Abstract
Objectives: To discover the perceived size of pool of doctors considered to be underperforming in general practice in the Northern Deanery and to discover whether these perceptions are based on formal assessments.
Design: Postal questionnaire.
Setting: Area covered by the Northern Deanery.
Subjects: Seven health authority directors of primary care, seven secretaries of local medical committees, and 14 chief officers of community health councils.
Results: The response rate was 100% for directors of primary care and secretaries of local medical committees and, after one reminder, 92% for chief officers of community health councils. Numbers of doctors perceived to be underperforming ranged from none to over 15 in different health authority areas. Main areas for concern were communication skills, clinical skills, and management skills. Patients’ representatives were concerned about lack of power of patients and health authorities and doctors’ lack of accountability. Health authorities were concerned about lack of power, identification of underperforming doctors, and doctors’ professional loyalty. Local medical committees were concerned about the problem of identifying underperformance. A number of methods were used for identification, and there was no common method applied.
Conclusions: The number of doctors thought to be underperforming was small. Work still needs to be done on developing tools that can be used in everyday practice to enable doctors to confirm for themselves, their colleagues, and their patients that they are providing an adequate level of care.
Key messages
To quantify the problem of underperforming general practitioners in the Northern Deanery, a postal survey was carried out among representatives of healthcare commissioners, doctors, and patients
A small but not insignificant number of doctors were identified as providing a poor level of performance
Main areas for concern were communication skills, clinical skills, and management skills.
Various methods were used for identifying underperforming doctors, but there was no common method applied
Perceived problems with the present system of dealing with underperforming doctors included identification, lack of power of patients and health authorities, and doctors’ professional loyalty and lack of accountability
Introduction
The General Medical Council’s performance procedures were introduced in the summer of 1997.1 These new procedures give the GMC, for the first time, the power to discipline doctors whose performance is found to be seriously deficient. If doctors are found to be underperforming, the GMC now has the power to suspend the doctors’ registration and make the lifting of this suspension conditional on a period of retraining.2 There are, however, a number of uncertainties around these new procedures, not least the scale of the problem and the type of retraining that will be required.
In an effort to quantify the size of the problem in general practice in the Northern Deanery and identify the areas in which training may be required in the future, I carried out a postal survey of interested parties.
Methods
In early 1988 I conducted a postal survey of the three groups perceived to be interested in general practice in the Northern Deanery: NHS commissioners, represented by the seven directors of primary care at the relevant health authorities; general practitioners, represented by the seven secretaries of local medical committees; and patients, represented by the 14 chief officers of community health councils. The response rate was excellent, with 100% responses from the directors of primary care and the secretaries of local medical committees and 11/14 responses from the secretaries of community health councils to the first request for information. The response from the community health councils rose to 13/14 after one reminder.
I used standard development methods for the questionnaire, including piloting to ensure clarity, question structure, and time to complete.3 The first series of questions related to whether responders had referred or were planning to refer general practitioners to the GMC under the procedures for seriously deficient performance. The respondents were also asked to identify the areas in which these doctors were perceived to be underperforming. The development of this part of the questionnaire was based on views obtained during unstructured interviews with a sample population of general practitioners and health authority directors of primary care. The facility to add further areas of concern was allowed, as was further free comment.
Respondents were then asked to gauge how many doctors in their area needed help with their performance but not at such a level as to require referral; they were asked to indicate the size of the population of underperforming doctors by circling a range. A further question asked them to identify areas that they perceived to be problematic in this population of doctors; they were able to identify more than one area.
Respondents were asked what methods, either formal or informal, were used to identify underperforming doctors. In the final question respondents were asked to identify up to three deficiencies in the current systems relating to the identification and management of poorly performing doctors, and these were analysed with standard qualitative analysis techniques.4
Results
Referral of doctors to the GMC
The seven health authorities had already referred five doctors under the new GMC procedures and were also considering referral in five further cases. The community health councils had referred six doctors and were considering the case of five others. The local medical committees had not referred any doctors but were considering the cases of two. It is impossible to say from the data if there was overlap of referral between organisations, but the numbers involved, while small, are not insignificant. The total number of general practitioners in the Northern Deanery is 1633.5
Table 1 shows the respondents’ areas of concern relating to these underperforming doctors. Respondents were allowed to identify more than one area of concern. Clinical skills and communication skills were common areas of concern, and practice management was also often felt to be an area of deficiency. Health authorities, but less so community health councils, identified poor record keeping as an area of concern.
Table 1.
Respondents’ areas of concern in relation to doctors referred, or being considered for referral, to GMC for deficient performance. Values are number of responses
| Respondent
|
|||
|---|---|---|---|
| Areas of concern | Health authority | Local medical committee | Community health council |
| Clinical skills | 3 | 1 | 6 |
| Communication skills | 4 | 0 | 6 |
| Records | 4 | 1 | 2 |
| Concerns about prescribing | 1 | 0 | 0 |
| Concerns about referral | 1 | 0 | 0 |
| Management | 3 | 1 | 4 |
| Other | 0 | 0 | 1 (“poor doctor”) |
Doctors needing help with their performance
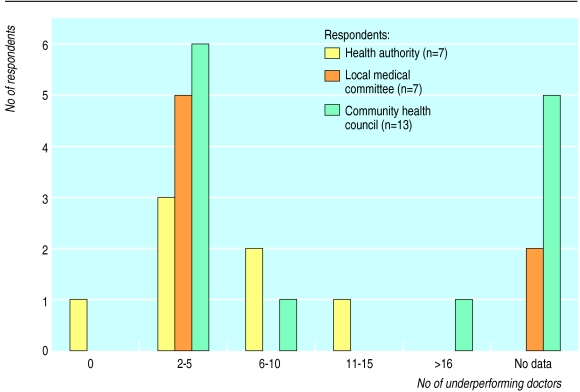
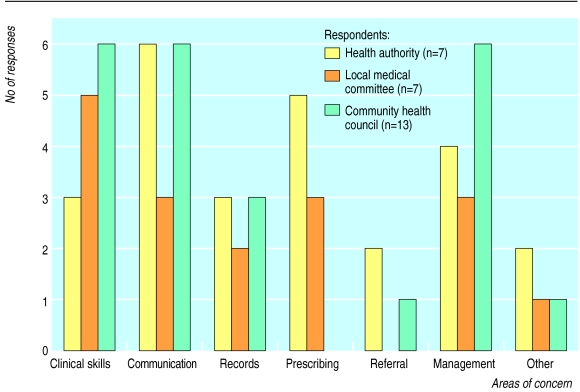
Figure 1 shows the respondents’ estimates of the number of doctors who were in need of help with their performance but not at such a level as to require referral, and figure 2 shows the respondents’ areas of concern about these underperforming doctors. The areas of concern identified were similar to those listed for the doctors who had been referred to the GMC or considered for referral. The health authorities and local medical committees were also concerned about the doctors’ prescribing, and to a lesser degree health authorities about referrals. Concerns about management (which was not defined in the questionnaire) were common, especially among the patients’ representatives.
Figure 1.
Respondents’ estimates of the number of local general practitioners in need of help for underperformance
Figure 2.
Respondents’ perceptions of areas of concern in the population of underperforming doctors
Methods used to identify underperforming doctors
Health authorities listed many different formal mechanisms for identifying underperforming doctors, including targets, practice inspections, input from the pharmaceutical advisor, and a number of quality systems such as King’s Fund organisational audit,6 the Royal College of General Practitioners fellowship by assessment,7 and a local health authority practice accreditation scheme. Two health authorities also used the complaints mechanisms. Of the 13 community health councils that responded, six used the complaints mechanisms to identify underperforming doctors, and this was the only formal mechanism used by the councils. The local medical committees had no formal mechanisms other than one being involved with the local practice accreditation scheme.
Sources of help for underperforming doctors
The questionnaire offered respondents a choice of organisations that might provide help to underperforming doctors, and table 2 shows their responses. They were able to identify more than one source of help. One community health council thought that the GMC itself should be a source of help to such doctors.
Table 2.
Respondents’ choices of organisations that might provide help to underperforming doctors
| Respondent
|
|||
|---|---|---|---|
| Source of help | Health authority | Local medical committee | Community health council |
| Health authority | 4 | 6 | 11 |
| Local medical committee | 5 | 8 | 10 |
| Royal College of General Practitioners | 4 | 4 | 8 |
| University | 4 | 3 | 5 |
| General practitioner tutor | 5 | 5 | 8 |
| Others | Deanery (1), mentors (1) | 0 | Community health council (1), GMC (1) |
Perceived deficiencies in present system
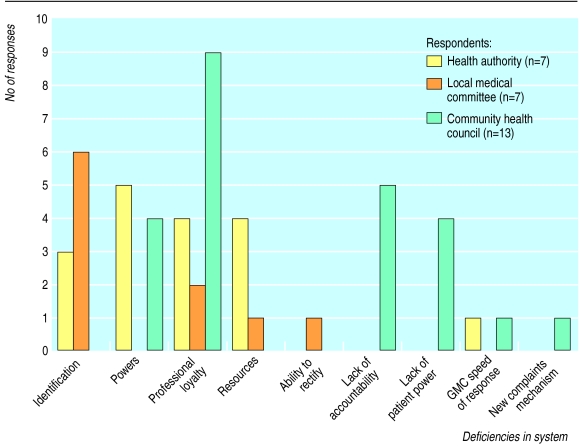
Figure 3 lists the deficiencies in the present system that respondents identified. The health authorities felt limited by their lack of power, had problems identifying underperforming doctors, and were limited by doctors’ loyalty to colleagues. They also identified problems with resources, including time. The local medical committees saw the main problem as identification of underperforming doctors but also noted doctor loyalty as a problem. The community health councils, however, did not see identification as a problem but saw the major problems to be doctors’ professional loyalty, their lack of accountability to the health service, and the lack of patients’ and health authorities’ power in these situations.
Figure 3.
Respondents’ choices of deficiencies in current system of dealing with underperforming doctors
Discussion
The purpose of the performance procedures is to protect the public from doctors providing seriously deficient care, and the profession has a responsibility to help with this. It is also important to recognise that some doctors may need help to enable them to avoid being drawn into these procedures. It is unclear whether mechanisms exist at present to identify these doctors. Preventive help rather than punitive action should surely be the aim in the long term.
The results of this small survey seem to point to a small but significant number of doctors being referred under the performance procedures and a larger pool of doctors who may fall into this system if action is not taken to help them. The areas of concern cited were, however, only perceptions. There were few, if any, formal mechanisms being used for the routine assessment of performance of doctors in practice, and the tools used would seem to be crude measures of performance. It seems unlikely that poorly performing doctors would involve themselves in activities such as the King’s Fund organisational audit or the Royal College of General Practitioners fellowship by assessment, both of which require a high level of commitment. Formal targets or practice inspections will provide, at best, crude measures of performance. Complaints will identify poor performance, but perhaps too late in a doctor’s career.
A variety of methods have been put forward to assess clinical competence for the purpose of re-certification.8 Southgate and Jolly, from the United Kingdom, recommend information sources such as practice logs, patterns of referral and prescribing, and direct observation, whereas Hays, from Australia, proposes practice audit, external audit, standardised patients, and direct observation by trained assessors.8 In our survey the health authorities were using some of the external audit data that they held, such as targets and prescribing. There does not seem, as yet, to be any mechanism to assess and use data relating to day to day practice. The NHS Executive have recently proposed a national framework for assessing performance.9 This does not, however, seem real or relevant to everyday practice. Is an admission rate for severe ear, nose, and throat infection a true indicator of management of acute care in primary care? It may well be that developments such as the Royal College of General Practitioners clinical practice evaluation programme (CPEP)10 will help in this area.
Our survey also seemed to identify deficiencies in the NHS systems for bringing about change in underperforming doctors. The medical profession clearly has a major responsibility in overcoming its natural reticence in “blowing the whistle” on seriously underperforming colleagues. It also needs to recognise its responsibility to help doctors whose performance is slipping to rectify their problems before these threaten their ability to practice to an acceptable level. The GMC and the medical profession must either reassure the public that present systems are able to protect them or else review the existing systems in the light of experience and make changes to increase the public’s confidence.
See Editor’s choice
Footnotes
Funding: None.
Conflict of interest: None.
References
- 1.Medical (Professional Performance) Act 1995. London: Stationery Office; 1997. (Commencement No 3.) [Google Scholar]
- 2.General Medical Council. The new performance procedures. London: GMC; 1997. [Google Scholar]
- 3.Fink A, Kosecoff J. How to conduct surveys. Newbury Park: Sage; 1985. [Google Scholar]
- 4.Britten N, Jones R, Murphy E, Stacy R. Qualitative research methods in general practice and primary care. Fam Pract. 1995;12:104–114. doi: 10.1093/fampra/12.1.104. [DOI] [PubMed] [Google Scholar]
- 5.Department of Health; NHS Executive. GMS statistics England and Wales. Leeds: NHSE; 1997. [Google Scholar]
- 6.King’s Fund organisational audit primary care standards. London: King’s Fund; 1993. [Google Scholar]
- 7.Royal College of General Practitioners. Fellowship by assessment. London: RCGP; 1997. (Occasional Paper No 50.) [Google Scholar]
- 8.Newble D, Jolly B, Wakeford R, editors. The certification and re-certification of doctors. Issues in the assessment of clinical competence. Cambridge: Cambridge University Press; 1994. p. 184. , 192-4. [Google Scholar]
- 9.The new NHS modern and dependable: a national framework for assessing performance. Leeds: NHS Executive; 1998. [Google Scholar]
- 10.Royal College of General Practitioners. RCGP clinical practice evaluation programme (CPEP). London: RCGP; 1997. [Google Scholar]