Abstract
Physical inactivity is an established risk factor for cardiovascular diseases. However, while physical activity is recommended as a component of healthy lifestyle, the amount (intensity, duration and frequency) of physical activity required to protect against coronary heart disease (CHD) and cerebrovascular disease (i.e., stroke) is unclear. In general, there is a graded inverse association of physical activity with CHD and total cardiovascular disease (the combination of CHD and stroke). The patterns of association between physical activity dose and stroke are less clear; individual studies suggest a threshold effect for benefits, while meta-analytic studies report a graded inverse association. Despite known differences in physical activity behaviors between men and women, the patterns of association between dose of activity and cardiovascular diseases are similar by gender. Observational studies of walking behaviors and one recent clinical trial suggest that lower “doses” of physical activity are associated with a lower risk of cardiovascular disease. Thus, with very few specific cautions, there is enough evidence to recommend to healthy adults that any activity is beneficial and that more activity is even better.
Keywords: observational studies, physical activity, cardiovascular disease, coronary heart disease
Introduction
Ischemic cardiovascular disease (CVD) is the leading cause of death in adults in the United States and developed countries worldwide.1 Physical inactivity was cited as one of 9 major contributors to heart disease mortality worldwide in the 2004 INTERHEART study (an international case-control study of risk factors for myocardial infarction).2 The authors estimated that the proportion of myocardial infarction attributable to physical inactivity was 12%, an attributable risk proportion that fell in between hypertension (18%) and type 2 diabetes mellitus (10%)—established heart disease risk factors whose prevalence is also inversely associated with physical activity levels.
Evidence of a protective effect of physical activity on health outcomes has been apparent since the origin of modern medicine. Hippocrates was referring to physical activity when he stated that: “All parts of the body which have a function, if used in moderation and exercised in labours in which each is accustomed, become thereby healthy, well-developed and age more slowly, but if unused and left idle they become liable to disease, defective in growth, and age quickly.”3 Quantitative epidemiology studies conducted by Professor Jeremy Morris beginning in the 1940s demonstrated that men who engaged in high levels of occupational physical activity were less likely to develop cardiovascular disease.4 Since that time, numerous studies have replicated those findings in a range of settings, using both occupational and leisure activity, and in relation to other causes of morbidity and mortality.
Based on the strength and consistency of these observations, the American College of Sports Medicine (ACSM), the Centers for Disease Control and Prevention (CDC) and other professional and government health organizations teamed up to publish a number of position statements providing recommendations for physical activity to improve health outcomes. Over time, these recommendations have expanded beyond the benefits of aerobic activity to other components of physical activity such as strength training and flexibility.5 While the statements have consistently recommended regular physical activity, the definition of regular activity has shifted over time. As a result, health professionals and the lay public remain unclear about the amount of physical activity required to experience health benefits.
Consequently, we still do not have an answer to the question, “How much activity is enough?” Given the legions of adults who do not engage in any leisure time activity and the shift towards sedentary occupations and motorized transportation, it is critical that we address the equally important question: “How little activity is required to show some health benefit?” The present review will summarize what is known about the relationship between physical activity dose and cardiovascular health. Because an overwhelming volume of research is focused on aerobic activities which improve cardiorespiratory fitness, the current review will focus on aerobic activities and consider other components of physical fitness (i.e., muscular fitness, flexibility) within the context of an physically active lifestyle. Although the atherosclerotic process affects many vascular beds throughout the body, the focus of this review is coronary heart disease, and cerebrovascular disease (i.e., stroke). We also include a summary measure of cardiovascular diseases, which includes CHD, stroke and procedures to prevent clinical CHD such as coronary artery bypass grafting or angioplasty.
Defining Activity “Dose”
Physical activity “dose” reflects a combination of the duration, intensity or frequency of activity. Thus, defining the amount of physical activity required for health benefits could refer to one or all of these components. The 1995 CDC/ACSM physical activity recommendations for adults prescribed a minimum of 30 minutes of moderate- to vigorous-intensity activity on “most days” of the week.6 Lack of specificity about the definition of “most days” and whether those 30 minutes needed to be carried out in activity bouts of at least 10 minutes generated confusion in the public. The authors (many of whom were involved in both statements) attempted to clarify both issues in the 2007 update by proposing specific scenarios with combinations based on both the duration of the exercise session, frequency and intensity of activity.7 For example, the authors recommended that adults engage in moderate intensity physical activities (defined as those activities that lead to notable increases in heart rate and breathing) for at least 30 minutes per day, five days per week. Alternatively, adults can engage in vigorous intensity activities, which cause rapid breathing and substantial increases in heart rate for 20 minutes per day at least 3 days per week. The ideal physical activity program represents a combination of both moderate- and vigorous-intensity physical activities in bouts lasting at least 10 minutes per session. Specific recommendations vary for older adults8 and children9 and whether the goal is weight loss, weight maintenance10 or disease prevention. All recommendations share components that address the frequency, intensity and duration of activities.
Recent recommendations regarding physical activity dose have had the benefit of summary findings presented at the 2000 Hockley Valley Symposium in Toronto, Canada, which was convened specifically to address the question of physical activity dose response and health outcomes.11 The Hockley Valley Symposium is perhaps the single most comprehensive meeting of physical activity experts on the amount of physical activity required to experience a range of health benefits. A substantial portion of the conference was devoted to addressing cardiovascular disease outcomes (e.g., coronary heart disease and cerebrovascular disease), established cardiovascular disease risk factors (e.g., obesity, hypertension, diabetes, lipids), and novel risk factors (e.g., depression and anxiety).
Physical Activity and Cardiovascular Diseases
Cardiovascular Disease
In his 2001 summary report from the Hockley Valley Symposium, Kohl reported findings from 8 published studies based on 5 large cohort studies of the association between physical activity dose and cardiovascular disease.12 With follow-up data ranging from 5 to 26 years, the majority of studies (5 out of 8) reported a graded inverse association of physical activity intensity and/or duration with the incidence of CVD. Despite the consistent inverse association observed across studies, it is still not possible to determine a summary “minimum dose” required to prevent CVD because of the variety of instruments used to quantify physical activity.
In 2003, Yu and colleagues tested the association of activity dose (both intensity and frequency) on the 10-year incidence of CVD, CHD and all-cause mortality in 2512 middle-aged British men.13 Physical activity was measured using the Minnesota Leisure Time Physical Activity Questionnaire14 and used to generate an “activity index”. Activities in the “light” tertile having intensity codes of <4 (e.g., bowling, walking sailing), moderate activity had activity codes from 4.5 to 5.5 (e.g., golfing, digging, dancing) and heavy activity had intensity codes >6.0 (e.g., swimming, jogging, stair climbing). In age-adjusted models, the relative hazard of CVD and CHD mortality decreased with increasing intensity and duration of total leisure time activity. However, following additional adjustment for blood pressure, body mass index, cigarette smoking, family history of heart disease, social class and occupational activity, the association between the highest level of activity as compared with the lowest, attenuated to non-significance (hazard ratio=0.64, 95% CI: 0.40-1.04). Increasing frequency of heavy activities was associated with a 62% lower likelihood of CVD mortality (upper tertile vs. the lowest), and the trend across activity levels was statistically significant (p<0.01) even following risk factor adjustment. Neither the time spent engaging in job-related physical activity nor the combination of light and moderate activities, was associated with CVD mortality. Patterns were similar with CHD was studied separately. Findings from the present study underscore the importance of higher intensity activities to lower CVD risk.
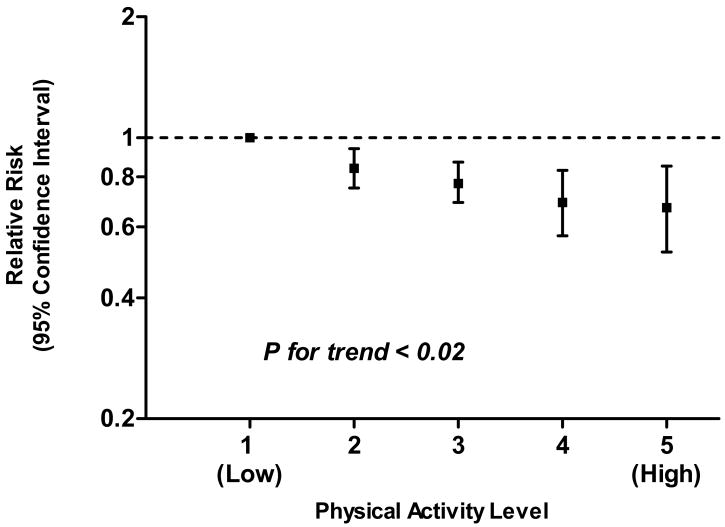
Based on epidemiologic evidence that overall levels of physical activity are lower in men as compared with women and because women engage in different types of activities than men, Oguma and colleagues reviewed the literature on the association of physical activity with cardiovascular disease in women.15 Figure 1 displays the meta-analytic results from the reviewed studies. When physical activity levels from the longitudinal studies were combined into a 5-level ranking from low-to-high, there was a graded inverse association of relative physical activity level with the incidence of CVD in women. As compared with women in the lowest combined quintile of relative activity, women in the highest quintile were 37% less likely to experience cardiovascular disease events. However, one caution is that one of the three studies included in that particular meta-analytic estimate was based on the Lipid Research Clinics Study16 which directly measured cardiorespiratory fitness, an objective measure that is commonly more strongly associated with morbidity and mortality than activity.
Figure 1.
Meta-Analytic results15 of the association between physical activity dose-response and cardiovascular disease in 3 prospective studies of women
Coronary Heart Disease
CHD is the leading cause of death in the United States.1 At the time of the Hockley Symposium, there were 23 observational studies (20 of which were prospective observational studies) describing the association of the amount of leisure time or occupational activity on CHD.12 Only 8 of these studies failed to observe a dose-response association. Some studies that did not report an inverse graded association did report threshold effects or “U” shaped associations indicating elevated risks of mortality at both the lowest and the highest levels of activity. The complete absence of moderate to vigorous physical activity is associated with a higher incidence of cardiovascular morbidity and mortality as described in numerous previous studies. Conversely, intense vigorous exercise, particularly in untrained individuals, also conveys elevated risks for CHD events.17 Consequently, an uptick in disease incidence at the extreme ends of the activity spectrum is plausible, particularly if the estimates account for the study participants' usual physical activity levels. The risks associated with vigorous exercise in men and women who engage in regular activity is minimal; when adverse events with heavy exercise are observed, they quite often result from underlying undiagnosed congenital heart defects, familial long Q-T syndrome, or hypertrophic cardiomyopathy.
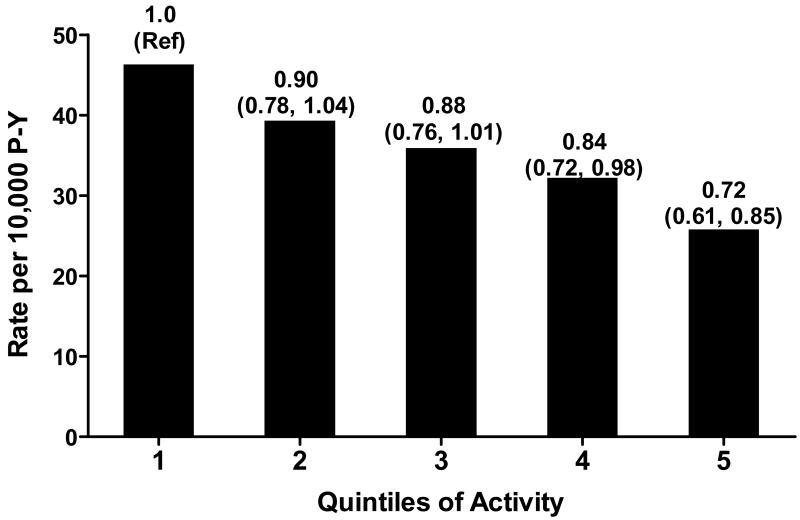
In 2002, the Health Professionals Follow-Up Study reported findings on the association between exercise type and intensity in relation to incident CHD from 44,452 men who were followed from 1986-1998.18 Men were queried about the time they regularly spent in activities of varying intensity. Time spent in each activity was multiplied by it's metabolic equivalent (MET) value from the Ainsworth compendium19 to generate a MET-hour score. The physical activity survey was administered every 2 years. In over 475,755 person-years of follow up, 1,700 incident cases of CHD were identified. Figure 2 displays the graded monotonic inverse association between time-averaged physical activity participation and incident CHD. Overlayed on the bar chart are the multivariable adjusted relative risks for incident CHD at each subsequently higher quintile of physical activity (median = 49.1 MET-hours/week) as compared with the lowest level (median=1.2 MET-hours/week). Multivariable estimates are adjusted for age, smoking, alcohol intake, family history of CHD, diabetes, hypertension, hypercholesterolemia, use of vitamin E supplements and numerous dietary factors.
Figure 2.
Crude Rates and Adjusted Relative Risks (95% Confidence Intervals) for CHD by weekly MET-hours of physical activity, Health Professionals Follow-Up Study.18 The median value and range MET-hour/week are as follows: Q1=1.2 (0-2.9); Q2=5.0 (3.0-7.9); Q3=12.1 (8.0-17.7); Q4=24.1 (17.8-34.5); Q5=49.1 (34.6-69.2).
In that same study, Tenesescu and colleagues18 reported an inverse association between exercise intensity and incident CHD, with self-reported exercise MET-levels >6 associated with a statistically significant 17% decreased risk (relative risk=0.83, 95% confidence interval [CI]: 0.74 to 0.97) as compared with MET intensity of 1-3.9.18 The authors also tested and confirmed that these patterns of inverse association remained consistent for every major exercise type (e.g., running, jogging, rowing, cycling, swimming, and racquet sports) and resistance training.
Meta-analytic results from two longitudinal studies that categorized activity into 5 levels and studied the incidence of CHD in women, also reported a graded inverse association. As compared with women in the lowest physical activity category, relative risks were 0.83 (95% CI= 0.69-0.99), 0.77 (95% CI: 0.64-0.92), 0.72 (95% CI: 0.59-0.87), and 0.57 (95% CI: 0.41-0.79) in categories 2-5, respectively (p for trend = 0.014).15 Surprisingly, the pooled relative risk from 4 studies that investigated the continuous association between activity and CHD, was not statistically significant (RR=0.81, 95% CI: 0.56-1.17). The authors propose that hetereogeneity in the measurement of physical activity across studies and differential adjustment for confounders could account for the absence of association.
Cerebrovascular Disease
Cerebrovascular disease (i.e., stroke) is the third leading cause of death in the US.1 On average, stroke occurs at older ages than CHD, on average, which requires observational studies with extended follow-up time, a large sample size or a high risk population in order to have enough events. Of the 15 studies (13 of which were prospective) with 16 separate publications that Kohl reviewed,12 6 reported an inverse dose-response relation between physical activity and stroke incidence. No dose-response association was observed in 8 of those studies, while a handful of others reported increased risks at the tail-ends of the physical activity spectrum. While the “U” shaped association between physical activity and CVD is biologically plausible, reasons for the excess risk for cerebrovascular disease on the uppermost end of activity are less clear. Because of the relatively smaller number of events, ischemic versus hemorrhagic strokes were pooled for analysis. Findings for the association between physical activity and stroke were relatively weaker and less robust than for those observed when CVD was the outcome. Plausible explanations for the difference are heterogeneity in stroke subtypes (e.g., hemorrhagic vs. ischemic) and fewer overall events.
In 2004, Wendel-Vos and colleagues20 conducted a meta-analysis of case-control and observational studies of physical activity and stroke subtypes. While assessing dose response wasn't a primary objective of the analysis, the authors assembled 31 case-control and cohort studies that assessed physical activity in at most 3 levels. Using studies that reported at least three levels of activity, the authors compiled the activity doses into a relative activity score and determined that high levels of activity at work (versus the lowest levels) were significantly associated with hemorrhagic (RR=0.31, 95% CI: 0.13-0.76) and ischemic (RR=0.57, 95% CI: 0.43-0.77) stroke, whereas moderate work-related activity was not statistically significantly related to either stroke subtype. Similarly, only the highest levels of leisure time activity were significantly inversely associated with incident total (RR=0.78, 95% CI: 0.71-0.85), hemorrhagic (RR=0.74, 95% CI: 0.57-0.96) and ischemic strokes (RR=0.79, 95% CI: 0.69-0.91). In summary, there appeared to be a threshold affect above which occupational or leisure time activity lowered the risk of both stroke, but no apparent U-shaped association as was shown in previous studies.
Individual findings from five cohort studies that investigated the dose-response association between physical activity and stroke in women and were reviewed by Oguma et al.15, Each individual study reported relatively weak associations between activity and stroke that only achieved borderline statistical significance when the most extreme activity categories were compared (e.g., highest vs. lowest). However, when pooled relative risks were calculated the relative risk of stroke was statistically significantly lower in the uppermost tertile of relative physical activity score as compared with the lowest tertile (RR=0.63, 95% CI: 0.46-0.86), and borderline significant in the middle versus the low tertile (RR=0.73, 95% CI: 0.52-1.01). The p value for the trend was highly statistically significant at p<0.00001.
In 2000, the Nurse's Health Study followed 72,488 women for up to 8 years (560,087 person years) and 407 had incident strokes, of which 63% were ischemic.21 Based on self reported physical activity levels (converted to MET-hours of activity per week) and categorized into quintiles, the relative risk for stroke decreased with increasing quintile of physical activity. As compared with quintile 1 (<2 MET-hrs/week), the relative risks for quintiles 2 (2.1-4.6 MET hrs/week), 3 (4.7-10.4 MET-hrs/week), 4 (10.5-21.7 MET-hrs/week) and 5 (>21.7 MET-hrs/week) were 0.87, 0.83, 0.76 and 0.52, respectively (p for trend =0.003). The inverse association was statistically significant when ischemic stroke was examined separately, but not for hemorrhagic stroke.
How Little Activity is Required?
Forty percent (40.5%) of adults age >18 years—an estimated 90 million people, who responded to the National Health Interview Survey in 2005 reported that they never engage in any physical activity.22 In fact, when physical activity was measured by accelerometry in the National Health and Nutrition Examination Survey (NHANES) 1999-2002, less than 5% of the adult population met physical activity guidelines of 30 minutes of moderate activity per week when activity was defined in 10 minute bouts.23 Consequently, our nation of largely inactive adults, it is equally important to determine the minimum “dose” of activity required to lower risk of cardiovascular disease.
One of the most common light-to-moderate activities is walking. While walking specifically for exercise may reach levels of intensity to be described as moderate, quite often walking is a primary mode of transportation and thus no special effort is expended to raise the intensity of the effort. Whether walking is associated with the incidence of cardiovascular diseases has addressed in a number of observational studies. Meta-analytic results of the association of walking with cardiovascular outcomes in women reported that as little as one hour of walking per week was associated with a lower relative risk for CHD (RR=0.60, 95% CI: 0.39-0.94, n=3 studies), stroke (RR= 0.78, 95% CI: 0.56-1.08) and overall CVD (RR=0.80, 95% CI: 0.74-0.87).15
In 2002, Manson et al compared walking to more vigorous activities in relation to cardiovascular events in 73,749 women who participated in the Women's Health Initiative Observational Study.24 At baseline, women were queried about the frequency and duration of several types of physical activities and walking. Walking behaviors were determined by women's responses to questions about the frequency of walking outside a woman's home in bouts of 10 minutes or more without stopping, the usual walking pace and average duration of these walks.
The rate and relative risk of CHD and total CVD was inversely associated with quintile of MET-hours as determined by the product of reported duration and intensity of walking. Only the uppermost quintile of walking corresponding to approximate 3.5 hours/week of moderate walking or 30 minutes per week of brisk walking (14.75 MET-hours/week) was associated with a lower risk of developing CHD (RR=0.82, 95% CI: 0.67-1.00) as compared with the lowest quintile of walking (0 to 1.19 MET hours/week). A usual walking pace of >4 miles/hour was associated with a multivariable adjusted relative risk of CHD that was nearly half that of men who walked <2 miles/hour (RR=0.51, 95% CI=0.31-0.84).25 Walking was similarly associated with a lower likelihood of stroke in women, in a magnitude similar to that of more vigorous activities.21
The Dose Response to Exercise in Women (DREW) Study is a randomized trial investigate the effect of exercise dose on cardiorespiratory fitness and blood pressure in 464 sedentary postmenopausal overweight or obese women.26 Participants were randomized to a control group or intervention groups who were assigned physical activity at a dose of 50% (4 kcal/kg energy expenditure per week), 100% (8 kcal/kg energy expenditure per week) or 150% (12 kcal/kg energy expenditure per week) of the current recommended dose of activity for healthy adults for a six-month intervention period. As compared with the control group, fitness increased by 4.2%, 6% and 8% in the 50%, 100%, 150% activity groups, respectively, after adjustment for age, race/ethnicity, weight and peak heart rate. There were no changes in systolic or diastolic blood pressure values, weight, or body fat percent from baseline for any of the exercise groups versus the control groups. However, waist circumference was significantly smaller at follow-up in all three exercise groups as compared with the control group (p<0.05).
The DREW investigators reported that their most significant finding was that fitness increased with even minimal levels of activity. Moving from being totally sedentary to an activity level of approximately 72.2 minutes per week—a little over 10 minutes per day, resulted in improved cardiorespiratory fitness. These shifts in activity level can surely be achieved through walking programs and other small changes in activity behaviors among the sedentary. Prior research has confirmed an inverse association between cardiorespiratory fitness and the development of cardiovascular disease risk factors in young27 and middle-aged adults.28 Fitness is inversely associated with cardiovascular and total mortality in men and women across the lifespan.29, 30 If physical activity behaviors are continued at their new higher levels (at 50% of current recommendations) perhaps even greater fitness changes over the long term would have been observed. These longer term changes in fitness may in turn lower long term cardiovascular risk by modifying CVD risk factors. In the DREW study, blood pressure levels and other cardiovascular disease risk factors may not have changed significantly because the time period of observation (6 months) was relatively short. Cardiovascular disease develops over decades, thus it may be more plausible that activity patterns need to also be carried out over the long term.
Conclusion
In sum, the literature describes a dose-response relationship between physical activity and cardiovascular disease morbidity and mortality. Women and men demonstrate similar CVD risk lowering benefits by engaging in regular physical activity. More activity is associated with a lower risk of developing cardiovascular disease when compared to less physical activity. Although there may be a threshold over which activity levels convey greater risk, only those who are totally sedentary (i.e., “weekend warriors”) or who have pre-existing health conditions are at risk for acute CV events with sudden, vigorous-intensity physical activity. The gradual introduction of activity combined with physician evaluation prior to starting an exercise program may mitigate these risks. Low levels of activity that can be achieved by adopting walking programs can lower cardiovascular disease risks and these activity recommendations are generally safe and applicable to all adults across the age spectrum.
Acknowledgments
Material in this manuscript was presented at the 3rd Annual Building Healthy Lifestyles Conference at Arizona State University, Mesa, AZ on February 28-29, 2008.
References
- 1.Lloyd-Jones D, Adams R, Carnethon M, De Simone G, Ferguson TB, Flegal K, Ford E, Furie K, Go A, Greenlund K, Haase N, Hailpern S, Ho M, Howard V, Kissela B, Kittner S, Lackland D, Lisabeth L, Marelli A, McDermott M, Meigs J, Mozaffarian D, Nichol G, O'Donnell C, Roger V, Rosamond W, Sacco R, Sorlie P, Stafford R, Steinberger J, Thom T, Wasserthiel-Smoller S, Wong N, Wylie-Rosett J, Hong Y. Heart Disease and Stroke Statistics--2009 Update. A Report From the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2008 doi: 10.1161/CIRCULATIONAHA.108.191261. [DOI] [PubMed] [Google Scholar]
- 2.Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, McQueen M, Budaj A, Pais P, Varigos J, Lisheng L. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364(9438):937–952. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 3.Freeman LW. Mosby's Complementary & Alternative Medicine: A Research-based Approach. 2. Elsevier Health Sciences; 2004. [Google Scholar]
- 4.Paffenbarger RS, Jr, Blair SN, Lee IM. A history of physical activity, cardiovascular health and longevity: the scientific contributions of Jeremy N Morris, DSc, DPH, FRCP. Int J Epidemiol. 2001;30(5):1184–1192. doi: 10.1093/ije/30.5.1184. [DOI] [PubMed] [Google Scholar]
- 5.Williams MA, Haskell WL, Ades PA, Amsterdam EA, Bittner V, Franklin BA, Gulanick M, Laing ST, Stewart KJ. Resistance Exercise in Individuals With and Without Cardiovascular Disease: 2007 Update: A Scientific Statement From the American Heart Association Council on Clinical Cardiology and Council on Nutrition, Physical Activity, and Metabolism. Circulation. 2007;116(5):572–584. doi: 10.1161/CIRCULATIONAHA.107.185214. [DOI] [PubMed] [Google Scholar]
- 6.Pate RR, Pratt M, Blair SN, Haskell WL, Macera CA, Bouchard C, Buchner D, Ettinger W, Heath GW, King AC, et al. Physical activity and public health. A recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. JAMA. 1995;273(5):402–407. doi: 10.1001/jama.273.5.402. [DOI] [PubMed] [Google Scholar]
- 7.Physical Activity and Public Health: Updated Recommendation for Adults From the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116(9):1081–1093. doi: 10.1161/CIRCULATIONAHA.107.185649. [DOI] [PubMed] [Google Scholar]
- 8.Physical Activity and Public Health in Older Adults: Recommendation From the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116(9):1094–1105. doi: 10.1161/CIRCULATIONAHA.107.185650. [DOI] [PubMed] [Google Scholar]
- 9.Katzmarzyk PT, Baur LA, Blair SN, Lambert EV, Oppert JM, Riddoch C. Ontario: summary statement and recommendations. Appl Physiol Nutr Metab; Expert panel report from the International Conference on Physical Activity and Obesity in Children; 24-27 June 2007; Toronto. 2008. pp. 371–388. [DOI] [PubMed] [Google Scholar]
- 10.Kumanyika SK, Obarzanek E, Stettler N, Bell R, Field AE, Fortmann SP, Franklin BA, Gillman MW, Lewis CE, Poston WC, II, Stevens J, Hong Y. Population-Based Prevention of Obesity: The Need for Comprehensive Promotion of Healthful Eating, Physical Activity, and Energy Balance: A Scientific Statement From American Heart Association Council on Epidemiology and Prevention, Interdisciplinary Committee for Prevention (Formerly the Expert Panel on Population and Prevention Science) Circulation. 2008;118(4):428–464. doi: 10.1161/CIRCULATIONAHA.108.189702. [DOI] [PubMed] [Google Scholar]
- 11.Bouchard C. Physical activity and health: introduction to the dose-response symposium. Med Sci Sports Exerc. 2001;33(6 Suppl):S347–350. doi: 10.1097/00005768-200106001-00002. [DOI] [PubMed] [Google Scholar]
- 12.Kohl HW., 3rd Physical activity and cardiovascular disease: evidence for a dose response. Med Sci Sports Exerc. 2001;33(6 Suppl):S472–483. doi: 10.1097/00005768-200106001-00017. discussion S493-474. [DOI] [PubMed] [Google Scholar]
- 13.Yu S, Yarnell JW, Sweetnam PM, Murray L. What level of physical activity protects against premature cardiovascular death? The Caerphilly study. Heart. 2003;89(5):502–506. doi: 10.1136/heart.89.5.502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Conway JM, Irwin ML, Ainsworth BE. Estimating energy expenditure from the Minnesota Leisure Time Physical Activity and Tecumseh Occupational Activity questionnaires - a doubly labeled water validation. J Clin Epidemiol. 2002;55(4):392–399. doi: 10.1016/s0895-4356(01)00497-8. [DOI] [PubMed] [Google Scholar]
- 15.Oguma Y, Shinoda-Tagawa T. Physical activity decreases cardiovascular disease risk in women: review and meta-analysis. Am J Prev Med. 2004;26(5):407–418. doi: 10.1016/j.amepre.2004.02.007. [DOI] [PubMed] [Google Scholar]
- 16.Stevens J, Cai J, Evenson KR, Thomas R. Fitness and fatness as predictors of mortality from all causes and from cardiovascular disease in men and women in the lipid research clinics study. Am J Epidemiol. 2002;156(9):832–841. doi: 10.1093/aje/kwf114. [DOI] [PubMed] [Google Scholar]
- 17.Thompson PD, Franklin BA, Balady GJ, Blair SN, Corrado D, Estes NAM, III, Fulton JE, Gordon NF, Haskell WL, Link MS, Maron BJ, Mittleman MA, Pelliccia A, Wenger NK, Willich SN, Costa F, Collaboration With the American College of Sports M Exercise and Acute Cardiovascular Events: Placing the Risks Into Perspective: A Scientific Statement From the American Heart Association Council on Nutrition, Physical Activity, and Metabolism and the Council on Clinical Cardiology. Circulation. 2007;115(17):2358–2368. doi: 10.1161/CIRCULATIONAHA.107.181485. [DOI] [PubMed] [Google Scholar]
- 18.Tanasescu M, Leitzmann MF, Rimm EB, Willett WC, Stampfer MJ, Hu FB. Exercise type and intensity in relation to coronary heart disease in men. JAMA. 2002;288(16):1994–2000. doi: 10.1001/jama.288.16.1994. [DOI] [PubMed] [Google Scholar]
- 19.Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM, Strath SJ, O'Brien WL, Bassett DR, Jr, Schmitz KH, Emplaincourt PO, Jacobs DR, Jr, Leon AS. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc. 2000;32(9 Suppl):S498–504. doi: 10.1097/00005768-200009001-00009. [DOI] [PubMed] [Google Scholar]
- 20.Wendel-Vos GC, Schuit AJ, Feskens EJ, Boshuizen HC, Verschuren WM, Saris WH, Kromhout D. Physical activity and stroke. A meta-analysis of observational data. Int J Epidemiol. 2004;33(4):787–798. doi: 10.1093/ije/dyh168. [DOI] [PubMed] [Google Scholar]
- 21.Hu FB, Stampfer MJ, Colditz GA, Ascherio A, Rexrode KM, Willett WC, Manson JE. Physical activity and risk of stroke in women. Jama. 2000;283(22):2961–2967. doi: 10.1001/jama.283.22.2961. [DOI] [PubMed] [Google Scholar]
- 22.National Center for Health Statistics. Health 2007: Chartbook on Trends in the Health of Americans. Department of Health and Human Services; [March, 2008]. Available at: http://www.cdc.gov/nchs/hus07.pdf. [PubMed] [Google Scholar]
- 23.Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–188. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 24.Manson JE, Greenland P, LaCroix AZ, Stefanick ML, Mouton CP, Oberman A, Perri MG, Sheps DS, Pettinger MB, Siscovick DS. Walking compared with vigorous exercise for the prevention of cardiovascular events in women. N Engl J Med. 2002;347(10):716–725. doi: 10.1056/NEJMoa021067. [DOI] [PubMed] [Google Scholar]
- 25.Tanasescu M, Leitzmann MF, Rimm EB, Hu FB. Physical Activity in Relation to Cardiovascular Disease and Total Mortality Among Men With Type 2 Diabetes. Circulation. 2003;107(19):2435–2439. doi: 10.1161/01.CIR.0000066906.11109.1F. [DOI] [PubMed] [Google Scholar]
- 26.Church TS, Earnest CP, Skinner JS, Blair SN. Effects of Different Doses of Physical Activity on Cardiorespiratory Fitness Among Sedentary, Overweight or Obese Postmenopausal Women With Elevated Blood Pressure: A Randomized Controlled Trial. JAMA. 2007;297(19):2081–2091. doi: 10.1001/jama.297.19.2081. [DOI] [PubMed] [Google Scholar]
- 27.Carnethon MR, Gidding SS, Nehgme R, Sidney S, Jacobs DR, Jr, Liu K. Cardiorespiratory Fitness in Young Adulthood and the Development of Cardiovascular Disease Risk Factors. JAMA. 2003;290(23):3092–3100. doi: 10.1001/jama.290.23.3092. [DOI] [PubMed] [Google Scholar]
- 28.Laaksonen DE, Lakka HM, Salonen JT, Niskanen LK, Rauramaa R, Lakka TA. Low Levels of Leisure-Time Physical Activity and Cardiorespiratory Fitness Predict Development of the Metabolic Syndrome. Diabetes Care. 2002;25(9):1612–1618. doi: 10.2337/diacare.25.9.1612. [DOI] [PubMed] [Google Scholar]
- 29.Ekelund LG, Haskell WL, Johnson JL, Whaley FS, Criqui MH, Sheps DS. Physical fitness as a predictor of cardiovascular mortality in asymptomatic North American men. The Lipid Research Clinics Mortality Follow-up Study. New England Journal of Medicine. 1988;319(21):1379–1384. doi: 10.1056/NEJM198811243192104. [DOI] [PubMed] [Google Scholar]
- 30.Gulati M, Pandey DK, Arnsdorf MF, Lauderdale DS, Thisted RA, Wicklund RH, Al-Hani AJ, Black HR. Exercise Capacity and the Risk of Death in Women: The St James Women Take Heart Project. Circulation. 2003;108(13):1554–1559. doi: 10.1161/01.CIR.0000091080.57509.E9. [DOI] [PubMed] [Google Scholar]