Clonal hematopoiesis is a key feature of myeloproliferative neoplasms (MPN), a hematopoietic stem cell disorder comprising three disease entities: polycythemia vera (PV), essential thrombocytosis (ET) and primary myelofibrosis (PMF). Although the clinical characteristics of these three diseases are quite distinct, they do share genetic mutations that drive clonal myeloproliferation, which is their common defining feature. Continual technological advances have led to the identification of increasing numbers of genetic defects in MPN patients. In this issue of Haematologica, Stegelmann et al.1 present their results from a genome-wide single-nucleotide polymorphism (SNP) profiling study in a large cohort of MPN patients that significantly furthers our understanding of the molecular causes and diversity of MPN.
Genetic defects driving clonality in myeloproliferative neoplasms
The identification of activating mutations in the gene coding for the tyrosine kinase JAK2 (JAK2-V617F and JAK2 exon 12 mutations) in almost all PV patients and in a large percentage of ET and PMF patients,2–7 led to a series of follow-up studies to investigate their functional consequences.8 Nevertheless, how a single mutation can contribute to the pathogenesis of three phenotypically distinct disease entities is still largely unclear. One study, using a JAK2-V617F transgenic mouse model, suggested that the disease phenotype could be determined by the ratio of mutant JAK2 to wild-type protein.9 However, there is growing evidence for a more complex mechanism of MPN phenotype initiation. Observations of strain-specific differences in JAK2-V617F-associated disease phenotypes between Balb/c and C57Bl/6 mice suggest an involvement of germ line features in the resultant phenotype.8 However, besides JAK2 mutations and other oncogenic events targeting the JAK-STAT pathway (such as mutations in the MPL gene, coding for the thrombopoietin receptor and truncations of the erythropoietin receptor),8 there are still many uncharacterized somatic cytogenetic lesions present within the MPN clone, harboring a series of candidates for both the induction of clonal expansion and the MPN phenotype decision.
TET2 and CBL mutations in myeloproliferative neoplasms
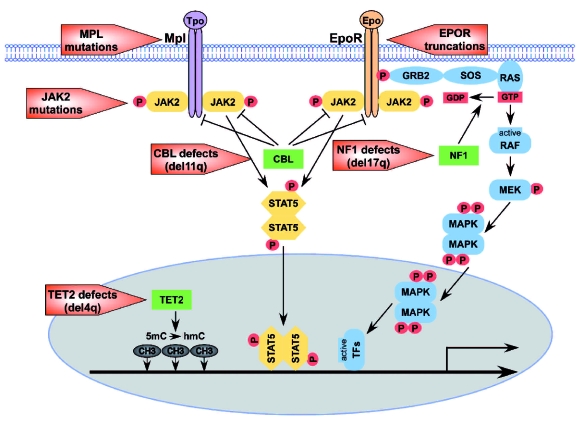
Classical cytogenetic methods made it possible to detect large genetic aberrations in patients with specific diseases which revealed cytogenetic lesions usually containing a large number of genes. Recurrent defects found in MPN, such as the deletions on chromosome 20q (del20q) and 13q (del13q), are thought to harbor important tumor suppressors, the majority of which must still be identified.8, 10 The development of microarray based methods has allowed the high resolution screening of a large number of patients for the detection of somatic chromosomal aberrations. Detection of loss of heterozygosity (LOH) by microarray genotyping has become a valuable tool in cancer biology. Additional probes on the array for measuring the abundance of gene copies can discriminate between a deletion or a copy number neutral acquired uniparental disomy (UPD), underlying the LOH. Recently, microarray based mapping of the recurrent UPDs and deletions on chromosomes 4q and 11q led to the discovery of TET2 and CBL mutations being involved in the pathogenesis of various myeloid malignancies.11,12 In MPN, TET2 is mutated in about 13% of all cases with the highest frequency in PMF (17%), followed by PV (16%) and ET (5%).11, 13 Stem cells carrying TET2 mutations have been shown to exhibit a proliferative advantage in a murine competitive repopulation model.14 Although the mechanism of action of TET2 is not known, it may involve epigenetic gene regulation, as another Ten-Eleven-Translocation family member, TET1 has been shown to catalyze the conversion of 5-methylcytosine in DNA to 5-hydroxymethylcytosine.15 In contrast to TET2, the function of the E3 ubiquitin ligase CBL in hematopoiesis seems to be clearer, as CBL is involved in the ubiquitylation of factors important for tyrosine kinase function, specifically influencing STAT5 phosphorylation.16 Tyrosine kinase signaling is tightly regulated not only by dephosphorylation, but also by degradation of receptors and signaling molecules. Interaction studies revealed a role of CBL in ubiquitylation of the cytokine receptors Epo-R and c-Kit, various tyrosine kinases (e.g. Jak2, Tyk2, Abl) and adapter proteins important for cytokine signaling such as Grb2.17 CBL shows clear properties of a classical tumor suppressor, such as increased proliferative response due to loss of function in both the homo- and heterozygous state. Nevertheless, CBL mutants were shown to have gain-of-function properties in the absence of wild-type CBL, augmenting the cytokine hypersensitivity of the loss-of-function phenotype to a broader spectrum of cytokines.16 Therefore, CBL was proposed to be a tumor suppressor with features of an oncogene, regulating the degradation of pleiotropic factors (Figure 1).
Figure 1.
Mechanisms and pathways targeted by mutations in MPN. Schematic diagram of pathways involved in MPN pathogenesis. Red boxes summarize germ line and somatic mutations in MPN and MPN-like phenotypes. Clonal advantage based on cytokine hypersensitivity can be triggered by genetic defects directly targeting cytokine receptors, such as MPL mutations and EPO-R C-terminal truncations, as well as mutations affecting elements of downstream signaling cascades. Defects identified so far in MPN predominantly activate the JAK-STAT and the mitogen-activated protein kinase (MAPK) pathways. Gain-of-function mutations in JAK2 (JAK2-V617F and JAK2 exon 12 mutations) directly affect signal transduction, whereas loss of function mutations in CBL and NF1 intervene indirectly. The ubiquitin ligase CBL regulates the degradation of surface receptors and JAK2. NF1, a GTPase activating protein decreases signal potential of Ras, an important protooncogene in the MAPK pathway. Besides defects in cytokine signal transduction, mutations potentially directly affecting gene transcription have been found in TET2. TET2 might be involved in epigenetic transcriptional regulation by enzymatically catalyzing the conversion of 5-methylcytosine to 5-hydroxymethylcytosine, as shown for another TET family member TET1.
Inactivation of NF1 in myeloproliferative neoplasms
In this issue of Haematologica, Stegelmann et al.1 present the results of a screen for somatic genetic lesions in a cohort of 151 MPN patients using 250K SNP arrays. Genotyping 250,000 SNPs distributed throughout the genome gives sufficient resolution for identifying even single gene defects. Applying an unbiased approach on patient selection, Stegelmann et al.1 could detect copy number altering genetic defects (deletions, gains) at frequencies spanning from 15% in PV to 62% in post-PV myelofibrosis (MF). The frequencies of copy number neutral UPDs in their cohort were similar (14% in PV up to 62% in post-PV MF). Beyond the most frequent aberrations, the previously described and well known 9pUPD and del20q aberrations were detected. Most of the genetic lesions identified spanned large regions containing several genes. In 2 patients, microdeletions on 17q could be detected, exclusively targeting the NF1 gene. Sequencing of the remaining NF1 allele revealed a mutation in one of the 2 cases, suggesting that clonal expansion can be induced by haploin-sufficiency of NF1 as well as full inactivation. NF1 mutations are also found in Von Recklinghausen’s disease (also known as Neurofibromatosis type 1), where both germ line and spontaneous mutations cause various tumors, primarily in the peripheral nerve system.18 The NF1 gene codes for neurofibromin, a GTPase activating protein that inactivates the small GTPase Ras by accelerating Ras-associated hydrolysis of guanosine triphosphate (GTP) into guanosine diphosphate (GDP) and phosphate (Figure 1).19 Loss of NF1 causes Ras to remain in its active state (bound to GTP) stimulating induction-independent cell proliferation.19 Ras is an important signaling molecule within the mitogen-activated protein kinase (MAPK) pathway, a pathway triggered by various cytokines. Of specific relevance to hematologic diseases is the involvement of Ras in granulocyte-macrophage colony-stimulating factor (GM-CSF) signaling, which promotes survival of myeloid cells, and an NF1 knockout mouse model has been shown to develop an MPN phenotype.20 From the 2 cases reported by Stegelmann et al.,1 one wild-type, the other homozygous for JAK2-V617F, NF1 loss is likely to give additional growth potential even to cells homozygous for JAK2-V617F, but it is acquired independently from the JAK2 mutational status. Furthermore, both patients progressed to secondary myelofibrosis, one from ET and the other from PV, whereas the latter finally transformed to acute myeloid leukemia. Whether NF1 plays a role in this transformation needs further investigation, although the occurrence of NF1 mutations in various childhood (up to 15% in juvenile myelomonocytic leukemia (JMML)) and adult leukemias is suggests that it does.21
Relationship between the different genetic defects in myeloproliferative neoplasms
Due to the rapid evolvement of microarray and next generation sequencing technology, abundant information on defects involved in MPN pathogenesis will soon be available. In principle, it will then be possible to draw a map of genetic aberrations for each patient. Important information necessary for drawing such a map is the acquisition order and clonal relationship of genetic lesions. This can be determined by looking at mutational burdens in isolated cell types, or by genotyping single colony forming hematopoietic progenitor cells for the known defects.8, 22–25 Currently, only a few conclusions can be drawn on the relatedness and acquisition of the genetic defects in MPN. First, the oncogenic mutations in JAK2 and MPL have not been observed combined in a single clone. Second, the most frequent cytogenetic aberrations, del20q and del13q have been observed in the same patient, but only in different clones. 22–25 Concerning the order of acquisition of the defects identified to date, there is increasing evidence that there is no predefined acquisition order of these lesions for MPN.8 For the recently discovered mutations in CBL, TET2 and NF1, TET2 mutations tend to be acquired rather early in the disease course, whereas CBL and NF1 might be late events, eventually being involved in leukemic transformation. TET2 has been observed to be acquired both before and after JAK2-V617F,11,26,27 whereas CBL has been observed preferentially in the absence of the classical oncogenic mutations or succeeding JAK2-V617F,16,28 similar to the data on NF1 provided by Stegelmann et al.1 Furthermore, there is some evidence that both CBL and NF1 mutations are associated with leukemic transformation, however this needs to be confirmed in larger studies. Specific mutational analysis of progenitor colonies on a larger scale is required to place TET2, CBL and NF1 into the clonal hierarchy of the progenitor pool to determine whether they integrate into the model of random mutation acquisition.
Evidence for a “mutator” phenotype in myeloproliferative neoplasms
The large amount of cytogenetic aberrations detected in MPN clearly points to the existence of a “mutator” phenotype in MPN pathogenesis. Chromosomal instability might be triggered by known defects, or by as yet unidentified mutations. These unknown somatic or germ line mutator defects could affect non-protein coding sequences or epigenetic factors. Evidence supporting an inherited predisposition to acquire specific mutations was recently provided by the identification of a JAK2 gene haplotype that confers susceptibility to JAK2-V617F and JAK2 exon 12 mutation positive MPN.22,29–31 Since this “GGCC” haplo-type (also known as 46/1) has a relatively low penetrance, additional somatic and germ line mutator defects are expected to be at work in MPN.
Perspective
The recent findings of new somatic mutations and the first insights into elements predisposing for MPN represent big steps in the field, but render the picture of the underlying cause of MPN even more complex. More mutations are predicted to be identified as the resolution of cytogenetic analysis increases, as well as by broad application of next generation sequencing. Additionally, increased feature density on microarrays succeeding the 250K technology has opened up the possibility for whole genome association studies, with the potential to reveal even more important genetic loci in MPN pathogenesis. The construction of a comprehensive network of all the disease-contributing defects is one of the predominant but now seemingly realistic future challenges in MPN genetics.
Footnotes
No potential conflicts of interests relevant to this article were reported.
The work was supported by grants from the Austrian Science Fund (FWF) and the MPD Foundation.
References
- 1.Stegelmann F, Bullinger L, Griesshammer M, Holzmann K, Habdank M, Kuhn S, et al. High-resolution single-nucleotide polymorphism array-profiling in myeloproliferative neoplasms identifies novel genomic aberrations. Haematologica. 2010;95:666–9. doi: 10.3324/haematol.2009.013623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.James C, Ugo V, Le Couedic JP, Staerk J, Delhommeau F, Lacout C, et al. A unique clonal JAK2 mutation leading to constitutive signalling causes polycythaemia vera. Nature. 2005;434(7037):1144–8. doi: 10.1038/nature03546. [DOI] [PubMed] [Google Scholar]
- 3.Kralovics R, Passamonti F, Buser A, Teo S, Tiedt R, Passweg J, et al. A gain-of-function mutation of JAK2 in myeloproliferative disorders. N Engl J Med. 2005;352(17):1779–90. doi: 10.1056/NEJMoa051113. [DOI] [PubMed] [Google Scholar]
- 4.Levine R, Wadleigh M, Cools J, Ebert B, Wernig G, Huntly B, et al. Activating mutation in the tyrosine kinase JAK2 in polycythemia vera, essential thrombocythemia, and myeloid metaplasia with myelofibrosis. Cancer Cell. 2005;7(4):387–97. doi: 10.1016/j.ccr.2005.03.023. [DOI] [PubMed] [Google Scholar]
- 5.Baxter EJ, Scott LM, Campbell PJ, East C, Fourouclas N, Swanton S, et al. Acquired mutation of the tyrosine kinase JAK2 in human myeloproliferative disorders. Lancet. 2005;365(9464):1054–61. doi: 10.1016/S0140-6736(05)71142-9. [DOI] [PubMed] [Google Scholar]
- 6.Scott LM, Tong W, Levine RL, Scott MA, Beer PA, Stratton MR, et al. JAK2 exon 12 mutations in polycythemia vera and idiopathic erythrocytosis. N Engl J Med. 2007;356(5):459–68. doi: 10.1056/NEJMoa065202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pietra D, Li S, Brisci A, Passamonti F, Rumi E, Theocharides A, et al. Somatic mutations of JAK2 exon 12 in patients with JAK2 (V617F)-negative myeloproliferative disorders. Blood. 2008;111(3):1686–9. doi: 10.1182/blood-2007-07-101576. [DOI] [PubMed] [Google Scholar]
- 8.Kralovics R. Genetic complexity of myeloproliferative neoplasms. Leukemia. 2008;22(10):1841–8. doi: 10.1038/leu.2008.233. [DOI] [PubMed] [Google Scholar]
- 9.Tiedt R, Hao-Shen H, Sobas MA, Looser R, Dirnhofer S, Schwaller J, et al. Ratio of mutant JAK2-V617F to wild-type Jak2 determines the MPD phenotypes in transgenic mice. Blood. 2008;111(8):3931–40. doi: 10.1182/blood-2007-08-107748. [DOI] [PubMed] [Google Scholar]
- 10.Kralovics R, Skoda RC. Molecular pathogenesis of Philadelphia chromosome negative myeloproliferative disorders. Blood Rev. 2005;19(1):1–13. doi: 10.1016/j.blre.2004.02.002. [DOI] [PubMed] [Google Scholar]
- 11.Delhommeau F, Dupont S, Della Valle V, James C, Trannoy S, Masse A, et al. Mutation in TET2 in myeloid cancers. N Engl J Med. 2009;360(22):2289–301. doi: 10.1056/NEJMoa0810069. [DOI] [PubMed] [Google Scholar]
- 12.Grand F, Hidalgo-Curtis C, Ernst T, Zoi K, Zoi C, McGuire C, et al. Frequent CBL mutations associated with 11q acquired uniparental disomy in myeloproliferative neoplasms. Blood. 2009;113(24):6182–92. doi: 10.1182/blood-2008-12-194548. [DOI] [PubMed] [Google Scholar]
- 13.Tefferi A, Pardanani A, Lim KH, Abdel-Wahab O, Lasho TL, Patel J, et al. TET2 mutations and their clinical correlates in polycythemia vera, essential thrombocythemia and myelofibrosis. Leukemia. 2009;23(5):905–11. doi: 10.1038/leu.2009.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Delhommeau F, Dupont S, Della Valle V, James C, Trannoy S, Massé A, et al. Mutation in TET2 in myeloid cancers. N Engl J Med. 2009;360(22):2289–301. doi: 10.1056/NEJMoa0810069. [DOI] [PubMed] [Google Scholar]
- 15.Tahiliani M, Koh KP, Shen Y, Pastor WA, Bandukwala H, Brudno Y, et al. Conversion of 5-methylcytosine to 5-hydroxymethylcytosine in mammalian DNA by MLL partner TET1. Science. 2009;324(5929):930–5. doi: 10.1126/science.1170116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sanada M, Suzuki T, Shih LY, Otsu M, Kato M, Yamazaki S, et al. Gain-of-function of mutated C-CBL tumour suppressor in myeloid neoplasms. Nature. 2009;460(7257):904–8. doi: 10.1038/nature08240. [DOI] [PubMed] [Google Scholar]
- 17.Schmidt MH, Dikic I. The Cbl interactome and its functions. Nat Rev Mol Cell Biol. 2005;6(12):907–18. doi: 10.1038/nrm1762. [DOI] [PubMed] [Google Scholar]
- 18.Reynolds RM, Browning GG, Nawroz I, Campbell IW. Von Recklinghausen's neurofibromatosis: neurofibromatosis type 1. Lancet. 2003;361(9368):1552–4. doi: 10.1016/s0140-6736(03)13166-2. [DOI] [PubMed] [Google Scholar]
- 19.Bollag G, Clapp DW, Shih S, Adler F, Zhang YY, Thompson P, et al. Loss of NF1 results in activation of the Ras signaling pathway and leads to aberrant growth in haematopoietic cells. Nat Genet. 1996;12(2):144–8. doi: 10.1038/ng0296-144. [DOI] [PubMed] [Google Scholar]
- 20.Birnbaum RA, O'Marcaigh A, Wardak Z, Zhang YY, Dranoff G, Jacks T, et al. Nf1 and Gmcsf interact in myeloid leukemogenesis. Mol Cell. 2000;5(1):189–95. doi: 10.1016/s1097-2765(00)80415-3. [DOI] [PubMed] [Google Scholar]
- 21.Balgobind BV, Van Vlierberghe P, van den Ouweland AM, Beverloo HB, Terlouw-Kromosoeto JN, van Wering ER, et al. Leukemia-associated NF1 inactivation in patients with pediatric T-ALL and AML lacking evidence for neurofibromatosis. Blood. 2008;111(8):4322–8. doi: 10.1182/blood-2007-06-095075. [DOI] [PubMed] [Google Scholar]
- 22.Olcaydu D, Harutyunyan A, Jager R, Berg T, Gisslinger B, Pabinger I, et al. A common JAK2 haplotype confers susceptibility to myeloproliferative neoplasms. Nat Genet. 2009;41(4):450–4. doi: 10.1038/ng.341. [DOI] [PubMed] [Google Scholar]
- 23.Schaub FX, Jager R, Looser R, Hao-Shen H, Hermouet S, Girodon F, et al. Clonal analysis of deletions on chromosome 20q and JAK2-V617F in MPD suggests that del20q acts independently and is not one of the predisposing mutations for JAK2-V617F. Blood. 2009;113(9):2022–7. doi: 10.1182/blood-2008-07-167056. [DOI] [PubMed] [Google Scholar]
- 24.Buxhofer-Ausch V, Gisslinger H, Berg T, Gisslinger B, Kralovics R. Acquired resistance to interferon alpha therapy associated with homozygous MPL-W515L mutation and chromosome 20q deletion in primary myelofibrosis. Eur J Haematol. 2009;82(2):161–3. doi: 10.1111/j.1600-0609.2008.01183.x. [DOI] [PubMed] [Google Scholar]
- 25.Beer PA, Jones AV, Bench AJ, Goday-Fernandez A, Boyd EM, Vaghela KJ, et al. Clonal diversity in the myeloproliferative neoplasms: independent origins of genetically distinct clones. Br J Haematol. 2009;144(6):904–8. doi: 10.1111/j.1365-2141.2008.07560.x. [DOI] [PubMed] [Google Scholar]
- 26.Saint-Martin C, Leroy G, Delhommeau F, Panelatti G, Dupont S, James C, et al. Analysis of the ten-eleven translocation 2 (TET2) gene in familial myeloproliferative neoplasms. Blood. 2009;114(8):1628–32. doi: 10.1182/blood-2009-01-197525. [DOI] [PubMed] [Google Scholar]
- 27.Beer PA, Delhommeau F, Lecouedic JP, Dawson MA, Chen E, Bareford D, et al. Two routes to leukemic transformation following a JAK2 mutation-positive myeloproliferative neoplasm. Blood. 2009 doi: 10.1182/blood-2009-08-236596. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 28.Grand FH, Hidalgo-Curtis CE, Ernst T, Zoi K, Zoi C, McGuire C, et al. Frequent CBL mutations associated with 11q acquired uniparental disomy in myeloproliferative neoplasms. Blood. 2009;113(24):6182–92. doi: 10.1182/blood-2008-12-194548. [DOI] [PubMed] [Google Scholar]
- 29.Jones AV, Chase A, Silver RT, Oscier D, Zoi K, Wang YL, et al. JAK2 haplotype is a major risk factor for the development of myeloproliferative neoplasms. Nat Genet. 2009;41(4):446–9. doi: 10.1038/ng.334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kilpivaara O, Mukherjee S, Schram AM, Wadleigh M, Mullally A, Ebert BL, et al. A germline JAK2 SNP is associated with predisposition to the development of JAK2(V617F)-positive myeloproliferative neoplasms. Nat Genet. 2009;41(4):455–9. doi: 10.1038/ng.342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Olcaydu D, Skoda RC, Looser R, Li S, Cazzola M, Pietra D, et al. The 'GGCC' haplotype of JAK2 confers susceptibility to JAK2 exon 12 mutation-positive polycythemia vera. Leukemia. 2009;23(10):1924–6. doi: 10.1038/leu.2009.110. [DOI] [PubMed] [Google Scholar]