Abstract
The current study examined the relationship between the family environment and symptoms and functioning over time in a group of adolescents and young adults at clinical high risk for psychosis (N = 63). The current study compared the ability of interview-based versus self-report ratings of the family environment to predict the severity of prodromal symptoms and functioning over time. The family environmental factors were measured by interviewer ratings of the Camberwell Family Interview (CFI), self-report questionnaires surveying the patient’s perceptions of criticism and warmth, and parent reported perceptions of their own level of criticism and warmth. Patients living in a critical family environment, as measured by the CFI at baseline, exhibited significantly worse positive symptoms at 6-month follow-up, relative to patients living in a low-key family environment. In terms of protective effects, warmth and an optimal level of family involvement interacted such that the two jointly predicted improved functioning at 6-month follow-up. Overall, both interview-based and self-report ratings of the family environment were predictive of symptoms and functioning at follow-up; however patient’s self-report ratings of criticism had stronger predictive power. These results suggest that the family environment should be a specific target of treatment for individuals at risk for psychosis.
Keywords: Expressed Emotion, Family Environment, Prodrome, Psychosis, Schizophrenia, Ultra High Risk
1.1 Introduction
Schizophrenia and other forms of psychosis are chronic and seriously disabling disorders. Available drug treatments are palliative rather than curative and only address positive symptoms, with little or no effect on negative symptoms and functional impairment. In step with other chronic somatic illnesses, such as diabetes and heart disease, researchers have shifted focus to early intervention and prevention. In the field of schizophrenia, this focus has generated an emergent body of research aimed at delaying or preventing fully psychotic symptoms from developing through the identification of the prodromal phase of illness. The prodrome to psychosis is characterized by attenuated psychotic symptoms and/or a family history of psychosis with functional deterioration (Yung and McGorry, 1996). Such “ultra high risk” (UHR) individuals have high rates of conversion to psychosis, ranging from 30–60% over approximately two years (Cannon et al., 2008; Miller et al., 2002). As identification of UHR individuals improves, it is critical that studies focus on intervention-sensitive factors that mitigate the risk of conversion to psychosis.
Despite the strong contribution of genetics to the development of psychosis, adoption studies have highlighted that the family environment can also have a substantial impact on outcomes (Tienari et al., 2003; 2006). Furthermore, Expressed Emotion (EE), a measure of the family environment, is the strongest psychosocial predictor of clinical and functional outcome for individuals with schizophrenia (Butzlaff and Hooley, 1998) and a critical domain of intervention in treatment studies (Miklowitz et al., 2004). The Camberwell Family Interview (CFI; Leff and Vaughn, 1985), the gold standard measure of EE, is a 1–2 hour semi-structured interview that is conducted with the patient’s primary caregiver. The CFI is designed to elicit family attitudes about the patient’s behavior and symptoms and is thought to reflect the family emotional environment and the interactions between family members (Hooley, 2007). When rating the interview, family member comments are rated to determine whether they represent attitudes that reflect five different indices: hostility, emotional overinvolvement (EOI), criticism, warmth, and positive remarks. A rating of high-EE is made based on six or more critical comments, or the presence of hostility, or a rating of 4 or more comments on an index of emotionally overinvolved attitudes.
Criticism and hostility, both components of high-EE, have consistently been linked to poor outcomes among patients with schizophrenia (Butzlaff and Hooley, 1998). Research findings have demonstrated that 65% of patients with schizophrenia relapse within one year while living in a high-EE environment, compared to about 35% in low-EE environments (Butzlaff and Hooley, 1998; Kavanagh, 1992). Despite consistent findings of high-EE having high predictive validity, the results of studies examining how EOI, one of the components of a high-EE environment, relates to outcomes have been mixed. For instance, EOI predicted negative clinical outcomes among patients with chronic schizophrenia (Miklowitz et al., 1983) and positive clinical outcomes with patients at imminent risk for psychosis (O’Brien et al., 2006). In the early stages of developing the criteria for EE, warmth in conjunction with EOI was observed to have a positive effect on patients, but this finding has not been empirically tested (Leff and Vaughn, 1985). Due to the inconsistency of how EOI relates to outcomes, EOI was not included in the rating of “High-EE” status for the purposes of this study. Instead, EOI was analyzed independently and in relation to warmth to highlight how EOI operates in a UHR population.
In addition to testing the effect of EE on outcomes, the current study examined patient and parent self-reported perceptions of criticism and warmth in the family environment. Self-report ratings of perceived criticism and warmth were assessed in order to determine whether there was a significant difference between interview-based versus self-report ratings of the family environment and their comparative impact on outcomes. This is the first study to date to examine the effects of interview-based (e.g. CFI measured EE ratings) versus self-report (e.g. patient perceptions of criticism) ratings of the family environment and their relative effects on outcomes in a population at high risk for psychosis.
The current study hypothesized that:
-
High-EE families will significantly differ from low-EE families, such that:
-
high-EE family members will report higher mean levels of how critical they are and lower mean levels of their own expressions of warmth.
In addition,
patients living in high-EE environments will report higher mean levels of perceived criticism from their primary caregiver, and lower mean levels of perceived warmth.
-
A matched sample based on EE status, symptoms, and functioning, as measured at baseline, will report significantly different levels of symptoms and functioning at follow-up, such that patients living in high-EE family environments will report more severe symptoms and worse functioning at the 6-month follow-up, relative to the low-EE sample..
Interview-based ratings of the family environment (e.g. CFI) and self-report ratings (patient and family perceptions of criticism and warmth) of the family environment at baseline will BOTH be predictive of a change in symptoms and functioning at follow-up, such that higher levels of criticism and lower levels of warmth will be predictive of worse symptoms and functioning at follow-up.
Emotional overinvolvement and warmth will interact, such that moderate levels of EOI in the presence of warmth will be predictive of better functioning at follow-up.
2.1 Method
2.2 Participants
Sixty-three outpatient participants, age 12 to 35, were recruited to participate in the study from individuals already enrolled in one of two prodromal research clinics: the Staglin Music Festival Center for the Assessment and Prevention of Prodromal States (CAPPS) at the University of California, Los Angeles and the Prodromal Assessment, Research and Treatment (PART) study at the University of California, San Francisco. An inclusion criterion for the CAPPS and PART studies were met by research diagnostic criteria for a “prodromal syndrome,” as defined by the Structured Interview for Prodromal Syndromes (SIPS; Miller et al., 2002). A “prodromal syndrome” is defined by: 1) attenuated positive symptoms 2) brief, intermittent psychotic symptoms OR 3) decline in role functioning AND either a diagnosis of schizotypal personality disorder or a first-degree relative with a psychotic disorder. The current study also included subjects with recent-onset (e.g. within the past 3 months) symptoms that reached a psychotic intensity but did not reach criteria for a DSM-IV diagnosis of a psychotic disorder such as schizophrenia, schizophreniform or schizoaffective disorder. See Table 1 for the distribution of subjects in each prodromal syndrome.
Table 1.
Characterization of study participants (N=63)
| Gender (n, %) | |
| Male | 41 (65.1%) |
| Female | 22 (34.9%) |
| Age (mean years, SD) | 15.89 (2.80) |
| Education (mean years, SD) | |
| Father | 12.98 (1.91) |
| Mother | 13.17 (1.73) |
| Ethnicity (n, %) | |
| Caucasian | 34 (54%) |
| Latino/Hispanic | 9 (14.3%) |
| African American/Black | 10 (15.9%) |
| Asian American/Pacific Islander | 2 (3.2%) |
| Other | 8 (12.7%) |
| Prodromal Syndrome (n, %) | |
| Attenuated Positive Symptom Prodromal Syndrome | 50 (79.4%) |
| Brief Intermittent Psychotic Symptom Syndrome | 4 (6.3%) |
| Genetic Risk and Deterioration Prodromal Syndrome | 4 (6.3%) |
| Non Specific Psychotic Syndrome | 5 (8%) |
The sample consisted of more males than females and was ethnically diverse (Table 1). Fifty-six participants were recruited to participate from CAPPS and seven participants were recruited from PART. CAPPS and PART use the same stringent inclusion criteria and both sites are held to high reliability standards (ICC > .80). Twenty-four of the 63 subjects were included in a previously published study regarding family factors in a UHR population (O’Brien et al., 2006). Due to the current study’s focus on family factors, participants were recruited if they had family members who had consented to participate. Sixty-one participants had a family member complete the CFI and rated perceptions of the family environment, while the remaining two participants only completed the self-report ratings of perceived criticism and warmth. Eighty-two percent of the sample that was administered the CFI were mothers (N=50), 16% fathers (N=10), and 1.6% other relatives (N=1; grandmother). The sample distribution of family members is representative of other studies that examine the effects of EE (O’Brien et al., 2006; Weisman et al., 1998).
2.3 Measures
The outcome measures used were prodromal symptom severity, as measured by symptoms rated on the Scale of Prodromal Symptoms during the Structured Interview for Prodromal Syndromes (SOPS/SIPS; Miller et al., 2002); and social/occupational functioning, as measured by the aggregate score on the Strauss Carpenter Outcome Scale (SCOS; Strauss and Carpenter, 1972). The family environmental factors were measured by the CFI (Leff & Vaughn, 1985) and self-report questionnaires surveying the patient perceptions of criticism (PC; Hooley and Teasdale, 1989) and warmth (PW; Study authors’ adaptation of Hooley and Teasdale, 1989); and family member reported perceptions of their own level of criticism (FMPC) and warmth (FMPW).
The SIPS assesses symptoms in four domains (positive, negative, disorganized, and general symptoms) and rates symptom severity on a 0–6 scale, with 0 representing the absence of a symptom and 6 representing “severe and psychotic.” When a positive symptom is in the 3–5 range of severity that symptom is considered an “attenuated psychotic symptom.” Individuals diagnosed with a prodromal syndrome are considered at imminent risk for psychosis.
2.4 Procedure
The data included in this study were collected from participants in the CAPPS and PART studies. After an intake that determined study eligibility, participants at both sites completed assessment measures at baseline and 6 months. All family factor assessments and patient surveys were completed at baseline (e.g. CFI, PC, PW). Primary caregivers completed the CFI interview before rating their own level of criticism and warmth (FMPC and FMPW) during the baseline clinical assessment. The CFI was administered and rated by the first author and two research assistants, who had been trained to high standards of reliability on the measure by an expert rater (Jamie Zinberg, M.A.). For training purposes, ten videos were rated independently and followed up with consensus meetings. Raters achieved very good consistency reliability (ICC = .93). For the remainder of the sample, two raters coded each CFI. In addition, CFI interviewers and raters were blind to the ratings on the outcome measures.
2.5 Data Analysis Technique
The following data analysis techniques are described to provide some background to the statistical approaches used to test the study hypotheses. In order to test the first hypothesis that high EE-families will significantly differ from low-EE families, independent sample t-tests were conducted. Differences between the EE groups were tested based on mean levels of perceptions of criticism and warmth (e.g. PC, PW, FMPC, FMPW).
In order to test the second hypothesis, a matched sample of low-EE participants was generated to match the high-EE participants. The matched sample was based on the high-EE group’s mean levels of baseline prodromal symptomatology, baseline functioning, age, gender, and education. The matched sample grouped patients within one standard deviation of baseline symptoms and levels of functioning. The purpose of using a matched sample technique was to highlight the specific effect of the family environment over time by effectively controlling for a number of factors at baseline. While a regression analysis could have been conducted instead, entering all the matching variables into the model would have resulted in a substantial loss of power. Another benefit of the matching technique is that it controls for the variability (e.g. differences in symptom severity) between the high and low EE groups observed at baseline and the unequal sample sizes between the high-EE (N = 19) and low-EE (N = 42) groups.
To test the third hypothesis, two sets of regression analyses were conducted. The first tested whether patient perceived criticism and warmth were predictive of a change in positive symptoms and functioning over time. Due to baseline and follow-up symptoms being significantly related to one another, change scores were calculated to represent a change in symptoms over time. The second regression analysis tested whether the interview-based measure of the family environment predicted change in positive symptoms over time. CFI-rated hostility and criticism were entered into the first step and CFI-rated warmth was entered into the second step. In order to determine whether self-report measures were more or less predictive of symptoms and functioning over time, beta weights and semi partial correlation statistics are reported.
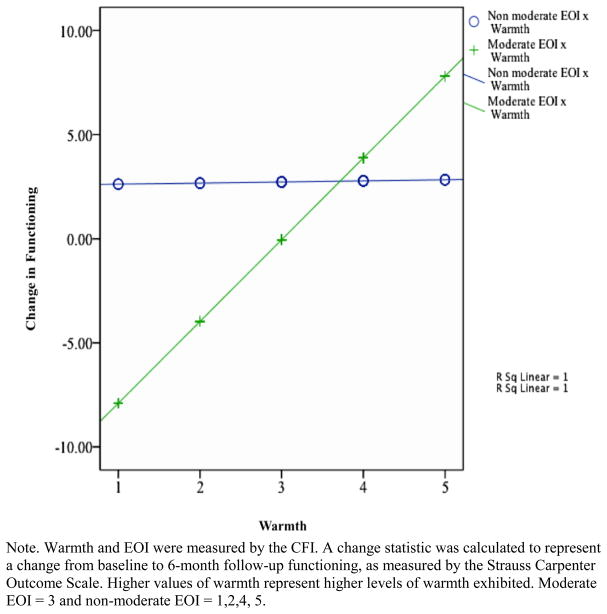
In order to test the fourth hypothesis to determine if EOI and warmth interact to predict functioning over time, a hierarchical regression analysis was used. In order to test if “moderate” levels of EOI interact with warmth, two values of EOI were created to reflect a moderate (EOI = 3 based on a 0–5 scale) and non-moderate level of EOI (EOI = 0, 1, 2, 4, 5). The moderate rating of EOI is based on the mean level of EOI in this sample. The reason for creating an indicator variable that represented EOI as either moderate or non-moderate was based on the hypothesis that moderate levels of EOI represent an “optimal” level of involvement whereas high and/or low levels of EOI might be predictive of poor outcomes. Thus participants were classified into moderate or extreme classification of EOI. The EOI classification was then entered into a regression analysis to determine if moderate levels of EOI interacted with warmth differently from non-moderate levels of EOI. The regression analysis included the predictors of EOI at a moderate level, CFI-rated warmth, and the interaction term of moderate EOI x warmth. The results will be plotted using the coefficients in the regression analysis. The outcome variable was change in functioning over time, based on the SCOS.
3.1 Results
3.2 Preliminary analyses
At baseline, about twice as many families were identified as being low in EE (n = 42; 68.9% of the sample) than those identified as meeting criteria for high-EE status (n = 19; 31.1% of the sample). The distribution of high-and low-EE individuals is consistent with the rates of EE identified in previous studies with UHR and first episode populations (Hooley and Richters, 1995; O’Brien et al., 2006). Of the 19 family members identified as having high-EE attitudes, 13 exhibited hostility during the CFI. Over the course of the study, 19 subjects converted to psychosis, reflecting a 30% conversion rate. Of the 63 patients, 59 had follow-up data. Four subjects dropped out of the study, reflecting a 6% attrition rate.
Prior to running the main analyses, associations between the outcome variables and demographic variables (gender, age, ethnicity, and socioeconomic status) were assessed using t-tests, one-way ANOVAs, and Pearson correlations. Analyses were also run to determine if there were significant differences between the CAPPS and PART samples on demographic variables, symptoms or functioning measures. None of these analyses were significant except for the relationship between overall functioning (SCOS) at follow up and age (r=−.45, p=. 003). Therefore, age was used as a covariate in subsequent analyses examining follow-up functioning. In order to examine the relationship between interview-based and self-report ratings of the family environment, Pearson correlation analyses were conducted (Table 2). Family member ratings of their own levels of warmth (FMPW) were significantly negatively related to CFI-rated criticism (r =−.40, p < .01) and significantly positively related to CFI-rated warmth (r =.54, p < .01). Patient ratings of perceived parental warmth were significantly related to the CFI-ratings of warmth (r = .52, p < .01).
Table 2.
Pearson Correlation Analyses Correlating Interview-Based (CFI Rated Criticism and Warmth) and Self-Report (Perceptions of Criticism and Warmth) Ratings of the Family Environment.
| CFI-Criticism | CFI-Warmth | |
|---|---|---|
| PC-Mother + Father | −.10 | .19 |
| PW-Mother + Father | −.25 | .52** |
| FMPC | .04 | −.11 |
| FMPW | −.41** | .54** |
| CFI-Criticism | 1 | −.40** |
Note. PC=perceived criticism; PW-perceived warmth; FMPC=family member perception of own level of criticism; FMPW=family member perception of own level of warmth.
p <.01
3.3 Main analyses
The results of the first hypothesis indicated that family members rated as high in EE reported significantly higher mean levels of their own level of criticism and lower levels of warmth (Table 3). Unexpectedly, there were no significant differences in the mean level of patient reported perceptions of criticism and warmth between high and low-EE families. A chi-square test resulted in no significant associations between conversion to psychosis and EE status (χ2(1, N = 61) = 1.74, p =.19).
Table 3.
Results of independent sample t-tests testing the first hypothesis that there are significant mean differences in patient and family perceptions of criticism and warmth, between the high and low EE groups. (N=61)
| High EE | Low EE | t-statistic | |
|---|---|---|---|
| mean (SD) | mean (SD) | ||
| PC- Mother + Father | 8.92 (6.02) | 10.39 (5.20) | .802 |
| PW-Mother + Father | 10.46 (4.41) | 13.82 (6.22) | 1.749 |
| FMPC | 6.25 (2.05) | 4.87 (1.89) | −2.093* |
| FMPW | 7.33 (1.88) | 8.87 (1.36) | 2.958** |
Note. PC = perceived criticism; PW = perceived warmth; FMPC = is the family member’s perception of his or her own level of criticism; FMPW = the family member’s perception of his or her own level of warmth.
p < 0.05;
p <.01
Results of the second hypothesis revealed significant mean differences in positive symptoms at follow-up, such that patients from high-EE families had more severe positive symptoms at follow-up relative to the patients from low-EE families (Table 4). There were no significant differences between the high and low-EE groups in functioning as measured by the SCOS at follow-up.
Table 4.
Results of Independent Sample t-tests Examining Symptomatic and Functionining Differences, Between the EE Groups Based on a Matched Sample (N=38)
| High-EE | Low-EE | t-statistic | |
|---|---|---|---|
| (mean, SD) | (mean, SD) | ||
| Positive symptoms | 9.75 (3.22) | 6.46 (3.69) | −2.40* |
| Negative symptoms | 10.25 (6.33) | 9.92 (6.73) | −.125 |
| Functioning | 11.92 (.29) | 11.23 (1.59) | −1.47 |
Note. Functioning was measured by the Strauss Carpenter Outcome Scale. EE status was measured based on 6 or more critical comments and/or the presence of hostility.
p < 0.05
The results of the third hypothesis were significant (R2 = .21; p = .001) and indicated that perceived criticism predicted 21% of the variance of change in positive symptoms (β = −.45; t = −2.80; p < .01 part r2= .21). In order to test if this result might be related to the presence of suspicious thinking, a Pearson correlation analysis was conducted. The non-significant result indicated that patient-perceived criticism was not related to suspicious thinking at baseline, as rated by the SIPS (r = .30, p = .06). Patient perceived warmth and family member’s perceptions of their own levels of criticism and warmth did not significantly predict a change in symptoms. Self-report ratings of the family environment were not predictive of functioning over time. The results, testing the interview-based ratings of the family environment, were also significant. CFI-rated hostility and criticism ratings were entered in the first step and CFI-rated warmth was entered in the second step. The results were significant (R2=.17, p = .03) and indicated that 15% of the variance in the change in positive symptoms was predicted by hostility and 7% by criticism in the family environment (β = −.42; t = −2.52; p < .01 part r2 = .15; β = −.34; t = −2.03; p < .05 part r2 = .07). Warmth, however, did not significantly add to the predictive model of follow-up symptoms.
The results of the fourth hypothesis were significant and provided evidence for the interactive effect of EOI and warmth on predicting functioning over time (Table 5; Figure 1). EOI and warmth did not independently predict functioning, however; the interaction effect was significant (β = 3.90; t = 2.90; p = .006). The interaction term plotting moderate levels of EOI and warmth was significant, however, there was not a significant relationship between non-moderate levels of EOI and warmth, as can be seen in the figure based on the flat regression line representing the non-moderate value of EOI. The model tested provided evidence for the moderating effects of warmth on the relationship between a moderate level of EOI and changes in functioning over time. Specifically, those participants who reported relatively higher levels of warmth were more likely to experience improved changes in functioning when EOI was at an optimal (e.g. moderate) level. Those participants who reported relatively lower levels of warmth were likely to experience a similar change in functioning regardless of level of EOI.
Table 5.
Hierarchical Regression Analysis Analyzing the Family Environment as it Predicts Change in Functioning, as Measured by the Strauss Carpenter Outcome Scale.
| R2 | F | R2Δ | adjR2 | B | SEB | β | part r2 | |
|---|---|---|---|---|---|---|---|---|
| Step1 | .000 | .000 | .000 | −.026 | ||||
| EOI | .007 | .354 | .003 | .00 | ||||
| Step 2 | .027 | 1.05 | .027 | −.024 | ||||
| Warmth | .458 | .447 | .191 | .03 | ||||
| Step 3 | .134* | 4.59 | .107 | .064 | ||||
| EOI x Warmth | .716 | .334 | 1.67* | .11 |
Note. EOI=Emotional Family Environment; EOI x Warm=The interaction term of EOI by Warmth. A change statistic was calculated representing a change from baseline to 6-month follow-up functioning, as measured by the Strauss Carpenter Outcome Scale.
p<.05
Figure 1.
Moderating Effects of Warmth on the Relationship Between a Moderate Level of Emotional Overinvolvement (EOI) and Change in Functioning Over Time.
4.1 Discussion
This study tested the longitudinal effects of the family environment on symptoms and functioning in individuals at high clinical risk for psychosis. The results identified the specific impact of high-EE on positive attenuated psychotic symptoms, such that patients living in high-EE environments exhibited worsening positive symptoms over time compared to those living in low-EE environments. This finding is particularly important considering that worsening positive symptoms signal the conversion from the prodrome to psychosis. This result was further supported when criticism and hostility, factors of high-EE, were found to be significantly predictive of a change in positive symptoms over time. One explanation for this finding might be that if a patient is living in a hostile family environment, it is likely a stressful experience for him/her and that stress could be the mechanism that accounts for the worsening of the high-risk symptoms over time.
Another important finding was the interactive relationship between EOI and warmth and its joint impact on improving functioning over time. Typically, EOI has been associated with negative outcomes and the only other study that examined the family environment in a UHR sample suggested that EOI had a positive effect on outcome (O’Brien et al., 2006). The current study helps to clarify that seeming contradiction. EOI can act as a protective factor when exhibited at moderate levels and within the context of warmth. Emotionally warm and moderately involved parents may play a role in the patient’s improved functioning by mitigating the patient’s experience of stress. There may be an optimal level of parental emotional involvement that is neither too distant nor too enmeshed, that provides appropriate social support for this age group.
The analyses comparing the effects of interview-based versus self-report ratings of the family environment on outcomes provided some interesting findings. The current study found that both interview-based and self-report measures of the family environment were predictive of changes in positive symptoms over time. By examining the Beta weights and the semi partial correlations, patient perceptions of criticism were more predictive of changes in positive symptoms over time than the CFI-rated family factors. This finding is consistent with the Hooley and Teasdale (1989) study with a sample of depressed patient, which found that patient’s perceived criticism was more predictive of symptoms than the CFI criticism scale. The clinical utility of such a brief measure of family attitudes that has yielded strong predictive value of clinical outcomes has considerable implications for patients, families, and mental health practitioners. Many clinicians may be aware of the important role of family criticism in the psychosocial outcome of UHR patients and those with schizophrenia, but identifying high rates of criticism is far easier with a brief patient report questionnaire than with the CFI, which is time consuming to administer and code. By using the very brief PC questionnaire, clinicians could efficiently identify patients whose family environments might put them at elevated risk for symptom exacerbation.
4.2 Limitations
The current study was limited by a relatively small sample size, which restricted the type of analyses that could have been conducted. For instance, structural equation modeling would be a useful statistical approach to examine the effects of family factors due to the ability to examine interactions in a more rigorous way. The small sample size also limited the power to detect if the family environment is predictive of conversion to psychosis. In order to further identify factors in the family environment that increase clinical risk, it is critical to have a large sample size with complete follow-up data, preferably with multiple time points.
4.3 Future Directions
The findings in the current study have significant clinical implications as well as indications for future research. In terms of future research studies, it would be beneficial to test if the findings from the current study are maintained over longer periods of follow-up. In addition, more complex models are warranted to examine possible interactive effect of the family environment and biological risk factors. Due to the significant effect of family factors on prodromal symptoms and functioning, it would be interesting to examine whether those same variables are predictive of conversion to psychosis in a larger sample. Furthermore, it would be beneficial to examine possible neurobiological characteristics in patients (e.g. dysregulation of cortisol) that might make particular individuals more vulnerable or protected from stress in the family environment.
From a clinical perspective, family members should be informed about the results of the current study. It is important to note that when communicating the results of the current study and additional research findings regarding the possible effects of the family environment on symptoms and functioning, it is critical to avoid imposing blame on family members. This can be a fine line to walk with families. At the same time of explaining that they did not cause the symptoms or difficulty with functioning, they are told that they can still affect these outcomes in their loved one. To start, family members should be informed that they could play a protective role for their relative who is at high clinical risk for developing psychosis. In particular, family members should be informed of the importance of maintaining a “low-key” home environment. Examples that describe aspects of a low-EE environment could be shared with families. In addition, it could be beneficial if family members are informed of the importance of combining appropriate protectiveness and concern with warmth, as this led to improved functioning in the current study. Future research studies should test the efficacy of providing this type of psychoeducation to families.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Jamie L. Zinberg, Email: jzinberg@psych.ucla.edu.
Rachel L. Loewy, Email: rloewy@lppi.ucsf.edu.
Shannon Casey-Cannon, Email: scasey-cannon@alliant.edu.
Mary P. O’Brien, Email: maryobrien@cox.net.
Carrie E. Bearden, Email: cbearden@mednet.ucla.edu.
Sophia Vinogradov, Email: sophia.vinogradov@ucsf.edu.
Tyrone D. Cannon, Email: cannon@psych.ucla.edu.
References
- Butzlaff RL, Hooley JM. Expressed emotion and psychiatric relapse. Arch Gen Psychiatry. 1998;55(6):547–552. doi: 10.1001/archpsyc.55.6.547. [DOI] [PubMed] [Google Scholar]
- Cannon TD, Cadenhead KD, Cornblatt B, Woods SW, Jean A, Walker E, Seidman LJ, Perkins D, Ming T, McGlashan T, Heinssen R. Prediction of psychosis in youth at high clinical risk: A multisite longitudinal study in North America. Arch Gen Psychiatry. 2008;65(1):28–37. doi: 10.1001/archgenpsychiatry.2007.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hooley JM. Expressed emotion and relapse of psychopathology. Annu Rev Clin Psychol. 2007;3:329–352. doi: 10.1146/annurev.clinpsy.2.022305.095236. [DOI] [PubMed] [Google Scholar]
- Hooley JM, Richters JE. Expressed emotion: A developmental perspective. In: Cicchetti D, Toth SL, editors. Emotion, cognition, and representation. University of Rochester Press; Rochester, NY, US: 1995. pp. 136–166. [Google Scholar]
- Hooley JM, Teasdale JD. Predictors of relapse in unipolar depressives: Expressed emotion, marital distress, and perceived criticism. J Abnorm Psychol. 1989;98:229–235. doi: 10.1037//0021-843x.98.3.229. [DOI] [PubMed] [Google Scholar]
- Kavanagh DJ. Recent developments in expressed emotion and schizophrenia. Br J Psychiatry. 1992;160:601–620. doi: 10.1192/bjp.160.5.601. [DOI] [PubMed] [Google Scholar]
- Leff J, Vaughn C. Expressed emotion in families. Guilford Press; New York: 1985. [Google Scholar]
- Miklowitz DJ. The role of family systems in severe and recurrent psychiatric disorders: A developmental psychopathology view. Dev Psychopathol. 2004;16:667–688. doi: 10.1017/s0954579404004729. [DOI] [PubMed] [Google Scholar]
- Miklowitz DJ, Goldstein MJ, Falloon IR. Premorbid and symptomatic characteristics of schizophrenics from families with high and low expressed emotion. J Abnorm Psychol. 1983;92(3):359–367. doi: 10.1037//0021-843x.92.3.359. [DOI] [PubMed] [Google Scholar]
- Miller TJ, McGlashan TH, Rosen JL. Prospective diagnosis of the initial prodrome for schizophrenia based on the structured interview for prodromal syndromes: preliminary evidence of inter-rater reliability and predictive validity. Am J Psychiatry. 2002;159:863–865. doi: 10.1176/appi.ajp.159.5.863. [DOI] [PubMed] [Google Scholar]
- O’Brien MP, Gordon JL, Bearden CE, Lopez SR, Kopelowicz, Cannon TD. Positive family environment predicts improvement in symptoms and social functioning among adolescents at imminent risk for onset of psychosis. Schizophr Res. 2006;81:269–275. doi: 10.1016/j.schres.2005.10.005. [DOI] [PubMed] [Google Scholar]
- Strauss JS, Carpenter WT. The prediction of outcome in schizophrenia: I. Characteristics of outcome. Arch Gen Psychiatry. 1972;27:739–746. doi: 10.1001/archpsyc.1972.01750300011002. [DOI] [PubMed] [Google Scholar]
- Tienari P, Wahlberg K, Wynne L. Finnish Adoption Study of Schizophrenia: Implications for Family Interventions. Fam Syst Health. 2006;24(4):442–451. [Google Scholar]
- Tienari P, Wynne LC, Läksy K, Moring J, Neiminene P, Sorri A, Lahti I, Wahlberg K. Genetic Boundaries of the Schizophrenia Spectrum: Evidence From the Finnish Adoptive Family Study of Schizophrenia. Am J Psychiatry. 2003;160(9):1587–1594. doi: 10.1176/appi.ajp.160.9.1587. [DOI] [PubMed] [Google Scholar]
- Weisman AG, Nuechterlein KH, Goldstein MJ, Snyder KS. Expressed emotion, attributions, and schizophrenia symptom dimensions. J of Abnorm Psychol. 1998;107:355–359. doi: 10.1037//0021-843x.107.2.355. [DOI] [PubMed] [Google Scholar]
- Yung AR, McGorry PR. The prodromal phase of first-episode psychosis: Past and current conceptualizations. Schizophr Bull. 1996;22(2):353–370. doi: 10.1093/schbul/22.2.353. [DOI] [PubMed] [Google Scholar]