Abstract
OBJECTIVES
National leaders have suggested that patients with an out-of-hospital cardiac arrest (OOHCA) may benefit from transport to specialized hospitals. We sought to assess the survival of OOHCA patients by transport distance and hospital proximity.
METHODS
Prospective, cohort study of OOHCA patients in 11 Resuscitation Outcomes Consortium (ROC) sites across North America. Transport distance and hospital proximity was calculated using weighted centroid of census tract location by Geographic Information Systems (GIS). Patients were stratified into quartiles based on transport distance to the receiving hospital calculated via GIS. Descriptive statistics were used to describe characteristics by transport distance and to compare proximity to other hospitals. Multivariate logistic regression was used to evaluate the impact of transport distance on survival.
RESULTS
26,628 patients were identified, 7,540 (28%) were transported by EMS and included in the final analysis. The median transport time was 6.3 minutes (IQR 5.4); the median transport distance being 2.4 miles (3.9 km). Most patients were taken to the closest hospital (71.7%; N=5,412). However, unadjusted survival to discharge was lower for those taken to the closest compared to further hospitals (12.1% vs. 16.5%) despite similar patient characteristics. Transport distance was not associated with survival on logistic analysis (OR 1.00; 95% CI 0.99–1.01).
CONCLUSIONS
Survival to discharge was higher in OOHCA patients taken to hospitals located further than the closest hospital while transport distance was not associated with survival. This suggests that longer transport distance/time might not adversely affect outcome. Further studies are needed to inform policy decisions regarding best destination post cardiac arrest
INTRODUCTION
Out of hospital cardiac arrest (OOHCA) continues to be a leading cause of death in the United States (U.S.).1 Survival from OOHCA varies considerably across the country and until recently had been relatively stagnant over the last several decades.2 However, the advent of recent interventions such as induced-hypothermia and early cardiac catheterization, along with higher quality cardiopulmonary resuscitation (CPR) in the prehospital setting, has led to a distinct increase in survival.3–5 Despite these advances, various regions and hospitals in the U.S. have been slow to adopt such measures in order to improve outcomes from OOHCA.
Based on this information, as well as the success of regionalized trauma centers and their impact on survival in injured patients,6, 7 many leaders have called for development and implementation of cardiac arrest centers.8 Some areas of the country, such as the state of Arizona, are actively developing such centers.9 However, before such centers are deemed appropriate, it must be determined that it is safe to bypass closer hospitals in order to transport a patient to a hospital further away but with additional resources to optimize the care of such patients. To date, there has been limited data evaluating the safety and impact of such a practice on survival of OOHCA patients.10–12
In light of the growing interest in developing and implementing regionalization of specialized care for OOHCA, we sought to assess the impact of transport distance on survival in OOHCA patients and to assess the characteristics of hospitals that care for OOHCA patients. We hypothesized that an increase in transport distance would not be associated with a decrease in survival, nor would transport to a closer hospital be associated with improvement in survival.
METHODS
This was a secondary analysis of a prospective, observational, multi-center, population-based cohort study in 10 of 11 North American sites participating in the Resuscitation Outcomes Consortium (ROC). One site was excluded due to incomplete case capture across the study’s time frame. This project was approved by 74 U.S. Institutional Review Boards (IRB) and 34 Canadian Research Ethics Boards as well as 26 Emergency Medical Services (EMS) IRBs and the IRB at the Ohio State University Medical Center.
We included all patients who suffered an OOHCA and were entered into the ROC Epistry—Cardiac Arrest from December 2005 through June 2007. This is a multi-center epidemiologic-based cardiac arrest registry, the methodology of which has been detailed elsewhere.13 Briefly, this is a population-based registry of all EMS-attended 9-1-1 calls for patients with OOHCA occurring in the geographical areas of all participating sites in North America. This contains information submitted from over 200 EMS agencies and over 200 hospitals that participate in ROC covering an area of approximately 33,000 square miles servicing a population of approximately 20,000,000 people. Prehospital and in-hospital data are included in Epistry. Quality Assurance (QA) measures are in place that are consistent between sites (initial EMS provider training with continued education, annual review of random records to ensure accurate data entry) as well as to the consortium as a whole (annual site visits by Data Coordinating Center to review records submitted, data abstraction process, review site QA measures) to ensure consistent and reliable data collection. Some aspects of the individual sites QA processes (timing of training, schedule of training at individual sites) vary and are specific to each site.
For this project, we identified all adult patients (≥18 years of age) who suffered an OOHCA; however, the primary analysis was restricted to those patients transported to a hospital. Patients were considered to have an OOHCA based on Utstein criteria.14 Patients were excluded if they were not treated by EMS or if resuscitation was not initiated (due to family request, a do not attempt resuscitative directive signed and dated by a physician), if they were treated by EMS but not transported, if the etiology of the arrest was non-cardiac, or if there were missing data in key variables or outcomes.
Variables collected and included in the analysis were: gender, age, presenting rhythm (ventricular fibrillation/pulseless ventricular tachycardia [VF/VT] vs. other), witnessed vs. unwitnessed arrest, bystander CPR (yes, no), bystander automated external defibrillator use (yes, no), advanced life support vs. basic life support first responder, response time (in minutes, defined as time from 9-1-1 call to first responder arrival time), census tract of event, and ROC site (10 total). Age and response time were continuous variables, all others were categorical. Hospital-level variables that were collected and analyzed included: presence/absence of a cardiac catheterization lab, presence/absence of an electrophysiology lab, mean number of beds and the teaching status of the institution (yes/no). Whether or not a patient received specific interventions is not available via Epistry. The outcome of interest was survival to hospital discharge, defined as leaving the hospital alive. Epistry does not have data pertaining to the neurologic status of patients at discharge.
Two methods of transport distance, point and driving, were calculated using Geographic Information Systems (GIS) (ArcGis version 9.1 ESRI, Redland CA). Since the exact address and/or latitude/longitude coordinates of each arrest are not routinely captured in Epistry, the location of the arrest was estimated via the population-weighted centroid of the census tract.15 Although this is somewhat less accurate than the actual distance, prior work has shown that it has very good correlation with the exact distance from a point location.16 Point distance, or straight line (Euclidean) distance, from this weighted centroid to each hospital was calculated via the distance formula. This, in essence, calculates the shortest distance between two points. Driving distance was calculated via network distance along the road network to the nearest hospital as well as to the transported hospital. Network distance was calculated with ESRI’s Network Analysis extension in ArcInfo 9.1, which computed the shortest distance along the road network to the hospitals.15 Hospitals or centroids of census tract that did not fall on a network location were moved to the closest geographical point. Distance was rounded to the nearest mile.17 In order to identify how well point distance and driving distance correlated, Pearson’s correlation coefficients were calculated.
We also created a categorical, hospital variable to evaluate the impact of “bypassing” the closest hospital to go to a specialized hospital that is further away in order to ascertain the safety of it. This did not assume that an ambulance actually drove past one hospital to go to another, although this could happen if the closest hospital was encountered on the way to the furthest hospital. Furthermore, this variable would also serve as a potential surrogate for hospital characteristics, as the assumption is that a further hospital would have more resources. The hospital variable was a categorical variable for whether or not a patient was transported to the closest hospital. The closest hospital was defined as the closest hospital in miles to the event itself as defined above. If the patient was located at an equal distance between two hospitals, we assumed the patient was taken to the closest hospital.
Descriptive statistics were used to describe the study population and were reported as means with 95% confidence intervals or medians with inter-quartile ranges (IQR), where appropriate. Similar descriptive statistics were utilized to characterize the hospitals. In order to ascertain any differences in patient characteristics based on transport distance to the hospital, patients were stratified into quartiles of transport distance. Continuous and categorical variables were compared via X2 Analysis, Wilcoxon rank sum test, and Student’s t test, where appropriate. Pearson’s correlation coefficients were calculated to determine if there was any correlation between presenting rhythm and type of hospital (closer vs. further). Multivariable logistic regression analysis was used to evaluate the association between transport distance and survival as well as bypassing the closest hospital and survival, adjusting for the previously mentioned confounders. A p-value <0.05 was considered statistically significant for all tests. Hosmer-Lemeshow goodness of fit was used to assess the overall model fit.
In order to test the safety of such a practice in those patients whom might be most salvageable, we performed a sensitivity analysis including only patients who had return of spontaneous circulation (ROSC) on arrival in the ED in the models mentioned above. Additionally, to account for any potential clustering of patients based on the ROC site, we performed a random-effects model to account for any potential clustering.18 Furthermore, in order to add further validity to the concept of regionalization similar to that instilled by trauma centers in the U.S., we performed a subset analysis of those patients taken only to a Level I trauma center.
SPlus (v. 6.2, Seattle, WA) was used for database management and analyses.
RESULTS
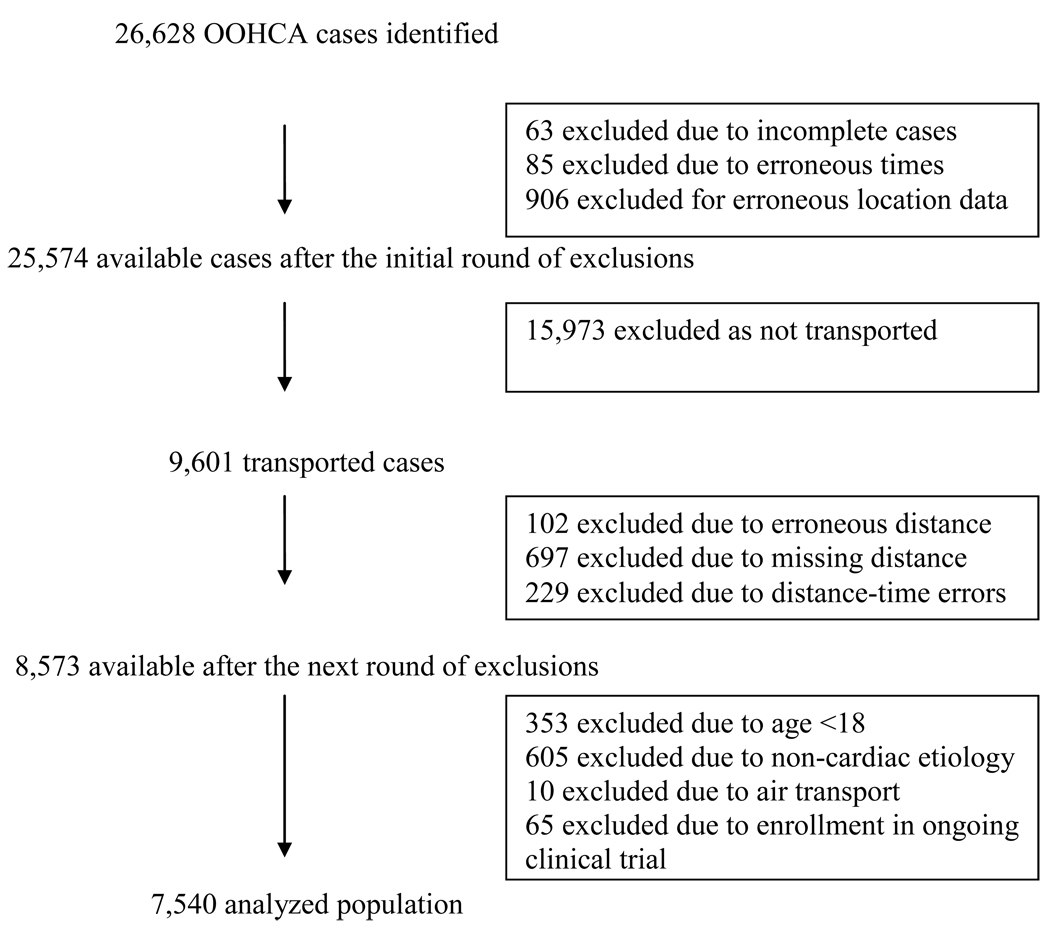
A total of 26,628 patients were identified, of which 7,540 (28%) were transported to a hospital with complete data (Figure 1). Of these, 5,412 (72%) were transported to the closest hospital. The majority of patients were male, arrested in a private setting, and had a non-VF/VT presenting rhythm (Table 1). Receiving hospitals located further from the events were more likely to have a cardiac catheterization lab, an electrophysiology lab, higher patient volumes, and were a teaching institution. (Table 2)
Figure 1.
Table 1.
Patient and System Characteristics for Transported Patients with an Out of Hospital Cardiac Arrest by Transport Distance
| 1st Quartile 0.06 m/0.09km (N=1887) |
2nd Quartile 1.37 m/2.20 km (N=1883) |
3rd Quartile 2.42 m/3.89 km (N=1883) |
4th Quartile 3.84 m/6.18 km (N=1885) |
|
|---|---|---|---|---|
| % (n) Male | 66% (1245) | 64% (1213) | 65% (1214) | 65% (1218) |
| Median Age in years (IQR) | 66 (25) | 68 (24) | 68 (25) | 66 (25) |
| % (n) Public location of arrest | 26% (482) | 20% (370) | 20% (371) | 19% (354) |
| % (n) VF/VT | 33% (631) | 31% (592) | 32% (607) | 35% (654) |
| % (n) Bystander Witness | 46% (868) | 42% (789) | 44% (834) | 43% (817) |
| % (n) Bystander CPR | 31% (584) | 27% (509) | 27% (505) | 30% (557) |
| % (n) ALS | 44% (836) | 52% (987) | 48% (907) | 50% (946) |
| Median Response Time in minutes (IQR) |
5.00 min (2.35) | 5.08 min (2.52) | 5.38 min (2.97) | 5.87 min (3.76) |
m=mile
km=kilometer
IQR: interquartile range
VF/VT: Ventricular fibrillation/Ventricular tachycardia
CPR: cardiopulmonary resuscitation
ALS: advanced life support was first on scene
Table 2.
Hospital Characteristics
| Closest Hospital (n=5412) |
Further Hospital (n=2128) |
|
|---|---|---|
| Catheterization Lab | 3140 (58%) | 1700 (80%) |
| Electrophysiology Lab | 634 (12%) | 490 (23%) |
| Beds | 342 (247) | 431 (352) |
| Teaching Institute | 2489 (46%) | 1505 (71%) |
%=percentage
SD=standard deviation
The overall mean difference in transport distance in patients taken to the further hospital compared to the closest hospital was 1.70 miles (2.74 kilometers). The correlation between point distance and driving distance was very high, ρ=0.90. When comparing overall survival, those taken to a further hospital had better survival compared to a closer hospital (16.5% vs. 12.1%, p<0.001). Those patients with VF/VT transported to a further hospital had better survival than those taken to a closer hospital (32.8% vs. 25.6%, p<0.001). In a small subset of patients with a mean transport difference greater than 5 miles (N=151), those transported to a further hospital had a trend for improved survival (17.5% vs. 12.1%, p=0.06). The overall survival by presenting rhythm for each ROC site is displayed in Table 3. The vast majority of survivors had VF/VT as their presenting rhythm. There was poor correlation between presenting rhythm and which hospital a patient was transported to (ρ=0.03)
Table 3.
Patient Survival by Presenting Rhythm
| ROC Site | Non-VF/VT n (%) |
VF/VT n (%) |
|---|---|---|
| A | 2 (1.1%) | 5 (6.3%) |
| B | 9 (3.8%) | 28 (30.8%) |
| C | 13 (5.3%) | 28 (24.1%) |
| D | 16 (2.2%) | 21 (9.2%) |
| E | 24 (10%) | 57 (49.1%) |
| F | 25 (3.5%) | 73 (18.1%) |
| G | 25 (4.9%) | 152 (35.8%) |
| H | 34 (14.6%) | 120 (51.3%) |
| I | 35 (10.1%) | 94 (30.4%) |
| J | 48 (5.2%) | 100 (22.6%) |
ROC: Resuscitation Outcomes Consortium
VF/VT: Ventricular Fibrillation/Ventricular Tachycardia
n=raw number of survivors
%=mortality percentage by ROC site
On multivariate analysis, after adjusting for several confounders (Table 4), transport distance, both point and driving distance, were not associated with survival (Odds Ratio [OR] 1.00; 95% Confidence Interval [CI] 0.99–1.01). Additionally, when assessing the impact of “bypassing” the closest hospital (Table 5), those patients transported to the closest hospital were found to have decreased survival compared to those taken to a further hospital (OR 0.82; 95% CI 0.69–0.97).
Table 4.
Multivariable Logistic Regression Model Assessing the Effect of Transport Distance on Survival to Hospital Discharge, Adjusting for Potential Confounders
| Odds Ratio | 95% Confidence Interval | |
|---|---|---|
| Distance (per km) | 1.00 | (0.99, 1.01) |
| Male | 0.90 | (0.76, 1.07) |
| Age (per year) | 1.05 | (1.02, 1.08) |
| Non-VF/VT Initial Rhythm | 0.19 | (0.16, 0.22) |
| EMS Witnessed | 2.14 | (1.76, 2.62) |
| Bystander Resuscitation | 2.22 | (1.02, 4.85) |
| Bystander AED | 3.49 | (2.25, 5.42) |
| Response time | 0.67 | (0.56, 0.80) |
| Site 2 | 1.60 | (0.69, 3.70) |
| Site 3 | 5.06 | (2.18, 11.8) |
| Site 4 | 11.9 | (5.30, 26.9) |
| Site 5 | 3.51 | (1.59, 7.78) |
| Site 6 | 4.35 | (1.84, 10.3) |
| Site 7 | 5.84 | (2.62, 13.1) |
| Site 8 | 16.1 | (7.23, 35.7) |
| Site 9 | 5.32 | (2.42, 11.7) |
| Site10 | 8.52 | (3.88, 18.7) |
| ALS first responder | 1.16 | (0.94, 1.42) |
VF/VT: Ventricular Fibrillation /Ventricular Tachycardia
AED: Automated External Defibrillator
ALS: Advanced Life Support was first on scene
Table 5.
Multivariable Logistic Regression Model Assessing the Effect of Bypass of Closest Hospital on Survival to Hospital Discharge, Adjusting for Potential Confounders
| Odds Ratio | 95% Confidence Interval | |
|---|---|---|
| Transport to Closest Hospital | 0.82 | (0.69, 0.97) |
| Male | 0.90 | (0.69, 1.07) |
| Age (per year) | 1.05 | (1.02, 1.08) |
| Non-VF/VT Initial Rhythm | 0.19 | (0.16, 0.22) |
| Witnessed | 2.14 | (1.76, 2.61) |
| Bystander Resuscitation | 2.29 | (1.05, 4.98) |
| Bystander AED | 3.53 | (2.27, 5.47) |
| Response time | 0.67 | (0.57, 0.79) |
| Site 2 | 1.58 | (0.68, 3.66) |
| Site 3 | 4.86 | (2.09, 11.3) |
| Site 4 | 11.5 | (5.08, 25.9) |
| Site 5 | 3.51 | (1.58, 7.76) |
| Site 6 | 4.16 | (1.76, 9.85) |
| Site 7 | 5.76 | (2.58, 12.9) |
| Site 8 | 15.1 | (6.77, 33.5) |
| Site 9 | 5.30 | (2.41, 11.6) |
| Site 10 | 8.54 | (3.89, 18.8) |
| ALS first responder | 1.16 | (0.94, 1.43) |
VF/VT: Ventricular Fibrillation/Ventricular Tachycardia
AED: Automated External Defibrillator
ALS: Advanced Life Support was first on scene
On sensitivity analysis, evaluating only those patients with ROSC on ED arrival, transport distance, both point and driving distance, were not associated with survival (OR 1.00; 95% CI 0.98–1.02). No difference in survival was seen in those transported to the closest hospital compared to those taken to a further hospital (OR 0.86; 95% CI 0.66–1.12). Unadjusted survival was similar in those without ROSC, regardless of hospital destination (2.4% vs. 1.6%, p=0.14). After allowing site to be a random effect, transport distance, both point and driving distance, were not associated with survival (OR 1.00; 95% CI 1.00–1.01). Decreased survival in those transported to the closest hospital compared to those taken to the further hospital was also observed (OR 0.98; 95% CI 0.96–0.99).
In the subset analysis evaluating patients only taken to Level I trauma centers, those taken to a further hospital also had better unadjusted survival compared to those taken to a closer hospital (18.7% vs. 13.9%, p=0.01).
DISCUSSION
In this project, we have observed that transport distance in patients with an OOHCA is not associated with survival, and that transport to a closer hospital may indeed be associated with lower odds of survival. This is consistent with prior literature that has investigated whether an increase in transport time is associated with a decrease in the odds of survival.10–12 This data, coupled with the prior literature, suggests that transport to further hospitals, such as cardiac arrest receiving centers, should not negatively impact the survivability from OOHCA.
In two different patient populations, Spaite et al demonstrated that transport interval, as measured by time, was not associated with an increase in mortality.11, 12 Additionally, Davis et al found a similar relationship in San Diego.10 We used transport distance rather than transport time because distance offers a fixed data point that could be used by EMS directors, physicians, and health policy leaders, to model appropriate transport protocols to potential cardiac arrest centers. Such an assumption has been justified as a valid measure in developing policy with regards to access to medical centers and hospitals.19 Furthermore, transport time can vary based on time of the day, day of the week, traffic volume, and weather conditions, whereas transport distance will remain constant. Moreover, prior work has shown a strong correlation between straight line distance via GIS and travel time, further justifying it use.19, 20 Finally, prior work has shown that transport time is not associated with mortality in OOHCA patients.10–12 We feel that our findings add to and complement existent literature supporting the potential benefit of regionalization of cardiac arrest care.
Our project has a few distinct differences compared to the previously mentioned work. We were able to demonstrate these findings in a large, heterogeneous population, across multiple different geographic areas in two different countries, potentially increasing the generalizability of these findings. Furthermore, rather than evaluate transport time, a variable that is highly dependent on several factors, we chose to evaluate transport distance, a fixed and more independent variable. By using a fixed variable such as distance, it is possible to develop transport protocols to the most capable facilities (i.e. hypothermia capabilities, 24 hour cardiac catheterization capabilities) that are located within a certain distance from the site of the arrest rather than estimate what the potential transport time might be. These findings, coupled with prior literature, suggest that neither transport time, nor transport distance are associated with mortality, thus adding to the safety and potential benefit of receiving cardiac arrest centers.
These findings are not surprising given the current literature in the care of OOHCA patients. It is no longer considered true that only prehospital interventions (shorter response time, early defibrillation, bystander CPR) improve survival for OOHCA.21–23 Recent studies have shown that various hospital characteristics as well as standardized in-hospital care of OOHCA patients is associated with improved outcomes.4, 24–27 Although not specifically evaluated in this project, those hospitals that were located further from the site of arrest were more likely to have more capabilities, to have higher volumes of patients, and to be a teaching institution, all of which have been shown to be associated with improved outcomes in other patient populations.28–33 Additionally, prior work via ROC has shown that hospitals with a congregation of specialized services are associated with improved outcomes in OOHCA patients.34 This information, coupled with evidence suggesting that standardized, bundled treatment strategies improves survival,35 are the foundational arguments for post-OOHCA resuscitation centers.
Clearly, there are additional barriers that will need to be overcome at the state, regional, and local levels before the establishment of cardiac arrest centers can be safely and efficiently developed and implemented. It would be ideal to model other effects on a policy change to centralize resuscitation care, such as the reduction in other capabilities within smaller hospitals and potential increased overcrowding in the larger centers. One limitation addressed in this project is the generalizability of these findings with other systems. ROC was developed and implemented in order to make their findings generalizable to all parts of the U.S. and Canada. The findings of this project were obtained from more than 200 hospitals and more than 200 EMS agencies, constituting urban, suburban, and rural settings, suggesting that it is not limited to one type of system or one type of geographical region. By assessing the potential impact of transport distance over such a wide array of settings through several vast populations further suggests that the practice of bypassing a closer hospital to transport to a further, more capable hospital may indeed be safe and perhaps necessary.
LIMITATIONS
This project is not without its limitations. We did not evaluate for the impact of hospital characteristics or interventions at the hospital or patient level. The objective was to assess the impact of transport distance to determine the safety of transporting to hospitals with perhaps more advanced capabilities. However, we did attempt to incorporate these characteristics using our surrogate marker of hospital bypass. As the hospitals located further from the event tended to have more capabilities and qualities that may be associated with improved survival, this appeared to be an appropriate surrogate for more specialized centers. However, future projects should evaluate if hospitals with more experience with and higher volumes of characteristics such as hypothermia and cardiac catheterization improve survival.
It is possible that hospitals located closer to the site of the arrest may serve as a marker for selection bias. Patients in whom ROSC was not achieved and who would not survive regardless of where they are transported may have selectively been transported to the closest hospital. While this may be true, we attempted to account for this in our sensitivity analysis evaluating only those patients with ROSC at ED arrival and found similar findings, suggesting that such bias is minimal. Although not reaching statistical significance in our study, it is possible that the lack of statistical significance can be accounted for by the decrease in sample size (N=1,681) which is partly attributable to the fact that the ROSC at ED arrival variable was not captured in the first version of Epistry.
Finally, we were unable to adjust for unmeasured confounders, such as bypassing hospitals that may be full or the triaging of patients by medics or the EMS dispatcher.
CONCLUSIONS
In this project, transport distance is not associated with survival to discharge in OOHCA patients. This supports the concept that transporting a patient to a further hospital with more advanced capabilities may be beneficial and safe. Future research should evaluate the impact of hospital-based interventions and policy changes that promote resuscitation centers on survival in OOHCA patients in order to evaluate the potential effectiveness of cardiac arrest receiving centers.
Acknowledgments
Funding: The ROC is supported by a series of cooperative agreements to 10 regional clinical centers and one Data Coordinating Center (5U01 HL077863,HL077881,HL077871 HL077872, HL077866, HL077908, HL077867, HL077885, HL077887, HL077873, HL077865) from the National Heart, Lung and Blood Institute in partnership with the National Institute of Neurological Disorders and Stroke, U.S. Army Medical Research & Material Command, The Canadian Institutes of Health Research (CIHR) - Institute of Circulatory and Respiratory Health, Defense Research and Development Canada, the American Heart Association and the Heart and Stroke Foundation of Canada. Additional support for this project was provided to one author (MTC) via the American Heart Association Scientist Development Grant #0835250N.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Presented in Abstract Form at the Society for Academic Emergency Medicine Annual Research Forum, New Orleans, LA; May 17, 2009
Conflict of Interest Statement
None of the authors of this paper have any financial or personal relationships with other people or organizations that could inappropriately influence (bias) this paper.
Reference List
- 1.Rosamond W, Flegal K, Furie K, et al. Heart disease and stroke statistics--2008 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2008 January 29;117(4):e25–e145. doi: 10.1161/CIRCULATIONAHA.107.187998. [DOI] [PubMed] [Google Scholar]
- 2.Nichol G, Thomas E, Callaway CW, et al. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2008 September 24;300(12):1423–1431. doi: 10.1001/jama.300.12.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bernard SA. Hypothermia improves outcome from cardiac arrest. Crit Care Resusc. 2005 December;7(4):325–327. [PubMed] [Google Scholar]
- 4.Reynolds JC, Callaway CW, El K, Sr, Moore CG, Alvarez RJ, Rittenberger JC. Coronary Angiography Predicts Improved Outcome Following Cardiac Arrest: Propensity-adjusted Analysis. J Intensive Care Med. 2009 March 25; doi: 10.1177/0885066609332725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kellum MJ, Kennedy KW, Barney R, et al. Cardiocerebral resuscitation improves neurologically intact survival of patients with out-of-hospital cardiac arrest. Ann Emerg Med. 2008 September;52(3):244–252. doi: 10.1016/j.annemergmed.2008.02.006. [DOI] [PubMed] [Google Scholar]
- 6.MacKenzie EJ, Rivara FP, Jurkovich GJ, et al. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med. 2006 January 26;354(4):366–378. doi: 10.1056/NEJMsa052049. [DOI] [PubMed] [Google Scholar]
- 7.Demetriades D, Martin M, Salim A, et al. Relationship between American College of Surgeons trauma center designation and mortality in patients with severe trauma (injury severity score > 15) J Am Coll Surg. 2006 February;202(2):212–215. doi: 10.1016/j.jamcollsurg.2005.09.027. [DOI] [PubMed] [Google Scholar]
- 8.Lurie KG, Idris A, Holcomb JB. Level 1 cardiac arrest centers: learning from the trauma surgeons. Acad Emerg Med. 2005 January;12(1):79–80. doi: 10.1197/j.aem.2004.11.010. [DOI] [PubMed] [Google Scholar]
- 9.Geyer B, Bobrow BJ, Spaite D, et al. A Statewide Network of Cardiac Arrest Centers Significantly Improves Outcomes from Out of Hospital Cardiac Arrest. Acad.Emerg.Med. 16[S1]. 4-1-2009. Ref Type: Abstract. [Google Scholar]
- 10.Davis DP, Fisher R, Aguilar S, et al. The feasibility of a regional cardiac arrest receiving system. Resuscitation. 2007 July;74(1):44–51. doi: 10.1016/j.resuscitation.2006.11.009. [DOI] [PubMed] [Google Scholar]
- 11.Spaite DW, Stiell IG, Bobrow BJ, et al. Effect of Transport Interval on Out-of-Hospital Cardiac Arrest Survival in the OPALS Study: Implications for Triaging Patients to Specialized Cardiac Arrest Centers. Ann Emerg Med. 2009 January 22; doi: 10.1016/j.annemergmed.2008.11.020. [DOI] [PubMed] [Google Scholar]
- 12.Spaite DW, Bobrow BJ, Vadeboncoeur TF, et al. The impact of prehospital transport interval on survival in out-of-hospital cardiac arrest: implications for regionalization of post-resuscitation care. Resuscitation. 2008 October;79(1):61–66. doi: 10.1016/j.resuscitation.2008.05.006. [DOI] [PubMed] [Google Scholar]
- 13.Morrison LJ, Nichol G, Rea TD, et al. Rationale, development and implementation of the Resuscitation Outcomes Consortium Epistry-Cardiac Arrest. Resuscitation. 2008 August;78(2):161–169. doi: 10.1016/j.resuscitation.2008.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cummins RO, Chamberlain DA, Abramson NS, et al. Recommended guidelines for uniform reporting of data from out-of-hospital cardiac arrest: the Utstein Style. A statement for health professionals from a task force of the American Heart Association, the European Resuscitation Council, the Heart and Stroke Foundation of Canada, and the Australian Resuscitation Council. Circulation. 1991 August;84(2):960–975. doi: 10.1161/01.cir.84.2.960. [DOI] [PubMed] [Google Scholar]
- 15.Sharkey JR, Horel S. Neighborhood socioeconomic deprivation and minority composition are associated with better potential spatial access to the ground-truthed food environment in a large rural area. J Nutr. 2008 March;138(3):620–627. doi: 10.1093/jn/138.3.620. [DOI] [PubMed] [Google Scholar]
- 16.Apparicio P, Abdelmajid M, Riva M, Shearmur R. Comparing alternative approaches to measuring the geographical accessibility of urban health services: Distance types and aggregation-error issues. Int J Health Geogr. 2008;7:7. doi: 10.1186/1476-072X-7-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Voti L, Richardson LC, Reis IM, Fleming LE, Mackinnon J, Coebergh JW. Treatment of local breast carcinoma in Florida: the role of the distance to radiation therapy facilities. Cancer. 2006 January 1;106(1):201–207. doi: 10.1002/cncr.21557. [DOI] [PubMed] [Google Scholar]
- 18.Wears RL. Advanced statistics: statistical methods for analyzing cluster and cluster-randomized data. Acad Emerg Med. 2002 April;9(4):330–341. doi: 10.1111/j.1553-2712.2002.tb01332.x. [DOI] [PubMed] [Google Scholar]
- 19.Fone DL, Christie S, Lester N. Comparison of perceived and modelled geographical access to accident and emergency departments: a cross-sectional analysis from the Caerphilly Health and Social Needs Study. Int J Health Geogr. 2006;5:16. doi: 10.1186/1476-072X-5-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Haynes R, Jones AP, Sauerzapf V, Zhao H. Validation of travel times to hospital estimated by GIS. Int J Health Geogr. 2006;5:40. doi: 10.1186/1476-072X-5-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.De MV, Stiell IG, Wells GA, Spaite DW. Optimal defibrillation response intervals for maximum out-of-hospital cardiac arrest survival rates. Ann Emerg Med. 2003 August;42(2):242–250. doi: 10.1067/mem.2003.266. [DOI] [PubMed] [Google Scholar]
- 22.Eisenberg MS. Improving survival from out-of-hospital cardiac arrest: back to the basics. Ann Emerg Med. 2007 March;49(3):314–316. doi: 10.1016/j.annemergmed.2006.07.008. [DOI] [PubMed] [Google Scholar]
- 23.Herlitz J, Engdahl J, Svensson L, Angquist KA, Young M, Holmberg S. Factors associated with an increased chance of survival among patients suffering from an out-of-hospital cardiac arrest in a national perspective in Sweden. Am Heart J. 2005 January;149(1):61–66. doi: 10.1016/j.ahj.2004.07.014. [DOI] [PubMed] [Google Scholar]
- 24.Herlitz J, Castren M, Friberg H, et al. Post resuscitation care: what are the therapeutic alternatives and what do we know? Resuscitation. 2006 April;69(1):15–22. doi: 10.1016/j.resuscitation.2005.08.006. [DOI] [PubMed] [Google Scholar]
- 25.Engdahl J, Abrahamsson P, Bang A, Lindqvist J, Karlsson T, Herlitz J. Is hospital care of major importance for outcome after out-of-hospital cardiac arrest? Experience acquired from patients with out-of-hospital cardiac arrest resuscitated by the same Emergency Medical Service and admitted to one of two hospitals over a 16-year period in the municipality of Goteborg. Resuscitation. 2000 February;43(3):201–211. doi: 10.1016/s0300-9572(99)00154-9. [DOI] [PubMed] [Google Scholar]
- 26.Spaulding CM, Joly LM, Rosenberg A, et al. Immediate coronary angiography in survivors of out-of-hospital cardiac arrest. N Engl J Med. 1997 June 5;336(23):1629–1633. doi: 10.1056/NEJM199706053362302. [DOI] [PubMed] [Google Scholar]
- 27.Borger van der Burg AE, Bax JJ, Boersma E, et al. Impact of percutaneous coronary intervention or coronary artery bypass grafting on outcome after nonfatal cardiac arrest outside the hospital. Am J Cardiol. 2003 April 1;91(7):785–789. doi: 10.1016/s0002-9149(03)00008-0. [DOI] [PubMed] [Google Scholar]
- 28.Nathens AB, Jurkovich GJ, Maier RV, et al. Relationship between trauma center volume and outcomes. JAMA. 2001 March 7;285(9):1164–1171. doi: 10.1001/jama.285.9.1164. [DOI] [PubMed] [Google Scholar]
- 29.Thiemann DR, Coresh J, Oetgen WJ, Powe NR. The association between hospital volume and survival after acute myocardial infarction in elderly patients. N Engl J Med. 1999 May 27;340(21):1640–1648. doi: 10.1056/NEJM199905273402106. [DOI] [PubMed] [Google Scholar]
- 30.Tu JV, Austin PC, Chan BT. Relationship between annual volume of patients treated by admitting physician and mortality after acute myocardial infarction. JAMA. 2001 June 27;285(24):3116–3122. doi: 10.1001/jama.285.24.3116. [DOI] [PubMed] [Google Scholar]
- 31.Hannan EL, Wu C, Ryan TJ, et al. Do hospitals and surgeons with higher coronary artery bypass graft surgery volumes still have lower risk-adjusted mortality rates? Circulation. 2003 August 19;108(7):795–801. doi: 10.1161/01.CIR.0000084551.52010.3B. [DOI] [PubMed] [Google Scholar]
- 32.Meguid RA, Brooke BS, Chang DC, Sherwood JT, Brock MV, Yang SC. Are surgical outcomes for lung cancer resections improved at teaching hospitals? Ann Thorac Surg. 2008 March;85(3):1015–1024. doi: 10.1016/j.athoracsur.2007.09.046. [DOI] [PubMed] [Google Scholar]
- 33.Polanczyk CA, Lane A, Coburn M, Philbin EF, Dec GW, DiSalvo TG. Hospital outcomes in major teaching, minor teaching, and nonteaching hospitals in New York state. Am J Med. 2002 March;112(4):255–261. doi: 10.1016/s0002-9343(01)01112-3. [DOI] [PubMed] [Google Scholar]
- 34.Callaway CW, Schmicker R, Kampmeyer M, et al. Influence of Receiving Hospital Characteristics on Survival after Cardiac Arrest. Circulation. 118(18S) 10-1-2008. [Google Scholar]
- 35.Sunde K, Pytte M, Jacobsen D, et al. Implementation of a standardised treatment protocol for post resuscitation care after out-of-hospital cardiac arrest. Resuscitation. 2007 April;73(1):29–39. doi: 10.1016/j.resuscitation.2006.08.016. [DOI] [PubMed] [Google Scholar]