Abstract
This study aimed to determine the role of Bartonella as an endocarditis agent in cattle. Bartonella bovis was identified by PCR, gene sequences analysis, and specific internal transcribed spacer amplicon product size in 2 bovine endocarditis cases with high antibody titers, which demonstrates that B. bovis is a pathogen for cattle.
Keywords: Bartonella bovis, cattle, endocarditis, dispatch
Bacteria-induced vegetative valvular endocarditis is one of the main cardiac disorders in adult cattle (1). The prevalence of endocarditis may reach 5.2 cases per 10,000 cows (2), but the disease is often misdiagnosed and only discovered during the slaughtering process or at necropsy. Bacterial endocarditis is often linked to a primary source of infection and the presence of other infectious lesions, such as mastitis, metritis, arthritis, or liver abscesses. The most frequent pathogens isolated from cardiac valves or the bloodstream of cows with endocarditis are Arcanobacterium pyogenes (up to 90% of the strains), Streptococcus sp., and numerous Enterobacteriaceae (2).
The development of molecular techniques (PCR) led to the identification of many noncultivable or poorly cultivable bacteria as agents of human endocarditis, such as Coxiella burnetii, different Bartonella species, or Tropheryma whipplei (3,4). In dogs, Bartonella species cause 8% of all bacterial endocarditis and up to 19% of noncultivable bacterial endocarditis (5). In cats, bacterial endocarditis is infrequent, but a fatal case caused by B. henselae was recently reported (6). Bartonellae can therefore be considered as potential agents of endocarditis even in their own reservoir species. Cattle host B. bovis, which has also been isolated from cats (7) and was recently suggested as the etiologic agent in a human case of bartonellosis (8). However, the role of Bartonella species in bovine endocarditis has never been explored. Therefore, our objective was to determine the putative role of Bartonella sp. as an agent of endocarditis in cattle.
The Study
Twenty-two cases of bovine endocarditis were diagnosed in adult cows (ages 5–15 years, mean 7.4 years) at the School of Veterinary Medicine, Toulouse, France, from September 2004 through June 2006. Eighteen cows were hospitalized for poor condition, anorexia, weight loss, wasting syndrome, and abnormal cardiac auscultation. Endocarditis was diagnosed at physical examination. Lesions of the cardiac valves were confirmed at necropsy for all 18 animals. Four additional cases of endocarditis were identified at necropsy after an apparent sudden death. Most of the damaged valves of these 22 animals had large, cauliflower-like lesions.
For each cow, fragments of the vegetative valve and of 1 normal-appearing valve were collected. DNA extraction from each valve sample was performed by using Nucleospin Tissue extraction kit (Macherey-Nagel, Hoerdt, France) according to the supplier’s recommendation.
PCR amplification was performed on all normal-appearing and vegetative valves for the hypervariable V3 zone of the eubacterial 16S rRNA detection, and the 3′ end of citrate synthase gene (gltA) Bartonella sp. DNA detection. Additional PCR amplification was performed on gltA-positive valves for the following Bartonella-specific genes or genomic region: rpoB, ribC, groEL, internal transcribed spacer (ITS) of 16S–23S rRNA (9,10). Amplification products, including those for the 16S rRNA, were subsequently sequenced.
Serology by indirect fluorescent antibody assay (IFA) was performed as reported elsewhere (11) on the supernatant extracted from a cardiac blood clot from each cow. Vero cells infected with the type strain of B. bovis (CIP 106692T), B. chomelii (CIP 107869 T), and B. schoenbuchensis (NCTC 13165T), respectively, were used as antigens.
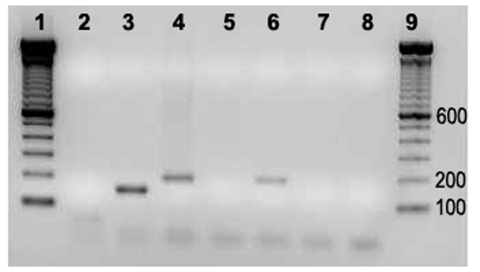
The 22 vegetative valves included 8 pulmonary valves, 7 tricuspid valves, 6 aortic valves, and 1 mitral valve. The only vegetative mitral valve and 1 of the 6 aortic vegetative valves showed positive results for Bartonella-specific gltA gene amplification. For both cows, the normal-appearing control valve was PCR negative for this gene. The PCR-positive cows (nos. 04–927 and 05–1406) were the 2 oldest cows (13 and 15 years old, respectively). ITS 16–23 rRNA amplification was obtained only for the damaged valve of cow 04–927; the size of the amplicon product was ≈190 bp, which was identical to the size of the product obtained with the B. bovis reference strain (Figure). Amplification of the 16S rRNA and all the other genes studied were PCR positive for the damaged valves. A 16S rRNA PCR amplicon has been obtained from the normal-appearing valve of cow 05–1406 but could not be sequenced. Amplification of all the other genes studied were PCR negative for normal-appearing control valves of both cows. The genes rpoB (GenBank accession nos. EF432062, EF432061), ribC (accession nos. EF432060, EF432059), gltA (accession nos. EF432055, EF432056), groEL (accession nos. EF432058, EF432057) were partially sequenced. Sequence identities were respectively 100% with B. bovis (gltA) and 99% with B. bovis (groEL, ribC, rpoB). The sequence obtained with 16S rRNA (accession no. EF432054) had a 99% identity with B. bovis.
Figure.
PCR amplification of internal transcribed spacer 16S–23S on vegative and normal-appearing valves of cows 04–927 and 05–1406. 1, Molecular weight marker; 2, negative control; 3, Bartonella quintana; 4, B. bovis; 5 and 6, normal appearing and vegetative valves (Cow 04–927); 7 and 8, normal appearing and vegetative valves (Cow 05–1406); 9, molecular weight marker.
None of the cultures on rabbit blood agar (12) of fragments from the 22 vegetative valves yielded Bartonella isolates. The 2 PCR-positive cows had high IFA titers (5,120 and 640 for B. bovis antigen), whereas the 20 PCR-negative cows had low or negative titers (Table)
Table. Serologic and PCR results for the vegetative heart valves from 22 cows*.
| Case no. | Age, y | Valve | Bartonella PCR (gltA) | Indirect fluorescent antibody titer |
||
|---|---|---|---|---|---|---|
| B. bovis | B. chomelii | B. schoenbuchensis | ||||
| 05–1406 | 13 | Aortic | + | 5,120 | 320 | 640 |
| 04–927 | 15 | Mitral | + | 640 | 160 | 160 |
| 05–379 | 8 | Aortic | – | 40 | – | – |
| 04–269 | 7 | Aortic | – | – | – | – |
| 4071 | 3.5 | Pulmonary | – | 40 | 40 | 80 |
| 3977 | 5.5 | Aortic | – | – | – | – |
| 556 | 8.5 | Pulmonary | – | 80 | 40 | – |
| 5988 | 6 | Pulmonary | – | – | – | – |
| 1507 | 6.5 | Tricuspid | – | – | – | – |
| 766 | 12 | Tricuspid | – | – | – | – |
| 4002 | 5 | Tricuspid | – | – | – | – |
| 4815 | 8 | Pulmonary | – | – | – | – |
| 4768 | 5 | Pulmonary | – | – | – | – |
| 4921 | 6 | Tricuspid | – | – | – | – |
| 4784 | 5.5 | Aortic | – | – | – | – |
| 239 | 10 | Pulmonary | – | – | – | – |
| 269 | 7 | Aortic | – | – | – | – |
| 304 | 12 | Pulmonary | – | 40 | 40 | 40 |
| 528 | 6 | Tricuspid | – | – | – | – |
| 975 | 6.5 | Tricuspid | – | – | – | – |
| 1289 | 10 | Tricuspid | – | – | – | – |
| 116 | 6 | Pulmonary | – | – | – | – |
| 379 | 8 | Aortic | – | – | – | – |
*gltA, citrate synthase; +, positive; –, negative.
Conclusions
This is the first description, to our knowledge, of endocarditis associated with Bartonella in cattle. PCR amplification of the gltA gene, used for identification of Bartonella infection, gave an identity of 100% with the previously reported B. bovis gene sequence. The sequences of 4 additional genes (groEL, ribC, rpoB, and 16S rRNA) shared 99% identity with B. bovis genes. ITS amplification of 1 vegetative valve gave a fragment of ≈190 bp, which is the size expected for B. bovis (10). The lack of PCR amplification of the same genes from healthy-appearing valves indicated that the PCR amplification obtained with the vegetative valves was not the result of a B. bovis bacteremia. No definitive evidence exists that B. bovis had induced the primary lesion leading to the endocarditis. However, PCR amplification with universal primers for bacterial 16S rRNA allowed us to identify only Bartonella sequence in the damaged valves without apparent contamination with DNA from other bacteria.
Moreover, the high IFA antibody titer against B. bovis antigen and the low antibody titers of the PCR-negative endocarditis cases reinforced the likely role of B. bovis as the causative agent of these 2 bovine endocarditis cases. High antibody titers are commonly observed in human and canine cases of Bartonella endocarditis. In fact, high antibody titers are considered a major diagnostic criterion for Bartonella endocarditis in humans (3). Finally, the 2 B. bovis–infected vegetative valves were aortic and mitral valves, which are the most frequently involved valves in human and canine Bartonella endocarditis cases (5,13,14).
Two (9.1%) of the 22 endocarditis cases were Bartonella DNA positive. This percentage is within the range of 3% reported for human cases of endocarditis (14) and 19% (5) to 28% (13) reported for dogs. The 2 cases occurred in the oldest animals (Table), which suggests that B. bovis endocarditis could develop in geriatric cows, following chronic bacteremia in an overtly healthy animal. Nearly 30% of cattle >7 years of age are reportedly Bartonella bacteremic (12).
Cattle are the main reservoir for B. bovis, and diseases attributed to infection with this Bartonella species in cows are scarce (12). Nevertheless, these 2 cases demonstrated that B. bovis is a potential bovine pathogen and that B. bovis can induce endocarditis in the animal reservoir host, as previously shown for B. quintana, B. henselae, and B. vinsonii subsp. berkhoffii in humans, cats, and dogs, respectively (6,14,15). This study confirms that B. bovis can cause endocarditis in cows like B. henselae and B quintana in their respective feline and human reservoirs.
Acknowledgments
We thank Corinne Bouillin and Christelle Gandoin for their technical assistance.
Biography
Dr Maillard is an associate professor in large animal medicine at the National Veterinary School of Alfort, France. His research interest focuses on vectorborne bacterial diseases in ruminants.
Footnotes
Suggested citation for this article: Maillard R, Petit E, Chomel B, Lacroux C, Schelcher F, Vayssier-Taussat M, et al. Endocarditis in cattle caused by Bartonella bovis. Emerg Infect Dis [serial on the Internet]. 2007 Sep [date cited]. Available from http://www.cdc.gov/eid/content/13/9/1383.htm
References
- 1.Andrews AH, Williams BM. Endocarditis. In: Andrews AH, editor. Bovine medicine. Oxford: Blackwell Science Publishing; 2004. p. 726–8. [Google Scholar]
- 2.Reef VB, McGuirk SM. Diseases of the cardiovascular system. In: Smith BP, editor. Large animal internal medicine. St Louis: Mosby Publishing; 1996. p. 507–49. [Google Scholar]
- 3.Brouqui P, Raoult D. New insight into the diagnosis of fastidious bacterial endocarditis. FEMS Immunol Med Microbiol. 2006;47:1–13. 10.1111/j.1574-695X.2006.00054.x [DOI] [PubMed] [Google Scholar]
- 4.Houpikian P, Raoult D. Diagnostic methods. Current best practices and guidelines for identification of difficult-to-culture pathogens in infective endocarditis. Cardiol Clin. 2003;21:207–17. 10.1016/S0733-8651(03)00028-6 [DOI] [PubMed] [Google Scholar]
- 5.Sykes JE, Kittleson MD, Pesavento PA, Byrne BA, MacDonald KA, Chomel BB. Evaluation of the relationship between causative organisms and clinical characteristics of infective endocarditis in dogs: 71 cases (1992–2005). J Am Vet Med Assoc. 2006;228:1723–34. 10.2460/javma.228.11.1723 [DOI] [PubMed] [Google Scholar]
- 6.Chomel BB, Wey AC, Kasten RW, Stacy BA, Labelle P. Fatal case of endocarditis associated with Bartonella henselae type I infection in a domestic cat. J Clin Microbiol. 2003;41:5337–9. 10.1128/JCM.41.11.5337-5339.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bermond D, Boulouis HJ, Heller R, Van Laere G, Monteil H, Chomel BB, et al. Bartonella bovis Bermond et al. sp. nov. and Bartonella capreoli sp. nov., isolated from European ruminants. Int J Syst Evol Microbiol. 2002;52:383–90. [DOI] [PubMed] [Google Scholar]
- 8.Garcia-Esteban C, Escudero R, Barandika JF, Chaparro E, Rodriguez-Moreno I, Garcia-Perez A, et al. A molecular method for the identification of Bartonella species in clinical and environmental samples. In: Abstracts of the 4th International Conference on Rickettsiae, Logrono, Spain, 18–21 Jun 2005. Abstract 151. American Society for Rickettsiology, 2005. [Google Scholar]
- 9.La Scola B, Zeaiter Z, Khamis A, Raoult D. Gene-sequence-based criteria for species definition in bacteriology: the Bartonella paradigm. Trends Microbiol. 2003;11:318–21. 10.1016/S0966-842X(03)00143-4 [DOI] [PubMed] [Google Scholar]
- 10.Maillard R, Vayssier-Taussat M, Bouillin C, Gandoin C, Halos L, Chomel B, et al. Identification of Bartonella strains isolated from wild and domestic ruminants by a single-step PCR analysis of the 16S–23S intergenic spacer region. Vet Microbiol. 2004;98:63–9. 10.1016/j.vetmic.2003.09.022 [DOI] [PubMed] [Google Scholar]
- 11.Dalton MJ, Robinson LE, Cooper J, Regnery RL, Olson JG, Childs JE. Use of Bartonella antigens for serologic diagnosis of cat-scratch disease at a national referral center. Arch Intern Med. 1995;155:1670–6. 10.1001/archinte.155.15.1670 [DOI] [PubMed] [Google Scholar]
- 12.Maillard R, Grimard B, Chastant-Maillard S, Chomel B, Delcroix T, Gandoin C, et al. Effects of cow age and pregnancy on Bartonella infection in a herd of dairy cattle. J Clin Microbiol. 2006;44:42–6. 10.1128/JCM.44.1.42-46.2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.MacDonald KA, Chomel BB, Kittleson MD, Kasten RW, Thomas WP, Pesavento P. A prospective study of canine infective endocarditis in northern California (1999–2001): emergence of Bartonella as a prevalent etiologic agent. J Vet Intern Med. 2004;18:56–64. [DOI] [PubMed] [Google Scholar]
- 14.Raoult D, Fournier PE, Drancourt M, Marrie TJ, Etienne J, Cosserat J, et al. Diagnosis of 22 new cases of Bartonella endocarditis. Ann Intern Med. 1996;125:646–52. [DOI] [PubMed] [Google Scholar]
- 15.Breitschwerdt EB, Atkins CE, Brown TT, Kordick DL, Snyder PS. Bartonella vinsonii subsp. berkhoffii and related members of the alpha subdivision of the Proteobacteria in dogs with cardiac arrhythmias, endocarditis, or myocarditis. J Clin Microbiol. 1999;37:3618–26. [DOI] [PMC free article] [PubMed] [Google Scholar]