Error bars represent SE.
To determine whether these results could be replicated with an earlier study, data from a previously published study33 were reanalyzed. This previous study allowed us to examine the interaction between a medication that targets the dopamine system (olanzapine) and rs2023239. The analyses involved a 2 (medication: olanzapine vs cyproheptadine hydrochloride) × 2 (genotype: TT vs CT and CC) × 3 (drink: 1 vs 2 vs 3) repeated-measures ANOVA. The analyses revealed a genotype × drink interaction (F2,112 = 5.19, P = .01) such that individuals with the CT genotype reported greater reward from the alcoholic beverages. There were no significant genotype × medication interactions on this measure (P > .05). In lieu of positive affect, we examined self-reported high. The analyses revealed a significant medication × genotype × drink interaction on self-reported high (F2,112 = 3.39, P < .05). Individuals with the CT (or CC) genotype (n = 9) who received the active control medication (cyproheptadine) reported the greatest high after the third drink (Figure 4C). There were no significant differences between individuals with the CT genotype and those with the TT genotype for the olanzapine condition (Figure 4D).
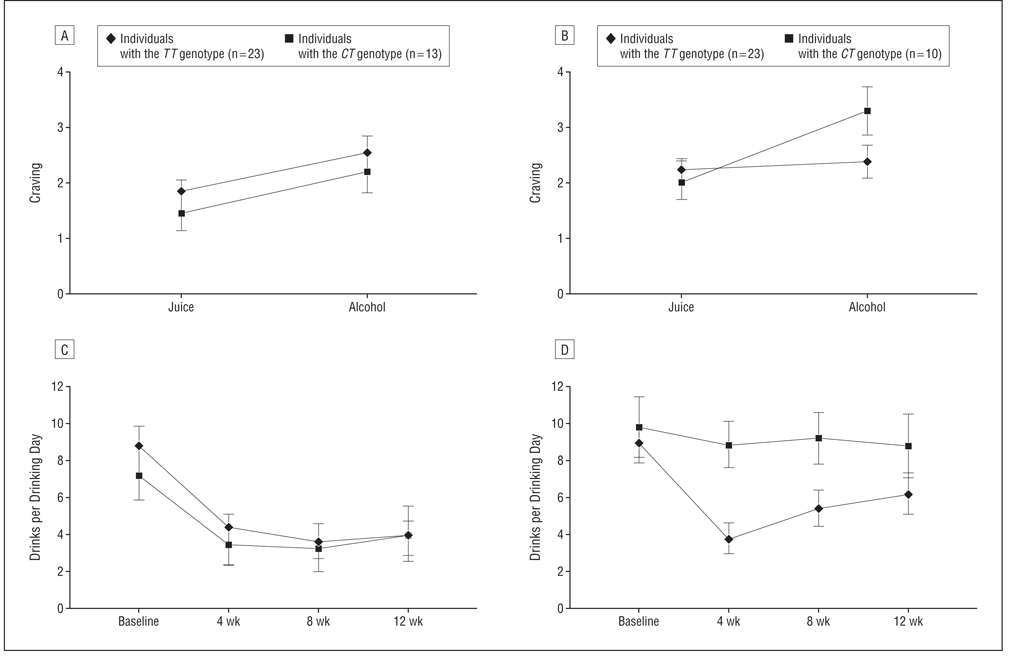
CUE-ELICITED CRAVING AND TREATMENT OUTCOME
Given the suggestion that there might be an interaction between CNR1 variation and olanzapine on the rewarding effects of alcohol, we reanalyzed data from a recent clinical trial of olanzapine.34 This study examined the effects of olanzapine (5 mg) on cue-elicited craving and drinks per drinking day during a 12-week trial in a sample of treatment-seeking alcohol-dependent individuals. In the reanalysis, rs2023239 was included as a moderator. There were 23 individuals in the CT group and 46 individuals in the TT group. The analyses revealed a significant medication × genotype × cue interaction on craving (F1,65 = 5.29, P < .05) such that individuals with the CT genotype reported greater cue-elicited craving when treated with placebo vs olanzapine (Figure 5A and B). Individuals with the CT genotype reported greater drinks per drinking day compared with individuals with the TT genotype when treated with placebo vs olanzapine (F1,65 = 3.94, P = .05) (Figure 5C and D).
Figure 5.
Cue-elicited craving and treatment outcome for the genotype × medication groups. When treated with olanzapine, there were no significant differences between individuals with the CT genotype and those with the TT genotype in mean cue-elicited craving (A). When treated with placebo, individuals with the CT genotype demonstrated significantly greater mean cue-elicited craving (B). During a 12-week trial, individuals with the CT and TT genotypes drank at similar levels when treated with olanzapine (C). In contrast, individuals with the CT genotype drank significantly more during placebo treatment (D). Error bars represent SE.
COMMENT
Frequently, studies of a genetic association lack mechanistic, translational data that link genetic variation with downstream changes in biological and behavioral phenotypes and the course of a disorder or treatment response. The present investigation was designed to translate the effects of variation in the CNR1 gene across different levels of phenotypes, from changes in receptor binding to neuronal activation after an alcohol cue challenge, to the subjective effects of alcohol consumption, and, ultimately, to treatment outcome differences. Based on previous studies suggesting that rs2023239 was the locus with the strongest association with substance abuse25 and in the region associated with differential brain activation to rewarding stimuli,29 this variation was advanced for more in-depth analysis. Analyses at the molecular level using human postmortem tissue suggest that the SNP was associated with greater CB1 receptors in critical prefrontal structures and, hence, might alter the response of the mesocorticolimbic circuitry that underlies drug-seeking behavior.
From the animal literature, it was clear that a variation in the CNR1 gene associated with increased levels of CB1 receptors in the PFC might alter the acquisition or expression of incentive salience for alcohol. To test this functional hypothesis, a neuroimaging paradigm examined the activation of mesocorticolimbic structures during exposure to the taste of an alcoholic beverage. The findings suggest that the C allele of rs2023239 is associated with greater activation of the NAcc, OFC, VTA, and VMPFC during exposure to alcohol vs either rest or control (ie, juice) cues. Not only do individuals with the CT genotype demonstrate greater activation in these key structures, but this activation (ie, the alcohol vs control contrast) is also strongly associated with alcohol use disorder and craving measures in individuals with the CT genotype. The findings from the neuroimaging study suggest that rs2023239 may be associated with changes in the mesocorticolimbic neurocircuitry, which, in turn, may mediate a change in the incentive salience of alcohol and the risk of an alcohol use disorder.
At the behavioral and clinical levels, data were analyzed from a new study and a previously published study of moderate to heavy non–treatment-seeking drinkers. In both studies, individuals with the CT genotype reported greater reward than those with the TT genotype when consuming alcohol. Specifically, individuals with the CT genotype seem to enjoy drinking alcohol more than those with the TT genotype. In addition, consistent with the neuroimaging results, there was a significant interaction with a medication that targets mesocorticolimbic neurocircuitry. These findings are also consistent with the animal studies that manipulated CB1 function and found that the CB1 receptor forms a critical link between alcohol and dopamine release in mesocorticolimbic structures. Thus, it seems that the CB1 receptor and the polymorphisms that alter the regulation of this receptor may affect the effects of alcohol on the mesocorticolimbic structures that underlie drugseeking behavior.5–17 The implication is that incentive salience may increase more rapidly with repeated exposure to alcohol in individuals with the CT genotype such that those with high levels of exposure might be expected to demonstrate greater levels of cue-elicited craving and might benefit from medications that target this neuronal circuitry.
In fact, this hypothesis was tested using data from a recent clinical trial.34 Individuals with the CT genotype demonstrated greater cue-elicited craving when treated with placebo but not when treated with a medication designed to dampen the mesocorticolimbic reactivity to cues. During a 12-week trial, alcohol-dependent individuals with the CT genotype demonstrated significant reductions in drinking during treatment with the active medication compared with placebo treatment. Conversely, individuals with the TT genotype responded equally well to the combination of placebo and psychosocial treatment vs active medication and psychosocial treatment. These findings are similar to those with the DRD4 variable number of tandem repeats reported by Hutchison and colleagues.34 Notably, χ2 tests indicated that these 2 loci were not linked in this sample.
Several limitations should be acknowledged. The sample size for the postmortem analyses is relatively small. Detecting the functional effects of genetic variation in postmortem tissue would benefit greatly from larger sample sizes. Because the results were consistent across the different studies in this article, we have confidence in these findings, although a larger sample size would be useful for providing a definitive test of the association between rs2023239 and CB1 receptor levels. Larger sample sizes in the context of the neuroimaging, behavioral, and clinical studies would also be helpful for testing the additive effects of genetic markers (eg, the DRD4 variable number of tandem repeats polymorphism33,34,49 and the μ-opioid receptor gene [OPRM1] A/G SNP50,51) that have also been linked to these phenotypes. Another commonly cited limitation is population stratification. Although it is always possible that the results may be confounded by population stratification or other third variables,52 it is highly unlikely in the present study because the participants in each of the data sets were predominantly white (approximately 95%) and the findings were consistent across multiple studies and levels of analysis. We did not use genomic controls because the cost of assaying hundreds of extra markers was high, the benefits of using genomic controls in a sample that is 95% white were uncertain,53 and a reasonable alternative was available (ie, using self-reported ancestry as a covariate). Finally, future studies may benefit from testing additional loci in CNR1. A recent study26 used a haplotype approach to identify 2 SNPs that are associated with alcohol and drug dependence, 1 of which is linkage disequilibrium with rs2023239.
Overall, these findings suggest that individuals with the CT genotype may carry a genetic vulnerability that affects CB1 receptor levels in the mesocorticolimbic structures that underlie the rewarding effects of alcohol and the attribution of incentive salience to alcohol cues. The neuroimaging data, specifically the correlations between blood oxygenation level–dependent activation and alcohol use problems, suggest that the increased reactivity of these structures in response to alcohol cues may play an important role in the pathogenesis of alcohol dependence for these individuals. For individuals without a genetic load for increased reactivity to cues, other factors may be more influential in the pathogenesis of alcohol dependence. Likewise, the treatment study is consistent with the notion that individuals with this genetic risk may benefit most from a treatment that targets mesocorticolimbic reactivity, whereas individuals without this genetic risk may benefit minimally from this type of treatment.
This last point illustrates the promise of a translational approach. Although the etiologic end point may be the same (eg, alcohol dependence), the pathogenesis may differ from one individual to another. Ultimately, there may be several different trajectories that lead to alcohol dependence, guided by differences in the underlying neurobiologic mechanisms. These differences provide important clues regarding the most effective approach to treatment. Although traditional association studies are valuable, translational approaches facilitate the discovery of the neurobiologic mechanisms that mediate the effect of genetic variation on the development of a disorder and the development of more effective treatment approaches. With translational data, it is possible to advance a conceptualization of how genetic variation may affect the neurobiologic mechanisms of alcohol dependence.
Acknowledgments
Funding/Support: This study was supported by grant AA012238 from the National Institute on Alcoholism and Alcohol Abuse (Dr Hutchison) and grant DA14369 from the National Institute on Drug Abuse (Dr Stitzel). Tissues were received from the New South Wales Tissue Resource Centre or the Prince of Wales Medical Research Institute Tissue Resource Centre, which is supported by the National Health and Medical Research Council of Australia, the University of Sydney, the Prince of Wales Medical Research Institute, the Neuroscience Institute of Schizophrenia and Allied Disorders, the National Institute of Alcohol Abuse and Alcoholism, and the New South Wales Department of Health.
Footnotes
Financial Disclosure: None reported.
REFERENCES
- 1.Rodríguez de Fonseca F, Del Arco I, Bermudez-Silva FJ, Bilbao A, Cippitelli A, Navarro M. The endocannabinoid system: physiology and pharmacology. Alcohol Alcohol. 2005;40(1):2–14. doi: 10.1093/alcalc/agh110. [DOI] [PubMed] [Google Scholar]
- 2.Colombo G, Serra S, Vacca G, Carai MA, Gessa GL. Endocannabinoid system and alcohol addiction: pharmacological studies. Pharmacol Biochem Behav. 2005;81(2):369–380. doi: 10.1016/j.pbb.2005.01.022. [DOI] [PubMed] [Google Scholar]
- 3.Hungund BL, Basavarajappa BS. Role of endocannabinoid and cannabinoid CB1 receptors in alcohol-related behaviors. Ann N Y Acad Sci. 2004;1025:515–527. doi: 10.1196/annals.1316.064. [DOI] [PubMed] [Google Scholar]
- 4.Egerton A, Allison C, Brett RR, Pratt JA. Cannabinoids and prefrontal cortical function: insights from preclinical studies. Neurosci Biobehav Rev. 2006;30(5):680–695. doi: 10.1016/j.neubiorev.2005.12.002. [DOI] [PubMed] [Google Scholar]
- 5.Maldonado R, Valverde O, Berrendero F. Involvement of the endocannabinoid system in drug addiction. Trends Neurosci. 2006;29(4):225–232. doi: 10.1016/j.tins.2006.01.008. [DOI] [PubMed] [Google Scholar]
- 6.De Vries TJ, Schoffelmeer AN. Cannabinoid CB1 receptors control conditioned drug seeking. Trends Pharmacol Sci. 2005;26(8):420–426. doi: 10.1016/j.tips.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 7.Kalivas PW, Volkow ND. The neural basis of addiction: a pathology of motivation and choice. Am J Psychiatry. 2005;162(8):1403–1413. doi: 10.1176/appi.ajp.162.8.1403. [DOI] [PubMed] [Google Scholar]
- 8.Economidou D, Mattioli L, Cifani C, Perfumi M, Massi M, Cuomo V, Trabace L, Ciccioppo R. Effect of the cannabinoid CB1 receptor antagonist SR-141716A on ethanol self-administration and ethanol-seeking behaviour in rats. Psychopharmacology (Berl) 2006;183(4):394–403. doi: 10.1007/s00213-005-0199-9. [DOI] [PubMed] [Google Scholar]
- 9.Colombo G, Agabio R, Fa M, Guano L, Lobina C, Loche A, Reali R, Gessa GL. Reduction of voluntary ethanol intake in ethanol-preferring sP rates by the cannabinoid antagoinst SR-141716. Alcohol Alcohol. 1998;33(2):126–130. doi: 10.1093/oxfordjournals.alcalc.a008368. [DOI] [PubMed] [Google Scholar]
- 10.Gallate JE, McGregor IS. The motivation for beer in rats: effects of ritanserin, naloxone and SR 141716. Psychopharmacology (Berl) 1999;142(3):302–308. doi: 10.1007/s002130050893. [DOI] [PubMed] [Google Scholar]
- 11.Gessa GL, Serra S, Vacca G, Carai MA, Colombo G. Suppressing effect of the cannabinoid CB1 receptor antagonist, SR147778, on alcohol intake and motivational properties of alcohol in alcohol-preferring sP rats. Alcohol Alcohol. 2005;40(1):46–53. doi: 10.1093/alcalc/agh114. [DOI] [PubMed] [Google Scholar]
- 12.Lallemand F, Soubrie PH, De Witte PH. Effects of CB1 cannabinoid receptor blockade on ethanol preference after chronic ethanol administration. Alcohol Clin Exp Res. 2001;25(9):1317–1323. [PubMed] [Google Scholar]
- 13.Arnone M, Maruani J, Chaperon F, Thiébot MH, Poncelet M, Soubrié P, Le Fur G. Selective inhibition of sucrose and ethanol intake by SR 141716, an antagonist of central cannabinoid (CB1) receptors. Psychopharmacology (Berl) 1997;132(1):104–106. doi: 10.1007/s002130050326. [DOI] [PubMed] [Google Scholar]
- 14.De Vries TJ, Shaham Y, Homberg JR, Crombag H, Schuurman K, Dieben J, Vander-schuren LJ, Schoffelmeer AN. A cannabinoid mechanism in relapse to cocaine seeking. Nat Med. 2001;7(10):1151–1154. doi: 10.1038/nm1001-1151. [DOI] [PubMed] [Google Scholar]
- 15.De Vries TJ, Homberg JR, Binnekade R, Raaso H, Schoffelmeer AN. Cannabinoid modulation of the reinforcing and motivational properties of heroin and heroin-associated cues in rats. Psychopharmacology (Berl) 2003;168(1–2):164–169. doi: 10.1007/s00213-003-1422-1. [DOI] [PubMed] [Google Scholar]
- 16.De Vries TJ, de Vries W, Janssen MC, Schoffelmeer AN. Suppression of conditioned nicotine and sucrose seeking by the cannabinoid-1 receptor antagonist SR141716A. Behav Brain Res. 2005;161(1):164–168. doi: 10.1016/j.bbr.2005.02.021. [DOI] [PubMed] [Google Scholar]
- 17.Colombo G, Serra S, Brunetti G, Gomez R, Melis S, Vacca G, Carai MM, Gessa L. Stimulation of voluntary ethanol intake by cannabinoid receptor agonists in ethanol-preferring sP rats. Psychopharmacology (Berl) 2002;159(2):181–187. doi: 10.1007/s002130100887. [DOI] [PubMed] [Google Scholar]
- 18.Poncelet M, Maruani J, Calassi R, Soubrie P. Overeating, alcohol and sucrose consumption decrease in CB1 receptor deleted mice. Neurosci Lett. 2003;343(3):216–218. doi: 10.1016/s0304-3940(03)00397-5. [DOI] [PubMed] [Google Scholar]
- 19.Hungund BL, Szakall I, Adam A, Basavarajappa BS, Vadasz C. Cannabinoid CB1 receptor knockout mice exhibit markedly reduced voluntary alcohol consumption and lack alcohol-induced dopamine release in the nucleus accumbens. J Neurochem. 2003;84(4):698–704. doi: 10.1046/j.1471-4159.2003.01576.x. [DOI] [PubMed] [Google Scholar]
- 20.Thanos PK, Dimitrakakis ES, Rice O, Gifford A, Volkow ND. Ethanol self-administration and ethanol conditioned place preference are reduced in mice lacking cannabinoid CB1 receptors. Behav Brain Res. 2005;164(2):206–213. doi: 10.1016/j.bbr.2005.06.021. [DOI] [PubMed] [Google Scholar]
- 21.Houchi H, Babovic D, Pierrefiche O, Ledent C, Daoust M, Naassila M. CB1 receptor knockout mice display reduced ethanol-induced conditioned place preference and increased striatal dopamine D2 receptors. Neuropsychopharmacology. 2005;30(2):339–349. doi: 10.1038/sj.npp.1300568. [DOI] [PubMed] [Google Scholar]
- 22.Racz I, Bilkei-Gorzo A, Toth ZE, Michel K, Palkovits M, Zimmer A. A critical role for the cannabinoid CB1 receptors in alcohol dependence and stress-stimulated ethanol drinking. J Neurosci. 2003;23(6):2453–2458. doi: 10.1523/JNEUROSCI.23-06-02453.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cippitelli A, Bilbao A, Hansson AC, del Arco I, Sommer W, Heilig M, Massi M, Bermúdez-Silva FJ, Navarro M, Ciccocioppo R, de Fonseca FR. European TARGALC Consortium. Cannabinoid CB1 receptor antagonism reduces conditioned reinstatement of ethanol-seeking behavior in rats. Eur J Neurosci. 2005;21(8):2243–2251. doi: 10.1111/j.1460-9568.2005.04056.x. [DOI] [PubMed] [Google Scholar]
- 24.Schmidt LG, Samochowiec J, Finckh U, Fiszer-Piosik E, Horodnicki J, Wendel B, Rommelspacher H, Hoehe MR. Association of a CB1 cannabinoid receptor gene (CNR1) polymorphism with severe alcohol dependence. Drug Alcohol Depend. 2002;65(3):221–224. doi: 10.1016/s0376-8716(01)00164-8. [DOI] [PubMed] [Google Scholar]
- 25.Zhang PW, Ishiguro H, Ohtsuki T, Hess J, Carillo F, Walther D, Onaivi ES, Arinami T, Uhl GR. Human cannabinoid receptor 1: 5′ exons, candidate regulatory regions, polymorphisms, haplotypes and association with polysubstance abuse. Mol Psychiatry. 2004;9(10):916–931. doi: 10.1038/sj.mp.4001560. [DOI] [PubMed] [Google Scholar]
- 26.Zuo L, Kranzler HR, Luo X, Covault J, Gelernter J. CNR1 variation modulates risk for drug and alcohol dependence. Biol Psychiatry. 2007;62(6):616–626. doi: 10.1016/j.biopsych.2006.12.004. [DOI] [PubMed] [Google Scholar]
- 27.Preuss UW, Koller G, Zill P, Bondy B, Soyka M. Alcoholism-related phenotypes and genetic variants of the CB1 receptor. Eur Arch Psychiatry Clin Neurosci. 2003;253(6):275–280. doi: 10.1007/s00406-003-0440-7. [DOI] [PubMed] [Google Scholar]
- 28.Herman AI, Kranzler HR, Cubells JF, Gelernter J, Covault J. Association study of the CNR1 gene exon 3 alternative promoter region polymorphisms and substance dependence. Am J Med Genet B Neuropsychiatr Genet. 2006;141(5):499–503. doi: 10.1002/ajmg.b.30325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chakrabarti B, Kent L, Suckling J, Bullmore E, Baron-Cohen S. Variations in the human cannabinoid receptor (CNR1) gene modulate striatal responses to happy faces. Eur J Neurosci. 2006;23(7):1944–1948. doi: 10.1111/j.1460-9568.2006.04697.x. [DOI] [PubMed] [Google Scholar]
- 30.Steffens M, Engler C, Zentner J, Feuerstein TJ. Cannabinoid CB1 receptor-mediated modulation of evoked dopamine release and of adenylyl cyclase activity in the human neocortex. Br J Pharmacol. 2004;141(7):1193–1203. doi: 10.1038/sj.bjp.0705706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Thomas BF, Gilliam AF, Burch DF, Roche MJ, Seltzman HH. Comparative receptor binding analyses of cannabinoid agonists and antagonists. J Pharmacol Exp Ther. 1998;285(1):285–292. [PubMed] [Google Scholar]
- 32.Lowry OH, Rosebrough NJ, Farr AL, Randall RJ. Protein measurement with the Folin phenol reagent. J Biol Chem. 1951;193(1):265–275. [PubMed] [Google Scholar]
- 33.Hutchison KE, Wooden A, Swift RM, Smolen A, McGeary J, Adler L, Paris L. Olanzapine reduces craving for alcohol: a DRD4 VNTR polymorphism by pharmacotherapy interaction. Neuropsychopharmacology. 2003;28(10):1882–1888. doi: 10.1038/sj.npp.1300264. [DOI] [PubMed] [Google Scholar]
- 34.Hutchison KE, Ray L, Sandman E, Rutter MC, Peters A, Davidson D, Swift R. The effect of olanzapine on craving and alcohol consumption. Neuropsychopharmacology. 2006;31(6):1310–1317. doi: 10.1038/sj.npp.1300917. [DOI] [PubMed] [Google Scholar]
- 35.Filbey FM, Claus E, Audette AR, Niculescu M, Banich MT, Tanabe J, Du YP, Hutchison KE. Exposure to the taste of alcohol elicits robust activation of the mesocorticolimbic neurocircuitry. Neuropsychopharmacology. 2008;33(6):1391–1401. doi: 10.1038/sj.npp.1301513. [published online ahead of print July 25, 2007], doi:10.1038/sj.npp.1301513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Barbor TF, Higgins-Biddle JC, Saunders JB, Monteiro MGb. AUDIT: The Alcohol Use Disorders Identification Test: Guidelines for Use in Primary Care. 2nd ed. Geneva, Switzerland: World Health Organization; 2006. [Google Scholar]
- 37.Bohn MJ, Krahn DD, Staehler BA. Development and initial validation of a measure of drinking urges in abstinent alcoholics. Alcohol Clin Exp Res. 1995;19(3):600–606. doi: 10.1111/j.1530-0277.1995.tb01554.x. [DOI] [PubMed] [Google Scholar]
- 38.Schneider W, Eschman A, Zuccolotto A. E-Prime User’s Guide. Pittsburgh, PA: Psychology Software Tools Inc; 2002. [Google Scholar]
- 39.Smith SM. Fast robust automated brain extraction. Hum Brain Mapp. 2002;17(3):143–155. doi: 10.1002/hbm.10062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Woolrich MW, Ripley BD, Brady M, Smith SM. Temporal autocorrelation in univariate linear modeling of FMRI data. Neuroimage. 2001;14(6):1370–1386. doi: 10.1006/nimg.2001.0931. [DOI] [PubMed] [Google Scholar]
- 41.Beckmann CF, Jenkinson M, Smith SM. General multilevel linear modeling for group analysis in FMRI. Neuroimage. 2003;20(2):1052–1063. doi: 10.1016/S1053-8119(03)00435-X. [DOI] [PubMed] [Google Scholar]
- 42.Woolrich MW, Behrens TE, Beckmann CF, Jenkinson M, Smith SM. Multilevel linear modeling for fMRI group analysis using Bayesian inference. Neuroimage. 2004;21(4):1732–1747. doi: 10.1016/j.neuroimage.2003.12.023. [DOI] [PubMed] [Google Scholar]
- 43.Worsley KJ, Evans AC, Marrett S, Neelin P. A three-dimensional statistical analysis for CBF activation studies in human brain. J Cereb Blood Flow Metab. 1992;12(6):900–918. doi: 10.1038/jcbfm.1992.127. [DOI] [PubMed] [Google Scholar]
- 44.McNair DM, Lorr M, Droppleman LF. Profile of Mood States. San Diego, CA: Educational & Industrial Testing Service; 1971. [Google Scholar]
- 45.Project MATCH Research Group. Matching alcoholism treatments to client heterogeneity: treatment main effects and matching effects on drinking during treatment. J Stud Alcohol. 1998;59(6):631–639. doi: 10.15288/jsa.1998.59.631. [DOI] [PubMed] [Google Scholar]
- 46.Monti PM, Rohsenow DJ, Swift RM, Gulliver SB, Colby SM, Mueller TI, Brown RA, Gordon A, Abrams DB, Niaura RS, Asher MK. Naltrexone and cue exposure with coping and communication skills training for alcoholics: treatment process and 1-year outcomes. Alcohol Clin Exp Res. 2001;25(11):1634–1647. [PubMed] [Google Scholar]
- 47.Killeen TK, Brady KT, Gold PB, Tyson C, Simpson KN. Comparison of self-report versus agency records of service utilization in a community sample of individuals with alcohol use disorders. Drug Alcohol Depend. 2004;73(2):141–147. doi: 10.1016/j.drugalcdep.2003.09.006. [DOI] [PubMed] [Google Scholar]
- 48.Sobell LC, Sobell MB. An approach to increasing confidence in treatment outcome conclusions with alcohol and drug abusers. In: Sobell LC, Sobell MB, Ward E, editors. Evaluating Alcohol and Drug Abuse Treatment Effectiveness: Recent Advances. New York, NY: Pergamon Press; 1980. pp. 177–183. [Google Scholar]
- 49.Hutchison KE, McGeary J, Smolen A, Bryan A, Swift RM. The DRD4 VNTR polymorphism moderates craving after alcohol consumption. Health Psychol. 2002;21(2):139–146. [PubMed] [Google Scholar]
- 50.Ray LA, Hutchison KE. A polymorphism of the μ-opioid receptor gene (OPRM1) and sensitivity to the effects of alcohol in humans. Alcohol Clin Exp Res. 2004;28(12):1789–1795. doi: 10.1097/01.alc.0000148114.34000.b9. [DOI] [PubMed] [Google Scholar]
- 51.Ray LA, Hutchison KE. Effects of naltrexone on alcohol sensitivity and genetic moderators of medication response: a double-blind placebo-controlled study. Arch Gen Psychiatry. 2007;64(9):1069–1077. doi: 10.1001/archpsyc.64.9.1069. [DOI] [PubMed] [Google Scholar]
- 52.Hutchison KE, Stallings M, McGeary J, Bryan A. Population stratification in the candidate gene study: fatal threat or red herring? Psychol Bull. 2004;130(1):66–79. doi: 10.1037/0033-2909.130.1.66. [DOI] [PubMed] [Google Scholar]
- 53.Wellcome Trust Case Control Consortium. Genome-wide association study of 14,000 cases of seven common diseases and 3,000 shared controls. Nature. 2007;447(7145):661–678. doi: 10.1038/nature05911. [DOI] [PMC free article] [PubMed] [Google Scholar]