Abstract
Study Design
Radiological analysis.
Purpose
To investigate sacralization of L5 on radiological studies of degenerative spondylolisthesis at L4-L5.
Overview of Literature
Degenerative spondylolisthesis commonly develops at L4-L5. Sacralization of L5 is thought to cause stress concentration at this level, which accentuates degenerative changes and promotes development of degenerative spondylolisthesis. However, there has been no study dedicated to determining whether the presence of sacralization at L5 influences the radiological findings in degenerative spondylolisthesis at L4-L5.
Methods
Seventy-eight patients with degenerative spondylolisthesis at L4-L5 were classified into two groups according to the presence of L5 sacralization: with (n=54) and without (n=24). Four radiographic parameters were measured and compared between the two groups: anterior slippage of L4 on L5 (% slip), facet orientation of L4-L5 (degrees), facet osteoarthritis of L4-L5 by Fujiwara's criteria (1~4 grades), and disc degeneration of L4-L5 by Frymoyer's criteria (grades 1~5).
Results
There was no significant difference in the degree of anterior slippage of L4 on L5 (17.02±6.21 versus 16.65±4.87, p=0.809), facet orientation (54.99±12.18 versus 56.23±4.35, p=0.642), facet osteoarthritis (3.43±0.59 versus 3.53±0.37, p=0.527), or disc degeneration (4.50±0.51 versus 4.35±0.61, p=0.340) between the two groups.
Conclusions
Our study shows that the influence of sacralization of L5 on radiological findings in degenerative spondylolisthesis at L4-L5 may be less significant than previously expected. Further studies in large patient groups are needed to clarify the role of L5 sacralization on the development of degenerative spondylolisthesis at L4-L5.
Keywords: Degenerative spondylolisthesis, Sacralization, Radiological findings
Introduction
Degenerative spondylolisthesis is a common pathologic entity of the lumbar spine, especially of L4-L5. The common radiological findings in degenerative spondylolisthesis include arthritic changes of the facet joints and disc degeneration, as well as anterior slippage of the corresponding level1,2. It has been reported that the incidence of L5 sacralization is higher in patients with degenerative spondylolisthesis at L4-L5 than in the general population3-5. Although there is some debate, it is possible that L5 sacralization contributes to the development of degenerative spondylolisthesis, lumbar disc degeneration and herniation, and low back pain6-11. The sacralization of L5 is thought to cause stress concentration on L4-L5, which can accentuate development of degenerative spondylolisthesis and promote degenerative changes. However, little attention has been directed to whether there are differences in radiological findings in degenerative spondylolisthesis at L4-L5 in patients with and without L5 sacralization. Therefore, the authors performed the current study to investigate the role of L5 sacralization in influencing radiographic findings in degenerative spondylolisthesis at L4-L5.
Materials and Methods
Seventy-eight patients with degenerative spondylolisthesis at L4-L5 were included in this study. There were 57 women and 21 men. Degenerative spondylolisthesis was defined as the anterior slippage of L4 on L5 on lateral radiographs of the lumbar spine. All patients were classified into one of two groups according to the presence of L5 sacralization, which was defined using Tini et al's criteria5 for anteroposterior radiographs of the lumbar spine: degenerative spondylolisthesis with (n=54) and without (n=24) sacralization of L5. Mean patient age at the time of surgery was 58.5 years (range, 35~72 years), with no statistically significant difference noted between the two groups (p<0.05). Patients with any signs of lytic lesions were excluded from the study.
Plain radiographs of the lumbar spine, including anteroposterior and lateral radiographs, were taken with a tube-film distance of 1.2 m. Magnetic resonance imaging was performed using a 1.5-Tesla unit (Siemens, Somatoplus, Germany) in all patients. Both T2-weighted images (T2WI) (repetition time [TR]=3000 ms, echo time [TE]=80 ms) and T1-weighted images (T1WI) (TR=600 ms, TE=20~30 ms) were taken. The slice thickness was 3 mm.
Two orthopaedic spine surgeons who were unaware of the purpose of this study independently measured four radiographic parameters twice: anterior slippage of L4 on L5, facet orientation of L4-L5, facet osteoarthritis of L4-L5, and disc degeneration of L4-L5. To minimize inter- and intraobserver error, the means of four measurements were calculated and used as the final value for the four radiographic findings.
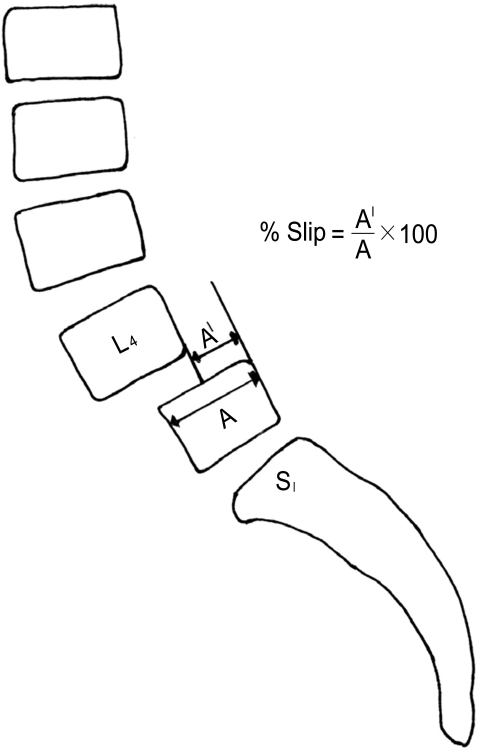
1. Anterior slippage of L4 on L5
The degree of anterior slippage of L4 on L5 was assessed on lateral radiographs of the lumbar spine and calculated as a percentage of the sagittal diameter of the slipped vertebral body: A'/A×100 (%) (Fig. 1).
Fig. 1.
The degree of anterior slippage of L4 on L5 was assessed on lateral radiographs of the lumbar spine and calculated as a percentage of the sagittal diameter of the slipped vertebral body: A'/A×100 (%).
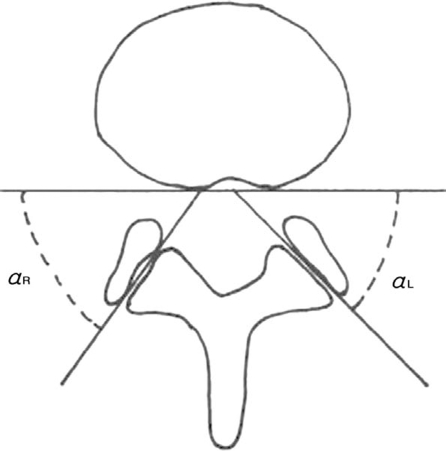
2. Facet orientation of L4-L5
Each facet joint angle was measured using axial T1WI, which was obtained parallel to the lower end plate at the L4-L5 intervertebral disc space. The right and left facet joint orientations in the coronal plane were then measured as the angle between the line drawn tangentially to the posterior wall of the vertebral body and the line drawn through the interarticular gap at the medial and lateral extremities of the facet joint (Fig. 2).
Fig. 2.
Each facet joint angle was measured using an axial T1-weighted image, which was scanned parallel to the lower end plate at the L4-L5 intervertebral disc space. The right and left facet joint orientations in the coronal plane were then measured as the angle between the line drawn tangentially to the posterior wall of the vertebral body and the line drawn through the interarticular gap at the medial and lateral extremities of the facet joint.
3. Facet osteoarthritis of L4-L5
Facet osteoarthritis was divided into four grades on axial T1WI using Fujiwara's criteria.12 Grade 1 indicated normal facet joints; Grade 2, joint space narrowing or mild osteophyte formation; Grade 3, sclerosis or moderate osteophyte formation; and Grade 4, marked osteophyte formation.
4. Disc degeneration of L4-L5
The degree of disc degeneration at L4-L5 was measured using sagittal T2WI, and degenerative status was classified into five grades according to the criteria of Frymoyer and Moskowitz13.
5. Statistical analysis
The independent sample T test and Mann-Whitney U test were used to determine the differences in the anterior slippage of L4 on L5, facet orientation of L4-L5, facet osteoarthritis of L4-L5, and disc degeneration of L4-L5. A p-value less than 0.05 was considered statistically significant.
Results
Independent sample T test showed no significant differences in the degree (% slip) of anterior slippage of L4 on L5 (17.02±6.21 versus 16.65±4.87, p=0.809) or facet orientation (degrees) of L4-L5 (54.99±12.18 versus 56.23±10.37, p=0.642) between patients with and without sacralization of L5, respectively.
The Mann-Whitney U test showed no significant differences in the grades of facet osteoarthritis (3.43±0.59 versus 3.53±0.37, p=0.527) or disc degeneration of L4-L5 (4.50±0.51 versus 4.35±0.61, p=0.340) between patients with and without L5 sacralization, respectively.
Discussion
L5 is linked to the sacrum by several types of articulation, and this leads to a relatively stable lumbosacral junction5. Therefore, sacralization of L5 leads to more stress concentration on the L4-L5 motion segment, which may result in further degenerative changes in the facet joint, disc degeneration, and anterior slippage of L4 on L5, similar to the motion segment immediately cephalad to a fusion4,14. Previous studies have reported an association between L5 sacralization and the development of degenerative disc disease in the lumbar spine6-11. L5 sacralization is also considered to be a predisposing factor for degenerative spondylolisthesis at L4-L55,12. However, there is no study looking at the radiological findings in degenerative spondylolisthesis at L4-L5 in patients with and without sacralization of L5.
In the current study, we found that the incidence of L5 sacralization was higher (54/78=69%) in patients with degenerative spondylolisthesis at L4-L5, a finding that is consistent with previous studies. However, contradictory to our expectation, there were no significant differences in the four radiographic parameters anterior slippage of L4 on L5, facet orientation of L4-L5, facet osteoarthritis of L4-L5, and disc degeneration of L4-L5 between patients with and without sacralization of L5. These findings suggest that L5 sacralization does not affect the radiological findings present in degenerative spondylolisthesis at L4-L5 without sacralization of L5. In other words, since degenerative changes in the facet joints and intervertebral disc are already far advanced in degenerative spondylolisthesis itself, the presence of sacralization does not have a significant additional effect on radiographic changes in degenerative spondylolisthesis.
There are several limitations to the current study. First, the number of cases included in this study was too small to draw definitive conclusions. Second, it is unclear whether advanced arthritic changes of the facet joints and the disc degeneration observed in degenerative spondylolisthesis are a cause of, or final result of, degenerative spondylolisthesis.
In conclusion, there were no significant differences in the anterior slippage of L4 on L5, facet orientation of L4-L5, facet osteoarthritis of L4-L5, or disc degeneration of L4-L5 between degenerative spondylolisthesis patients with and without sacralization of L5. These findings suggest that the influence of L5 sacralization on radiological findings in patients with degenerative spondylolisthesis at L4-L5 may be smaller than has been previously assumed. However, further study on a large patient group is needed to clarify the role of L5 sacralization in the development of degenerative spondylolisthesis at L4-L5.
References
- 1.Fitzgerald JA, Newman PH. Degenerative spondylolisthesis. J Bone Joint Surg Br. 1976;58:184–192. doi: 10.1302/0301-620X.58B2.932080. [DOI] [PubMed] [Google Scholar]
- 2.Rosenberg NJ. Degenerative spondylolisthesis. Predisposing factors. J Bone Joint Surg Am. 1975;57:467–474. [PubMed] [Google Scholar]
- 3.Cinotti G, Postacchini F, Fassari F, Urso S. Predisposing factors in degenerative spondylolisthesis. A radiographic and CT study. Int Orthop. 1997;21:337–342. doi: 10.1007/s002640050180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee CK, Langrana NA. Lumbosacral spinal fusion. A biomechanical study. Spine. 1984;9:574–581. doi: 10.1097/00007632-198409000-00007. [DOI] [PubMed] [Google Scholar]
- 5.Tini PG, Wieser C, Zinn WM. The transitional vertebra of the lumbosacral spine: its radiological classification, incidence, prevalence, and clinical significance. Rheumatol Rehabil. 1977;16:180–185. doi: 10.1093/rheumatology/16.3.180. [DOI] [PubMed] [Google Scholar]
- 6.Berlemann U, Jeszenszky DJ, Buhler DW, Harms J. The role of lumbar lordosis, vertebral end-plate inclination, disc height, and facet orientation in degenerative spondylolisthesis. J Spinal Disord. 1999;12:68–73. [PubMed] [Google Scholar]
- 7.Castellvi AE, Goldstein LA, Chan DP. Lumbosacral transitional vertebrae and their relationship with lumbar extradural defects. Spine. 1984;9:493–495. doi: 10.1097/00007632-198407000-00014. [DOI] [PubMed] [Google Scholar]
- 8.Elster AD. Bertolotti's syndrome revisited. Transitional vertebrae of the lumbar spine. Spine. 1989;14:1373–1377. [PubMed] [Google Scholar]
- 9.Magora A, Schwartz A. Relation between the low back pain syndrome and x-ray findings. 2 Transitional vertebra (mainly sacralization) Scand J Rehabil Med. 1978;10:135–145. [PubMed] [Google Scholar]
- 10.Otani K, Konno S, Kikuchi S. Lumbosacral transitional vertebrae and nerve-root symptoms. J Bone Joint Surg Br. 2001;83:1137–1140. doi: 10.1302/0301-620x.83b8.11736. [DOI] [PubMed] [Google Scholar]
- 11.Wigh RE, Anthony HF., Jr Transitional lumbosacral discs. Probability of herniation. Spine. 1981;6:168–171. doi: 10.1097/00007632-198103000-00011. [DOI] [PubMed] [Google Scholar]
- 12.Fujiwara A, Tamai K, Yamato M, et al. The relationship between facet joint osteoarthritis and disc degeneration of the lumbar spine: an MRI study. Eur Spine J. 1999;8:396–401. doi: 10.1007/s005860050193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Frymoyer JW, Moskowitz RW. Spinal degeneration. Pathogenesis and medical management. In: Frymoyer JW, editor. The adult spine principles and practice. 1st ed. New York: Raven Press Ltd; 1991. pp. 611–634. [Google Scholar]
- 14.Hambly MF, Wiltse LL, Raghavan N, Schneiderman G, Koenig C. The transition zone above a lumbosacral fusion. Spine. 1998;23:1785–1792. doi: 10.1097/00007632-199808150-00012. [DOI] [PubMed] [Google Scholar]