Abstract
Background
Remaining at home is a high priority for many older adults, but the capacity to “age in place” often is threatened by environmental barriers.
Purpose
To describe a client-centered occupational therapy, home modification intervention program and examine the impact of the intervention on daily activity performance over time.
Methods
Using a competence-environmental press framework, a client-centered home modification program for older adults was implemented. In this quasi-experimental, single group prospective study, participants’ subjective ratings of daily activity performance were evaluated before and after the intervention (baseline/post/post).
Findings
After home modification, participants’ perception of their daily activity performance at home improved significantly and was maintained 2 years post-modification.
Implications
Home modification may benefit older adults attempting to age in place.
Keywords: Aging, Home environment, Environmental modifications, Competence-environmental press framework
Older adults prefer to live out their later years in their own homes (American Association of Retired Persons [AARP], 2000). Strong emotional ties to their homes make forced moves a devastating event for many older adults (Carpenter et al., 2007; Fogel, 1992). At the same time, many older adults experience physical and cognitive frailty with deleterious effects on performance of daily activities (Fried & Guralnik, 1997; Gill, Williams, & Tinetti, 1995; Iwarsson, Nygren, Oswald, Wahl, & Tomsone, 2006). Frail older adults are vulnerable to the demands of the physical environment, which can result in excess (i.e., preventable) disability (Iwarsson & Isacsson, 1998; Iwarsson et al., 2006; Mann, Hurren, Tomita, Bengali, & Steinfeld, 1994; Oswald, Wahl, Schilling, & Iwarsson, 2007; Oswald, Wahl, Schilling, Nygren, et al., 2007; Stark, 2001; Steinfeld & Shea, 1993). Examples of environmental barriers include items located out of reach, controls or knobs that are difficult to grip and twist, and stairs (Mann et al.; Stark; Steinfeld & Shea). Older adults are willing to accept home modifications (Trickey, Maltais, Gosselin, & Robitalle, 1993), and some form of modifications occur in an estimated 38% of homes of older adults with disabilities (U.S. Department of Housing and Urban Development, 2001). Few studies, however, have systematically evaluated the effectiveness of home modifications in reducing excess disability or improving daily activity performance of older adults (Fange & Iwarsson, 2007).
Gitlin and colleagues reported that home modification slowed the rate of functional dependency, enhanced caregiver self-efficacy, and decreased mortality among frail older adults (1993, 2001, 2006). Mann, Ottenbacher, Fraas, Tomita, and Granger (1999) reported that home modification and assistive technologies reduced functional dependency in older adults and costs for personal assistance and healthcare. These studies suggest that older adults may benefit from environmental modifications but do not address the effect, if any, of a client-centered intervention on the outcome of daily activity performance.
Client-centeredness refers to a treatment approach that recognizes client preferences in treatment decisions (Law, Baptiste, & Mills, 1995; Oswald et al., 2007.) Client-centered occupational therapy has been associated with improved treatment outcomes (Law, 1998). Not surprisingly, adherence rates as low as 33–40% have been reported in home modification intervention studies that did not report using a client-centered approach (Cumming et al., 2001; Devor, Wang, Renvall, Feigal, & Ramsdell, 1994; Schoenfelder & Van Why, 1997). Homes hold great meaning for many older adults (Dovey, 1985), who may resist modifications they perceive as unattractive or cumbersome. Compliance with treatment might be enhanced if older adults are able to exert control over their home environments by making the final decision about the type of home modification implemented (Clemson, Cusick, & Fozzard, 1999).
There are variations in the intensity and type of environmental support provided during investigations of home modifications, making comparisons across studies difficult. Some studies focus only on standard safety modifications, such as removing throw rugs or adding grab bars (Cumming et al., 1999), others include structural changes to the home as well as assistive technology (Hammel, 2000; Mann et al., 1999), and still others focus only on assistive technology (Mann, Hurren, Tomita, & Charvat, 1995). A well-defined protocol for intervention is needed to define best practices in home modification (Gitlin et al., 2003). Our approach to providing home modifications employed a global approach to solving environmental problems. We used a combination of architectural modifications and adaptive equipment, believing this approach would provide participants with the broadest range of options and would most closely approximate how occupational therapists practice.
The primary aim of this preliminary study was to describe a client-centered occupational therapy, home modification intervention program and examine the impact of the intervention on daily activity performance over time. Costs associated with the intervention were also examined. The intervention used Lawton’s ecological model (Lawton & Nahemow, 1973) as a foundation and was designed to reduce the environmental press posed by environmental barriers in the homes of older adults. Consistent with a client-centered approach, the primary outcome of this study was the clients’ subjective perception of their performance.
Methods
We used a quasi-experimental design to conduct a single group (n=80) pre/post/post prospective study over a period of two years (Portney & Watkins, 2008).
Site
The study was conducted in a suburban naturally occurring retirement community (NORC) in the St. Louis metropolitan area. A NORC is defined as a building, neighborhood, or community in which a disproportionally large number of older adults live (Hunt, 1988). NORCs are not planned communities, but emerge naturally as individuals age in place or migrate to live close to peers or social services. An estimated 27% of older adults live in NORCs (AARP, 1992). Although NORCs vary by demographic and ownership characteristics (Callahan & Lanspery, 1997), they offer an opportunity to study interventions in communities that match imminent projected population rates of older adults. The St. Louis NORC is a geographically defined community of approximately one square mile, with 4,641 residents, of whom 32% (1,487) are age 65 or older (Missouri Census Data Center, 2002).
Participants
Between January and August of 2003, a convenience sample of 317 older adults volunteered to participate in a cross-sectional study to identify their needs for health and social services (Carpenter et al., 2007). Volunteers were recruited through neighborhood meetings, flyers, community newsletters, and word of mouth. All participants were screened by telephone prior to study enrollment. Participants were included if they were age 60 or older and if they lived within the geographic boundaries of the NORC. Exclusion criteria included a score of 10 or greater on the telephone version of the Short Blessed Memory Orientation and Concentration Test (Katzman et al., 1983) as these individuals were considered unable to provide informed consent. The needs assessment as well as all phases of the present study were reviewed and approved by the Washington University Institutional Review Board. All study participants were living independently in the community at the time of the assessment. All participants were interviewed in their homes.
During the needs assessment (Carpenter et al., 2007), we screened for potential home modification study participants by asking residents if they had difficulty or were worried about their ability to do their daily activities in their homes. When participants answered yes, the study staff then contacted them by phone. Individuals who reported difficulty performing daily activities as measured by scores of 6 or less on two or more activities on the telephone version of the Functional Impairment Measure ([FIM]; Petrella, Overend, & Chesworth, 2002) were invited to participate in the home modification study. A rolling enrollment of 80 volunteers agreed to participate.
All volunteers who met inclusion criteria and were invited agreed to participate in the study. However, attrition occurred in the sample at each data collection point. Of the 80 subjects enrolled, 77 completed the pretest at baseline, 67 participated in the three-month post-intervention assessment and 37 participated in a two-year follow up. The three participants who did not complete the pretest at baseline decided to move out of the NORC. Eight more participants did not complete the first posttest for reasons that included moving, severe mental health issues, death, and family crisis. Two participants who did complete the first posttest were excluded from analysis. The first individual exhibited significantly decreased cognition (score of 16 on Short-Blessed Memory Test [Katzman et al., 1983]); the second was excluded when it was discovered she was 57 years of age. Thus, a group of 67 individuals participated in the first posttest analysis. Thirty of these individuals did not participate in the two-year follow up (second posttest); 13 had moved, 8 were deceased, and 9 were lost to follow up. We compared the participants from the first post test (N=67) to the remaining 37 participants on their baseline scores for key demographic variables. There were no significant differences between the two groups except for gender. A greater proportion of females than males were available for the two-year follow up.
Baseline characteristics of participants are shown in Table 1. The mean age of the sample was 81.7 years (range 61–95 years). Of the initial 67 participants included in the analyses, 88% were female, 90.7 % were white, and 66.7% were widowed. Most of the participants had completed high school and some college. Approximately 75% lived in a condominium, and nearly 90% reported using a mobility device such as a cane, walker, or wheelchair. Most (73.3%) lived alone.
Table 1.
Characteristics of participants enrolled in the study (N=67).
| Sample characteristic | Percentage of sample |
|---|---|
| Gender | |
| Female | 88.0 |
| Age, mean years (SD) | 81.7 (6.0) |
| Ethnicity | |
| White | 90.7 |
| Black | 6.7 |
| Asian | 1.3 |
| Russian | 1.3 |
| Marital status | |
| Never married | 5.3 |
| Currently married | 18.7 |
| Divorced | 9.3 |
| Widowed | 66.7 |
| Lives alone | 73.3 |
| Type of housing | |
| Single family | 12.0 |
| Condominium | 76.0 |
| Apartment | 12.0 |
| Device use | |
| Cane | 50.7 |
| Walker | 32.0 |
| Wheelchair | 6.7 |
Measures
In a previous pilot study of home modifications (Stark, 2004), when older adults gave up an activity due to an environmental barrier, they no longer identified the activity as a potential target for intervention (e.g., if the washing machine was in the basement and they could not navigate the stairs, they did not identify this activity as problematic, even if laundry was an important activity). This led to problems using our proposed primary endpoint, the Canadian Occupational Performance Measure (COPM; Law et al., 1994), for the current study as the participants often omitted these important or meaningful activities during the assessment. This problem has been attributed to older adults’ lack of awareness of the potential benefits of home modification (Pynoos, 1993). To address this problem, we employed a method previously successful in measuring the activity patterns of older adults (Baum & Edwards, 2001; Everard, Lach, Fisher, & Baum, 2000) that inventories current and desired activity patterns using photographic images as visual cues. We adapted the COPM ratings of performance and satisfaction and added the objective measurement of person-environment fit. This new multi-step assessment procedure, summarized in Table 2, was used to establish current activity patterns, identify activities that were difficult but important to the older adult, and identify the environmental barriers that influenced that activity (person-environment fit). Although presented elsewhere (Stark, Somerville, & Morris, in press), the instrument is briefly described in the next paragraph.
Table 2.
Administration and scoring of the activity and performance measures.
| Measure | Definition | Metric | Data source | Formula/Scale |
|---|---|---|---|---|
| Proportion of activity | Sum of activity difficulty scores/number of activities individual wants or needs to do | Subjective | Sort of 38 photographs depicting activities in the home | a Difficult activity proportion = difficult(.5) + unable(0)+ able(1)/difficult +unable+ able |
| Performance of activity | The individuals perception of their performance of a meaningful activity | Subjective | Rating of 5–10 problems identified by participant | Mean calculated on Likert-type scale 1= “not able to do it”; 10 “able to do it extremely well” |
| Satisfaction with performance | The individuals satisfaction of their ability to perform an activity | Subjective | Rating of 5–10 problems identified by participant | Mean calculated on Likert-type scale: 1= “not satisfied at all”; 10= “extremely satisfied” |
| Magnitude of environmental barriers influence | The person-environment fit | Objective | Observation of 5–10 problems performed in the current environment | Sum calculated on performance based scale: 5=no activity (completely unable); 1=standby assist or safety risk |
Difficult, unable, and able are the sum of cards in each pile from the card sort.
To create the new activity inventory, we developed a unique set of 38 photographs depicting activities performed in the home. The photographs served as cues to assist older adults to recall their activity performance. The activities were derived from a previously conducted survey, a review of clinical records of a home modification treatment program, and the pilot study (Stark, 2004). The items represented basic activities of daily living (ADLs), such as taking a shower or using the toilet; instrumental activities of daily living (IADLs), such as preparing a meal or caring for children; and leisure activities, such as reading or visiting with friends.
As a first step, a sort technique (Cordingly, Webb, & Hiller, 1997; Valenta & Wigger, 1997) was used to identify and score current activity patterns. The activity cards were sorted into four categories: 1 = “I do not do and don’t want to do,” 2 = “I do now with no problem,” 3 = “I do now with difficulty,” and 4 = “I do not do but wish to do.” Participants were asked to identify any other daily activities in the home that were not represented on the cards. These items were included during the second step of the assessment but were not included in the final activity score calculation. For the activity score, we followed the approach used by the Activity Card Sort (Baum & Edwards, 2001; Everard et al., 2000). The score calculated is a proportion of difficult activities divided by the total number of activities that the individual needs or wants to do. The total number of activities (termed the based activity score) was computed by first assigning a score of 1 to each “do now,” “do with difficulty,” or “unable to do.” card from the sort. The base activity score was computed as a sum of these scores. Next, a difficulty with activity score was calculated by assigning a value of 0 to those they “do not do but wish to do,” 0.5 to those they “do with difficulty,” and 1 to activities that posed “no problem.” The difficulty with activity score is a sum of these scores. The final activity performance score was calculated as a proportion of the difficulty with activity score divided by the base activity score. Activities that participants “do not do and do not wish to do” were not included in the calculation, eliminating a penalty for individuals who participate in fewer activities. The formula for calculating this score is provided in Table 2. Cronbach’s alpha on all 38 activities for the activity sort was .90 for this sample.
The next step in the process was to focus on the subset of activities from categories 3 (I do now with difficulty) and 4 (I do not do but wish to do). The participant ranked the problematic activities from most to least important. The problems ranked as most important (up to 10) were selected for treatment and rated by the participant. An un-weighted goal attainment scaling approach (Stolee, Zaza, Pedlar, & Myers, 1999) was employed to measure subjective performance and satisfaction with performance. The COPM anchor points of 1 “not able to do it” and 10 “able to do it extremely well” were used to rate performance, and 1 “not satisfied at all” and 10 “extremely satisfied” were used for satisfaction (Law et al., 1994). Cronbach’s alpha for the goal attainment scale adapted from the COPM was .93 in this sample.
The strength of a barriers influence on performance is a more meaningful measure of person-environment fit than number of barriers in the home Oswald et al., 2007.). To quantify a mismatch between the environment’s demand character and a participant’s performance, an occupational therapist observed the participant performing the activity. Based on this observation, the therapist identified and rated the influence of the barrier on the performance (Chandler, Duncan, Weiner, & Studenski, 2001; Steinfeld & Danford, 1997). The instrument is scaled to measure whether the barrier resulted in 5 (no activity), 4 (total dependency on another to complete the task), 3 (moderate assistance needed), 2 (minimal assistance needed), 1 (stand by assistance needed or safety risk), and 0 (the client was independent with or without a device). The scores were summed to calculate the total barrier severity influencing participation in the home. Cronbach’s alpha for the severity of barrier influence index was .76 in this sample. Thus, four subscores were derived from the assessment: an activity performance score from the sort, a performance score and satisfaction score from the rating session, and a severity of environmental barrier score, or measure of person-environment from the performance-based assessment.
Because the intervention was based on a competence-press framework, competence was ascertained using socio-demographic characteristics and screenings of basic abilities using a battery of valid and reliable measures. The assessments and the time they were administered are presented in Table 3. We assessed visual acuity using the Lighthouse Near Acuity Vision test (Elam, 1997); mobility or the ability to rise from a chair, walk 15 feet and return, was ascertained using the Get up and Go test (Mathias, Nayak, & Isaacs, 1986). Cognition was evaluated using the Short Blessed Memory Test (Katzman et al, 1983). Strength and range of motion of the upper extremity were assessed using group muscle tests and goniometry and scored as within normal limits, within functional limits, or impaired (Radomski & Trombly Latham, 2008). Hearing impairment was assessed using a combination of high- and low-pitched sounds. Persons were asked to repeat the sounds “sa, se, si, so, su” while the examiner blocked the view of her lips. Each sound repeated correctly was assigned a score of 1. A score of 4 or less indicated a functional impairment (Edwards et al., 2006). The FIM was used to measure function in the motor and cognitive domains (Keith, Granger, Hamilton, & Sherwin, 1987).
Table 3.
Administration of assessments.
| Measures | Baseline | Post 1 (3 months) | Post 2 (2 years) |
|---|---|---|---|
| Covariates | |||
| Visual acuity (Lighthouse Near Visual Acuity) | x | x | |
| Mobility (Get up and Go) | x | x | |
| Memory (Short Blessed Test) | x | x | |
| Strength (Manual Muscle Testing) | x | x | |
| Range of motion (Goniometry) | x | x | |
| Hearing (Sound Repetition) | x | x | |
| Outcome Measures | |||
| Motor and cognitive function (FIM) | x | x | x |
| Activity performance (Card sort) | x | ||
| Performance and satisfaction (Self-rated) | x | x | x |
| Severity of environmental barrier (Performance) | x | x | x |
The entire assessment battery was completed at baseline (pretest). All measures except the activity subscale (which was used only for developing the treatment plan) were repeated at the first posttest, three months after the installation of home modifications. At the two-year follow up, only the primary outcomes of performance, satisfaction with performance, person-environment fit, and the FIM were repeated (see Table 3).
Intervention
The intervention was guided by two important concepts. First, treatment plans were developed based on the competence-environmental press framework, which posits that a mismatch between ability and environmental press results in maladaptive performance outcomes (Lawton & Nahemow, 1973). The home modification intervention was designed to enhance the fit between the older adult with functional limitations and his or her home environment by reducing the influence of environmental barriers. The home modification intervention was also based on client-centered treatment principles. The participants underwent a structured assessment process to identify and rank performance problems according to importance. The participants also reviewed and approved the intervention strategies implemented.
The occupational therapist who provided the intervention for this study was a licensed practitioner with two years of experience in community-based care. A level II fieldwork student assisted her for the duration of the project. The occupational therapist and student were trained by the principal investigator (PI) in home modification approaches. To ensure treatment fidelity (Resnick et al., 2005), the occupational therapist was monitored by the PI throughout the study via weekly case reviews that included evaluation of treatment plans and on-site observation.
visited potential participants initially give them verbal and written information regarding the study and to obtain informed consent. The baseline measures were conducted over two visits to ease the burden of assessment. All barriers identified during assessment were documented with photographs.
The intervention was implemented by a team that included the participant, a construction company, family members (if requested by participant), and the occupational therapist. Examples of common problems that the participants identified included difficulty using the toilet and shower and difficulty reaching items. The intervention included a range of typical home modification strategies (Pynoos, 1993), such as adaptive equipment (e.g., tub bench), architectural modifications (e.g., ramp), major home renovations (e.g., roll-in shower), and training in using the compensatory supports and strategies during daily activities. The plan was based on the therapist’s observation of the participant performing the activity. First, the barrier was identified and discussed with the participant. Next, a plan for removing the barrier was developed in consultation with the participant and team members. Client-centeredness was preserved by giving the participant choices for removing barriers. For each barrier identified, up to three home modification solutions were presented and discussed using drawings or photos. The client could then choose the solution most appealing to him or her. For example, one participant reported difficulty using the toilet. This individual was observed performing the task in her current environment. The therapist noted the barrier to performance was that the toilet seat was 15 inches—too low for her transfer. The solutions for this participant were designed to elevate the height of the toilet. The therapist consulted with the contractor regarding options for increasing the height of the toilet and then presented the options to the participant. During negotiation with the participant, the barrier to performance was first discussed (the therapist explained the transfer was difficult because the toilet height was too low). The three solutions and their relative benefits were then presented to the client. The solutions included (1) a new toilet that was 19 inches in height, (2) a raised toilet seat, or (3) a spacer between the floor and toilet base that raised the toilet to a height of 19 inches. In this case, the participant chose a raised toilet seat so she could take the device with her when she traveled. The participants also had the option of refusing the modifications. If this occurred and if it was possible, additional alternative modifications were identified. If the solutions were still not palatable to the participant, the problem was documented as no intervention provided.
For all architectural modifications, a construction company whose personnel were trained by the PI on barrier-free design performed all installations. The most common modifications provided included grab bars, handrails, additional lighting, and reacher devices. Less common modifications included providing ramps to enter the home and replacing bathtubs with walk-in showers. All home modifications were provided at no cost to the participant. After the home modifications were installed, participants practiced each activity under the supervision of the occupational therapist until performance was satisfactory to the participant and deemed safe by the occupational therapist. The total number of occupational therapy visits ranged from 3 to 10 (M=5). The average installation time for the modifications and training was 39 days. Cost of equipment, labor, and materials related to home modifications were documented.
Three months after modifications were completed, the same occupational therapist re-administered the posttest assessment battery (see Table 3). The three-month period was given to permit the participant time to become accustomed to the new environmental supports. At this posttest visit, the barrier status was noted and photographs of the modifications were taken to verify that the changes had been made.
Two years after the final treatment visit, at the request of the NORC leaders, each participant was contacted to participate in a follow-up two-year posttest to evaluate the intervention. A subsample of 37 of the original participants was visited in their homes. During this visit, participants were re-consented. Only the study endpoint measures were repeated.
Data analysis
Descriptive statistics were calculated for all study variables. Comparisons of the physical and cognitive changes in the sample were made from the baseline to the first posttest (3 months) using t tests for paired comparisons. We examined the main effect of the intervention on daily activity performance, satisfaction, person-environment fit, and the FIM using a repeated measures analysis of variance. For the subset that completed the second posttest (2-year follow up, n=37), a repeated measures analyses of variance was used to examine the time for each outcome variable (performance, satisfaction, FIM, and magnitudes of environmental barrier). Effect sizes were estimated with partial eta square. Single degree of freedom, repeated contrasts of baseline, first post-, and second posttest scores were computed if the main effect for measurement time was significant (Tabachnick & Fidell, 1989). We conducted all analyses using SPSS version 15.0.
Findings
The participants (N=67) identified 719 activities they had difficulty completing and 100 activities they had given up. Table 4 presents the types of problems that participants identified in their current homes. Participants agreed to address 257 of those problems as part of this study. We were able to address an average of 3.9 problems per participant (range 1–7).
Table 4.
Frequency of Activity Problems Reported by Older Adults (N=67).
| Have difficulty performing activity | Unable to perform activity | |||
|---|---|---|---|---|
| Activity | Frequency | % | Frequency | % |
| Reaching for things up high | 51 | 68.9 | 2 | 2.7 |
| Taking a bath/shower | 46 | 62.2 | 1 | 1.4 |
| Getting up from chair/sofa | 44 | 59.5 | 30 | 40.5 |
| Going up/down stairs | 40 | 54.1 | 6 | 8.1 |
| Picking something up off floor | 39 | 52.7 | 2 | 2.7 |
| Caring items | 34 | 45.9 | 1 | 1.4 |
| Opening jars | 34 | 45.9 | 1 | 1.4 |
| Sleeping | 30 | 40.5 | 1 | 1.4 |
| Reading | 28 | 37.8 | 1 | 1.4 |
| Cleaning living area | 27 | 36.5 | 2 | 2.7 |
| Getting dressed | 27 | 36.5 | 0 | 0.0 |
| Getting in/out of entrance doors | 26 | 35.1 | 1 | 1.4 |
| Getting in/out of the cara | 25 | 33.8 | 0 | 0.0 |
| Writing | 24 | 32.4 | 1 | 1.4 |
| Getting on/off toilet | 23 | 31.1 | 0 | 0.0 |
| Getting in/out of bed | 21 | 28.4 | 1 | 1.4 |
| Talking on the phone | 18 | 24.3 | 0 | 0.0 |
| Opening/closing doors | 16 | 21.6 | 1 | 1.4 |
| Repairing clothing | 17 | 23.0 | 7 | 9.5 |
| Washing and drying clothes | 17 | 23.0 | 4 | 5.4 |
| Preparing a meal | 13 | 17.6 | 2 | 2.7 |
| Paying the bills | 12 | 16.2 | 1 | 1.4 |
| Moving around in the home | 12 | 16.2 | 0 | 0.0 |
| Getting the mail | 11 | 14.9 | 1 | 1.4 |
| Controlling the environment | 11 | 14.9 | 0 | 0.0 |
| Ironing clothes | 9 | 12.2 | 2 | 2.7 |
| Taking out the trash | 9 | 12.2 | 4 | 5.4 |
| Responding to an emergency | 9 | 12.2 | 2 | 2.7 |
| Answering door or phonea | 8 | 10.8 | 0 | 0.0 |
| Repairing household objects | 7 | 9.5 | 9 | 12.2 |
| Taking medication | 6 | 8.1 | 0 | 0.0 |
| Grooming | 6 | 8.1 | 0 | 0.0 |
| Watching TV | 4 | 5.4 | 0 | 0.0 |
| Caring for pets | 3 | 4.1 | 5 | 6.8 |
| Listening to music/radio | 3 | 4.1 | 4 | 5.4 |
| Washing dishes | 3 | 4.1 | 1 | 1.4 |
| Visiting with family and friends | 2 | 2.7 | 3 | 4.1 |
| Eating | 2 | 2.7 | 0 | 0.0 |
| Caring for children | 1 | 1.4 | 3 | 4.1 |
| Resting | 1 | 1.4 | 1 | 1.4 |
| Total | 719 | 100.0 | 100 | 100.0 |
Activities not included in the activity card sort that were identified as problematic by participants.
We considered the proportion of modifications adopted at the first posttest to those recommended by the occupational therapists as the level of adherence (Cumming et al., 2001). Approximately 80% of the modifications recommended by the therapist were adopted, suggesting adequate adherence to the protocol for detecting a treatment effect. The total number of modifications for the sample was 267. The average cost of the intervention was approximately US$635 (range US$50–US$4,000 dollars) per participant or US$159 per problem. The majority of the sample received modifications ranging in cost from 0–US$500 with 14% receiving modifications that cost between US$500 and $999. About 10% received modifications that cost US$1,000 or more. The types and frequencies of a sample of most frequently prescribed modifications are reported in Table 5.
Table 5.
Frequency and Cost of Most Common Modifications.
| Modification | Frequency | Average Cost |
|---|---|---|
| Grab bar | 44 | $148 |
| Shower seat | 14 | $45 |
| Hand held shower | 11 | $58 |
| Floor Lamp | 18 | $67 |
| Desk Lamp | 20 | $37 |
| Reacher | 39 | $23 |
| Amplified cordless phone | 10 | $134 |
Note. N=67. Total number of modifications (N=257).
Costs presented in U.S. 2003 dollars.
Comparisons of the physical and cognitive changes in the sample were made from the baseline to the first posttest (3 months) using t tests for paired comparisons. There were no measurable physical or cognitive changes in the sample (see Table 6).
Table 6.
Within Group Pre to Post Test Scores for Key Functional Characteristics.
| Pre | Post | |||
|---|---|---|---|---|
| M | SD | M | SD | |
| Get up and Go test (mobility)a | 19.0 | 39.0 | 20.0 | 40.0 |
| Short Blessed (cognition)b | 2.7 | 3.3 | 2.4 | 2.5 |
| Visual acuityc | 49.4 | 11.4 | 50.9 | 8.7 |
| Auditiond | 0.5 | 0.5 | 0.6 | 0.5 |
| Upper extremity strengthe | 1.1 | 0.3 | 1.1 | 0.3 |
| Upper extremity range of motione | 1.2 | 0.4 | 1.3 | 0.5 |
Note. N=67. No significant differences detected between pre and posttesting using t tests for paired comparisons.
seconds, >30 indicates impairment.
score >7 indicates probable cognitive impairment.
score ≤ 49 indicates visual acuity problems;.
number correct/5.
scored 0=within normal limits, 1=within functional limits; 2=below functional limits.
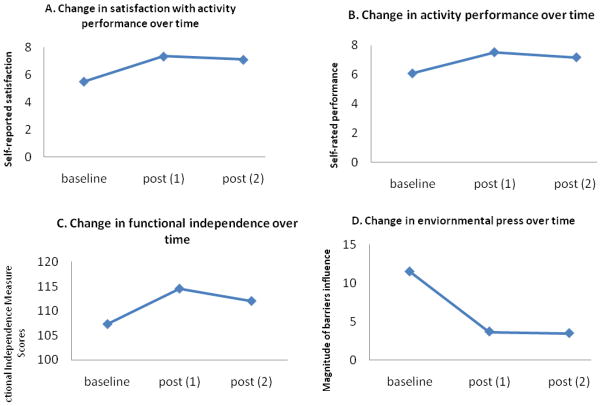
For satisfaction with performance, the contrasts indicated there was a significant increase in scores from baseline (M = 5.5, SD = 2.01) to the immediate posttest (M = 7.4, SD = 1.9, F(1, 36) = 55.5, p < .0001). This treatment effect accounted for 61% of the variability in the scores. There was a decrease from the first posttest to the two-year follow-up (M = 7.1 SD = 2.1, F(1, 36) = 6.22, p < .017).
For performance, the contrasts indicate that there was a significant increase in scores from baseline (M = 6.1, SD = 1.6) to the immediate posttest (M = 7.5, SD = 1.6, F(1, 36) = 36.8, p < .0001). This treatment effect accounted for 50% of the variability in the scores. There was no change from the first posttest to the two-year follow up (M = 7.2 SD = 1.6, F(1, 36) = 1.2, p = .27).
For functional independence, as measured by the total FIM score, contrasts indicated that there was a significant increase in scores from baseline (M = 107.4, SD = 7.9) to the immediate posttest (M = 114.5, SD = 5.8, F(1, 36) = 79.5, p < .0001). This treatment effect accounted for 50% of the variability in the scores. There was no change from the first posttest to the two-year follow up (M = 112.0 SD = 7.65, F(1, 36) = 1.7, p = .20).
For the magnitude of the influence of the environment or person-environment fit, contrasts indicated that there was a significant decrease in the scores from baseline (M = 11.5, SD = 5.2) to the immediate posttest (M = 3.7, SD = 3.0, F(1,36) = 104.0, p <.0001). There was a further decline in the scores (indicating fewer barriers) from the first posttest to the second posttest two years later (M = 3.4, SD = 3.9, F(1,36) = 35.8, p <.0001). These data are summarized in Figure 1.
Figure 1.
Change in self-rated satisfaction with performance over two years (A). Change in self-rated performance over two years (B). Change in Functional Independence Measure scores over two years (C). Change in environmental press over two years (D).
Note. n=37GLM with contrasts all significant at p<.0001 for baseline to post 1. No significant differences between post 1and post 2 for B, C. A statistically significant decrease was observed from post 1 to post 2 for satisfaction (A) and environmental press (D). Charts A & B represent self-reported performance. Charts C&D represent performance based assessments by occupational therapist.
Discussion
This client-centered home modification program targeted community-dwelling older adults with functional limitations and daily activity performance problems. The intervention aimed to compensate for the participants’ functional limitations by reducing the environmental press they experienced during everyday tasks. The preliminary findings suggest this approach had a positive impact on performance of daily activities. Activity performance measured subjectively (self-rated performance) and FIM scores improved and were maintained for two years post-intervention. Satisfaction with performance improved significantly immediately post-intervention, but waned over two years. The initial changes in performance could be attributed to the intervention because there were no significant changes in abilities (e.g., cognition, mobility) from baseline to the first (3-month) posttest.
The findings appear to support Lawton’s Ecological Model (Lawton & Nahemow, 1973) which theoretically describes the relationship between older persons and their environments. The Ecological model operationalizes activity performance as an outcome of the interaction between an individual’s abilities and the press of the environment (Iwarsson, 2005). This study describes an intervention that focused on reducing environmental press. At the first follow up (3 months), environmental press as measured by the magnitude of the barriers’ influence was reduced and self-rated performance was improved. Functional abilities (visual acuity, strength, cognition) did not change.
The results of this study reinforce the growing body of evidence that demonstrates environmental modifications have a positive impact on functional outcomes (Gitlin et al., 2001; Gitlin et al., 2003; Mann et al., 1999). This study offers new preliminary evidence that a client-centered home modification intervention supports activity performance for a period of two years. The strengths of this preliminary study include the use of a client-centered approach during a home modification intervention. This method appears successful as evidenced by the high adherence rates (Cumming et al., 2001; Devor et al., 1994; Schoenfelder & Van Why, 1997). The description of how client centeredness was operationalized during the occupational therapy process is also important for practitioners. The findings of this study suggest that home modification interventions might produce long-term benefits, a finding that deserves further study in future trials.
There are several limitations to this preliminary study that encourage caution when interpreting the results. The study was conducted with a relatively small sample and did not include a control group. Functional abilities such as strength and vision, while not likely to improve in this population, were only measured at baseline and at the first posttest. There were other limitations to the study design. One potential explanation for the change in performance may be due to attention from the occupational therapist and the desire to please (e.g., the Hawthorne effect [Landsberger, 1958]). Satisfaction scores did decline from the first (3-month) posttest to the two-year posttest, suggesting that attention from the therapist may have played a role in scores. Another related design flaw that introduces significant bias is the use of a single unblinded rater who was also the treating therapist.
It is also possible that other supportive changes occurred in the home over the course of the study and contributed to these findings. The change in the magnitude of the barriers’ influence score did continue to decline even two years post-intervention. Only changes noted in the initial treatment plan were photographed and verified at the follow-up visits. It is possible that the participants continued to make changes to their homes. It is important to understand if older adults or their family members continued to compensate for their functional limitations by adding additional environmental support. This question, related to the dose of the intervention, warrants further study. The time points that were used in this study could also have biased the results. It is possible that three months was not sufficient for the participants to become accustomed to the new environmental support. Optimal time points for follow up are not yet known. These flaws in measurement in this preliminary study should be addressed in future trials.
Our sample was skewed toward a fairly healthy, Caucasian population of community-dwelling older adults. Despite their relatively healthy status, these individuals identified a high number of problems performing their daily activities. They demonstrated measurable improvement in activity scores from the intervention. While the small sample limits the generalizability of the study, there are benefits to understanding the effect of home modifications on this group of individuals. This sample represents an underserved group that might benefit from occupational therapy services using a preventative model of care.
While the cost data may be helpful in planning services or future studies, the data should be interpreted with caution. The costs are in 2003 U.S. dollars, and there are differences between the U.S. and Canadian healthcare systems and possible differences between goods and services of the two countries.
Despite the limitations of the study design, the results of this preliminary study contribute new findings to the limited body of occupational therapy evidence that supports the use of home modifications. The client-centered approach to assessment and intervention yielded a positive outcome and was validated using objective measures. This study protocol is based on a strong theoretical model and introduces a new approach to measuring person-environment fit.
There is great complexity involved in supporting older adults in their decisions to age in place, thus a great deal more study is required. A randomized, controlled longitudinal study of a larger, more heterogeneous group of older adults is needed. Candidate endpoints that examine other potential health outcomes are also important.
Conclusion
This study of home modifications represents an attempt to enhance our current understanding of the impact of home modifications on the daily activity performance of community-dwelling older adults. These data suggest that older adults who are aging in place can improve their functional abilities with home modifications and thus improve their performance of daily activities. Despite the complexity of providing home modifications, we were able to systematically describe and measure meaningful performance outcomes with high levels of adherence. The surge in the aging population will begin taxing existing healthcare services unless solutions to dealing with the functional losses associated with aging are identified. Compensating for functional loss by providing environmental support appears to be a promising solution. This study joins the small but growing body of evidence suggesting that environmental modifications could forestall institutionalization and allow older adults to age in place. More specifically, we accept the argument of Gitlin et al. (2003), who maintain that because the majority of older adults live in private housing, reducing disability by improving person-environment fit in the home is an important intervention strategy that deserves further study.
Key messages
Providing environmental support to compensate for functional loss appears to be a promising, inexpensive solution to help older adults age in place.
There are measurable changes in function that can be detected two years after an occupational therapy environmental intervention.
Acknowledgments
Support for this project was provided by the Administration on Aging (Grant #: 90AM2612), the National Institutes for Health (Grant # K07 AG21164-02), John Morris, PI. and the State of Missouri in grants to the Jewish Federation of St. Louis, by the Harvey A. and Dorismae Friedman Research Fund at Washington University in St. Louis, and by the Washington University Center for Aging. A preliminary version of this paper was presented at the Gerontological Society of America, 2004. We would like to thank the study participants and the reviewers who provided invaluable feedback to the revision of this manuscript.
Contributor Information
Susan Stark, Email: starks@wusm.wustl.edu, Assistant Professor, Occupational Therapy and Neurology, Washington University School of Medicine, St. Louis, MO, Box 8505, 4444 Forest Park Blvd, Saint Louis, MO 63108. Telephone: 1 (314) 286-1626.
Amanda Landsbaum, Washington University School of Medicine, St. Louis, MO Box 8505, 4444 Forest Park Blvd., St. Louis MO 63108.
Janice Palmer, Washington University School of Medicine, Center for Aging, St. Louis, MO 4488 Forest Park Blvd., St. Louis MO 63108.
Emily K. Somerville, Washington University School of Medicine, St. Louis, MO, Box 8505, 4444 Forest Park Blvd., St. Louis MO 63108.
John C. Morris, Harvey A. and Dorismae Hacker Friedman Distinguished Professor of Neurology, Professor of Pathology and Immunology, Physical Therapy and Occupational Therapy, Washington University School of Medicine, St. Louis, MO 4488, Forest Park Blvd, St. Louis, MO 63108.
References
- American Association of Retired Persons. Understanding senior housing: For the 1990s. Washington, DC: Consumer Affairs Department; 1992. [Google Scholar]
- American Association of Retired Persons. Fixing to stay: A national housing survey on housing and home modification issues. 2000 Retrieved October 12, 2003, from the AARP Research web site: http://www.aarp.org/research/reference/publicopinions/aresearch-import-783.html.
- Baum C, Edwards D. Activity Card Sort. Harcourt Assessment, Inc; 2001. [Google Scholar]
- Callahan JJ, Lanspery S. Density makes a difference: Can we tap the power of NORCs? Perspective on Aging. 1997;26:13–20. [Google Scholar]
- Carpenter BD, Pickard JG, Palmer JL, Stark S, Neufeld PS, Morrow-Howell N, et al. Anticipating relocation: Concerns about moving among NORC residents. Journal of Gerontological Social Work. 2007;49(1–2):165–184. doi: 10.1300/J083v49n01_10. [DOI] [PubMed] [Google Scholar]
- Chandler JM, Duncan PW, Weiner DK, Studenski SA. Special feature: The home assessment profile-a reliable and valid assessment tool. Topics in Geriatric Rehabilitation. 2001;16(3):77–88. [Google Scholar]
- Clemson L, Cusick A, Fozzard C. Managing risk and exerting control: Determining follow through with falls prevention. Disability and Rehabilitation. 1999;13:531–541. doi: 10.1080/096382899297189. [DOI] [PubMed] [Google Scholar]
- Cordingly L, Webb C, Hiller V. Q Methodology. Nurse Researcher. 1997;4(3):31–45. doi: 10.7748/nr.4.3.31.s4. [DOI] [PubMed] [Google Scholar]
- Cumming R, Thomas M, Szonyi G, Salkeld G, O’Neill E, Westbury C, et al. Home visits by an occupational therapist for assessment and modification of environmental hazards: A randomized trial of falls prevention. Journal of the American Geriatrics Society. 1999;47:1397–1402. doi: 10.1111/j.1532-5415.1999.tb01556.x. [DOI] [PubMed] [Google Scholar]
- Cumming RG. Intervention strategies and risk-factor modification for falls prevention: A review of recent intervention studies. Clinical Geriatric Medicine. 2002;18:175–189. doi: 10.1016/s0749-0690(02)00004-6. [DOI] [PubMed] [Google Scholar]
- Cumming RG, Thomas M, Szonyi G, Frampton G, Salkeld G, Clemson L. Adherence to occupational therapist recommendations for home modifications for falls prevention. American Journal of Occupational Therapy. 2001;55:641–648. doi: 10.5014/ajot.55.6.641. [DOI] [PubMed] [Google Scholar]
- Devor M, Wang A, Renvall M, Feigal D, Ramsdell J. Compliance with social and safety recommendations in an outpatient comprehensive geriatric assessment program. Journal of Gerontology. 1994;49(4):M168–173. doi: 10.1093/geronj/49.4.m168. [DOI] [PubMed] [Google Scholar]
- Dovey K. Home and Homelessness. In: Altman I, Werner C, editors. Home environments: Vol 8. Human behavior and environment: Advances in theory and research. New York: Springer; 1985. pp. 33–64. [Google Scholar]
- Edwards D, Hahn M, Baum C, Perlmutter M, Sheedy C, Dromerick A. Screening patients with stroke for rehabilitation needs: Validation of the post-stroke rehabilitation guidelines. Neurorehabilitation and Neural Repair. 2006;20:42–48. doi: 10.1177/1545968305283038. [DOI] [PubMed] [Google Scholar]
- Elam J. Analysis of methods for predicting near-magnification power. Journal of the American Optometric Association. 1997;68:31–36. [PubMed] [Google Scholar]
- Everard K, Lach H, Fisher E, Baum C. Relationship of activity and social support to the functional health of older adults. The Journals of Gerontology Series B. Psychological and Social Science. 2000;55:S208–S212. doi: 10.1093/geronb/55.4.s208. [DOI] [PubMed] [Google Scholar]
- Fange A, Iwarsson S. Challenges in the development of strategies for housing adaptation evaluations. Scandinavian Journal of Occupational Therapy. 2007;14:140–149. doi: 10.1080/11038120600840150. [DOI] [PubMed] [Google Scholar]
- Fogel B. Psychological aspects of staying at home. Generations. 1992;16(2):15–19. [Google Scholar]
- Fried L, Guralnik J. Disability in older adults: Evidence regarding significance, etiology, and risk. Journal of the American Geriatrics Society. 1997;45:92–100. doi: 10.1111/j.1532-5415.1997.tb00986.x. [DOI] [PubMed] [Google Scholar]
- Gill T, Williams C, Tinetti M. Assessing risk for the onset of functional dependence among older adults: The role of physical performance. Journal of the American Geriatrics Society. 1995;43:603–609. doi: 10.1111/j.1532-5415.1995.tb07192.x. [DOI] [PubMed] [Google Scholar]
- Gitlin LN, Corcoran M, Winter L, Boyce A, Hauck WW. A randomized, controlled trial of a home environmental intervention: Effect on efficacy and upset in caregivers and on daily function of persons with dementia. The Gerontologist. 2001;41:4–14. doi: 10.1093/geront/41.1.4. [DOI] [PubMed] [Google Scholar]
- Gitlin LN, Corcoran MA. Expanding caregiver ability to use environmental solutions for problems of bathing and incontinence in the elderly with dementia. Technology and Disability. 1993;2:12–21. [Google Scholar]
- Gitlin LN, Hauck WW, Winter L, Dennis MP, Schulz R. Effect of an in-home occupational and physical therapy intervention on reducing mortality in functionally vulnerable older people: Preliminary findings. Journal of the American Geriatrics Society. 2006;54:950–955. doi: 10.1111/j.1532-5415.2006.00733.x. [DOI] [PubMed] [Google Scholar]
- Gitlin LN, Winter L, Corcoran M, Dennis MP, Schinfeld S, Hauck WW. Effects of the home environmental skill-building program on the caregiver-care recipient dyad: 6-month outcomes from the Philadelphia REACH initiative. The Gerontologist. 2003;43:532–546. doi: 10.1093/geront/43.4.532. [DOI] [PubMed] [Google Scholar]
- Hammel J. Assistive technology and environmental intervention (AT-EI) impact on the activity and life roles of aging adults with developmental disabilities: Findings and implications for practice. Aging and Developmental Disability. 2000:36–57. [Google Scholar]
- Hunt M. Transition over time: Naturally occurring retirement community. In: Gutman G, Blackie N, editors. Housing the very old. Burnaby, British Columbia: Simon Fraser University; 1988. pp. 161–172. [Google Scholar]
- Iwarsson S. A long-term perspective on person-environment fit and ADL dependence among older Swedish adults. The Gerontologist. 2005;45:327–336. doi: 10.1093/geront/45.3.327. [DOI] [PubMed] [Google Scholar]
- Iwarsson S, Isacsson A. ADL dependence in the elderly population living in the community: The influence of functional limitations and physical environmental demand. Occupational Therapy International. 1998;5:173–193. [Google Scholar]
- Iwarsson S, Nygren C, Oswald F, Wahl HW, Tomsone S. Environmental barriers and housing accessibility problems over a one-year period in later life in three European countries. Journal of Housing for the Elderly. 2006;20(3):23–43. [Google Scholar]
- Katzman R, Brown T, Fuld P, Peck A, Schechter R, Schimmel H. Validation of a short Orientation-Memory-Concentration Test of cognitive impairment. American Journal of Psychiatry. 1983;140:734–739. doi: 10.1176/ajp.140.6.734. [DOI] [PubMed] [Google Scholar]
- Keith RA, Granger CV, Hamilton BB, Sherwin FS. The functional independence measure: A new tool for rehabilitation. Advances in Clinical Rehabilitation. 1987;1:6–18. [PubMed] [Google Scholar]
- Landsberger H. Hawthorne revisited. Management and the worker, its critics, and developments in human relations in industry. New York: Cornell University Press; 1958. [Google Scholar]
- Law MC. Client centered occupational therapy. Thorofare, NJ: SLACK Inc; 1998. [Google Scholar]
- Law M, Baptiste S, Carswell A, McColl M, Polatajko H, Pollock N. Canadian Occupational Performance Measure. Toronto: Canadian Association of Occupational Therapists; 1994. [Google Scholar]
- Law M, Baptiste S, Mills J. Client centered practice: What does it mean and does it make a difference? Canadian Journal of Occupational Therapy. 1995;62:250–257. doi: 10.1177/000841749506200504. [DOI] [PubMed] [Google Scholar]
- Lawton MP, Nahemow L. Ecology and the aging process. In: Eisdorfer C, Lawton MP, editors. Psychology of adult development and aging. Washington, DC: American Psychological Association; 1973. pp. 619–674. [Google Scholar]
- Mann WC, Hurren D, Tomita M, Bengali M, Steinfeld E. Environmental problems in homes of older adults with disabilities. Occupational Therapy Journal of Research. 1994;14:191–211. [Google Scholar]
- Mann WC, Hurren D, Tomita M, Charvat BA. The relationship of functional independence to assistive device use of elderly persons living at home. Journal of Applied Gerontology. 1995;14:225–247. [Google Scholar]
- Mann WC, Ottenbacher KJ, Fraas L, Tomita M, Granger CV. Effectiveness of assistive technology and environmental interventions in maintaining independence and reducing home care costs for the frail elderly: A randomized controlled trial. Archives of Family Medicine. 1999;8:210–217. doi: 10.1001/archfami.8.3.210. [DOI] [PubMed] [Google Scholar]
- Mathias S, Nayak US, Isaacs B. Balance in elderly patients: The “get-up and go” test. Archives of Physical Medicine and Rehabilitation. 1986;67:387–389. [PubMed] [Google Scholar]
- Missouri Census Data Center. 2001 Missouri county population estimates. 2002 Retrieved July 13, 2007, from http://mcdc2.missouri.edu/publications/pdfs/v6n2-web.pdf.
- National Center for Health Statistics. Health monitor report. Washington, DC: Author; 2002. [Google Scholar]
- Oswald F, Wahl HW, Schilling O, Iwarsson S. Housing-related control beliefs and independence in activities of daily living in very old age. Scandinavian Journal of Occupational Therapy. 2007;14:33–43. doi: 10.1080/11038120601151615. [DOI] [PubMed] [Google Scholar]
- Oswald F, Wahl HW, Schilling O, Nygren C, Fange A, Sixsmith A, et al. Relationships between housing and healthy aging in very old age. The Gerontologist. 2007;47:96–107. doi: 10.1093/geront/47.1.96. [DOI] [PubMed] [Google Scholar]
- Petrella R, Overend T, Chesworth B. FIM after ip fracture: Is telephone administration valid and sensitive to change? American Journal of Physical Medicine & Rehabilitation. 2002;81:639–644. doi: 10.1097/01.CCM.0000026916.24522.BD. [DOI] [PubMed] [Google Scholar]
- Portney LG, Watkins MP. Foundations of clinical research: Applications to practice. 3. Norwalk, CT: Appleton & Lange; 2008. [Google Scholar]
- Pynoos J. Towards a national policy on home modification. Technology and Disability. 1993;2(4):1–8. [Google Scholar]
- Radomski MV, Trombly Latham C. Occupational therapy for physical dysfunction. 6. Philadelphia: Lippincott Willams & Wilkins; 2008. [Google Scholar]
- Resnick B, Inguito P, Orwig D, Yu Yahiro J, Hawkes W, Werner, et al. Treatment fidelity in behavior change research: A case example. Nursing Research. 2005;54:139–145. doi: 10.1097/00006199-200503000-00010. [DOI] [PubMed] [Google Scholar]
- Schoenfelder DP, Van Why K. A fall prevention educational program for community dwelling seniors. Public Health Nursing. 1997;14:383–390. doi: 10.1111/j.1525-1446.1997.tb00308.x. [DOI] [PubMed] [Google Scholar]
- Stark S. Creating disability in the home: The role of environmental barriers in the United States. Disability and Society. 2001;16:37–49. [Google Scholar]
- Stark S. Removing environmental barriers in the homes of older adults with disabilities improves occupational performance. Occupational Therapy Journal of Research. 2004;24:32–39. [Google Scholar]
- Stark S, Somerville E, Morris J. In-home occupational performance evaluation. American Journal of Occupational Therapy. doi: 10.5014/ajot.2010.08065. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinfeld E, Danford G. Environment as a mediating factor in functional assessment. In: Dittmar S, Gresham G, editors. Functional assessment and outcome measures for the rehabilitation health professional. Gaithersburg, MD: Aspen; 1997. pp. 37–56. [Google Scholar]
- Steinfeld E, Shea S. Enabling home environments: Identifying barriers to independence. Technology and Disability. 1993;2(4):69–79. Retrieved April 24, 2003, from http://www.cornellaging.com/gem/research_barriers_index.html.
- Stolee P, Zaza C, Pedlar A, Myers AM. Clinical experience with goal attainment scaling in geriatric care. Journal of Aging and Health. 1999;11:96–124. doi: 10.1177/089826439901100106. [DOI] [PubMed] [Google Scholar]
- Tabachnick BG, Fidell LS. Using multivariate statistics. 2. New York: Harper & Row; 1989. [Google Scholar]
- Trickey F, Maltais D, Gosselin C, Robitaille Y. Adapting older persons’ homes to promote independence. Physical and Occupational Therapy in Geriatrics. 1993;12(1):1–14. [Google Scholar]
- U. S. Department of Housing and Urban Development. Home modification among households with physical activity limitations. 2001 Retrieved January 5, 2007, from http://www.huduser.org/periodicals/USHMC/spring2001/summary-2.html.
- Valenta A, Wigger U. Q-methodology: Definition and application in health care informatics. Journal of the American Medical Informatics Association. 1997;4:501–510. doi: 10.1136/jamia.1997.0040501. [DOI] [PMC free article] [PubMed] [Google Scholar]