Abstract
Replication activity of 2009 pandemic H1N1 influenza virus in human lung cells was evaluated in this study. Twenty-two surgically removed human lung tissue samples were infected ex vivo with pandemic H1N1, A/California/04/2009, seasonal human H1N1 virus, A/ST/92/2009, or a highly pathogenic H5N1 virus, A/Vietnam/1194/04. Examination of nucleoprotein (NP) protein expression and vRNA replication in infected human lung tissues showed that while CA/04 replication varied between tissue samples, overall, it replicated more efficiently than seasonal H1N1 but less efficiently than H5N1 virus. Double immunostaining for viral antigens and cellular markers indicated that CA/04 replicates in type II alveolar epithelial cells.
Keywords: influenza, pandemic, H1N1, replication, lung infection
The newly emerged swine-origin influenza A virus (2009 pandemic H1N1) has spread globally in the months following the initial April 2009 outbreak in Mexico and California, USA[1, 2], causing the first influenza pandemic of the 21st century, as declared by the World Health Organization (WHO) on June 11, 2009 (http://www.who.int/mediacentre/news/statements/2009/h1n1_pandemic_phase6_20090611/en/). Initial genetic analysis found that the current pandemic strain contains viral segments from swine, human and avian hosts, obtained through multiple reassortment events which cannot be clearly defined at this time[3, 4]. At this stage overall infection severity is mild, according to WHO epidemiological data (http://www.who.int/csr/resources/publications/swineflu/technical_consultation_2009_05_06/en/index.html)[5]. However, 3917 fatal cases have been observed as of 20 September 2009, according to the WHO. The rapid worldwide transmission, combined with the chance of unpredictable adaptation mutations being introduced through continued circulation in humans, the possibility of further reassortment with current seasonal or avian influenza viruses, and the lack of pre-existing immunity to this virus in the general population pose uncertainties regarding the potential severity in humans in the coming pandemic phases. Experience from previous pandemics suggests that severity may change following initial human circulation [6, 7]. Experiments with mice, ferrets, pigs and non-human primates found that pandemic H1N1 virus is able to replicate in the lung tissues of infected animals[8–10], an attribute shared with the highly pathogenic H5N1 viruses but different to the seasonal human influenza viruses, which have only limited replication abilities in lung tissues[11, 12]. The observation of some severe, and even fatal, outcomes in patients without underlying health problems also poses concerns regarding the mechanism of pathogenesis of 2009 pandemic H1N1. The factors that contribute to the discrepancies between animal pathogenicity data and clinical presentation in most human cases are not clear at this stage. Information on pandemic H1N1 virus replication and growth properties in human tissues will be important for understanding the virulence potential of this virus in humans.
This study used surgically-removed lung tissues to evaluate viral gene expression in an ex vivo system and found that the current pandemic strain has a greater potential to replicate in human lung tissues, a property similar to that of highly pathogenic H5N1 viruses.
Results
Twenty-two surgically-removed human lung tissue samples from patients suffering from lung cancer or non-cancerous diseases that were not related to respiratory system infection were obtained from hospitals following an institutional Ethical Review Board-approved protocol. Only non-cancerous lung tissues were used in experiments, as confirmed by histological examination of hematoxylin and eosin stained tissue sections. Three influenza viruses, A/California/04/09 (2009 pandemic H1N1 strain, CA/04), A/Shantou/92/09 (seasonal H1N1 virus, ST/92), and A/Vietnam/1194/04 (H5N1 virus, VNM/1194) were used to infect the tissue samples. All three viruses were propagated and titrated in MDCK cells, and virus stocks stored at −80°C until use. For each tissue sample, virus infections were set up in triplicate. For virus inoculation, 15 lung tissue cubes (approximately 5mm × 4mm × 2mm) were incubated with 106 TCID50 of virus in 500μl inoculums in tissue culture flasks at 37°C in the presence of 5% CO2 for 1 hour. The tissue cubes were then washed three times with serum free F12K nutrient medium before being incubated at 37°C with 5% CO2 for a further 48 hours in 500μl of F12K medium containing 1% BSA and 0.5μg/ml TPCK. For negative controls, tissues were cultured with the same volume of PBS. At 48 hours post infection 5 cubes from each triplicate flask were rinsed with media and pooled for RNA extraction and determination of viral gene replication by real-time PCR quantitative detection of vRNA, while the remaining cubes were fixed and processed for detection of influenza virus nucleoprotein (NP) by immunohistochemical staining. 5–12 sections from each sample were examined for the expression of viral nucleoprotein in lung tissues.
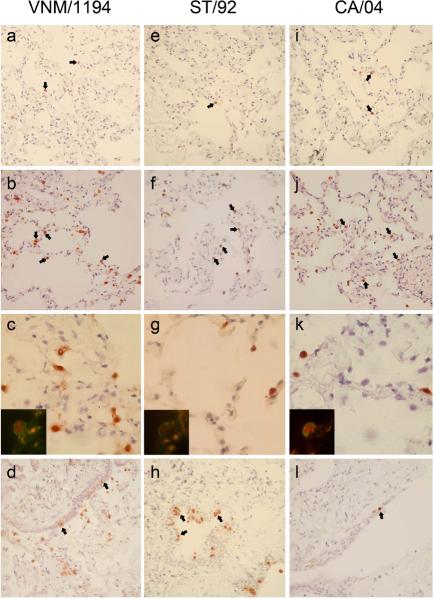
Detection of influenza A nucleoprotein (NP) in ex vivo infected human lung tissues was performed as previously described [13]. In brief, lung tissue sections were deparaffinized, rehydrated and blocked with 1% BSA/PBS followed by overnight incubation with mouse anti-influenza nucleoprotein monoclonal antibody at 4°C [13]. NP positive staining was detected by incubating sections with biotin-conjugated goat anti-mouse IgG (Calbiochem) followed by color development with streptavidin/peroxidase complex reagent. Of the twenty-two) lung tissue samples examined, 15 showed low levels of NP expression with CA/04 virus infection, with 1–5 NP positive cells per tissue section detected in the majority of the tissue cubes (Figure 1 i). In the other 7 cases, significant numbers (more than 5 per 40× field area) of NP positive cells were observed (Figure 1 j). By contrast, no NP positive cells were detected in 7 cases of tissue sections and NP positive cells observed only sporadically in sections from another 13 of the tissue samples infected with seasonal human H1N1 virus, ST/92 (Figure 1 e). Moderate numbers of NP positive cells were observed in sections from only two cases of ST/92-infected lung tissue samples (Figure 1 f). Consistent with previous reports[12], significant numbers of NP positive cells were observed in most of the lung tissues infected with the highly pathogenic H5N1 virus, VNM/1194/04 (Figure 1 b and Table 1).
Figure 1.
Expression of nucleoprotein (NP) in lung tissues infected with influenza viruses ex vivo. Three viruses were used: a–d: VNM/1194; e–h: ST/92; i–l: CA/04. NP positive cells exhibit brown staining in the nucleus and/or cytoplasm, as indicated by arrow heads for some positive cells. Images a, e and i show examples of infected lung tissue sections with few NP positive cells (less than 5 positive cells in one microscope field, 200× amplification), while panels b, f and j show sections containing significant numbers of NP positive cells (more than 15–20 positive cells in one microscope field, 200x amplification). Images c, g and k are at a higher magnification (× 1000) and contain insets portraying double staining of NP and human surfactant apoprotein A (SAP-A) to confirm that infected cells are type II alveolar cells (SAP-A stained green, NP stained red, magnification: × 1000). Panels d, h and l show NP positive terminal bronchiolar epithelial cells observed in infected lung tissues. All images are at × 400 magnification, unless otherwise indicated.
Table 1.
Replication efficiency of influenza viruses in ex vivo infected human lung tissues
| NP vRNA copy number a |
NP positive %b |
|||||
|---|---|---|---|---|---|---|
| Sample ID | CA/04 | ST/92 | VNM/1194 | CA/04 | ST/92 | VNM/1194 |
| 1 | 118.40 | 21.03 | 867.73 | 60 (6/10) | 20 (2/10) | 90 (9/10) |
| 2 | 184.40 | 38.38 | 15038.93 | 89 (8/9) | 20 (2/10) | 100 (9/9) |
| 3 | 21.19 | 11.57 | 200.53 | 37.5 (3/8) | 0 (0/9) | 89 (8/9) |
| 4 | 26.46 | 10.78 | 10390.36 | 11.1 (1/9) | 20 (1/5) | 70 (7/10) |
| 5 | 236.42 | 11.91 | 2731.48 | 87.5 (7/8) | 33.3 (3/9) | 100 (9/9) |
| 6 | 322.93 | 15.98 | 4609.89 | 60 (6/10) | 38.5 (5/13) | 100 (11/11) |
| 7 | 362.03 | 34.86 | 1032.13 | 33.3 (2/6) | 14.3 (1/7) | 14.3 (1/7) |
| 8 | 276.58 | 12.73 | ND | 100 (4/4) | 66.7 (2/3) | ND |
| 9 | 1246.17 | 20.20 | 9116.28 | 57.1 (4/7) | 20 (2/10) | 85.7 (6/7) |
| 10 | 476.69 | 31.46 | 4252.72 | 60 (6/10) | 33.3 (2/6) | 100 (6/6) |
| 11 | 78.23 | 26.84 | 1712.99 | 50 (3/6) | 0 (0/7) | 100 (10/10) |
| 12 | 655.21 | 29.81 | ND | 11.1 (1/9) | 0 (0/6) | ND |
| 13 | 1696.51 | 22.98 | ND | 25 (3/12) | 25 (3/12) | ND |
|
|
|
|||||
| P value | 0.011 | 0.017 | ||||
For each of the three tested viruses, lung tissues were inoculated with 106 TCID50 virus, and incubated at 37°C with 5% CO2 for 1 hour and then incubated for a further 48 hours in serum free F12K Nutrient Mixture (GIBCO, New York, USA) supplemented with 0.5μg/ml TPCK-trypsin. Replication efficiency of influenza viruses in 13 different ex vivo infected human lung tissues was assessed by quantitative RT-PCR and immunostaining to determine vRNA copy number and the frequency of NP positive cells, respectively.
NP gene copy numbers per 1000 copies of beta-actin gene as detected by real time RT-PCR.
number of tissue cubes with NP positive staining (at least one positive cell)/number of tissue cubes examined.
ND: not done.
P value for comparison of vRNA copy number between CA/04 and ST/92 is 0.011, and between CA/04 and VNM/1194 is 0.017.
The cell type in which NP expression is observed in CA/04, VNM/1194 and ST/92 infected tissues morphologically resembles type II alveolar epithelial cells (Figure 1 c, g and k); this was confirmed by double staining with antibodies recognizing human surfactant apoprotein A, the cellular marker for type II alveoli (insets, Figure 1 c, g and k). It was also observed that infection with ST/92 seasonal H1N1 virus resulted in more NP-positive terminal bronchiolar epithelial cells, compared to CA/04 infection (Figure 1 d, h and l). It remains to be investigated if current pandemic H1N1 virus may be still in the process of adaptation to replicate in human upper respiratory tract tissues. In summary, the replication characteristics of pandemic H1N1 in human lung tissues suggest that this virus is more similar to H5N1 virus.
To quantitatively estimate the replication activity of the three viruses in human lung tissues infected ex vivo, levels of viral NP RNA were determined using quantitative real-time RT-PCR. Infected lung tissues were collected at the end point of infection, homogenized in PBS using a pellet pestle system with sterile acid-washed and calcined sea-sand as an abrasive agent, and total RNA extracted using an RNeasy kit (Qiagen). Equal amounts of total RNA were reverse transcribed to cDNA using universal primer and SuperScript II Reverse Transcriptase (Invitrogen) as previously described[14]. For quantification of NP vRNA copy numbers, the SYBR Green based real-time PCR method (Roche) was performed using a protocol described previously[14]. In addition, beta-actin mRNA was quantified for normalization of the total RNA concentration; vRNA copy numbers were estimated on per 1000 copies of beta-actin mRNA basis. Consistent with the NP immunostaining observation, A/VNM/1194/04 H5N1 virus-infected lung tissues exhibited the highest vRNA copy numbers, followed by pandemic H1N1 virus, A/California/04/09, which demonstrated 10–100 fold higher viral copy numbers in majority cases than the seasonal H1N1 virus, A/ST/92/09. Statistical analysis demonstrated that the differences in NP vRNA copy number between pandemic H1N1 and seasonal H1N1 (P = 0.011), and pandemic H1N1 and H5N1 (P = 0.017), are significant. NP immunostaining and quantitative real-time RT-PCR results are summarized in Table 1.
As the rapid global transmission of swine-origin H1N1 virus continues, the trend of its severity has become a major concern for the preparedness and response to the development of this pandemic. The current pandemic virus is able to replicate in lower respiratory tract tissues and cause severe disease in animal models[8, 9], a property resembling that observed for the highly pathogenic H5N1 virus, but not the seasonal influenza virus[11]. The general severity observed in humans, however, tends towards mild, or even asymptomatic infections, although some cases are severe and can be fatal[5]. Host immunity developed through historical association with influenza virus may explain the difference between observations from animal experiments and the clinical presentation of human cases. However, initial serological surveys suggest that there is little pre-existing immunity in the human population, due to the early evolutionary segregation of the human H1N1 virus lineage from the classic swine H1N1 virus which contributed the hemagglutinin gene to the current pandemic virus[15]. Aspects of human cell-mediated immunity may also contribute to this discrepancy, but details remain to be elucidated. The current version of the 2009 pandemic H1N1 virus contains viral genes from different hosts and is believed to still be in the process of becoming further adapted to humans. The wide variability in disease presentation among infected cases and the unpredictability of viral mutations which may arise through continued circulation in humans raises uncertainties regarding the future severity of infections as the pandemic progresses. Understanding the replication abilities of pandemic H1N1 in human lung tissues is therefore extremely important. Using an ex vivo culture system, we found that this virus could replicate in the majority of lung tissues tested. Taken together, the quantitative RT-PCR and NP immunostaining results indicate that CA/04 replication ability in human lung tissue falls somewhere between that of H5N1 and seasonal H1N1 influenza virus (Table 1). However, the degree of CA/04 replication is highly variable; in some cases replication was similar to that of highly pathogenic H5N1 virus but in others resembled that of seasonal H1N1 virus. It is not yet clear whether such differences in replication ability in human lung tissues may relate to the observed variations in clinical outcome. It is possible that the observed differences between individual cases may attributable to variations in host immunity. Although serological studies have revealed that the majority of humans do not have antibodies to 2009 pandemic H1N1 virus, the levels of cellular immunity within the human population are less clear.
As this pandemic virus continues to infect humans and potentially gain more adaptive mutations as it circulates, it is important to study the growth and replication properties of this virus in human cells, as well as host immunity to this virus, to better understand the viral elements and host factors associated with virus replication in humans.
Acknowledgements
This study was supported by the Research Grants Council of the Hong Kong Special Administrative Region (SAR), China (HKU 74888/05M and 7500/06M), the Area of Excellence Scheme of the University Grants Committee (Grant AoE/M-12/06), the National Institutes of Health (NIAID contract HHSN2662007 00005C), the Research Fund for the Control of Infectious Diseases of the Health, Welfare and Food Bureau of the Hong Kong SAR, and the Li Ka Shing Foundation.
Footnotes
Potential conflict of interest: none
References
- 1.Ginsberg M, Hopkins J, Maroufi A, et al. Swine Influenza A (H1N1) infection in two children--Southern California, March-April 2009. MMWR Morb Mortal Wkly Rep. 2009;58:400–2. [PubMed] [Google Scholar]
- 2.Dawood FS, Jain S, Finelli L, et al. Emergence of a novel swine-origin influenza A (H1N1) virus in humans. N Engl J Med. 2009;360:2605–15. doi: 10.1056/NEJMoa0903810. [DOI] [PubMed] [Google Scholar]
- 3.Garten RJ, Davis CT, Russell CA, et al. Antigenic and genetic characteristics of swine-origin 2009 A(H1N1) influenza viruses circulating in humans. Science. 2009;325:197–201. doi: 10.1126/science.1176225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Smith GJ, Vijaykrishna D, Bahl J, et al. Origins and evolutionary genomics of the 2009 swine-origin H1N1 influenza A epidemic. Nature. 2009;459:1122–5. doi: 10.1038/nature08182. [DOI] [PubMed] [Google Scholar]
- 5.Fraser C, Donnelly CA, Cauchemez S, et al. Pandemic potential of a strain of influenza A (H1N1): early findings. Science. 2009;324:1557–61. doi: 10.1126/science.1176062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Taubenberger JK, Hultin JV, Morens DM. Discovery and characterization of the 1918 pandemic influenza virus in historical context. Antivir Ther. 2007;12:581–91. [PMC free article] [PubMed] [Google Scholar]
- 7.Cox NJ, Subbarao K. Global epidemiology of influenza: past and present. Annu Rev Med. 2000;51:407–21. doi: 10.1146/annurev.med.51.1.407. [DOI] [PubMed] [Google Scholar]
- 8.Maines TR, Jayaraman A, Belser JA, et al. Transmission and Pathogenesis of Swine-Origin 2009 A(H1N1) Influenza Viruses in Ferrets and Mice. Science. 2009 doi: 10.1126/science.1177238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Itoh YSK, Kiso M, et al. In vitro and in vivo characterization of new swine-origin H1N1 influenza viruses. Nature. 2009 doi: 10.1038/nature08260. doi:10.1038/nature08260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Munster VJ, de Wit E, van den Brand JM, et al. Pathogenesis and Transmission of Swine-Origin 2009 A(H1N1) Influenza Virus in Ferrets. Science. 2009 doi: 10.1126/science.1177127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gambotto A, Barratt-Boyes SM, de Jong MD, Neumann G, Kawaoka Y. Human infection with highly pathogenic H5N1 influenza virus. Lancet. 2008;371:1464–75. doi: 10.1016/S0140-6736(08)60627-3. [DOI] [PubMed] [Google Scholar]
- 12.Shinya K, Ebina M, Yamada S, Ono M, Kasai N, Kawaoka Y. Avian flu: influenza virus receptors in the human airway. Nature. 2006;440:435–6. doi: 10.1038/440435a. [DOI] [PubMed] [Google Scholar]
- 13.Zhang ZJZ, Huang K, Li KS, Yuen KY, Guan Y, Chen H, Ngl WF. Systemic infection of avian influenza A virus H5N1 subtype in human. Human Pathology. 2008 doi: 10.1016/j.humpath.2008.08.015. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang P, Song W, Mok BW, et al. Nuclear factor 90 negatively regulates influenza virus replication by interacting with viral nucleoprotein. J Virol. 2009;83:7850–61. doi: 10.1128/JVI.00735-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Katz JKH, Veguilla V, et al. Serum cross-reactive antibody response to a novel influenza A (H1N1) virus after vaccination with seasonal influenza vaccine. MMWR Morb Mortal Wkly Rep. 2009;58:521–4. [PubMed] [Google Scholar]