Abstract
Background
Two simple questions have been used to classify neurologic outcome in patients with stroke. Could they be similarly applied to patients with cardiac arrest?
Methods
As part of a randomized trial, study personnel interviewed by telephone survivors of out-of-hospital cardiac arrest to assess their outcomes three months after discharge. They asked two simple questions: 1) In the last two weeks, did you require help from another person for your everyday activities? & 2) Do you feel that you have made a complete mental recovery form your heart arrest? Next they administered the Mini-Mental State Examination (MMSE) from the Adult Lifestyles and Function Interview (ALFI) to assess cognition on a scale from 0 to 22 and the Health Utilities Index Mark 3 (HUI3) to assess quality of life on a scale from 0 (death) to 1 (perfect health).
Results
Based on responses to the two simple questions, 32 survivors were classified as dependent (n=5, 16%), independent (n=3, 9%) and full recovery (n=24, 75%). The mean ALFI-MMSE score was 19.1 (standard deviation 5.1), and the mean HUI3 score was 0.76 (standard deviation 0.28). The classification based on the two simple questions was significantly correlated with ALFI-MMSE (p=0.002) and HUI3 (p=0.001). Scores for the HUI3 were missing in 8 survivors.
Conclusions
Neurologic outcomes based on the two simple questions after cardiac arrest can be easily determined, sensibly applied, and readily interpreted. These preliminary findings justify further evaluation of this simple and practical approach to classify neurologic outcome in survivors of cardiac arrest.
Keywords: heart arrest, out-of-hospital CPR, outcome, quality of life
INTRODUCTION
Two simple questions with established reliability and validity have been used to classify outcome in stroke research.1–7 We hypothesized that they could be used to classify outcomes after cardiac arrest. We explored the correlation of two simple questions with other measures used in the Public Access Defibrillation (PAD) Trial to evaluate survivors’ outcomes three months after hospital discharge for resuscitation from out-of-hospital cardiac arrest.8,9
METHODS
In a prospective, multicenter clinical trial, community units were randomly assigned to a structured and monitored emergency-response system involving lay volunteers trained in cardiopulmonary resuscitation (CPR) alone or in CPR and the use of automated external defibrillators.8,9 Although the primary outcome in the PAD trial was survival to hospital discharge, after informed consent was obtained, study personnel interviewed by telephone those who were discharged to determine their subsequent outcomes.8 All of those discharged regained consciousness, and 32 of the 45 (71%) were classified as normal on Cerebral Performance Category (CPC)10 at hospital discharge, based on review of hospital records. The CPC and closely related Glasgow Outcome Scale (GOS)11 are both five-point ordered scales, where 5 is best on the GOS, and 1, on the CPC.
At three months, study personnel were able to locate and interviewed 33 survivors to assess outcome. We adapted two simple questions used to classify outcome in survivors of stroke,1 specifically: 1) In the last two weeks, did you require help from another person for your everyday activities? & 2) Do you feel that you have made a complete mental recovery form your heart arrest? Based on responses, we classified survivors as dependent (answered first question, yes), independent (answered first and second question, no), and full recovery (answered first question, no, and second question, yes). Study personnel then asked the first question from the 36-item short-form (SF-36) in the Medical Outcomes Study,12 specifically: “In the interval since your cardiac arrest, would you, in general, say your health is excellent, very good, good, fair, or poor?” Two other measures followed: the telephone version of the Mini-Mental State Examination (MMSE) from the Adult Lifestyles and Function Interview (ALFI) to assess cognition,13 and the Health Utilities Index Mark 3 (HUI3) to assess quality of life.14,15 The ALFI-MMSE scores range from 0 to 22 (best). The HUI3 scores range from 0 (death) to 1 (perfect health). Analyses involved contrasting results of the classification based on the two questions with results from the other measures using Fisher exact tests and one-way analysis of variance, as appropriate. Findings with p-values less than 0.05 were considered significant, and all testing was two-tailed. Analyses were conducted in Stata (version 10.1, StataCorp, College Station, TX).
RESULTS
Although study personnel interviewed 33 survivors, response to the recovery question was missing in one, so these analyses include 32 survivors: mean age was 55.6 years (standard deviation (SD) 16.1); median age, 60 years (interquartile range (IQR) 41–68); and 28 (87.5%), men. Collapse was witnessed in 78.1%, and 50.0% were engaged in sedentary activities at onset. All were discharged home except for three who went to rehabilitation facilities. The 32 survivors were classified by the two questions as dependent in 5 (15.6%), independent in 3 (9.4%), and full recovery in 25 (75.0%). Neither age nor sex was significantly related to outcome. The survivor was the source of the information in 28, and the survivor’s proxy, in 4, all of whom were classified as dependent. Only one survivor indicated dependency with full recovery and was classified as dependent.
Table 1 provides results of comparisons with other measures. The CPC at hospital discharge overestimated recovery compared to results at three months. At three months, those with better outcomes reported significantly better overall general health status. The ALFI-MMSE score was missing for one survivor who was classified as dependent. The HUI3 score was missing in eight survivors, three of whom were classified as full recovery, three as independent, and two as dependent. Overall the mean ALFI-MMSE score was 19.1 (SD 5.1), and median, 21 (IQR range 17–22). Overall the mean HUI3 score was 0.76 (SD 0.28), and median, 0.90 (IQR range 0.55–0.97). Both the ALFI-MMSE and HUI3 scores were significantly related to outcome based on the two questions, despite small numbers. If the survivor who indicated dependency with full recovery was classified as full recovery or excluded, all of the associations reported in Table 1 were stronger.
Table 1.
Two questions used to classify outcome after out-of-hospital cardiac arrest and correlations with other measures of outcome.
| 1) In the last two weeks, did you require help from another person for your everyday activities? | ||||
| No (N = 27) | Yes (N = 5) | |||
| 2) Do you feel that you have made a complete mental recovery from your heart arrest? | ||||
| Yes (N = 24) | No (N = 3) | |||
| Measure at hospital discharge | Full Recovery (N = 24) | Independent (N = 3) | Dependent* (N = 5) | P-value† |
| CPC | 0.075 | |||
| Normal | 21 | 3 | 2 | |
| Independent | 3 | 0 | 2 | |
| Dependent | 0 | 0 | 1 | |
| Measure at 3 months | ||||
| General Health Status | 0.004 | |||
| Excellent | 5 | 0 | 0 | |
| Very Good | 12 | 1 | 0 | |
| Good | 5 | 1 | 1 | |
| Fair | 2 | 0 | 1 | |
| Poor | 0 | 1 | 3 | |
| ALFI-MMSE (SD), N=31 | 20.4 (2.0) | 18.7 (2.9) | 11.2 (11.4) | 0.002 |
| HUI3 (SD), N=24 | 0.82 (0.21) | -- | 0.30 (0.32) | 0.001 |
CPC stands for Cerebral Performance Category; ALFI-MMSE, Adult Lifestyles and Function Interview - Mini-Mental State Examination; HUI3, Health Utility Index Mark 3; and SD, standard deviation.
One survivor reported both dependency and full recovery. All associations in the table were stronger if this survivor was classified as full recovery or excluded rather than as dependent.
P-value based on counts and Fisher exact test for CPC and General Health Status and on means and analysis of variance for ALFI-MMSE and HUI3.
DISCUSSION
We describe the use of two simple questions to classify neurologic outcomes after out-of-hospital cardiac arrest. Experience with the two questions in stroke survivors is extensive and favorable based on reliability, validity, similarity of responses from patients and their proxies, and comparability of responses to questioning face-to-face, by post, or by telephone.1–7 Although numbers are small in the current study, findings suggest that using the two questions allows a classification that correlates well with other measures of outcome at three months after cardiac arrest. The correlation of the HUI3 with CPC has been examined previously in 305 survivors of cardiac arrest.16 The HUI3 scores were similar in the current study with a median of 0.90 for the entire group compared to 0.84 in this prior study of cardiac arrest survivors and to 0.85 in the general population.16 As in this previous study where a HUI3 cutoff of 0.80 was used to define good quality of life, with full recovery the specificity was 100% (96.8% in the prior study with CPC normal), and the sensitivity was 66.7% (55.6% in the prior study). In the current study, the HUI3 may overestimate the quality of life in survivors because it was missing most often in those who did not report full recovery. At least as measured by the HUI3, this study and others that have used the HUI314,16 suggest that the quality of life of most survivors of cardiac arrest is good.
These two simple questions provide the investigator with a means based on self-report to classify conscious patients in the GOS, or the closely related CPC. Typically investigators classify conscious patients in the top three categories of these scales based on medical records whose quality of documentation may vary,10,11 but whatever approach is used, it may not be applied in a uniform fashion. What could be more important than the impression about recovery of the survivor or survivor’s proxy? Classification of neurologic outcome after cardiac arrest on the GOS or CPC would involve care providers answering two simple questions about survival and consciousness and survivors answering two simple questions about dependency and recovery, as illustrated in Figure 1. Depending on the purpose, more detailed testing could be done to rank the outcome of patients in a particular category.17 Such details would come at a price given the investigators having to travel to geographically dispersed survivors or survivors having to travel to the investigators. The GOS scores of 3, 4, and 5 would be difficult to determine on hospital discharge because the patient will not have been challenged with everyday activities. A similar problem exists with other scales applied at this time. Perhaps the best approach is to base outcome at hospital discharge on the two questions that care providers answer about survival and consciousness.
Figure 1.
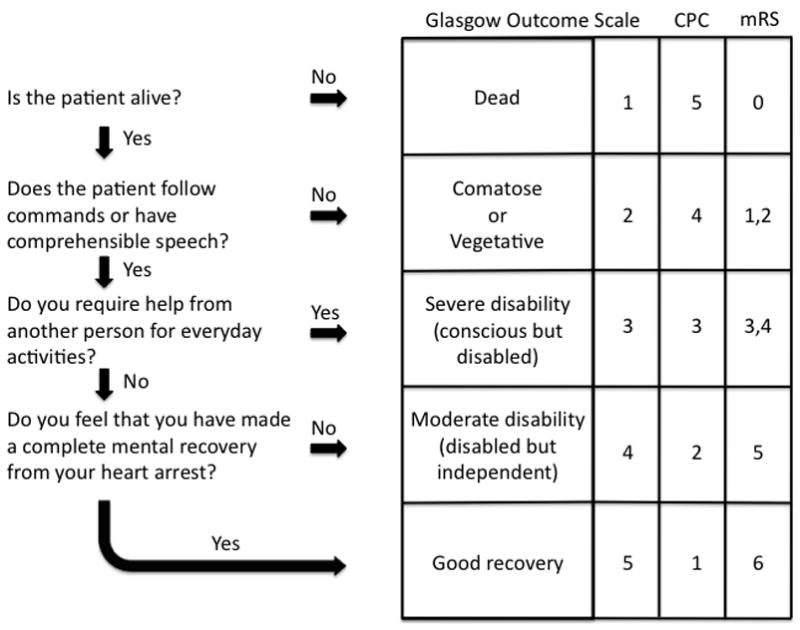
Minimalist approach to assigning scores on the Glasgow Outcome Scale (GOS) based on four simple questions, two answered by care providers and two by the survivor or survivor’s proxy. Suggested translation into scores on Cerebral Performance Category (CPC) and modified Rankin Scale (mRS)
Although information was collected in this randomized trial in a standardized and unbiased fashion, the numbers of survivors was small. Also information was collected over the telephone rather than in person. This practical approach may be important especially for multicenter trails where standardization of face-to-face evaluations at multiple centers may be difficult to achieve and face-to-face follow-up may be burdensome for patients and families. The use of the two simple questions in stroke outcome has its critics.18,19 Modification of the wording of the questions has been suggested to increase reliability.19 Also was our modification of the original recovery question optimal? The possibility exists of patients indicating complete recovery but needing help in everyday activities, as occurred in one of the survivors in this study. Such a combination of responses may relate to the level of function and independence prior to cardiac arrest. Investigators have also raised concerns over differences in response to the two simple questions by gender.20 The role of depression is uncertain. Many of these concerns apply to any outcome measure. Some investigators have acknowledged the loss of details about outcomes and lack of measurement precision when using the two simple questions but have detailed the advantages including low participant burden, high frequency of response, simple analyses, easily interpreted results, and ability to classify all patients on a single scale.19 For more complex outcomes measures, these advantages wane.
CONCLUSION
The two questions used in this study have advantages over other measures. They provide a simply means to classify outcome in survivors of cardiac arrest using the GOS, or the closely related CPC. This study shows that they can be administered over the telephone and correlate well with other more complicated measures of cognition and quality of life. These preliminary findings justify further evaluation of this simple and practical approach (Figure 1) to classify neurologic outcome in survivors of cardiac arrest.
Footnotes
CONFLICTS OF INTEREST
None.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Lindley RI, Waddell F, Livingstone M, et al. Can simple questions assess outcome after stroke? Cerebrovasc Dis. 1994;4:314–24. [Google Scholar]
- 2.Kay R, Wong KS, Yu YL, et al. Low-molecular-weight heparin for the treatment of acute ischemic stroke. N Engl J Med. 1995;333:1588–93. doi: 10.1056/NEJM199512143332402. [DOI] [PubMed] [Google Scholar]
- 3.The International Stroke Trial (IST): a randomised trial of aspirin, subcutaneous heparin, both, or neither among 19435 patients with acute ischaemic stroke. International Stroke Trial Collaborative Group. Lancet. 1997;349:1569–81. [PubMed] [Google Scholar]
- 4.Berge E, Abdelnoor M, Nakstad PH, Sandset PM. Low molecular-weight heparin versus aspirin in patients with acute ischaemic stroke and atrial fibrillation: a double-blind randomised study. HAEST Study Group. Heparin in Acute Embolic Stroke Trial. Lancet. 2000;355:1205–10. doi: 10.1016/s0140-6736(00)02085-7. [DOI] [PubMed] [Google Scholar]
- 5.Berge E, Fjaertoft H, Indredavik B, Sandset PM. Validity and reliability of simple questions in assessing short- and long-term outcome in Norwegian stroke patients. Cerebrovasc Dis. 2001;11:305–10. doi: 10.1159/000047658. [DOI] [PubMed] [Google Scholar]
- 6.McKevitt C, Dundas R, Wolfe C. Two simple questions to assess outcome after stroke: a European study. Stroke. 2001;32:681–6. doi: 10.1161/01.str.32.3.681. [DOI] [PubMed] [Google Scholar]
- 7.Celani MG, Cantisani TA, Righetti E, Spizzichino L, Ricci S. Different measures for assessing stroke outcome: an analysis from the International Stroke Trial in Italy. Stroke. 2002;33:218–23. doi: 10.1161/hs0102.100532. [DOI] [PubMed] [Google Scholar]
- 8.Ornato JP, McBurnie MA, Nichol G, et al. The Public Access Defibrillation (PAD) trial: study design and rationale. Resuscitation. 2003;56:135–47. doi: 10.1016/s0300-9572(02)00442-2. [DOI] [PubMed] [Google Scholar]
- 9.Hallstrom AP, Ornato JP, Weisfeldt M, et al. Public-access defibrillation and survival after out-of-hospital cardiac arrest. N Engl J Med. 2004;351:637–46. doi: 10.1056/NEJMoa040566. [DOI] [PubMed] [Google Scholar]
- 10.A randomized clinical trial of calcium entry blocker administration to comatose survivors of cardiac arrest. Design, methods, and patient characteristics. The Brain Resuscitation Clinical Trial II Study Group. Control Clin Trials. 1991;12:525–45. doi: 10.1016/0197-2456(91)90011-a. [DOI] [PubMed] [Google Scholar]
- 11.Jennett B, Bond M. Assessment of outcome after severe brain damage. Lancet. 1975;1:480–4. doi: 10.1016/s0140-6736(75)92830-5. [DOI] [PubMed] [Google Scholar]
- 12.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–83. [PubMed] [Google Scholar]
- 13.Roccaforte WH, Burke WJ, Bayer BL, Wengel SP. Validation of a telephone version of the Mini-Mental State Examination. J Am Geriatr Soc. 1992;40:697–702. doi: 10.1111/j.1532-5415.1992.tb01962.x. [DOI] [PubMed] [Google Scholar]
- 14.Nichol G, Stiell IG, Hebert P, Wells GA, Vandemheen K, Laupacis A. What is the quality of life for survivors of cardiac arrest? A prospective study. Acad Emerg Med. 1999;6:95–102. doi: 10.1111/j.1553-2712.1999.tb01044.x. [DOI] [PubMed] [Google Scholar]
- 15.Horsman J, Furlong W, Feeny D, Torrance G. The Health Utilities Index (HUI): concepts, measurement properties and applications. Health Qual Life Outcomes. 2003;1:54. doi: 10.1186/1477-7525-1-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stiell IG, Nesbitt LP, Nichol G, et al. Comparison of the Cerebral Performance Category score and the Health Utilities Index for survivors of cardiac arrest. Ann Emerg Med. 2009;53:241–8. doi: 10.1016/j.annemergmed.2008.03.018. [DOI] [PubMed] [Google Scholar]
- 17.Longstreth WT, Jr, Dikmen SS. Outcomes after cardiac arrest. Ann Emerg Med. 1993;22:64–9. doi: 10.1016/s0196-0644(05)80252-5. [DOI] [PubMed] [Google Scholar]
- 18.Dennis M, Wellwood I, O’Rourke S, MacHale S, Warlow C. How reliable are simple questions in assessing outcome after stroke? Cerebrovasc Dis. 1997;7:19–21. [Google Scholar]
- 19.Dorman P, Dennis M, Sandercock P. Are the modified “simple questions” a valid and reliable measure of health related quality of life after stroke? United Kingdom Collaborators in the International Stroke Trial. J Neurol Neurosurg Psychiatry. 2000;69:487–93. doi: 10.1136/jnnp.69.4.487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chong JY, Lee HS, Boden-Albala B, Paik MC, Sacco RL. Gender differences in self-report of recovery after stroke: the Northern Manhattan Study. Neurology. 2006;67:1282–4. doi: 10.1212/01.wnl.0000238161.71591.e9. [DOI] [PubMed] [Google Scholar]


