Abstract
Social anxiety disorder (SAD) and alcohol use disorders (AUD) co-occur at particularly high rates, resulting in greater impairment than either disorder alone. Thus, the development of effective treatments for patients with SAD and comorbid AUD is an important clinical and research aim. Yet little work has examined treatments for SAD with comorbid AUD. Given the efficacy of motivation enhancement therapy (MET) for AUD and cognitive-behavioral therapy (CBT) for SAD, combining MET with CBT may decrease symptoms of both AUD and SAD. The present case study outlines the successful use of combined MET-CBT to treat a 33-year-old man with a long history of generalized SAD with AUD. Following 19 sessions of MET-CBT, the patient was considered in remission for both disorders, with notable decreases in social anxiety and alcohol-related problems (with continued gains at 6-month follow-up). Although these data are preliminary, they indicate that the combination of MET and CBT may be a viable approach to the treatment for patients with SAD and comorbid AUD.
Keywords: social anxiety disorder, social phobia, alcohol use disorder, motivation enhancement therapy, cognitive-behavioral therapy, motivational interviewing
1 Theoretical and Research Basis
Social anxiety disorder (SAD) and alcohol use disorders (AUD) are among the most prevalent mental disorders (Kessler et al., 2005). Moreover, these disorders tend to co-occur at particularly high rates. To illustrate, in the National Epidemiologic Survey on Alcohol and Related Conditions (Grant et al., 2005), approximately 48% of individuals with a lifetime diagnosis of SAD also met criteria for a lifetime diagnosis of an AUD. Although the 12-month prevalence of AUD is 8.5% in the general population (Grant et al., 2004), that rate is elevated to 13.1% among individuals with SAD (Grant et al., 2005). In patients receiving treatment for alcohol-related problems, 23% to 39% meet diagnostic criteria for SAD (Kushner, Sher, & Beitman, 1990; Smail, Stockwell, Canter, & Hodgson, 1984; Thomas, Thevos, & Randall, 1999). Furthermore, SAD may serve as a risk factor for AUD, as adolescent SAD prospectively predicts the development of alcohol dependence by age 30, even after controlling for relevant disorders (e.g., depression, other anxiety disorders; Buckner et al., in press).
The high rates of comorbidity between SAD and AUD are a particular clinical concern because comorbidity tends to be associated with greater impairment than either condition alone. For instance, when compared to patients with SAD and no history of AUD, patients with current SAD and a lifetime history of AUD exhibited more severe SAD symptoms and were less likely to be married, indicating relative impairments in interpersonal functioning (Schneier, Martin, Liebowitz, Gorman, & Fyer, 1989). Among treatment-seeking participants in Project MATCH (Project MATCH Research Group, 1993), alcoholic patients with a lifetime diagnosis of SAD were more likely to have major depressive episodes and to experience more severe alcohol dependence, less peer social support, and lower occupational status than patients with AUD without SAD (Thevos, Thomas, & Randall, 1999; Thomas et al., 1999). Thus, although both SAD and AUD are debilitating in and of themselves, their combination is particularly pernicious, representing a substantial public health concern.
There is extensive and growing literature on the treatment of AUD and SAD in isolation. Several recent reviews (e.g., Heimberg, 2002; Ledley & Heimberg, 2005; Rodebaugh, Holaway, & Heimberg, 2004) and meta-analyses (Fedoroff & Taylor, 2001; Feske & Chambless, 1995; Gould, Buckminster, Pollack, Otto, & Yap, 1997; Taylor, 1996) attest to the efficacy of cognitive-behavioral therapy (CBT) for SAD as well as the durability of treatment gains. CBT (i.e., interventions including cognitive restructuring combined with in vivo exposure) has been shown to be as effective as or more effective than other interventions. Importantly, CBT has also been associated with significant improvements in quality of life (Eng, Coles, Heimberg, & Safren, 2001; Safren, Heimberg, Brown, & Holle, 1997). In sum, CBT appears to reduce social anxiety and increase quality of life in the short term, and these changes seem durable across extended follow-up periods.
For AUD, motivational enhancement therapy (MET) appears to be particularly promising. MET was designed to encourage fast, internally motivated change among patients with alcohol-related problems (Miller, Zweben, DiClemente, & Rychtarik, 1992). MET is a foursession intervention that incorporates feedback regarding the patient’s drinking behaviors relative to normative behavior combined with a brief course of motivational interviewing (MI; Miller & Rollnick, 2002). The underlying premise of MI is that individuals with problematic behaviors (e.g., problematic alcohol use) are often ambivalent about change. Although these individuals recognize that their problematic behavior causes impairment, they may be reluctant to change for a variety of reasons (e.g., fear of change, fear of failure, perceived benefits of the problematic behavior). Thus, the goal of MET is to explore and resolve ambivalence regarding change and to encourage patients to utilize their own change resources (versus the therapist’s outlining for the patient specific ways to change drinking behaviors). This goal is accomplished using patient-centered, directive interviewing to elicit change-related statements from the patient in a nonconfrontational manner.
MET occurs in three phases. In Phase 1, the therapist works with the patient to build motivation to change by using techniques such as supporting self-efficacy and building discrepancies between consequences of patients’ alcohol use and the ways in which they want to live their lives. In Phase 2, the therapist works to strengthen motivation to change using techniques such as eliciting self-change statements. The goal of Phase 2 in MET-CBT for SAD with comorbid AUD is to develop change plans regarding drinking behaviors, including ways to decrease overall drinking, drinking in social situations, and drinking to regulate anxiety reactions both in day-to-day life and as it pertains to CBT for SAD (e.g., drinking during or after exposures). Phase 3 consists of follow-through strategies (e.g., reviewing progress, renewing motivation to encourage continued use of the change plan). MET has been found to be as effective as CBT and 12-step facilitation for the treatment of AUD (Project MATCH Research Group, 1997).
Despite the high rates of comorbid AUD and SAD, very little attention has been focused on interventions addressing both conditions in combination. In fact, in the SAD literature, study of the treatment of comorbid AUD is virtually absent; the overwhelming majority of treatment outcome studies exclude patients with co-occurring AUD. Furthermore, we know of only one study that has evaluated a psychosocial treatment specifically designed to target patients with comorbid SAD-AUD (Randall, Thomas, & Thevos, 2001). In this study, alcoholic patients with SAD received individual CBT for AUD or CBT for SAD-AUD (treatment conditions did not differ in time devoted to AUD because CBT for SAD-AUD consisted of longer sessions). All patients demonstrated some improvement on social anxiety symptoms, although only half received the social anxiety–specific intervention. However, although patients in both conditions improved on alcohol-related outcome measures, CBT for SAD-AUD resulted in poorer alcohol-related outcomes at 3-month follow-up than CBT for AUD only. The relatively poor efficacy of combined treatment in this trial suggests a clear need for additional work using alternative treatment methods.
There are no studies in the literature examining the efficacy of CBT for SAD among patients with comorbid substance use problems. However, clinical experience suggests that CBT focused solely on SAD may be problematic. Patients with SAD and comorbid AUD may begin CBT feeling ambivalent about discontinuing alcohol use because they know of no means of managing anxiety other than using alcohol. Furthermore, by definition, exposure-based therapy provokes anxiety. Given that many of these patients use alcohol in response to negative affect (Buckner, Eggleston, & Schmidt, 2006) and to cope with social interactions (Thomas, Randall, & Carrigan, 2003), these patients may continue to drink as a means of managing social anxiety during therapeutic exposures. This response is of particular concern given that drinking to manage negative affect is associated with alcohol-related problems (Cooper, 1994; Cooper, Frone, Russell, & Mudar, 1995). Thus, both social anxiety and drinking could persist (and possibly worsen). In light of these concerns, we propose that it is necessary to target motivation to decrease alcohol use behaviors prior to CBT for SAD so that patients with SAD and comorbid AUD are better positioned to fully engage in CBT for SAD without reliance on alcohol.
Using MET to reduce problematic alcohol behaviors in concert with CBT for SAD appears to be the logical treatment choice for patients with SAD and comorbid AUD. MET for AUD is a time- and cost-efficient treatment for problematic alcohol use, the efficacy of which is supported by several reviews (Dunn, Deroo, & Rivara, 2001; Heather, 2005) and meta-analyses (Burke, Arkowitz, & Menchola, 2003; Moyer, Finney, Swearingen, & Vergun, 2002). In the treatment of SAD with comorbid AUD, MET can be used to explore ambivalence about drinking (e.g., the benefits of using alcohol to manage anxiety, the negative consequences associated with misusing alcohol) and to motivate patients to reduce their problem drinking, which is viewed as functionally related to their social anxiety.
In fact, recent work indicates that MET can be effectively used with patients with anxiety disorders. One group of researchers has recently examined the notion that MI techniques may increase motivation for engaging in CBT for anxiety disorders. Case studies suggest that the addition of MI to CBT for anxiety disorders may increase treatment adherence and enhance outcome (Westra, 2004; Westra & Phoenix, 2003). In a recent controlled study (Westra & Dozois, 2006), patients with anxiety disorders (including SAD) either received pretreatment with MI techniques or no pretreatment before beginning a course of CBT. Although both groups showed significant benefit, patients receiving the MI pretreatment rated themselves as more compliant with homework assignments and were more likely to be classified as responders on the primary outcome measures. These data clearly suggest that MET may be efficaciously combined with CBT in clinical settings, but this logical combination has yet to be applied to SAD with comorbid AUD.
2 Case Presentation
Preliminary findings from the treatment of a 33-year-old non-Hispanic Caucasian male patient with comorbid generalized SAD and AUD are provided to illustrate the potential utility of combining MET and CBT for the reduction of both SAD and AUD symptoms and associated impairment. The therapist was an advanced doctoral student in clinical psychology supervised by a licensed clinical psychologist.
3 Presenting Complaints
The patient presented for the treatment of social anxiety. He reported that his social anxiety caused significant impairment across a variety of domains of his life. For instance, he reported that this anxiety affected his job performance and opportunities for advancement at work. He also noted that he would like to be more comfortable meeting new people, as he would like to make more friends, join community clubs, and attend community events, but he avoided doing so because of his social anxiety. The patient did not initially indicate problems related to his alcohol use. It was only upon administration of the semistructured clinical interview that problems related to drinking became evident.
4 History
Familial and Social History Information
The patient reported that he was born and raised in the southern United States by both parents. He stated that he had experienced anxiety in social situations his entire life and that his parents tended to be anxious in social settings. He reported a history of alcoholism on his mother’s side of the family that he attributed to self-medication of anxiety reactions. He also stated that his paternal grandfather died of alcohol-related health problems.
The patient indicated he had a small group of close friends with whom he had been friends since childhood. He was married to a woman he described as his first girlfriend, and they had a 2-year-old daughter. The patient stated that his daughter was his primary reason for treatment, as he wanted to be a good role model and protect her from becoming socially anxious as well.
Employment History
The patient graduated from college with a bachelor’s degree in computer science. At intake, he was working as a computer programmer. He stated that the job was, in many ways, suited for his anxiety, as he worked independently the majority of the time (i.e., his job allowed him to avoid interpersonal interactions). However, he experienced intense and distressing anxiety in anticipation of group meetings. He also reported that his social anxiety interfered with his ability to network with his coworkers (e.g., he avoided lunches), and he believed this was hindering opportunities for career advancement.
Medical and Psychiatric History
The patient denied a history of significant medical problems. He reported attending religion-based premarital counseling, but he had never sought treatment for his social anxiety. At one point, he used self-help tapes aimed at decreasing social anxiety, but he did not find them particularly helpful. Furthermore, he reported using antidepressant medication 3 years prior to intake. He stated that the medication improved his mood somewhat, but he discontinued use because of unpleasant side effects.
5 Assessment
Clinical Interview
Anxiety Disorders Interview Schedule for DSM-IV (ADIS-IV; DiNardo, Brown, & Barlow, 1994)
The ADIS-IV is a structured diagnostic interview designed to provide detailed and thorough coverage of anxiety disorders. Additionally, it provides coverage of other Axis I disorders, including mood disorders, substance abuse or dependence, somatoform disorders, and psychosis. The ADIS-IV has been shown to be a reliable and valid measure of Diagnostic and Statistical Manual of Mental Disorders (fourth edition; American Psychiatric Association, 1994) anxiety and mood disorders (Brown, DiNardo, Lehman, & Campbell, 2001). The ADIS-IV also includes coverage of demographic information, medical history, and family psychiatric history.
In regard to SAD, the patient reported anxiety in a variety of social situations in which he might be observed by others (e.g., attending parties, talking in front of a group, talking to people in authority, being assertive, initiating and maintaining conversations) and that he believed this fear was excessive. He stated that he tended to avoid social situations, such as groups, unfamiliar people, and people in authority (e.g., his boss). He stated that his social anxiety had interfered in a number of areas of his life, including his job attainment and his ability to form new personal relationships. He also indicated that he was less likely to avoid social situations (e.g., parties) if alcohol was involved and that when under the influence of alcohol, his anxiety in social situations was reduced.
In regard to AUD, the patient met diagnostic criteria for alcohol abuse, reporting that in the past year, he repeatedly missed work or went to work late because of a hangover and that he repeatedly drove while intoxicated. He also stated that he often used alcohol to manage negative affect (e.g., anxiety, sadness) and endorsed some symptoms of alcohol dependence, including often drinking more than intended and physical tolerance. The diagnosis of alcohol abuse was confirmed using the Substance Use Disorders section of the Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Non-Patient Edition (SCID; First, Spitzer, Gibbon, & Williams, 2002). The SCID was used because it has demonstrated excellent interrater reliability for substance-related disorders (e.g., Buckner, Schmidt, Bobadilla, & Taylor, 2006), whereas these psychometrics have not been examined with the ADIS-IV. At intake, the patient met diagnostic criteria for SAD and alcohol abuse.
Self-Report Measures
Liebowitz Social Anxiety Scale–Self-Report Version (LSAS-SR; Liebowitz, 1987)
The LSAS-SR is a widely used instrument for the assessment of social anxiety. The LSAS-SR has demonstrated test-retest reliability, internal consistency, and convergent and discriminant validity (Baker, Heinrichs, Kim, & Hofmann, 2002; Fresco et al., 2001). A score of 60 for both the clinician-administered and self-report versions has been found to represent the best balance of sensitivity and specificity for discriminating between generalized and nongeneralized SAD (Mennin et al., 2002; Rytwinski et al., 2007). The LSAS-SR was administered at intake and again at follow-up. At intake, the patient’s LSAS-SR total score was 101, well into the severe range on this measure.
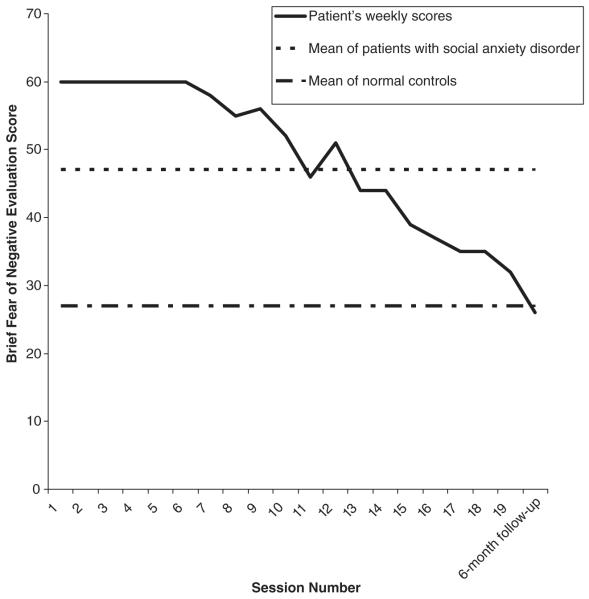
Brief Fear of Negative Evaluation Scale (BFNE; Leary, 1983)
The BFNE was used to provide a measure of social anxiety. The BFNE consists of 12 items rated on a 5-point Likerttype rating scale, ranging from 1 (not at all characteristic of me) to 5 (extremely characteristic of me). This measure has been shown to have good discriminant, convergent, and construct validity (Rodebaugh, Woods, et al., 2004; Weeks et al., 2005). The BFNE was administered before each therapy session to monitor the patient’s social anxiety from week to week. At intake, the patient scored a 60, the highest possible score on this measure.
Beck Depression Inventory (BDI; Beck & Steer, 1987)
The BDI is a 21-item self-report inventory that is used to assess the presence of depressive symptoms. Participants are asked to indicate which statement best describes the way they have been feeling during the past 2 weeks using a 0-to-3 scale. Total scores on the BDI can range from 0 to 63, with higher scores reflecting greater levels of depressive symptoms. The BDI has yielded adequate reliability estimates and is a well-validated measure of depressive symptomatology (Beck, Epstein, Brown, & Steer, 1988; Beck & Steer, 1987). The BDI was administered at intake and again at follow-up. At intake, the patient’s total BDI was 18.
Importance/Confidence Form (ICF)
Created to assess this patient’s motivation for treatment (per Miller & Rollnick, 2002), the ICF asked the patient to rate how important it was to change social anxiety–related behaviors and alcohol-related behaviors and how confident he was that he could make these changes. Ratings were made on a 0-to-10 scale with 0 being not at all important/confident and 10 being most important/most confident. The ICF was administered before each therapy session to monitor the patient’s motivation from week to week.
Social Anxiety Session Change Index (SASCI; Hayes, Miller, Hope, Heimberg, & Juster, in press)
The SASCI is a four-item self-report measure designed to provide session-by-session assessment of treatment progress in the treatment of social anxiety. The SASCI ranges from 4 to 28, with scores of 4 to 15 indicating improvement. This measure was administered at termination and follow-up to assess progress on aspects of social anxiety and avoidance since the beginning of treatment. The scale has been shown to have good psychometric properties (Hayes et al., in press).
The Alcohol Use Disorders Identification Test (AUDIT; Saunders, Aasland, Babor, de la Fuente, & Grant, 1993)
The AUDIT is a 10-item self-report measure that assesses multiple domains of alcohol-related problems. In a review of screening measures for alcohol problems, the AUDIT was found to be the most effective measure in identifying patients with at-risk or harmful drinking behaviors (Fiellin, Reid, & O’Connor, 2000; O’Connell et al., 2004). The AUDIT has demonstrated good psychometric properties in populations of varying ages (O’Connell et al., 2004). The AUDIT provides information on past-year, past-month, weekly, and daily alcohol use behaviors. A score of 8 to 15 suggests hazardous drinking, 16 to 19 is indicative of alcohol problems, and a score of 20 or more indicates possible alcohol dependence (Babor, Higgins-Biddle, Saunders, & Monteiro, 2001). The AUDIT was administered at termination and follow-up to assess alcohol-related problems following treatment.
6 Case Conceptualization
MET-CBT for SAD with comorbid AUD was recommended to treat this patient’s comorbid generalized SAD and AUD. Because the patient’s alcohol use could have interfered with SAD treatment (e.g., if exposures were performed under the influence of alcohol) and because of our concern that treatment could exacerbate the patient’s problematic drinking behaviors (e.g., drinking to cope with social anxiety induced as part of the treatment), the first four sessions of treatment consisted of MET to target the patient’s problematic alcohol use behaviors. MET was recommended to overcome ambivalence associated with the patient’s alcohol use and to build motivation and strengthen commitment to change problematic alcohol use. In addition, psychoeducation was provided during these initial sessions, as the patient felt he needed information on how his social anxiety would be managed before he could reduce his reliance on alcohol in social situations.
The CBT portion of treatment was based on the client workbook Managing Social Anxiety: A Cognitive-Behavioral Therapy Approach (Hope, Heimberg, Juster, & Turk, 2000). The treatment had five major components: (a) psychoeducation and orientation to CBT, (b) cognitive restructuring skills, (c) in-session and in vivo exposure to feared situations, (d) examination and modification of core beliefs, and (e) relapse prevention and termination. The structure of the treatment allows for some flexibility depending on needs of the individual patient. In the case of this patient, three sessions were allotted for the initial four chapters of the client workbook, which included psychoeducational material about social anxiety, an introduction to the treatment rationale, and development of the fear-and-avoidance hierarchy. In addition, we provided psychoeducation about the functional relationship between social anxiety and problematic alcohol behaviors. The patient was instructed to read relevant chapters in the workbook in advance of each session. The next two sessions focused on cognitive restructuring skills (e.g., teaching the patient to identify and challenge automatic thoughts). The first insession exposure occurred at Session 8. Treatment then proceeded with weekly in-session exposures, accompanying cognitive restructuring, and homework assignments for in vivo exposure related to the content of in-session work. Parts of later sessions were also dedicated to advanced cognitive restructuring in which core beliefs were examined. During the last two sessions (as termination approached), relapse prevention was discussed.
Focusing on alcohol use is entirely consistent with Hope et al.’s (2000; Hope, Heimberg, & Turk, 2006) protocol for individual CBT (I-CBT) for SAD, as discontinuation of all avoidance behaviors is encouraged, including reliance on alcohol. In addition, adjustments were made to this manual to further address the relations between social anxiety and alcohol-related problems. These adjustments included the following:
Adding alcohol use to existing weekly self-monitoring forms that ask patients to monitor anxiety and depression. The patient was asked to record alcohol use and indicate if it was related to social anxiety. Collecting this additional information facilitated a continued focus on the functional relationship between alcohol use and anxiety that was introduced during the MET lead-in to CBT.
Psychoeducational material that focused on the functional relationship between drinking and social anxiety.
Highlighting the importance of discontinuing alcohol use during exposures (in a manner consistent with the I-CBT manual for the discontinuation of more broadly defined safety behaviors) and offering specific strategies to do so that are consistent with the original manual (e.g., doing cognitive restructuring about what it would be like to go into a situation without alcohol so that the patient could act in ways that were consistent with his alcohol-related change plans).
Including material on goal setting and termination that is most relevant to patients with SAD and comorbid AUD, such as findings alternative ways to manage negative affect (e.g., taking a bath after work to relax versus drinking).
7 Course of Treatment and Assessment of Progress
The combination of MET and CBT resulted in decreased alcohol-related problems as well as decreased social anxiety. The majority of each of the first four sessions was devoted to MET to change alcohol-related behaviors, and homework consisted of reading psychoeducational materials (e.g., Hope et al., 2000). MET consisted primarily of highlighting the ways in which this patient’s alcohol use and social anxiety were related. In particular, sessions focused on how alcohol use to manage anxiety actually increased social anxiety in subsequent social situations. The patient indicated that he used alcohol to manage his anxiety in social situations in several ways. For instance, he used alcohol prior to social situations to manage anticipatory anxiety. Furthermore, if others were drinking in the social situation, he would drink to increase his sociability and for fear others would judge him negatively for not drinking. He agreed that his alcohol use created a vicious cycle in which after drinking in a social situation, his social anxiety would increase as he ruminated about the possibility that he behaved in an embarrassing manner while intoxicated. He also reported that his anticipatory anxiety regarding future social situations increased as he worried whether he would be as social, funny, and so on in subsequent situations as he was while under the influence of alcohol. After exploring the functional relationship between alcohol and social anxiety, weighing the pros and cons of alcohol use, and discussing how alcohol use fit in with his goals, the patient resolved to decrease his alcohol use (particularly, the use of alcohol to manage social anxiety).
By Session 4, the patient reported that he understood the interplay between his SAD and AUD and realized that it was necessary to treat them both if he was to decrease his social anxiety. On the ICF, he rated both the importance of changing his alcohol-related behaviors and his confidence in his ability to change these behaviors as an 8. This rating was not as high as the rating he gave for changing his social anxiety-related behaviors (ICF for social anxiety = 10 for importance), because he continued to see reducing his social anxiety as the most important treatment goal. Nevertheless, the patient’s importance and confidence ratings regarding alcohol-related behaviors were higher by Session 4 than they had been at intake (when both ratings were 7). Congruent with this shift, the patient reported that he had attended a social event without alcohol and had found it less challenging than he imagined. As a result, a change plan was developed to decrease alcohol use before, during, and after social situations (i.e., drinking to manage social anxiety). The change plan included daily monitoring of alcohol use. The patient’s goal for alcohol use was controlled drinking that was not for “social facilitation” or management of social anxiety.
Sessions 5 to 19 consisted primarily of CBT for SAD with continued monitoring of alcohol use behaviors. When the patient used alcohol, past-week alcohol use was discussed to determine whether this use remained consistent with his treatment goals. By Session 6, the patient’s ICF rating of importance to change his alcohol-related behaviors had risen to 9, as he began to observe the relation between his alcohol use and his mood. Through in-session review of his daily monitoring log of anxiety, depression, and alcohol use, the patient observed that his anxiety and depression were both greater on days following alcohol use.
During Session 13, the patient suggested a “no-drinking” social anxiety exposure for homework in which he would attend a party without using alcohol. At Session 14, he reported that the no-drinking exposure was a success, as he was able to use CBT skills during the party to manage his anxiety rather than rely on alcohol. Given the success of this homework exposure, the patient continued to develop other no-drinking exposures to practice CBT social anxiety management skills in situations in which he would have previously used alcohol to manage anxiety.
At termination, the patient was significantly improved in terms of both SAD and AUD. In fact, from Session 13 through Session 19 (i.e., termination session), the patient denied the use of alcohol to manage anxiety and reported no additional problems related to alcohol use. In addition to decreased alcohol-related problems, this patient also experienced clinically significant improvement in his social anxiety. His BFNE score decreased from 60 at intake to 32 at termination (see Figure 1). His termination SASCI score was 6. Given that SASCI scores of 4 to 15 indicate improvement, a score of 6 is very close to the best possible score of self-reported improvement of SAD symptoms. Furthermore, the patient’s AUDIT total score at termination was 11, indicative of a history of hazardous drinking in the past year (Babor et al., 2001). However, he demonstrated no alcohol-related problems in the past month. Given his treatment gains, the patient was considered in remission for both SAD and AUD.
Figure 1.
Decrease in Social Anxiety Over the Course of Combined Motivation Enhancement Therapy and Cognitive Behavioral Therapy for Social Anxiety Disorder With Comorbid Alcohol Use Disorder, Including 6-Month Follow-Up
Note: Clinical and nonclinical sample means from Weeks et al. (2005).
8 Complicating Factors
In the present case study, the sole complicating factor was the patient’s comorbid AUD. His depressive symptoms were not significant, nor did he present with any additional psychiatric complaint or any nonpsychiatric medical issue.
9 Managed Care Considerations
This patient was seen in the context of a specialty anxiety disorders clinic in a university setting. At this clinic, all patients pay out of pocket on a sliding fee scale. Thus, there were no managed care considerations with this case.
10 Follow-Up
Six months after termination, the patient returned to the clinic and underwent a follow-up assessment of his social anxiety and alcohol-related behaviors that included a brief unstructured clinical interview with his therapist and completion of self-report measures. Results indicated continued gains in both domains and that the patient remained in remission for both disorders. The clinical interview suggested that he no longer experienced excessive social anxiety. He reported that he no longer avoided situations that once made him anxious. Furthermore, he reported continued use of cognitive techniques (e.g., rational responses) to combat anxiety and that doing so had become “second nature.” He also indicated meaningful gains in quality of life. For instance, he interviewed for and obtained a job with a more desirable salary and more opportunities for networking and career growth. He also reported making new friends and enjoying the time he spent with family and friends, as he was no longer consumed in these situations by social anxiety–related worry.
The patient’s response to the interview was supported by the data collected on the self-report measures. His LSAS-SR score was 42, well below his intake score of 101. His BFNE score was 26, down from 60 at intake and 32 at termination (see Figure 1). On the SASCI, he continued to score a 6, indicating the patient believed that both his social anxiety and his anxiety-related avoidance had decreased since beginning treatment. His AUDIT total score at termination was 5, below the ranges indicative of hazardous drinking, alcohol problems, or alcohol dependence (Babor et al., 2001). Furthermore, his BDI decreased from an 18 at intake to an 8 at follow-up.
11 Treatment Implications of the Case
Although preliminary, these data point to the utility of combining MET with CBT in the treatment of SAD with comorbid AUD. As no empirically supported interventions currently exist for the treatment of AUD among those with SAD, it is appropriate to examine the utility of treatments found to be effective for each disorder independently. In this case, MET was chosen as a lead-in to CBT for SAD. The short duration of MET protocols (typically four sessions; Miller et al., 1992) provides a time-effective way to increase motivation to reduce problematic drinking behaviors prior to the implementation of CBT techniques aimed at decreasing social anxiety (e.g., exposure to feared social situations). By addressing alcohol use within the current CBT-for-SAD framework, the therapist in this case study was able to discuss with the patient the use of alcohol as an avoidance tactic (i.e., safety behavior) and thus was able to monitor alcohol use and work to change alcohol-related behaviors in a manner consistent with CBT for SAD (Hope et al., 2000, 2006). In ways such as these, techniques from both of these treatments worked in concert to increase motivation to change problematic alcohol-related behaviors while also targeting the patient’s social anxiety. Given the patient’s primary treatment goal was the reduction of social anxiety, this approach allowed for a treatment approach that was consistent with the patient’s goals. In other words, addressing alcohol use behaviors that contributed to his social anxiety allowed the focus of treatment to remain consistent with the patient’s agenda of reducing overall social anxiety.
12 Recommendations to Clinicians and Students
In the absence of data indicating that existing treatment protocols are effective in the treatment of comorbid SAD and AUD, we recommend that a prudent approach is to use a brief MET intervention prior to anxiety-provoking CBT techniques to decrease social anxiety (e.g., challenging cognitions, exposures). By arming socially anxious patients with an alcohol-related change plan prior to difficult and anxiety-provoking therapeutic techniques, we believe that the patient is at less risk to use alcohol to manage the anxiety that is necessarily increased during the course of CBT for SAD. It is of note that the patient presented in this case study readily observed the functional relationship between his alcohol use and social anxiety, allowing the course of MET in the present study to be limited to the standard four sessions (Miller et al., 1992). However, the course of MET in MET-CBT for SAD with comorbid AUD may depend on the specific patient’s readiness for change (see Miller & Rollnick, 2002). Although research indicates that many socially anxious individuals report using alcohol to manage anxiety (Thomas et al., 2003) and in response to situations involving negative affect and perceived peer pressure (Buckner, Eggleston, et al., 2006), it should not be assumed that a particular patient will quickly observe that his or her alcohol use acts as a typical safety behavior (i.e., decreases anxiety in the short term but maintains or increases anxiety in the long term; for discussion of safety aids and SAD, see Hope et al., 2000). Thus, it may take some patients longer to resolve ambivalence about alcohol use and to develop an alcohol-related change plan. On the other hand, some patients may initiate treatment with the understanding that their alcohol use has become problematic and may be ready to treat both the SAD and the AUD from the outset. In this case, the course of MET may be shorter. Thus, it is recommended that clinicians be prepared to use MET techniques in a manner appropriate for the motivation of each individual patient (see Miller & Rollnick, 2002).
It is also noteworthy that this patient attended treatment for 19 sessions versus the standard 16 sessions of CBT (Hope et al., 2006). This slightly longer treatment course was because of the incorporation of MET in the initial sessions and is consistent with the notion that comorbidity can result in a longer course of treatment (e.g., CBT) relative to patients without comorbid disorders. Patients with SAD and other types of comorbidity (e.g., depression) tend to demonstrate greater symptom severity at termination than patients with uncomplicated SAD (Erwin, Heimberg, Juster, & Mindlin, 2002), suggesting that perhaps comorbidity generally affects treatment response. It is therefore recommended that in reviewing the anticipated course of treatment with comorbid patients, clinicians indicate that the presence of a comorbid disorder may increase the duration of treatment (e.g., 20 to 25 sessions) so that patients have an accurate expectation of the course of their treatment.
In sum, although further clinical and empirical work is clearly necessary to evaluate the efficacy and effectiveness of MET-CBT for SAD with comorbid AUD, this initial evidence is promising. The excellent response to treatment demonstrated by the patient in this case example suggests that combining techniques from both MET and CBT may be a favorable approach to treating patients with both SAD and AUD. In light of the brief nature of MET, its addition to CBT may provide a time- and cost-effective manner to treat problematic alcohol use behaviors among socially anxious patients. Given the high rates of comorbid SAD and AUD, treatments aimed at ameliorating the symptomatology and associated functional impairment of these patients has the potential to benefit a great many patients.
Acknowledgments
This project was supported in part by a National Research Service Award from the National Institute of Drug Abuse (F31 DA021457) awarded to Julia D. Buckner.
Biography
Julia D. Buckner, a PhD candidate at Florida State University, is completing an internship at Yale University’s Division of Substance Abuse. Her work focuses on the nature and treatment of co-occurring anxiety and substance use disorders, for which she received a National Research Service Award from the National Institute on Drug Abuse.
Deborah Roth Ledley, PhD, is an associate director of the Adult Anxiety Clinic at Temple University. She has authored and coauthored numerous articles and chapters on the nature and treatment of anxiety disorders.
Richard G. Heimberg, PhD, is a director of the Adult Anxiety Clinic at Temple University. He is well known for developing cognitive-behavioral treatments for anxiety disorders. The Anxiety Disorders Association of America named him one of the four most influential psychological researchers in anxiety. In 2006, he received the Outstanding Mentor Award from the Association for Behavioral and Cognitive Therapies.
Norman B. Schmidt, PhD, is a director of clinical training at Florida State University and a director of the Anxiety and Behavioral Health Clinic. His work concerns the nature and treatment of anxiety disorders. For his research, he received the American Psychological Association’s Award for Distinguished Scientific Early Career Contribution to Psychology.
References
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: 1994. Author. [Google Scholar]
- Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. The Alcohol Use Disorders Identification Test: Guidelines for use in primary care. 2nd ed World Health Organization Department of Mental Health and Substance Dependence; Geneva, Switzerland: 2001. [Google Scholar]
- Baker SL, Heinrichs N, Kim H-J, Hofmann SG. The Liebowitz Social Anxiety Scale as a self-report instrument: A preliminary psychometric analysis. Behaviour Research and Therapy. 2002;40:701–715. doi: 10.1016/s0005-7967(01)00060-2. [DOI] [PubMed] [Google Scholar]
- Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: Psychometric properties. Journal of Consulting and Clinical Psychology. 1988;56:893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA. Manual for the revised Beck Depression Inventory. Psychological Corporation; San Antonio, TX: 1987. [Google Scholar]
- Brown TA, DiNardo PA, Lehman CL, Campbell LA. Reliability of DSM-IV anxiety and mood disorders: Implications for the classification of emotional disorders. Journal of Abnormal Psychology. 2001;110:49–58. doi: 10.1037//0021-843x.110.1.49. [DOI] [PubMed] [Google Scholar]
- Buckner JD, Eggleston AM, Schmidt NB. Social anxiety and problematic alcohol consumption: The mediating role of drinking motives and situations. Behavior Therapy. 2006;37:381–391. doi: 10.1016/j.beth.2006.02.007. [DOI] [PubMed] [Google Scholar]
- Buckner JD, Schmidt NB, Bobadilla L, Taylor J. Social anxiety and problematic cannabis use: Evaluating the moderating role of stress reactivity and perceived coping. Behaviour Research and Therapy. 2006;44:1007–1015. doi: 10.1016/j.brat.2005.08.002. [DOI] [PubMed] [Google Scholar]
- Buckner JD, Schmidt NB, Lang AR, Small J, Schlauch RC, Lewinsohn PM. Specificity of social anxiety disorder as a risk factor for alcohol and cannabis dependence. Journal of Psychiatric Research. doi: 10.1016/j.jpsychires.2007.01.002. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke BL, Arkowitz H, Menchola M. The efficacy of motivational interviewing: A meta-analysis of controlled clinical trials. Journal of Consulting and Clinical Psychology. 2003;71:843–861. doi: 10.1037/0022-006X.71.5.843. [DOI] [PubMed] [Google Scholar]
- Cooper ML. Motivations for alcohol use among adolescents: Development and validation of a four-factor model. Psychological Assessment. 1994;6:117–128. [Google Scholar]
- Cooper ML, Frone MR, Russell M, Mudar P. Drinking to regulate positive and negative emotions: A motivational model of alcohol use. Journal of Personality and Social Psychology. 1995;69:990–1005. doi: 10.1037//0022-3514.69.5.990. [DOI] [PubMed] [Google Scholar]
- DiNardo PA, Brown TA, Barlow DH. Anxiety Disorders Interview Schedule for DSM-IV: Lifetime Version (ADIS-IV-L) Oxford University Press; New York: 1994. [Google Scholar]
- Dunn C, Deroo L, Rivara FP. The use of brief interventions adapted from motivational interviewing across behavioral domains: A systematic review. Addiction. 2001;96:1725–1742. doi: 10.1046/j.1360-0443.2001.961217253.x. [DOI] [PubMed] [Google Scholar]
- Eng W, Coles ME, Heimberg RG, Safren SA. Quality of life following cognitive behavioral treatment for social anxiety disorder: Preliminary findings. Depression and Anxiety. 2001;13:192–193. [PubMed] [Google Scholar]
- Erwin BA, Heimberg RG, Juster H, Mindlin M. Comorbid anxiety and mood disorders among persons with social anxiety disorder. Behaviour Research and Therapy. 2002;40:19–35. doi: 10.1016/s0005-7967(00)00114-5. [DOI] [PubMed] [Google Scholar]
- Fedoroff IC, Taylor S. Psychological and pharmacological treatments of social phobia: A meta-analysis. Journal of Clinical Psychopharmacology. 2001;21:311–324. doi: 10.1097/00004714-200106000-00011. [DOI] [PubMed] [Google Scholar]
- Feske U, Chambless DL. Cognitive behavioral versus exposure only treatment for social phobia: A meta-analysis. Behavior Therapy. 1995;26:695–720. [Google Scholar]
- Fiellin DA, Reid MC, O’Connor PG. Screening for alcohol problems in primary care: A systematic review. Archives of Internal Medicine. 2000;160:1977–1989. doi: 10.1001/archinte.160.13.1977. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Non-patient Edition (SCID-I/NP) Biometrics Research, New York State Psychiatric Institute; New York: 2002. [Google Scholar]
- Fresco DM, Coles ME, Heimberg RG, Liebowitz MR, Hami S, Stein MB, et al. The Liebowitz Social Anxiety Scale: A comparison of the psychometric properties of self-report and clinician-administered formats. Psychological Medicine. 2001;31:1025–1035. doi: 10.1017/s0033291701004056. [DOI] [PubMed] [Google Scholar]
- Gould RA, Buckminster S, Pollack MH, Otto MW, Yap L. Cognitive-behavioral and pharmacological treatment for social phobia: A meta-analysis. Clinical Psychology: Science and Practice. 1997;4:291–306. [Google Scholar]
- Grant BF, Hasin DS, Blanco C, Stinson FS, Chou SP, Goldstein RB, et al. The epidemiology of social anxiety disorder in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry. 2005;66:1351–1361. doi: 10.4088/jcp.v66n1102. [DOI] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Ruan WJ, Pickering RP. Co-occurrence of 12-month alcohol and drug use disorders and personality disorders in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2004;61:361–368. doi: 10.1001/archpsyc.61.4.361. [DOI] [PubMed] [Google Scholar]
- Hayes SA, Miller NA, Hope DA, Heimberg RG, Juster HA. Assessing client progress session-by-session in the treatment of social anxiety disorder: The Social Anxiety Session Change Index. Cognitive and Behavioral Practice. doi: 10.1016/j.cbpra.2007.02.010. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heather N. Motivational interviewing: Is it all our clients need? Addiction Research and Theory. 2005;13:1–18. [Google Scholar]
- Heimberg RG. Cognitive-behavioral therapy for social anxiety disorder: Current status and future directions. Biological Psychiatry. 2002;51:101–108. doi: 10.1016/s0006-3223(01)01183-0. [DOI] [PubMed] [Google Scholar]
- Hope DA, Heimberg RG, Juster HA, Turk CL. Managing social anxiety: A cognitive-behavioral therapy approach (Client workbook) Oxford University Press; New York: 2000. [Google Scholar]
- Hope DA, Heimberg RG, Turk CL. Therapist guide for Managing Social Anxiety: A Cognitive-Behavioral Therapy Approach. Oxford University Press; New York: 2006. [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kushner MG, Sher KJ, Beitman BD. The relation between alcohol problems and the anxiety disorders. American Journal of Psychiatry. 1990;147:685–695. doi: 10.1176/ajp.147.6.685. [DOI] [PubMed] [Google Scholar]
- Leary MR. A brief version of the Fear of Negative Evaluation Scale. Personality and Social Psychology Bulletin. 1983;9:371–375. [Google Scholar]
- Ledley DR, Heimberg RG. Social anxiety disorder. In: Antony MM, Ledley DR, Heimberg RG, editors. Improving outcomes and preventing relapse in cognitive behavioral therapy. Guilford; New York: 2005. pp. 38–76. [Google Scholar]
- Liebowitz MR. Social phobia. Modern Problems of Psychopharmacology. 1987;22:141–173. doi: 10.1159/000414022. [DOI] [PubMed] [Google Scholar]
- Mennin DS, Fresco DM, Heimberg RG, Schneier FR, Davies SO, Liebowitz MR. Screening for social anxiety disorder in the clinical setting: Using the Liebowitz Social Anxiety Scale. Journal of Anxiety Disorders. 2002;16:661–673. doi: 10.1016/s0887-6185(02)00134-2. [DOI] [PubMed] [Google Scholar]
- Miller WR, Rollnick S, editors. Motivational interviewing: Preparing people for change. Vol. 2. Guilford; New York: 2002. [Google Scholar]
- Miller WR, Zweben A, DiClemente CC, Rychtarik RG. Motivational enhancement therapy manual: A clinical research guide for therapists treating individuals with alcohol abuse and dependence. National Institute on Alcohol Abuse and Alcoholism; Rockville, MD: 1992. [Google Scholar]
- Moyer A, Finney JW, Swearingen CE, Vergun P. Brief interventions for alcohol problems: A meta-analytic review of controlled investigations in treatment-seeking and non-treatment-seeking populations. Addiction. 2002;97:279–292. doi: 10.1046/j.1360-0443.2002.00018.x. [DOI] [PubMed] [Google Scholar]
- O’Connell H, Chin A-V, Hamilton F, Cunningham C, Walsh JB, Coakley D, et al. A systematic review of the utility of self-report alcohol screening instruments in the elderly. International Journal of Geriatric Psychiatry. 2004;19:1074–1086. doi: 10.1002/gps.1214. [DOI] [PubMed] [Google Scholar]
- Project MATCH Research Group Project MATCH: Rationale and methods for a multisite clinical trial matching patients to alcoholism treatment. Alcoholism: Clinical and Experimental Research. 1993;17:1130–1145. doi: 10.1111/j.1530-0277.1993.tb05219.x. [DOI] [PubMed] [Google Scholar]
- Project MATCH Research Group Matching alcoholism treatments to client heterogeneity: Project MATCH posttreatment drinking outcomes. Journal of Studies on Alcohol. 1997;58:7–29. [PubMed] [Google Scholar]
- Randall CL, Thomas S, Thevos AK. Concurrent alcoholism and social anxiety disorder: A first step toward developing effective treatments. Alcoholism: Clinical and Experimental Research. 2001;25:210–220. [PubMed] [Google Scholar]
- Rodebaugh TL, Holaway RM, Heimberg RG. The treatment of social anxiety disorder. Clinical Psychology Review. 2004;24:883–908. doi: 10.1016/j.cpr.2004.07.007. [DOI] [PubMed] [Google Scholar]
- Rodebaugh TL, Woods CM, Thissen DM, Heimberg RG, Chambless DL, Rapee RM. More information from fewer questions: The factor structure and item properties of the original and brief fear of negative evaluation scale. Psychological Assessment. 2004;16:169–181. doi: 10.1037/1040-3590.16.2.169. [DOI] [PubMed] [Google Scholar]
- Rytwinski NK, Fresco DM, Heimberg RG, Coles ME, Liebowtitz MR, Stein MB, et al. Screening for social anxiety disorder with the self-report version of the Liebowitz Social Anxiety Scale. 2007 doi: 10.1002/da.20503. Manuscript submitted for publication. [DOI] [PubMed] [Google Scholar]
- Safren SA, Heimberg RG, Brown EJ, Holle C. Quality of life in social phobia. Depression and Anxiety. 1997;4:126–133. doi: 10.1002/(SICI)1520-6394(1996)4:3<126::AID-DA5>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption—II. Addiction Research and Theory. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Schneier FR, Martin LY, Liebowitz MR, Gorman JM, Fyer AJ. Alcohol abuse in social phobia. Journal of Anxiety Disorders. 1989;3:15–23. [Google Scholar]
- Smail P, Stockwell T, Canter S, Hodgson R. Alcohol dependence and phobic anxiety states: I. A prevalence study. British Journal of Psychiatry. 1984;144:53–57. doi: 10.1192/bjp.144.1.53. [DOI] [PubMed] [Google Scholar]
- Taylor S. Meta-analysis of cognitive-behavioral treatments for social phobia. Journal of Behavior Therapy and Experimental Psychiatry. 1996;27:1–9. doi: 10.1016/0005-7916(95)00058-5. [DOI] [PubMed] [Google Scholar]
- Thevos AK, Thomas SE, Randall CL. Baseline differences in social support among treatment-seeking alcoholics with and without social phobia. Substance Abuse. 1999;20:107–121. doi: 10.1080/08897079909511399. [DOI] [PubMed] [Google Scholar]
- Thomas SE, Randall CL, Carrigan MH. Drinking to cope in socially anxious individuals: A controlled study. Alcoholism: Clinical and Experimental Research. 2003;27:1937–1943. doi: 10.1097/01.ALC.0000100942.30743.8C. [DOI] [PubMed] [Google Scholar]
- Thomas SE, Thevos AK, Randall CL. Alcoholics with and without social phobia: A comparison of substance use and psychiatric variables. Journal of Studies on Alcohol. 1999;60:472–479. doi: 10.15288/jsa.1999.60.472. [DOI] [PubMed] [Google Scholar]
- Weeks JW, Heimberg RG, Fresco DM, Hart TA, Turk CL, Schnieier FR, et al. Empirical validation and psychometric evaluation of the Brief Fear of Negative Evaluation Scale in patients with social anxiety disorder. Psychological Assessment. 2005;17:179–190. doi: 10.1037/1040-3590.17.2.179. [DOI] [PubMed] [Google Scholar]
- Westra HA. Managing resistance in cognitive behavioural therapy: The application of motivational interviewing in mixed anxiety and depression. Cognitive Behaviour Therapy. 2004;33:161–175. doi: 10.1080/16506070410026426. [DOI] [PubMed] [Google Scholar]
- Westra HA, Dozois DJ. Preparing clients for cognitive behavioral therapy: A randomized pilot study of motivational interviewing for anxiety. Cognitive Therapy and Research. 2006;30:481–498. [Google Scholar]
- Westra HA, Phoenix E. Motivational enhancement therapy in two cases of anxiety disorder. Clinical Case Studies. 2003;2:306–322. [Google Scholar]