Abstract
Aim
Survival after out-of-hospital cardiac arrest (OOHCA) varies between regions, but the contribution of different factors to this variability is unknown. This study examined whether survival to hospital discharge was related to receiving hospital characteristics, including bed number, capability of performing cardiac catheterization and hospital volume of OOHCA cases.
Material and Methods
Prospective observational database of non-traumatic OOHCA assessed by emergency medical services was created in 8 US and 2 Canadian sites from December 1, 2005 to July 1, 2007. Subjects received hospital care after OOHCA, defined as either (1) arriving at hospital with pulses, or (2) arriving at hospital without pulses, but discharged or died ≥ 1 day later.
Results
A total of 4087 OOHCA subjects were treated at 254 hospitals, and 32% survived to hospital discharge. A majority of subjects (68%) were treated at 116 (46%) hospitals capable of cardiac catheterization. Unadjusted survival to discharge was greater in hospitals performing cardiac catheterization (34% versus 27%, p=0.001), and in hospitals that received ≥40 patients / year compared to those that received <40 (37% vs 30%, p=0.01). Survival was not associated with hospital bed number, teaching status or trauma center designation. Length of stay (LOS) for surviving subjects was shorter at hospitals performing cardiac catheterization (p<0.01).After adjusting for all variables, there were no independent associations between survival or LOS and hospital characteristics.
Conclusions
Some subsets of hospitals displayed higher survival and shorter LOS for OOHCA subjects but there was no independent association between hospital characteristics and outcome.
Out-of-hospital cardiac arrest (OOHCA) has an incidence of 52.1 per 100,000 population, making it the third-leading cause of death in North America [1]. Survival after OOHCA treated by emergency medical services (EMS) is about 7.9%, but varies greatly between sites and regions (median 8.4%, ranging between 3.0% – 16.3%) [1]. This large variation in survival is associated with differences in the characteristics of both patients, circumstances of arrest, and with EMS or hospital systems of care. The relative contributions of these factors to survival are unknown.
One possible influence on patient survival is the level of care received in the hospital after successful resuscitation by EMS. For example, specific interventions such as hypothermia [2,3] and multidisciplinary changes in hospital care [4,5] produced two-fold increases in survival after OOHCA. Several papers have suggested the existence of hospital-related differences in survival after OOHCA [6–9]. Observational studies suggest that early percutaneous coronary intervention can improve outcomes after cardiac arrest [10,11]. However, the association between specific characteristics of hospitals and survival after OOHCA is unknown.
Most hospitals treat few post-cardiac arrest patients [6]. Therefore, it is difficult to compare individual hospital survival rates. However, in a large database, survival can be compared between categories of hospitals. The Resuscitations Outcome Consortium (ROC) developed and implemented a prospective, EMS-based registry to describe processes of care and outcome of patients assessed by EMS for OOHCA [12]. The present study used this database to test the hypothesis that survival to hospital discharge was associated with characteristics of receiving hospitals, including size (bed number), capability of performing cardiac catheterization, and total volume of OOHCA patients received.
METHODS
Data were obtained from the ROC Cardiac Arrest Epidemiological Registry or “Epistry” which has been described in detail previously [12]. This registry is a prospective database of all persons evaluated for OOHCA by participating EMS agencies. Over 250 EMS agencies at sites in Canada and the US contribute data on an ongoing basis. Multiple mechanisms for surveillance are used at local sites to assure investigators of capture of all appropriate cases. Data are abstracted from EMS records and hospital records by data coordinators who use common data definitions. Data are transmitted to a central coordinating center by web-entry into an electronic database or batch upload of multiple cases grouped together. Within-form error checks are used to decrease data entry errors.
Subjects included were OOHCA patients of any age who received hospital care. “Cardiac arrest” was defined as receiving either (1) chest compressions by professional responder (paramedic, first-responder or other health professional arriving as part of the organized EMS response), or (2) rescue shock by professional responder or a bystander using an automated external defibrillator (AED). Cardiac arrest cases that were associated with trauma were excluded. “Received hospital care” was defined as either (1) arrived at the hospital with pulses, or (2) arrived at the hospital without documented pulses, but was discharged or died > 1 day later (i.e. was not pronounced dead on arrival at the hospital). When the subject was delivered to one hospital, and transferred to a second hospital on the same day, the second hospital was considered to be the treating hospital. These definitions were selected in order to exclude cases of EMS-treated OOHCA who never had restoration of pulses, and therefore who were not exposed to in-hospital post-resuscitation care. Subjects were entered into the database between December 1, 2005 and July 1, 2007, a time-period that excludes any interventional ROC trials.
Hospital characteristics were obtained from three sources. First, the EMS Structures Survey collected standardized data from each ROC site completed by local investigators who described the local hospitals that receive patients from their EMS systems [13]. Second, the American Hospital Directory is a publicly available database on US hospitals that is collated from a variety of public and payor databases (Medicare, licensed beds) (www.ahd.com). Third, the 2006–2007 Guide to Canadian Healthcare Facilities is a collation of data on Canadian hospitals provided by member hospitals (Volume 14, 2006–2007, www.cha.ca). Investigators examined the data from all three sources for each hospital that received subjects in the Epistry database in order to collate hospital characteristics. In the event of discrepancies, the report of local investigators who were familiar with the local hospital was used.
Hospitals were categorized based on several characteristics. Number of beds was used to categorize hospitals as large (>400 beds), medium (251–400 beds), and small (<250 beds). Capacity to perform acute cardiovascular interventions was defined as the presence of a cardiac catheterization laboratory, but the databases did not distinguish between capacity to perform emergent and elective catheterization or PCI. Trauma center designation was categorized as Level 1, Level 2, or non-trauma center. A teaching hospital was defined as one that listed active residency programs based at that hospital.
Patient and arrest characteristics were tabulated with descriptive statistics and compared between the number of hospital beds (size category) and cardiac catheterization capabilities of hospitals. Sample sizes within cardiac catheterization designation were similar across the different hospital size categories. Chi-Square tests examined the independent association of hospital size category and catheterization capability with the primary outcome, survival to hospital discharge. Hospital length of stay was considered as a secondary outcome.
To account for known potential confounders, we used multiple logistic regression to examine the association of hospital type and survival to hospital discharge. We adjusted for variables previously associated with outcome: site; hospital characteristics including trauma level designation (1,2, non-trauma), teaching institution; patient characteristics including gender, age (<1, 1–11, 12–19, 20–39, 40–60, 61–75, >75, unknown), witnessed collapse (witnessed, unwitnessed, or unknown), initial ECG rhythm (VT/VF, PEA, asystole, AED no-shock, or cannot determine), bystander attempts at cardiopulmonary resuscitation (CPR), and EMS process characteristics including response time (time from call to dispatch to first EMS vehicle arrival at scene). Variables were considered significantly associated with the outcome if p < 0.05.
In order to describe the relationship between hospital volume of OOHCA patients and outcome, we plotted survival versus annualized number of cardiac arrests in the database for all hospitals. To avoid bias against hospitals with small volumes of cardiac arrest patients (<10 post-cardiac arrest patients a year), this analysis included all hospitals, regardless of size.
Analyses of data were performed in S-Plus, v 6.2 (TIBCO Software, Palo Alto CA) or STATA v9.1 (StataCorp LP, College Station TX).
RESULTS
Complete data were available from 8 sites in the US and 2 in Canada. EMS agencies delivered subjects to a total of 254 hospitals (144 in US and 110 in Canada). The distribution of hospital sizes was similar in the US and Canada (Table 1). A larger proportion of US hospitals performed cardiac catheterization and maintained residency programs than Canadian hospitals (Table 1). About 48% of hospitals reported being able to perform cardiac catheterization. Similar proportions of hospitals were designated Level 1 or 2 Trauma Centers in both US and Canada.
TABLE 1.
Study hospital characteristics between US and Canadian ROC sites.
| All Hospitals (n=254) | Canadian Hospitals (n=110) |
US Hospitals (n=144) | |
|---|---|---|---|
| Number of Beds | |||
| ≤100 | 42 (16.5%) | 21 (19.1%) | 21 (14.6%) |
| 101–200 | 60 (23.6%) | 19 (17.3%) | 41 (28.5%) |
| 201–300 | 49 (19.3%) | 16 (14.5%) | 33 (22.9%) |
| 301–400 | 32 (12.6%) | 16 (14.5%) | 16 (11.1%) |
| > 400 | 46 (18.1 %) | 24 (21.8%) | 22 (15.3%) |
| Missing Bed Number | 25 (9.8%) | 14 (12.7%) | 11 (7.6%) |
| Catheterization Laboratory | 140 (55.1%) | 27 (24.5%) | 113 (78.5%)* |
| Electrophysiology Laboratory | 38 (15.0%) | 17 (16%) | 21 (15%) |
| Trauma Level 1 | 36 (14%) | 17 (16%) | 19 (13%) |
| Trauma Level 2 | 19 (8%) | 10 (9%) | 9 (6%) |
| Residency Program | 111 (44%) | 33 (30%) | 78 (54%)* |
p<0.05 between US and Canadian hospitals
During this time interval, EMS treated 28,974 OOHCA cases and transported 10,496 cases to a hospital. Among these, 163 subjects (1.6%) were transported to hospitals outside of the surveillance area of the database, and no further information is available for those subjects. Of the remaining 10,333 subjects, 2395 (22.8%) had pulses at ED arrival while an additional 1767 (16.8%) did not have a pulse upon ED arrival or lacked EMS documentation of a pulse, but died or were discharged ≥1 days later. Survival data or other key data were missing for 75 cases (1.8%), leaving a total of 4087 subjects who received hospital care after OOHCA. Overall survival to hospital discharge for the 4087 patients who received hospital care was 32%.
A larger proportion of subjects delivered to the hospital with pulses or hospitalized >1 day were treated at large (37%) versus medium (29%) and small (29%) hospitals (Table 2). Overall, 68% of subjects were treated at hospitals with cardiac catheterization capabilities. Hospitalized subjects were more often male and had an initial ECG rhythm of ventricular fibrillation or ventricular tachycardia (VF/VT) (Table 3). Median length of stay was longer in patients who survived to discharge (Table 4). For surviving patients, length of stay was longer at hospitals without cardiac catheterization capabilities (p<0.01). This association was confounded by the fact that more Canadian hospitals, which have different incentive for length of stay, lacked cardiac catheterization capability. In a multivariable regression adjusting for country, initial VF/VT rhythm, age and witnessed collapse, the length of stay was not significantly associated with cardiac catheterization capability (0.18, 95%CI −1.47,1.82), medium size (0.41, 95%CI −1.12,1.95) or large size (0.32, 95%CI −1.28, 1.92).
TABLE 2.
Distribution of subjects and hospitals defined by number of beds and cardiac catheterization (CATH) availability.
| Small (≤250 beds) |
Medium (251–400 beds) |
Large (>400 beds) |
Missing ** |
Total | |
|---|---|---|---|---|---|
| CATH | |||||
| Subjects (N) | 963 | 790 | 897 | 137 | 2787 |
| Hospitals (N) | 50 | 30 | 31 | 6 | 117 |
| No CATH | |||||
| Subjects (N) | 529 | 396 | 277 | 98 | 1300 |
| Hospitals (N) | 51 | 17 | 12 | 6 | 86 |
| Missing ** | |||||
| Subjects (N) | 0 | 0 | 0 | 0 | 0 |
| Hospitals (N) | 0 | 0 | 0 | 0 | 0 |
| Total | |||||
| Subjects (N) | 1492 | 1186 | 1174 | 235 | 4087 |
| Hospitals (N) | 101 | 47 | 43 | 12 | 203* |
A subset of 51 hospitals treated no subjects during the study interval.
Some subjects were transferred to hospitals for which bed number (n=235 subjects in 12 hospitals) were not known.
TABLE 3.
Characteristics of subjects versus hospital bed number and cardiac catheterization (CATH) capability. Designations are the same as in TABLE 2.
| Total N=4087 |
Large CATH N=897 |
Medium CATH N=790 |
Small CATH N=963 |
Large No CATH N=277 |
Med No CATH N=396 |
Small No CATH N=529 |
|
|---|---|---|---|---|---|---|---|
| Median Age in years (IQR) | 66 (25) | 65 (27) | 62 (23) | 65 (24) | 71 (22) | 69 (24) | 68 (22) |
| %Male | 63% | 62% | 64% | 60% | 62% | 64% | 64% |
| Median Interval Dispatch to EMS Arrival in min (IQR) | 5.0 (3.0) | 5.0 (3.0) | 5.0 (2.0) | 5.0 (2.0) | 6.0 (2.0) | 5.0 (3.0) | 6.0 (3.0) |
| Initial ECG Rhythm | |||||||
| VF/VT | 41% | 40% | 37% | 41% | 44% | 44% | 40% |
| PEA | 23% | 21% | 26% | 27% | 14% | 16% | 24% |
| Asystole | 22% | 21% | 24% | 22% | 28% | 23% | 19% |
| Witnessed Collapse | |||||||
| EMS | 14% | 13% | 14% | 13% | 16% | 12% | 13% |
| Bystander | 51% | 51% | 48% | 50% | 55% | 54% | 52% |
| None | 29% | 26% | 28% | 28% | 29% | 33% | 31% |
TABLE 4.
Hospital length of stay by hospital bed number and cardiac catheterization (CATH) capability.
| Total N=4087 |
Large CATH N=897 |
Medium CATH N=790 |
Small CATH N=963 |
Large No CATH N=277 |
Medium No CATH N=396 |
Small No CATH N=529 |
|
|---|---|---|---|---|---|---|---|
| Length of Stay - All Subjects Median (IQR) days | 3.0 (8.0) |
3.0 (8.0) |
4.0 (8.0) |
3.0 (7.0) |
2.0 (7.0) |
3.0 (8.3) |
2.5 (7.0) |
| Length of Stay – Discharged Alive Median (IQR) days | 10.0 (12.0) |
11.0 (13.8) |
9.0 (9.0) |
8.0 (9.0) |
16.0 (20.0) |
15.5 (27.8) |
12.0 (13.0) |
| Length of Stay – Died in Hospital Median (IQR) days | 1.0 (3.0) |
2.0 (3.0) |
2.0 (4.0) |
1.0 (3.0) |
1.0 (3.0) |
1.0 (3.0) |
1.0 (3.0) |
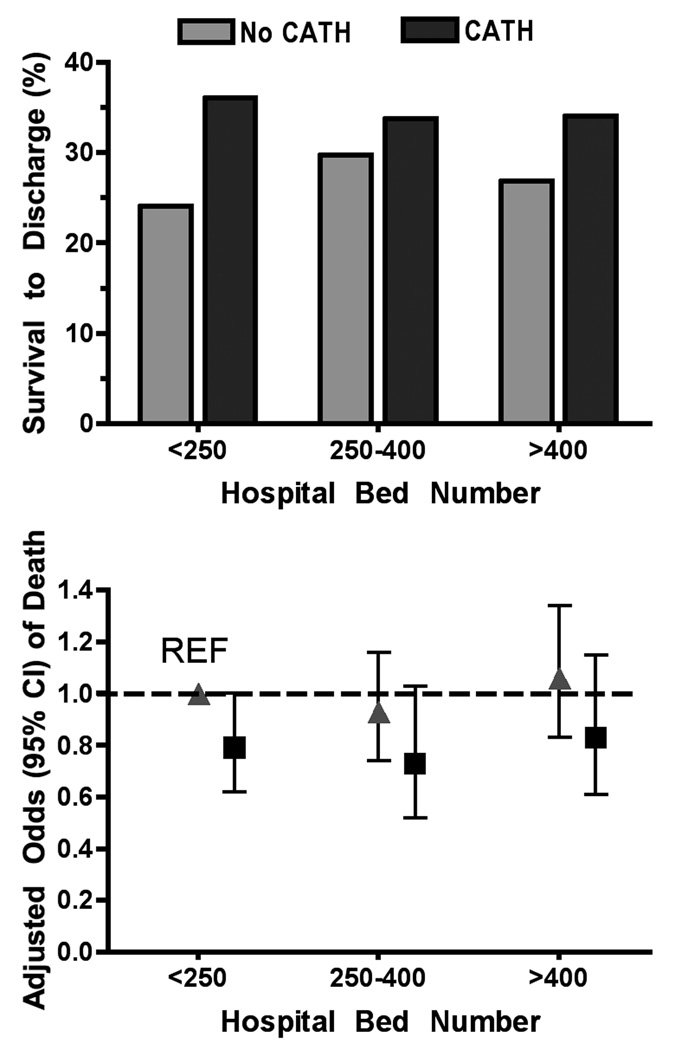
Survival to hospital discharge had a significant univariable relationship with the availability of cardiac catheterization (OR = 1.43 95% CI 1.26–1.61, p<0.001). Survival to hospital discharge was greater in hospitals with cardiac catheterization capability than those without (34% versus 29%) (FIGURE 1). This association was more prominent in small (<250 bed) hospitals (36% vs. 27%), than in medium (34% vs. 30%) or large hospitals (33% vs. 25%). Number of hospital beds did not have a significant relationship with survival (p=0.67).
FIGURE 1.
Survival to discharge was greater in CATH than in no CATH hospitals regardless of bed number. Odds of death (triangles=No CATH; squares=CATH) were adjusted for witnessed collapse, VF/VT, and age.
Subject characteristics associated with survival in the multivariable logistic model included an initial rhythm of VF/VT, younger age, and witnessed collapse (p<0.001). After adjusting for all covariates, the odds of death in a hospital with cardiac catheterization capabilities versus a hospital without cardiac catheterization was 0.79 (95% CI 0.62–1.001). The odds of death relative to a small hospital was 0.92 (95% CI 0.74–1.15) for medium-sized hospitals and 1.05 (95% CI 0.83–1.34) for large hospitals. Survival rates did vary by volume of cardiac arrest cases treated (Table 5) with a high of 37.3% in hospitals with an annualized enrollment of ≥40 ROC patients a year and a low of 28.3% in hospitals with an annualized enrollment of 30–39 ROC patients a year. Survival was associated with case volume (Chi-Square =9.8, p=0.04), but this relationship was attenuated when odds of death were adjusted for all covariates (Table 5).
TABLE 5.
Outcomes by hospital volume of OOHCA cases. Hospitals with no treated cases (n=51) are excluded.
| Yearly ROC Cases | Number of Hospitals | Survival to Discharge (%) | Adjusted Odds of Death (95% CI) |
|---|---|---|---|
| 1–9 | 103 | 28.7% | Reference |
| 10–19 | 55 | 30.8% | 0.85 (0.65, 1.12) |
| 20–29 | 23 | 32.6% | 0.89 (0.65, 1.21) |
| 30–39 | 11 | 28.3% | 1.04 (0.75, 1.45) |
| ≥40 | 11 | 37.3% | 0.91 (0.67, 1.25) |
Adjusted for witnessed collapse, VF/VT, age and cardiac catheterization capability.
DISCUSSION
After resuscitation by EMS or in the ED after OOHCA, the unadjusted probability of survival to discharge is associated with care at a hospital capable of cardiac catheterization or treating ≥40 OOHCA patients annually. Mean length of stay is also shorter for patients hospitalized at hospitals capable of cardiac catheterization. The characteristics of patients delivered to different categories of hospitals do not differ, but after adjusting for response and patient characteristics, there was no independent association between survival and hospital characteristics. Therefore, it remains unclear whether EMS selection results in preferential transport of patients more or less likely to survive to specific hospitals. These data suggest some predilection for the most viable post-cardiac arrest patients to be treated at hospitals capable of cardiac catheterization.
The principal limitation of this study is that we are unable to describe whether therapeutic hypothermia, cardiac catheterization or other procedures were actually applied to individual patients. Cardiac catheterization availability may be surrogate for a more comprehensive cardiac and critical care program. Future studies should examine the influence of specific in-hospital procedures and therapies. Additional analyses with neurological and functional outcomes were not attempted because the current database lacks complete information on these measures at the time of discharge. One advantage of this prospective database is that future data collection can be expanded to record the actual cardiac procedures and treatment for individual subjects as well as more detailed outcomes. Those data will better answer what specific types of hospital care are associated with survival and improved outcome.
This study is also limited by the multiple out-of-hospital factors that affect patient outcome. When adjusted for all available clinical predictors, there was no significant independent effect of cardiac catheterization availability on survival. This result is similar to a recent analysis of survival after in-hospital cardiac arrest [14]. In that analysis, care at a tertiary care facility resulted in higher unadjusted survival rate, but this effect was diminished when adjusted for differences between the hospital populations. In another series, differences in survival after OOHCA between two hospital systems were attributable in large part to out-of-hospital factors [15]. Those prior studies and the present data underline the importance of optimizing multiple aspects of care, and not relying on a single aspect of the entire system of treatment, both in-hospital and out-of-hospital, in order to improve survival after cardiac arrest.
Availability of cardiac catheterization was expected to be beneficial because of the high incidence of coronary artery occlusion in out-of-hospital cardiac arrest [16,17]. Primary percutaneous coronary intervention (PCI) by experienced cardiologists is associated with superior survival and fewer complications for patients with ST-elevation myocardial infarction (STEMI) [18], and also may benefit non-STEMI patients [19–21]. This study did not directly compare early intervention to conservative management, but do indicate that post-cardiac arrest patients are currently directed towards hospitals with availability of coronary intervention.
Invasive coronary interventions may be underutilized for post-cardiac arrest patients [22]. Some authors have proposed triage and transfer of high-risk cardiac patients without cardiac arrest to cardiac centers, which are capable of primary PCI [23], and some regions also transfer patients after cardiac arrest [24]. The benefit of transfer and longer transport may only affect outcomes for selected “high-risk” STEMI patients [25], and emergent PCI may only benefit a subset of post-cardiac arrest patients [26]. Regardless, more data are required to establish whether treatment of post-cardiac arrest patients in a fashion similar to high-risk STEMI patients is beneficial.
This study adds to the discussion about whether patients with restoration of pulses after OOHCA should be transported to the nearest hospital or to specialized centers [27]. In many critical illnesses, specialized care improves outcomes [28]. For example, implementation of trauma systems is associated with improved survival after life-threatening injury [29, 30], particularly at individual trauma centers with higher volumes of cases [31]. Likewise, care of stroke patients at specialized stroke units is associated with better survival and better functional recovery, independent of reperfusion [32, 33]. Better survival in these studies was related to improved systems of care rather than single interventions. This paper helps identify the important covariates that should be measured in order to test whether similar systems of care also may benefit OOHCA.
The present data suggest that patients with greater chance of survival are being treated at larger cardiac hospitals, but cannot separate the contribution of hospital and patient characteristics. Other retrospective analyses found relationships between survival after OOHCA and different aspects of hospital care, including case volume and coronary interventions, [6, 7, 34–36]. The present analysis provided a more complete description than a previous study [6] that excluded hospitals with less than 12 patients a year, and found no independent effect of case volume. One limitation of the present analysis is the fact that some hospitals would treat post-cardiac arrest patients delivered to the hospital from sources other than ROC EMS agencies. For most facilities, the ROC database does include the majority of EMS services serving the surrounding geographical region. Thus, the volume of cardiac arrest patients used in this analysis is probably a good surrogate for total volume of post-cardiac arrest patients.
In summary, patients with restoration of pulses after out-of-hospital cardiac arrest who were treated at hospitals capable of invasive cardiac procedures and hospitals that treat a large volume of cardiac arrest patients had increased rates of survival. However, there was no independent effects of hospital characteristics after adjusting for multiple other factors associated with survival after cardiac arrest. These associations underline the need to study implementation of regional systems of care for post-cardiac arrest patients in a prospective fashion with attention to multiple important covariates. Future research should determine if these observations are robust and identify whether specific hospital procedures are associated with survival.
Acknowledgements
Funding Sources:
The ROC is supported by a series of cooperative agreements to 10 regional clinical centers and one Data Coordinating Center (5U01 HL077863, HL077881, HL077871 HL077872, HL077866, HL077908, HL077867, HL077885, HL077887, HL077873, HL077865) from the National Heart, Lung and Blood Institute in partnership with the National Institute of Neurological Disorders and Stroke, U.S. Army Medical Research & Material Command, The Canadian Institutes of Health Research (CIHR) - Institute of Circulatory and Respiratory Health, Defence Research, the American Heart Association and Development Canada and the Heart and Stroke Foundation of Canada.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest Statement
The authors do not have any direct conflicts of interest related to the topics in this paper.
A preliminary version of these data was presented at the Resuscitation Science Symposium, New Orleans, LA, November 5, 2008, and appear in abstract form in the proceedings, as:
Callaway CW, Schmicker R, Kampmeyer M, Powel J, Nichol G, Rea TD, Daya M, Aufderheide T, Davis D, Rittenberger J, Idris AH. Influence of receiving hospital characteristics on survival after cardiac arrest. Circulation 2008;118 (Supp 2):S1446.
REFERENCES
- 1.Nichol G, Thomas E, Callaway CW, Hedges J, Powell JL, Aufderheide TP, Rea T, Lowe R, Brown T, Dreyer J, Davis D, Idris A, Stiell I. Resuscitation Outcomes Consortium Investigators. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2008;300:1423–1431. doi: 10.1001/jama.300.12.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hypothermia after Cardiac Arrest Study Group. Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med. 2002;346:549–556. doi: 10.1056/NEJMoa012689. [DOI] [PubMed] [Google Scholar]
- 3.Bernard SA, Gray TW, Buist MD, Jones BM, Silvester W, Gutteridge G, Smith K. Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N Engl J Med. 2002;346:557–563. doi: 10.1056/NEJMoa003289. [DOI] [PubMed] [Google Scholar]
- 4.Sunde K, Pytte M, Jacobsen D, Mangschau A, Jensen LP, Smedsrud C, Draegni T, Steen PA. Implementation of a standardised treatment protocol for post resuscitation care after out-of-hospital cardiac arrest. Resuscitation. 2007;73:29–39. doi: 10.1016/j.resuscitation.2006.08.016. [DOI] [PubMed] [Google Scholar]
- 5.Rittenberger JC, Guyette FX, Tisherman SA, DeVita MA, Alvarez RJ, Callaway CW. Outcomes of a hospital-wide plan to improve care of comatose survivors of cardiac arrest. Resuscitation. 2008;79:198–204. doi: 10.1016/j.resuscitation.2008.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Carr BG, Kahn JM, Merchant RM, Kramer AA, Neumar RW. Inter-hospital variability in post-cardiac arrest mortality. Resuscitation. 2009;80:30–34. doi: 10.1016/j.resuscitation.2008.09.001. [DOI] [PubMed] [Google Scholar]
- 7.Langhalle A, Tyvold SS, Lexow K, Hapnes SA, Sunde K, Steen PA. In-hospital factors associated with improved outcome after out-of-hospital cardiac arrest. A comparison between four regions in Norway. Resuscitation. 2003;56:247–263. doi: 10.1016/s0300-9572(02)00409-4. [DOI] [PubMed] [Google Scholar]
- 8.Skrifvars MB, Pettilä V, Rosenberg PH, Castrén M. A multiple logistic regression analysis of in-hospital factors related to survival at six months in patients resuscitated from out-of-hospital ventricular fibrillation. Resuscitation. 2003;59:319–328. doi: 10.1016/s0300-9572(03)00238-7. [DOI] [PubMed] [Google Scholar]
- 9.Liu JM, Yang Q, Pirrallo RG, Klein JP, Aufderheide TP. Hospital variability of out-of-hospital cardiac arrest survival. Prehosp Emerg Care. 2008;12:339–346. doi: 10.1080/10903120802101330. [DOI] [PubMed] [Google Scholar]
- 10.Peels HO, Jessurun GAJ, ven der Horst ICC, Arnold AER, Piers LH, Zijlstra F. Outcome in transferred and nontransferred patients after percutaneous coronary intervention for ischaemic out-of-hospital cardiac arrest. Catheterization Cardiovasc Interventions. 2008;71:147–151. doi: 10.1002/ccd.21265. [DOI] [PubMed] [Google Scholar]
- 11.Garot P, Lefevre T, Eltchaninoff H, Morice MC, Tamion F, Abry B, Lesault PF, Le Tarnec JY, Pouges C, Margenet A, Monchi M, Laurent I, Dumas P, Garot J, Louvard Y. Six-month outcome of emergency percutaneous coronary intervention in resuscitated patients after cardiac arrest complicating ST-elevation myocardial infarction. Circulation. 2007;115:1354–1362. doi: 10.1161/CIRCULATIONAHA.106.657619. [DOI] [PubMed] [Google Scholar]
- 12.Morrison LJ, Nichol G, Rea TD, Christenson J, Callaway CW, Stephens S, Pirrallo RG, Atkins DL, Davis DP, Idris AH, Newgard C ROC Investigators. Rationale, development and implementation of the Resuscitation Outcomes Consortium Epistry-Cardiac Arrest. Resuscitation. 2008;78:161–169. doi: 10.1016/j.resuscitation.2008.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Davis DP, Garberson LA, Andrusiek DL, Hostler D, Daya M, Pirrallo R, Craig A, Stephens S, Larsen J, Drum AF, Fowler R. A descriptive analysis of Emergency Medical Service Systems participating in the Resuscitation Outcomes Consortium (ROC) network. Prehosp Emerg Care. 2007;11:369–382. doi: 10.1080/10903120701537147. [DOI] [PubMed] [Google Scholar]
- 14.Skrifvars MB, Castrén M, Aune S, Thoren AB, Nurmi J, Herlitz J. Variability in survival after in-hospital cardiac arrest depending on the hospital level of care. Resuscitation. 2007;73:73–81. doi: 10.1016/j.resuscitation.2006.08.022. [DOI] [PubMed] [Google Scholar]
- 15.Hollenberg J, Lindqvist J, Ringh M, Engdahl J, Bohm K, Rosenqvist M, Svensson L. An evaluation of post-resuscitation care as a possible explanation of a difference in survival after out-of-hospital cardiac arrest. Resuscitation. 74:242–252. doi: 10.1016/j.resuscitation.2006.12.014. 200. [DOI] [PubMed] [Google Scholar]
- 16.Spaulding CM, Joly LM, Rosenberg A, Monchi M, Weber SN, Dhainaut JF, Carli P. Immediate coronary angiography in survivors of out-of-hospital cardiac arrest. N Engl J Med. 1997;336:1629–1633. doi: 10.1056/NEJM199706053362302. [DOI] [PubMed] [Google Scholar]
- 17.Reynolds JC, Callaway CW, El Khoudary SR, Moore CG, Alvarez RJ, Rittenberger JC. Coronary angiography predicts improved outcome following cardiac arrest: propensity-adjusted analysis. Journal of Intens Care Med. 2009 doi: 10.1177/0885066609332725. epub March 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Antman EM, Hand M, Armstrong PW, Bates ER, Green LA, Halasyamani LK, Hochman JS, Krumholz HM, Lamas GA, Mullany CJ, Pearle DL, Sloan MA, Smith SC Jr; 2004 Writing Committee Members, Anbe DT, Kushner FG, Ornato JP, Jacobs AK, Adams CD, Anderson JL, Buller CE, Creager MA, Ettinger SM, Halperin JL, Hunt SA, Lytle BW, Nishimura R, Page RL, Riegel B, Tarkington LG, Yancy CW. 2007 Focused Update of the ACC/AHA 2004 Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines: developed in collaboration With the Canadian Cardiovascular Society endorsed by the American Academy of Family Physicians: 2007 Writing Group to Review New Evidence and Update the ACC/AHA 2004 Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction, Writing on Behalf of the 2004 Writing Committee. Circulation. 2008;117:296–329. doi: 10.1161/CIRCULATIONAHA.107.188209.
- 19.Choudhry NK, Singh JM, Barolet A, Tomlinson GA, Detsky AS. How should patients with unstable angina and non-ST-segment elevation myocardial infarction be managed? A meta-analysis of randomized trials. Am J Med. 2005;118:465–474. doi: 10.1016/j.amjmed.2005.02.016. [DOI] [PubMed] [Google Scholar]
- 20.Hoenig MR, Doust JA, Aroney CN, Scott IA. Early invasive versus conservative strategies for unstable angina & non-ST-elevation myocardial infarction in the stent era. Cochrane Database Syst Rev. 2006;3:CD004815. doi: 10.1002/14651858.CD004815.pub2. [DOI] [PubMed] [Google Scholar]
- 21.O'Donoghue M, Boden WE, Braunwald E, Cannon CP, Clayton TC, de Winter RJ, Fox KA, Lagerqvist B, McCullough PA, Murphy SA, Spacek R, Swahn E, Wallentin L, Windhausen F, Sabatine MS. Early invasive vs conservative treatment strategies in women and men with unstable angina and non-ST-segment elevation myocardial infarction: a meta-analysis. JAMA. 2008;300:71–80. doi: 10.1001/jama.300.1.71. [DOI] [PubMed] [Google Scholar]
- 22.Merchant RM, Abella BS, Khan M, Huang KN, Beiser DG, Neumar RW, Carr BG, Becker LB, Vanden Hoek TL. Cardiac catheterization is underutilized after in-hospital cardiac arrest. Resuscitation. 2008;79:398–403. doi: 10.1016/j.resuscitation.2008.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Henry TD, Atkins JM, Cunningham MS, Francis GS, Groh WJ, Hong RA, Kern KB, Larson DM, Ohman EM, Ornato JP, Peberdy MA, Rosenberg MJ, Weaver WD. ST-segment elevation myocardial infarction: recommendations on triage of patients to heart attack centers: is it time for a national policy for the treatment of ST-segment elevation myocardial infarction? J Am Coll Cardiol. 2006;47:1339–1345. doi: 10.1016/j.jacc.2005.05.101. [DOI] [PubMed] [Google Scholar]
- 24.Henry TD, Sharkey SW, Burke MN, Chavez IJ, Graham KJ, Henry CR, Lips DL, Madison JD, Menssen KM, Mooney MR, Newell MC, Pedersen WR, Poulose AK, Traverse JH, Unger BT, Wang YL, Larson DM. A regional system to provide timely access to percutaneous coronary intervention for ST-elevation myocardial infarction. Circulation. 2007;116:721–728. doi: 10.1161/CIRCULATIONAHA.107.694141. [DOI] [PubMed] [Google Scholar]
- 25.Rathore SS, Epstein AJ, Nallamothu BK, Krumholz HM. Regionalization of ST-segment elevation acute coronary syndromes care: putting a national policy in proper perspective. J Am Coll Cardiol. 2006;47:1346–1349. doi: 10.1016/j.jacc.2005.11.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Anyfantakis ZA, Baron G, Aubry P, Himbert D, Feldman LJ, Juliard JM, Ricard-Hibon A, Burnod A, Cokkinos DV, Steg PG. Acute coronary angiographic findings in survivors of out-of-hospital cardiac arrest. Am Heart J. 2009;157:312–318. doi: 10.1016/j.ahj.2008.09.016. [DOI] [PubMed] [Google Scholar]
- 27.Lurie KG, Idris A, Holcomb JB. Level 1 cardiac arrest centers: learning from the trauma surgeons. Acad Emerg Med. 2005;12:79–80. doi: 10.1197/j.aem.2004.11.010. [DOI] [PubMed] [Google Scholar]
- 28.Pronovost PJ, Angus DC, Dorman T, Robinson KA, Dremsizov TT, Young TL. Physician staffing patterns and clinical outcomes in critically ill patients: a systematic review. JAMA. 2002;288:2151–2162. doi: 10.1001/jama.288.17.2151. [DOI] [PubMed] [Google Scholar]
- 29.Nathens AB, Jurkovich GJ, Maier RV, Grossman DC, MacKenzie EJ, Moore M, Rivara FP. Relationship between trauma center volume and outcomes. JAMA. 2001;285:1164–1171. doi: 10.1001/jama.285.9.1164. [DOI] [PubMed] [Google Scholar]
- 30.Celso B, Tepas J, Langland-Orban B, Pracht E, Papa L, Lottenberg L, Flint L. A systematic review and meta-analysis comparing outcome of severely injured patients treated in trauma centers following the establishment of trauma systems. J Trauma. 2006;60:371–378. doi: 10.1097/01.ta.0000197916.99629.eb. [DOI] [PubMed] [Google Scholar]
- 31.MacKenzie EJ, Rivara FP, Jurkovich GJ, Nathens AB, Frey KP, Egleston BL, Salkever DS, Scharfstein DO. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med. 2006;354:366–378. doi: 10.1056/NEJMsa052049. [DOI] [PubMed] [Google Scholar]
- 32.Foley N, Salter K, Teasell R. Specialized stroke services: a meta-analysis comparing three models of care. Cerebrovasc Dis. 2007;23:194–202. doi: 10.1159/000097641. [DOI] [PubMed] [Google Scholar]
- 33.Stroke Unit Trialists' Collaboration. Organised inpatient (stroke unit) care for stroke. Cochrane Database Syst Rev. 2007;4:CD000197. doi: 10.1002/14651858.CD000197.pub2. [DOI] [PubMed] [Google Scholar]
- 34.Herlitz J, Engdahl J, Svensson L, Angquist KA, Silfverstolpe J, Holmberg S. Major differences in 1-month survival between hospitals in Sweden among initial survivors of out-of-hospital cardiac arrest. Resuscitation. 2006;70:404–409. doi: 10.1016/j.resuscitation.2006.01.014. [DOI] [PubMed] [Google Scholar]
- 35.Herlitz J, Bång A, Gunnarsson J, Engdahl J, Karlson BW, Lindqvist J, Waagstein L. Factors associated with survival to hospital discharge among patients hospitalised alive after out of hospital cardiac arrest: change in outcome over 20 years in the community of Göteborg, Sweden. Heart. 2003;89:25–30. doi: 10.1136/heart.89.1.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Werling M, Thorén AB, Axelsson C, Herlitz J. Treatment and outcome in post-resuscitation care after out-of-hospital cardiac arrest when a modern therapeutic approach was introduced. Resuscitation. 2007;73:40–45. doi: 10.1016/j.resuscitation.2006.08.018. [DOI] [PubMed] [Google Scholar]