Abstract
Study Design
A retrospective study.
Purpose
To categorize the MR appearance of ischemic vertebral collapse and to correlate surgical and histologic findings.
Overview of Literature
X-ray and MRI findings of delayed posttraumatic vertebral collapse shows several patterns. Histopathologic signs of osteonecrosis were present only in minor portion of cases sampled for biopsy of delayed post-traumatic vertebral collapse in the literature.
Methods
Twenty-one patients (22 vertebral bodies), with surgically and histopathologically proven ischemic vertebral collapse were included. The patients were examined with a 1.5 T MR imager. Spin echo T1- and T2-weighted images were obtained in axial and sagittal planes. Two experienced musculoskeletal radiologists, who reached consensus, evaluated the MR images. Then, MR-pathology correlations were made.
Results
Four different MR patterns were identified. Fluid patterns, were seen in 14% (3/22) of the affected vertebral bodies, and were characterized by hypo-intense signals on T1-weighted images, and hyper-intense signals, similar to water, on T2-weighted images. Extensive bone necrosis was predominant. Compression pattern, the most common pattern, found in 41% (9/22 vertebral bodies), was characterized by a marked decrease of anterior column height. Bone necrosis, granulation tissue, marrow fibrosis, and reactive new bone formation were found in relatively equal proportion. Granulation pattern, seen in 27% (6/22 vertebral bodies), was characterized by hypo-intense signals on T1-weighted images, and intermediate signals on T2-weighted images. Extensive granulation tissue was predominant. Mixed patterns were present in 18% (4/22), of the vertebral bodies.
Conclusions
Awareness of histopathologic correlation of MR patterns in patients with delayed post-traumatic vertebral collapse may facilitate effective interpretation of clinical MR images of the spine.
Keywords: MR patterns, Delayed vertebral collapse, Pathology
Introduction
Kümmell's disease (delayed post-traumatic vertebral collapse) is a relatively uncommon entity1-5 and this condition is recognized as a form of vertebral osteonecrosis6,7 or as a varied type of non-union that differs from that of a long bone2.
The mechanism of the intra-vertebral vacuum phenomenon, which is considered virtually a pathognomonic radiographic finding of delayed post-traumatic vertebral collapse, is still unknown. The main hypothesis is the ischemic theory8. Maldague et al.3, since their original description, have stated that the presence of gas in the vertebral bodies implies the absence of fluid or blood at the fracture site, i.e., ischemia. However, there is currently no proof that ischemia or osteonecrosis serves as the major pathologic mechanisms of the intra-vertebral vacuum phenomenon8. The proposed absence of fluid in the vertebral cleft is contradicted by MR imaging, which clearly demonstrates the presence of a fluid-like collection associated with gas in the vertebral body4,8-10.
The vacuum phenomenon observed in degenerative disc disease is caused by the accumulation of gas, predominantly nitrogen11. Likewise, it is presumed that intra-osseous vacuum clefts result from the release of gas within cracks in the subchondral bone after a vertebral fracture3,12. The phenomenon probably represents an ununited vertebral fracture with possible formation of pseudoarthrosis12 and may be accentuated on the hyperextension stress views3,6,12.
Although the MR appearance of delayed post-traumatic vertebral collapse has been described as hypo-intense signal intensity on T1-weighted images and hyper-intense signal intensity on T2-weighted images2,4, we have found various MR appearances of this disorder, and to our knowledge, MR categorization of this condition has not been previously described. We expected that these different MR findings of each vertebral collapse can be matched with pathologic findings.
The purposes of this study were to categorize the MR appearance of delayed post-traumatic vertebral collapse and to correlate findings on MR imaging with pathologic examination.
Materials and Methods
Twenty-one patients (5 men and 16 women; age range, 54~77 years old; mean 66) with pathologically proven bone necrosis of the vertebral body were investigated. Two vertebral bodies were affected in one patient; thus, 22 vertebral bodies were evaluated.
All patients had no known malignancies or predisposing conditions for osteonecrosis, such as steroid treatment or radiation therapy. Nineteen of the 21 patients had histories of falling. Corpectomy of the affected vertebral body, and anterior and posterior instrumentation around the lesion were performed in all patients.
Anteroposterior and lateral radiographs of the thoracic and lumbar spines were obtained with the patients in the standing position. Sequential extension and flexion stress views were obtained in the lateral decubitus position.
The patients were examined with a 1.5 T-MR imager (Signa; General Electric Medical Systems, Milwaukee, WI, USA) in a supine position. Spin echo T1-weighted (350-700/10-40 [TR/TE]) and fast spin echo T2-weighted (2400-5000/70-120 [TR/TE]) images were obtained in the axial and sagittal planes. Field of view was 15~25 cm for axial scanning and 25~40 cm for sagittal scanning; and two signals were acquired. A 4-mm section thickness and a 1-mm section gap were used. The image matrix consisted of 512-256×256-128 elements. The intervals between the episodes of falling and the time of MR imaging, ranged from 1 month to 4 years (mean, 8.5 months).
Delayed post-traumatic vertebral collapse was present at L1 (n=10), T12 (n=9), T10 (n=1), T11 (n=1), and L4 (n=1) vertebral bodies (Figs. 1-4).
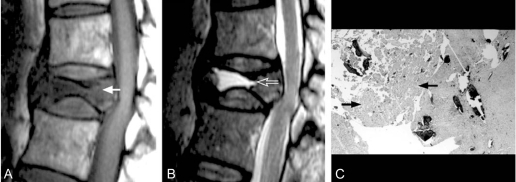
Fig. 1.
A 65-year-old woman with delayed post-traumatic vertebral collapse of T12 (pattern A, fluid pattern). (A) Spin echo T1-weighted (567/18) sagittal MR image shows a predominant area of hypo-intense signal intensity (arrow). (B) Fast spin echo T2-weighted (4,000/108) sagittal image obtained at the same level as in A shows a predominant area of hyper-intense signal intensity similar to water (arrow). (C) Corresponding photomicrograph of the specimen reveals extensive bone necrosis (arrows).
Fig. 4.
A 61-year-old woman with delayed post-traumatic vertebral collapse of L1 (pattern D, mixed pattern). (A) Spin echo T1-weighted (367/18) sagittal MR image shows an area (arrow) of hypo-intense signal intensity with a region of signal void (arrowhead). (B) Fast spin echo T2-weighted (2,400/105) sagittal image obtained at the same level as in A shows a region (arrow) of hyperintense signal intensity similar to water and an area of signal void (arrowhead). (C) Corresponding photomicrograph of the specimen reveals bone necrosis (curved arrow), reactive new bone (open arrow), and granulation tissue (straight solid arrow).
Two experienced musculoskeletal radiologists, who reached consensus, evaluated the MR images. MR patterns were categorized by predominant areas, which occupied more than 50% of the entire lesion of the affected vertebral body. Then, findings on pathologic examination were reviewed and MR-pathology correlations were made. All histologic slides were examined by two experienced musculoskeletal pathologists, who reached consensus, blinded to the MR imaging findings. However, we did not evaluate the interobserver variability for determining the MRI patterns and pathologic patterns. The consensus was reached by discussion between the two radiologists and pathologists.
Results
The intra-vertebral vacuum phenomenon was present in 64% (14/22) of the affected vertebral bodies (Fig. 2). Areas of signal void on MR images, which corresponded to the intra-vertebral vacuum, were present in 50% (7/14) of the affected vertebral bodies with intra-vertebral vacuum phenomenon detected on plain radiographs (Fig. 2B).
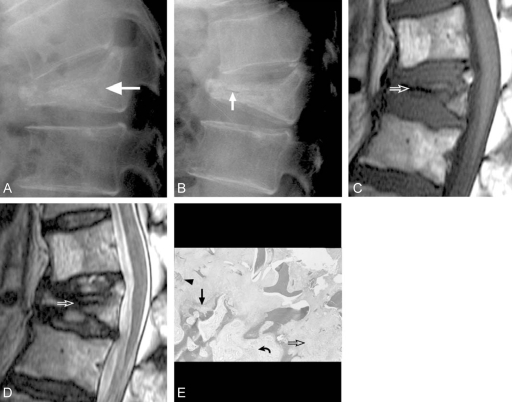
Fig. 2.
A 58-year-old woman with delayed post-traumatic vertebral collapse of L1 (pattern B, compression pattern). (A) Lateral radiograph in the lateral decubitus position with flexion stress shows a markedly compressed vertebral body (arrow) of L1 without an evident intra-vertebral vacuum cleft. Note the preservation of the height of the posterior wall of L1 body. (B) Lateral radiograph in the lateral decubitus position with hyperextension stress shows a linear intra-vertebral vacuum cleft (arrow). (C) Spin echo T1-weighted (500/10) sagittal MR image shows a markedly compressed vertebral body with a linear area of signal void (arrow). Note the preservation of the height of the posterior wall of L1 body. (D) Fast spin echo T2-weighted (4,200/120) sagittal image obtained at the same level as in C shows a markedly compressed vertebral body with a linear area of signal void (arrow). (E) Corresponding photomicrograph of the specimen reveals dead bone (arrowhead), marrow fibrosis (open arrow), reactive new bone formation (solid straight arrow), and granulation tissue formation (curved arrow).
With regard to the MR appearance, four different MR patterns were identified in patients with delayed post-traumatic vertebral collapse, and the findings on MR images reflected the findings on pathologic examinations (Figs. 1-4).
Pattern A (fluid pattern), seen in 14% (3/22) of the affected vertebral bodies, was characterized by a predominant area of hypo-intense signal intensity on T1-weighted images, and hyper-intense signal intensity, similar to water, on T2-weighted images (Fig. 1A and B). Extensive bone necrosis with resorption of dead bone was predominant on pathologic examination (Fig. 1C).
Pattern B (compression pattern), the most common pattern, found in 41% (9/22) of the affected vertebral bodies, was characterized by a marked decrease of anterior column height and a preservation of posterior wall height of the affected vertebral bodies (Fig. 2A and B). This pattern showed hypo-intense signal intensity on T1-weighted images, and intermediate signal intensity on T2-weighted images (Fig. 2C and D). Bone necrosis, granulation tissue formation, marrow fibrosis, and reactive new bone formation were found in a relatively equal proportion (Fig. 2E).
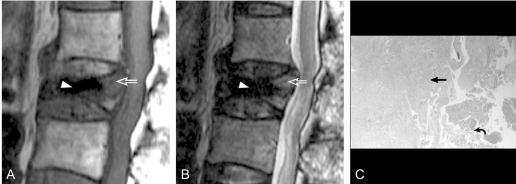
Pattern C (granulation pattern), seen in 27% (6/22) of the affected vertebral bodies, was characterized by predominant areas of hypo-intense signal intensity on T1-weighted images, and intermediate signal intensity on T2-weighted images (Fig. 3A and B). Extensive granulation tissue was predominant on pathologic examination (Fig. 3C).
Fig. 3.
A 68-year-old man with delayed post-traumatic vertebral collapse of L1 (pattern C, granulation pattern). (A) Spin echo T1-weighted (367/18) sagittal MR image shows a predominant area (arrow) of hypo-intense signal intensity with a region of signal void (arrowhead). (B) Fast spin echo T2-weighted (2,400/105) sagittal image obtained at the same level as in A shows an area (arrow) of intermediate signal intensity with a region of signal void (arrowhead). (C) Corresponding photomicrograph of the specimen reveals an extensive granulation tissue formation (straight arrow), and focal areas of bone necrosis (curved arrow).
Pattern B (compressesion type) showed thinner signal void and had a bone density at the posterior 1/3 of the vertebral body, however sometimes there was no signal void, while pattern C (granulation type) showed a wider and more prominent area of signal void and a wider area of the posterior portion of the vertebral body was composed of hypointense signal density in T1 and intermediate signal density in T2-weighted images. Simple X-ray findings also had some differences between patterns B and C. Pattern B showed much more compression anteriorly and a very thin hairy intarvertebral vacuum phenomenon in the extension stress view, while pattern C showed a more distinct vacuum phenomenon and the degree of anterior compression of the vertebral body was not as severe as pattern B. Intravertebral vacuum could not be confirmed easily in most cases of pattern B.
Pattern D (mixed pattern), seen in 18% (4/22) of the affected vertebral bodies, was characterized by coexistence of each pattern on the MR images (Fig. 4A and B). Pathologic examination also revealed mixed histologic findings of each pattern (Fig. 4C).
Pattern D has no predominant feature on MRI and pathology. It is composed of almost equal amount of fluid, dead bone, marrow fibrosis, granulation tissue and reactive new bone formation.
Discussion
Delayed post-traumatic vertebral collapse is rarely reported and has several postulated pathomechanisms, such as bone ischemia1-3,13,14. Although findings on the radiographs of an intra-vertebral vacuum cleft are considered virtually pathognomonic of this disorder3, the absence of a vacuum cleft does not exclude delayed post-traumatic vertebral collapse from the differential diagnosis15. Even though vertebral body fracture and collapse are readily seen on plain radiographs, identification of vertebral osteonecrosis is often more difficult.
Histopathologic signs of osteonecrosis were present only in minor portion of cases sampled for biopsy of delayed post-traumatic vertebral collapse in the literature3,8,16. New bone formation and marrow fibrosis, which are consistent with bone repair secondary to a fracture, were more commonly found than bone necrosis. Unlike the previous reports3,8,16, histopathologic signs of osteonecrosis were present in all patients in our study regardless of the extent of bone necrosis. The authors believe this to be related to the fact that corpectomies were performed on all patients of our series, allowing for more detailed pathologic analysis.
Our results showed that the MR patterns of delayed post-traumatic vertebral collapse could be categorized and that each pattern reflected the findings on pathologic examinations. Pattern A, fluid pattern, suggested extensive bone necrosis. Pattern B, compression type, was related to a relatively equal proportion of bone necrosis, granulation tissue formation, marrow fibrosis, and reactive new bone formation. Pattern C, granulation pattern, corresponded to extensive granulation tissue formation secondary to a fracture or osteonecrosis. Pattern D, mixed pattern on MR images, was found to have mixed features of each pattern on pathologic examinations. However, relationships between the MR patterns, the intervals between the episodes of trauma, and the time of MR imaging, could not be determined in our study, because the patients could not exactly recall the time of trauma, and the interval between the trauma and vertebral collapse varied among patients.
Naul et al.4 described a distinct MR appearance of delayed post-traumatic vertebral collapse such as; marked and discrete hyper-intensity on T2-weighted images, and hypo-intensity on T1-weighted images, at the location of the intra-vertebral cleft. Hasegawa et al.2 also noticed MR imaging findings of delayed post-traumatic vertebral collapse a low signal intensity on T1-weighted images and high signal intensity on T2-weighted images, suggesting a false joint lined by fibrocartilaginous tissue. This appearance would be concordant to pattern A in our series. However, various patterns of different pathologic features in our study, are more pronounced when compared to those of Naul et al.4 and Hasegawa et al.2 (Figs. 2-4).
Delayed post-traumatic vertebral collapse of pattern B (Fig. 2), C (Fig. 3), or D (Fig. 4) could be interpreted as a malignant tumor affecting the vertebral body, although that of pattern A (Fig. 1) in our study could be differentiated from tumor without difficulty. Howerver, it is not always difficult to differentiate osteoporotic vertebral collapse with metastatic fractures in the presence of fluid, air signal void and absence of soft tissue or epidural mass formation.
Malghem et al.10 found that the high signal intensity suggestive of water content seen on T2-weighted or T2*-weighted MR images gradually appeared and increased as the patient was maintained in a supine position for more than 20 minutes. For these authors, this phenomenon suggested a slow transudation in the cleft. Although we did not record the time between positioning of the patient in the supine position and the acquisition of MR imaging, MR imaging was performed in a usual fashion without intentional delay and MR sequences were performed in the same order in all cases. Therefore, we believe that the effect, derived from the changes in content of the vacuum cleft after supine positioning in our study, which may have influenced the MR imaging findings, would be nearly the same in all cases. Like the experience of Malghem et al.10, the areas of signal void on MR images, which corresponded to the intra-vertebral vacuum, were present in only 50% of the affected vertebral bodies with intra-vertebral vacuum phenomenon on plain radiographs in our study.
The present study has several potential limitations. First, the MR image interpretations, as well as the pathologic evaluations, were performed by consensus of two observers; therefore, inter-observer variability could not be determined. Second, a direct MR-pathology mapping could not be made. Third, biochemical analysis of the fluid within the gap could not be performed. Fourth, we did not check the enhanced MRI images for differentiation with other pathologies, such as metastasis and infection.
In summary, four distinct MR patterns, with regard to predominant pathologic areas, were identified in our study. And, awareness of histopathologic explanation of these MR patterns in patients with delayed post-traumatic vertebral collapse may facilitate effective interpretation of clinical MR images of the spine.
References
- 1.Brower AC, Downey EF., Jr Kummell disease: report of a case with serial radiographs. Radiology. 1981;141:363–364. doi: 10.1148/radiology.141.2.7291557. [DOI] [PubMed] [Google Scholar]
- 2.Hasegawa K, Homma T, Uchiyama S, Takahashi H. Vertebral pseudarthrosis in the osteoporotic spine. Spine. 1998;23:2201–2206. doi: 10.1097/00007632-199810150-00011. [DOI] [PubMed] [Google Scholar]
- 3.Maldague BE, Noel HM, Malghem JJ. The intravertebral vacuum cleft: a sign of ischemic vertebral collapse. Radiology. 1978;129:23–29. doi: 10.1148/129.1.23. [DOI] [PubMed] [Google Scholar]
- 4.Naul LG, Peet GJ, Maupin WB. Avascular necrosis of the vertebral body: MR imaging. Radiology. 1989;172:219–222. doi: 10.1148/radiology.172.1.2740507. [DOI] [PubMed] [Google Scholar]
- 5.Resnick D, Niwayama G, Guerra J, Jr, Vint V, Usselman J. Spinal vacuum phenomena: anatomical study and review. Radiology. 1981;139:341–348. doi: 10.1148/radiology.139.2.7220878. [DOI] [PubMed] [Google Scholar]
- 6.Bhalla S, Reinus WR. The linear intravertebral vacuum: a sign of benign vertebral collapse. AJR Am J Roentgenol. 1998;170:1563–1569. doi: 10.2214/ajr.170.6.9609175. [DOI] [PubMed] [Google Scholar]
- 7.Francois RJ, Eulderink F, Bywaters EG. Commented glossary for rheumatic spinal diseases, based on pathology. Ann Rheum Dis. 1995;54:615–625. doi: 10.1136/ard.54.8.615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lafforgue P, Chagnaud C, Daumen-Legre V, Daver L, Kasbarian M, Acquaviva PC. The intravertebral vacuum phenomenon ("vertebral osteonecrosis"). Migration of intradiscal gas in a fractured vertebral body? Spine. 1997;22:1885–1891. doi: 10.1097/00007632-199708150-00015. [DOI] [PubMed] [Google Scholar]
- 9.Chevalier X, Wrona N, Avouac B, Larget-Piet B. Thigh pain and multiple vertebral osteonecroses: value of magnetic resonance imaging. J Rheumatol. 1991;18:1627–1630. [PubMed] [Google Scholar]
- 10.Malghem J, Maldague B, Labaisse MA, et al. Intravertebral vacuum cleft: changes in content after supine positioning. Radiology. 1993;187:483–487. doi: 10.1148/radiology.187.2.8475295. [DOI] [PubMed] [Google Scholar]
- 11.Ford LT, Gilula LA, Murphy WA, Gado M. Analysis of gas in vacuum lumbar disc. AJR Am J Roentgenol. 1977;128:1056–1057. doi: 10.2214/ajr.128.6.1056. [DOI] [PubMed] [Google Scholar]
- 12.Kumpan W, Salomonowitz E, Seidl G, Wittich GR. The intravertebral vacuum phenomenon. Skeletal Radiol. 1986;15:444–447. doi: 10.1007/BF00355102. [DOI] [PubMed] [Google Scholar]
- 13.Nicholas JJ, Benedek TG, Reece GJ. Delayed traumatic vertebral body compression fracture; part I: clinical features. Semin Arthritis Rheum. 1981;10:264–270. doi: 10.1016/0049-0172(81)90003-2. [DOI] [PubMed] [Google Scholar]
- 14.Van Eenenaam DP, el-Khoury GY. Delayed post-traumatic vertebral collapse (Kummell's disease): case report with serial radiographs, computed tomographic scans, and bone scans. Spine. 1993;18:1236–1241. [PubMed] [Google Scholar]
- 15.Chou LH, Knight RQ. Idiopathic avascular necrosis of a vertebral body. Case report and literature review. Spine. 1997;22:1928–1932. doi: 10.1097/00007632-199708150-00024. [DOI] [PubMed] [Google Scholar]
- 16.Feldmann JL, Alcalay M, Queinnec JY, de Bray JM. Spinal cord compression related to vertebral osteonecrosis. Clin Exp Rheumatol. 1988;6:297–300. [PubMed] [Google Scholar]