Abstract
Increased discounting of delayed rewards may reflect a decision bias that contributes to excessive use of alcohol and, more generally, to an impulsive, disinhibitory predisposition that is characterized by a preference for immediate over long-term rewards. The current study examined the association between delay discounting of rewards and the co-variation among several types of disinhibitory problems that are often comorbid with alcohol dependence (AD). Lifetime problems with alcohol, marijuana, other drugs, childhood conduct disorder, and adult antisocial behavior were assessed in a sample of 426 young adults, 257 of whom had a lifetime diagnosis of AD. Higher delay discounting rates were associated with the covariation among all domains of disinhibitory problems and were not uniquely associated with any one domain. Higher delay discounting rates also were associated with lower intelligence, lower working memory capacity, and higher trait impulsivity. The results suggest that increased delay discounting of rewards may reflect aspects of a general vulnerability to externalizing, disinhibitory disorders.
Keywords: delay discounting, alcoholism, comorbidity, impulsivity, antisocial behavior
Individuals with alcohol dependence (AD) tend to discount future rewards relative to immediate rewards at higher rates compared to those without AD (Bjork, Hommer, Grant, & Danube, 2004; Finn, 2002; Mitchell, Fields, D’Esposito, & Boettiger, 2005; Petry, 2001). This pattern of increased discounting of delayed rewards may reflect decision biases that contribute to excessive use of alcohol and, more generally, to an impulsive predisposition that is characterized by a preference for immediate over long-term rewards and reduced cognitive capacity (Finn, 2002; Mitchell, Fields, D’Esposito & Boettiger, 2005).
However, because increased delayed discounting of rewards is thought to be a key component of impulsivity (Crean, de Wit, & Richards, 2000; Mitchell, 1999; Reynolds, 2006a) and because AD is highly comorbid with other disinhibitory disorders (Krueger et al., 2002), high rates of delay discounting also should be associated with other forms of disinhibitory psychopathology, such as childhood conduct disorder (CCD). In fact, considerable evidence suggests that this is the case. Abuse of and dependence on other substances, such as opiates, stimulants, and tobacco, also has been associated with increased delay discounting rates (Bornovalova, Daughters, Hernandez, & Richards, 2005; Epstein et al., 2003; Heil, Johnson, Higgins, & Bickel, 2006; Hoffman, et al., 2006; Johnson, Bickel, & Baker, 2007; Kirby & Petry, 2004; Kirby, Petry, & Bickel 1999; Madden, Petry, Badger, & Bickel 1997; Mitchell, 1999; Ohmura, Takanashi, & Kitamura, 2005; Reynolds, 2006a; 2006b; Reynolds, Karraker, Horn, & Richards, 2003). Furthermore, several studies show that elevated discounting rates are associated with other forms of disinhibitory psychopathology including antisocial personality disorder (Crean et al., 2000; Dom, De Wilde, Hulstijn, van Brink, & Sabbe., 2006a; 2006b; Petry, 2002).
The primary aims of this study were to investigate the association between delay discounting and disinhibitory disorders that are co-morbid with AD and to explore the personality and cognitive correlates of delay discounting. The overarching hypothesis was that increased delay discounting will be associated with different disinhibitory phenotypes, such as AD, CCD, other disinhibitory problems / symptoms, and self-reported impulsivity, and reductions in cognitive ability associated with behavioral disinhibition. The central thesis was that increased delay discounting rates reflect specific processes that contribute to impulsivity, which is a core feature of disinhibitory disorders (Finn, 2002).
The basic study design was a 2 × 2 [AD: CCD] independent-groups model to enable an evaluation of the relative association between delay discounting and both AD and CCD. CCD was chosen as an indicator of antisocial disinhibitory psychopathology because our sample is younger (ages 18–30) and, while a history of CCD is a prerequisite for adult antisocial personality, CCD is often not assessed in studies of early-onset AD. The first hypothesis was that the combination of AD and a history of CCD would be associated with higher delay discounting rates than AD without CCD because the combination of AD and CCD represents a more severe form of disinhibitory psychopathology (Finn, Mazas, Justus, & Steinmetz, 2002).
However, recent research suggests that the high level of covariation among externalizing disorders is better conceptualized as a single latent dimension of disinhibitory problems rather than as the co-occurrence of distinct disorders (Krueger & Markon, 2006; Krueger et al., 2002; 2005). Although some studies have assessed delay discounting in AD with and without comorbid antisocial personality or other cluster B personality disorders (Dom et al., 2006a; 2006b; Petry, 2002), these studies have failed to directly evaluate the relative influence of delay discounting on specific domains of comorbid externalizing problems, or the covariance among comorbid externalizing problems. This study addressed this issue by using structural equation modeling to examine the association between delay discounting and a single latent disinhibitory disorders factor that reflected the covariation among externalizing problems. Our recruitment strategy was designed to ensure sufficient variation and range in severity of lifetime problems with alcohol, marijuana, other drugs, CCD, and adult antisocial behavior. The second hypothesis was that increased delay discounting rates would be positively associated with the covariation among different types of externalizing - disinhibitory problems, rather than being specific to any one problem domain.
This study also explored the association between discounting of delayed rewards, self-reported traits of impulsivity and harm avoidance, measures of cognitive ability (i.e., executive working memory capacity and intelligence), and increased responsiveness to reward cues, all of which have been associated with both disinhibitory disorders and impulsive behaviors. Several delay discounting studies reported a significant positive association between delay discounting rates and self-reported measures of trait-impulsivity (de Wit, Flory, Acheson, McCloskey, & Manuck, 2007; Kirby & Petry, 2004; Kirby et al., 1999; Mitchell et al., 2005), while others reported no association (Crean et al., 2000; Dom et al., 2006b; Dom, De Wilde, Hulstijn, & Sabbe, 2007; Mitchell, 1999). Nonetheless, preference for a smaller immediate reward over a larger delayed reward has been used as a behavioral model of impulsivity and has been observed in impulsive substance using populations (Dom et al., 2006b; Johnson & Bickel, 2002; 2008; Kirby et al., 1999; Kirby & Petry, 2004; Madden et al., 2003; Petry, 2002; Reynolds, 2006a). We hypothesized that increased discounting rates would be associated with higher levels of trait impulsivity, but not with low harm avoidance, a personality trait that has been associated with externalizing behaviors via different disinhibitory mechanisms (Finn, 2002; Finn et al., 2002).
Disinhibitory disorders and increased discounting of delayed rewards also have been associated with low intelligence and reduced working memory capacity (de Wit et al., 2007; Dom et al., 2007; Finn & Hall, 2004; Finn et al., 2002; Hinson, Jameson, & Whitney, 2003; Hoffman et al., 2006; Kirby & Petry, 2004). Lower intelligence and reduced working memory capacity are thought to contribute to impulsive decisions by interfering with an individual’s ability to optimize goal-directed behavior while keeping distal, less salient stimuli in mind (de Wit et al., 2007; Finn & Hall, 2004; Hinson et al., 2003). Therefore, we hypothesized that increased discounting of delayed rewards would be associated with lower intelligence and working memory capacity. Finally, studies also suggest that highly salient and temporally proximal stimuli exert greater influence on decision making in antisocial alcoholic individuals than in controls (Finn, 2002; Finn et al., 2002). This study used a reward incentive salience manipulation to test the hypothesis that delay discounting rate would be more strongly associated with AD and / or CCD when the rewards were highly salient.
In summary, this study was designed to add to our knowledge of the association between increased delay discounting and AD by examining the association between delay discounting rates and lifetime disinhibitory problems, disinhibitory personality traits, and cognitive capacity. The overarching hypothesis was that increased delay discounting would be associated with the covariation among AD and related disinhibitory disorders, high trait impulsivity, and reduced cognitive capacity.
Methods
Participants
Recruitment
Participants were recruited using advertisements placed in local and student newspapers and around the community. These advertisements were designed using the approach used by Widom (1977) and others (Bauer & Hesselbrock, 1993; Finn et al., 2002) to elicit responses from individuals varying in terms of the level of impulsive, disinhibited traits and levels of alcohol use. The advertisements and flyers asked for “daring, rebellious, defiant individuals,” “carefree, adventurous individuals who have led exciting and impulsive lives,” “impulsive individuals,” “heavy drinkers wanted for psychological research,” persons with a “drinking problem,” persons who “got into a lot of trouble as a child,” persons “interested in psychological research,” “quiet, reflective and introspective persons,” and “social drinkers.” This approach has been very effective in attracting responses from individuals who vary in the expected levels of disinhibited traits, AD, CCD, antisocial personality (ASP), and behavioral disinhibition (Finn et al., 2002).
Telephone screening interview
Each respondent was screened via telephone to determine if they met study inclusion criteria. Respondents who met study inclusion criteria were told that they must abstain from using alcohol and other drugs for at least 12 hours before testing. Those who met study inclusion criteria were between ages 18 and 30, read and spoke English, had at least a grade 6 education level, did not report any severe head injuries, had no history of psychosis, and had consumed alcohol on at least one occasion in their life.
Group inclusion and exclusion criteria
The inclusion criteria for the control group were [1] not meeting DSM-IV (Diagnostic and Statistical Manual of Mental Disorders – 4th Edition, American Psychiatric Association, 1994) criteria for a lifetime history of AD, CCD, ASP, alcohol abuse or any other substance abuse or dependence, [2] not using marijuana more than eight times in the last 6 months, [3] not using any other mood altering drug in the last 6 months, [4] not using marijuana more than 15 times in their life, and [5] not using other mood altering drugs recreationally more than 4 times in their life. The inclusion criteria for the AD-alone group were meeting DSM-IV criteria for a history of AD but not CCD or ASP. The inclusion criteria for the ADCCD group were meeting DSM-IV criteria for a history of both AD and CCD. The inclusion criteria for the CCD-alone group were meeting DSM-IV criteria for a history of CCD but not AD. We chose to focus on CCD instead of ASP during recruitment, because CCD is a prerequisite to ASP and directly associated with adult antisocial behavior, and because delinquent behaviors after the age of 15 are often associated with alcohol or drug use.
Test session exclusion criteria
At the beginning of each testing session, participants were asked about their alcohol and drug use in the past 24 hours and were given a breath alcohol test using an AlcoSensor IV (Intoximeters Inc., St. Louis, MO). Participants were rescheduled if they reported consuming alcohol or drugs in the past 12 hours, if their breath alcohol level was greater than 0.0%, if they reported feeling hung-over, or if they appeared impaired, high, overly sleepy, or ill.
Sample characteristics
The sample consisted of 426 young adults: 129 (69 men, 60 women) with a history of AD with no history of CCD, 62 (32 men, 30 women) with a history of CCD and no history of AD, 128 (75 men, 53 women) with a history of both AD and CCD, and 107 (54 men, 53 women) controls. The sample was 77% Caucasian, 13% African American, 6% Asian, and 4% Hispanic. The control group was 60% Caucasian, 15% African American, 3% Hispanic or Latino, 21% Asian American or Asian, and 1% other ethnicity; the CCD-alone group was 81% Caucasian, 18% African American, and 2% Hispanic or Latino; the AD-alone group was 91% Caucasian, 5% African American, 2% Hispanic or Latino, 2% Asian American or Asian, 1% other ethnicity; the ADCCD group was 84% Caucasian, 9% African American, 5% Hispanic or Latino, and 3% Asian American or Asian.
Forty-three percent of the total sample (n = 184) met DSM-IV criteria for lifetime history of marijuana abuse or dependence, including 24 participants in the CCD-alone group, 66 in the AD-alone group, and 94 in the ADCCD group. Within marijuana dependent or abusing individuals, 61% (n = 112) were currently experiencing problems and 39% (n = 72) had past problems with marijuana use. Independent of marijuana use, 29% of the total sample (n = 124), including 25 CCD-alone, 37 AD-alone, and 62 ADCCD participants, met DSM-IV criteria for lifetime history of abuse or dependence of one or more illicit drugs. Of these individuals, 93% (n = 115) reported past problems associated with illicit drug use, while 25% (n = 31) were currently using illicit drugs. Although the drug abusing or dependent individuals most commonly abused marijuana (90%), 52 (25%) also reported abusing cocaine, 72 (35%) reported abusing other stimulants, 56 (27%) reported abusing sedatives, 20 (10%) reported abusing opiates, and 34 (17%) reported abusing other drugs, such as nitrous oxide or ecstasy.
Assessment Procedures and Materials
Diagnostic interview
Subjects were administered the Semi-Structured Assessment for the Genetics of Alcoholism (SSAGA-II, Bucholz et al., 1994) to ascertain lifetime diagnoses and symptoms of AD, CCD, adult antisocial personality, and marijuana and other drug abuse or dependence. Indicators of lifetime problems with childhood conduct, adult antisocial behavior, alcohol use, marijuana use, and other drug use were determined by summing positive responses to relevant SSAGA-II questions in the respective diagnostic sections.
Recent alcohol and other substance use
Alcohol use was quantified as the average frequency of drinking (days per week), the average quantity consumed per day, and the density of consumption (largest number of drinks consumed on a single occasion) over the past 6 months. Drug use was quantified as the average frequency of use (days per week) for marijuana, stimulants, sedatives and opiates over the past 3 months.
Personality assessment
Impulsivity was assessed with the impulsivity subscale of the Eysenck Impulsivity – Venturesomeness questionnaire (Eysenck & Eysenck, 1978); this self-report measure has been shown to be associated with elevated delay-discounting rates observed in heroin abusers (Kirby et al., 1999; Kirby & Petry, 2004). Impulsivity data were missing for one AD subject and one ADCCD subject. Harm avoidance was measured with the harm avoidance subscale of the Multidimensional Personality Questionnaire (MPQ; Tellegen, unpublished manuscript, 1982). The MPQ harm avoidance subscale assesses the tendency to avoid dangerous or risky activities and behavioral inhibition (Waller, Lilienfeld, Tellegen, & Lykken, 1991). Harm avoidance is inversely related to impulsive, thrill-seeking and risk-taking personality traits (Kadden, Donovan, Litt, & Cooney, 1996). While low harm avoidance has been associated with antisocial traits and substance abuse risk (Finn, 2002; Masse & Tremblay, 1997), it is thought to reflect different processes (i.e., decreased inhibition in the face of threat) than those reflected in impulsivity (Finn, 2002).
Cognitive measures
Working memory capacity was assessed with the Operation-Word span test (Conway & Engle, 1994). This test taps into complex working memory functions including the competition for attentional resources (i.e., divided attention) and the maintenance, or decay, of mental representations over brief distraction periods. The test involves solving simple mathematical operations while trying to remember words. The subjects were presented with a stack of index cards, each card containing a short mathematical equation followed by a word (e.g., 6/3 + 2 = 4 DOG). They were instructed to read the math operation aloud, respond “yes” or “no” to indicate whether the answer was correct, and then say the word (e.g., “dog”) aloud. After a series of operation-word pairs, the subjects were prompted to recall the words in that series in the order they were given. Series varied in length from 3 to 6 operation- word pairs and each series length was repeated three times during the task. The dependent measure on this test was calculated by adding the number of correctly recalled words across all test series. Test data was missing for one ADCCD participant on this measure.
General intelligence was measured using Shipley Institute of Living Scale estimates of IQ (Zachary, 1986). The Shipley is a self-administered measure of intelligence that assesses both verbal intelligence and logical reasoning and is strongly correlated with the WAIS Full Scale IQ (Zachary, 1986). Research shows that Shipley IQ estimates are associated with antisocial traits and alcohol abuse (Finn & Hall, 2004). Data for one control participant and one ADCCD participant were missing on this measure.
Delay Discounting Task
The delay discounting task consisted of “ascending” and “descending” choice trials on which participants were asked to indicate whether they preferred a specific amount of money “now” (i.e., the immediate reward) or $50 “later”( i.e., 1 week, 2 weeks, 1 month, 3 months, 6 months, 1 year). On ascending trials, the immediate reward value began with $0.05, followed by $1.25 and was then increased from $2.50 to $50 in 20 steps of $2.50. On descending trials, the immediate reward was reduced from $50 to $2.50 in 20 steps of $2.50 and ended with values of $1.25 and $0.05. Thus, subjects made 22 choices on both ascending and descending trials for each of the 6 payment delays. The immediate reward values were printed on a deck of index cards that were flipped by the participants after each trial. At each delay, the 44 ascending and descending trials were administered in order regardless of participants’ behavior. The delay blocks were always administered shortest to longest. During each delay block, the experimenter placed a laminated card displaying the delay on the table and instructed the participants that the $50 reward would now be available after the time displayed on the card. The experimenter recorded all 264 responses made by the participants during the task.
Reward incentive salience
The salience of any particular stimulus is determined by attributes, such as size, color, and brightness, and by context-dependent factors including validity and uncertainty or both (Estes, 1994). Differences in incentive salience are also derived from the stimulus’ rewarding or motivational properties and from outcomes associated with that stimulus through past experiences. For example, monetary rewards may vary in their degree of incentive salience (Robinson & Berridge, 2003), such that more tangible, highly probable, and larger amounts of money carry more incentive salience than less tangible, lower probable, smaller amounts of money. Small amounts of money also may vary across individuals in their motivational properties based on subjective utility of those amounts. In the present study, participants were randomly assigned to one of two reward salience conditions (high or low).
The high salience condition included the presence of real money (i.e., highly tangible) and a 100% probability (highly probable) of receiving any money after the task. The low salience condition included a promissory note for money (i.e., less tangible) and a 17% probability (less probable) of receiving any money after the task. The purpose of manipulating reward salience was to assess group differences in response to salience to monetary rewards, not to systematically test the effects of varying the two parameters of tangibility and probability of reward. In the high salience condition, $50 in USD ($10 and $20 denominations) was counted in full view of the participant and then placed on the table in front of the participant. The participant was told that she or he would receive an amount of money either immediately or at a delayed date, determined by drawing a numbered bead (1–264) from a plastic container after the task was completed. The numbered beads reflect all possible trial choices. If the number corresponded to a choice where the immediate amount was preferred, she or he would immediately be paid the amount indicated in cash. If the number corresponded to a choice where the delayed amount was preferred, the participant would receive a payment voucher that could be redeemed at the specified delay date. In the low salience condition, a $50 voucher was placed on the table in front of the participant. The participant was told that she or he had one in six chance of obtaining the money associated with her or his choice, which would be determined by drawing a bead with the number “6” printed on it at the end of the task. Those who drew a “6” received money in the same manner as in the high salience condition by drawing a numbered bead (1–264) that corresponded to a specific choice trial. In the high reward salience condition, there were 27 control men and 27 control women, 16 CCD-alone men and 14 CCD-alone women, 35 AD-alone men and 30 AD-alone women, and 38 ADCCD men and 26 ADCCD women. In the low reward condition, there were 27 control men and 26 control women, 16 CCD-alone men and 16 CCD-alone women, 34 AD-alone men and 30 AD-alone women, and 37 ADCCD men and 27 ADCCD women.
Delay discounting data from a total of 33 participants (9 controls - 4 men & 5 women; 4 CCD-alone - 1 man & 3 women; 8 AD-alone - 4 men & 4 women; 12 ADCCD - 4 men & 8 women) were not included in the analyses. Exclusion criteria were consistent with the guidelines proposed by Johnson & Bickel (2008) for identifying and eliminating unsystematic discounting data. The authors suggested eliminating individuals who (1) did not discount by at least 10% from the first to the last delay (31 cases excluded here), and (2) exhibited increases in the magnitude of switch points (starting at the second delay) by a magnitude greater than 20% of the larger reward (2 cases excluded here). All subsequent analyses were conducted using the remaining 393 cases.
Estimation of discounting rate
We assumed that the general form of delay discounting of future rewards can be adequately modeled using a single-parameter hyperbolic function (Mazur, 1987) Vp = V / (1 + k·dt), where Vp was the present (discounted) value, the constant V was the amount of the delayed reward (i.e., $50), dt was the length of time the reward is delayed expressed in days (i.e., 0, 7,14, 28, 91,182, and 364), and k was the discounting rate. All k estimates carry the reciprocal of days (1/days) as units in the modeling. At each delay, the Vp represented an arithmetic average of the ascending and descending run values at which the subject switched from selecting the present to the delayed reward or vice versa. Using non-linear regression, we estimated k separately for each subject by fitting the single-parameter hyperbolic model to the observed data with the discounted value Vp set to $50 at zero delay. Resulting k values of zero reflected no discounting, while k values greater than 0 indicated that the delayed reward is discounted relative to the immediate reward. The dependent measure used in all analyses was the log10 transformed k value.
Data Analyses
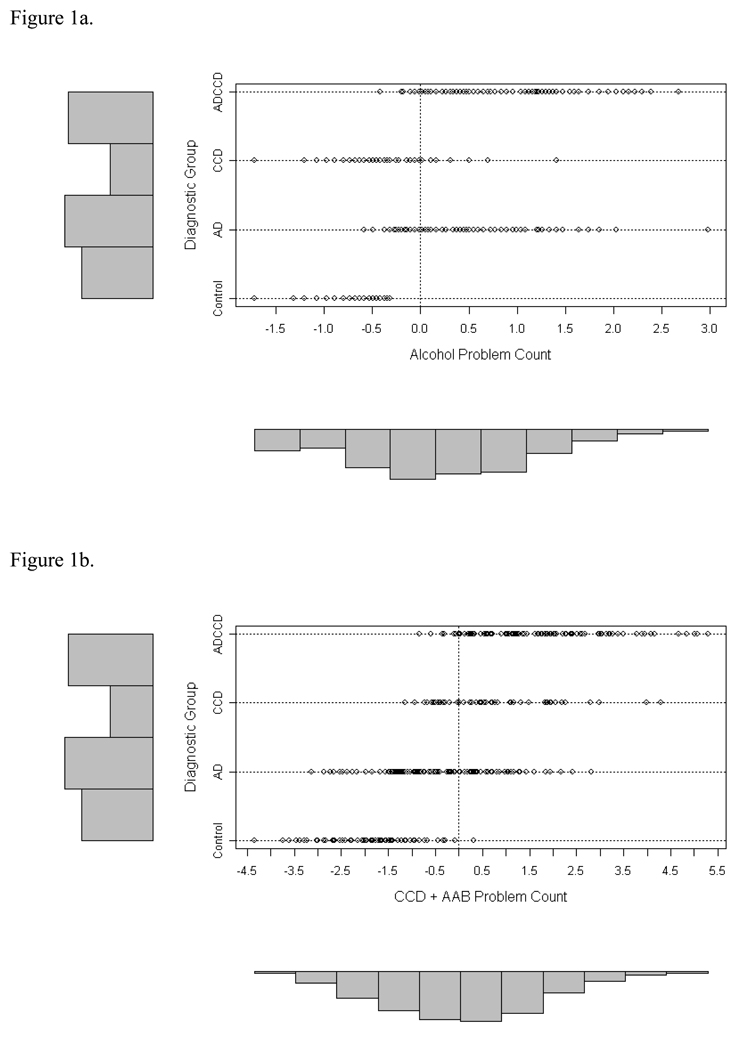
Prior to the analyses, missing data on the cognitive and impulsivity measures were imputed using a single imputation procedure with a multiple regression equation using all available data as predictors. The relative influences of AD and CCD on delay discounting rates were investigated using a 2 × 2 × 2 × 2 (AD by CCD by gender by reward salience condition) ANOVA. Planned comparisons were used to test the hypotheses that the ADCCD group would have significantly higher delay discounting rates than both the AD-alone and CCD-alone groups. Structural Equation Modeling (SEM) using Amos 6.0 (Arbuckle, 1995) was used to test the hypothesis that delay discounting rates would be positively associated with the covariance among these disorders, rather than being specific to any one disinhibitory disorder. SEM examined the association between a latent disinhibitory disorders (DD) factor and the rate of delay discounting (log10 k). The DD factor was indicated by lifetime problems with alcohol, marijuana and other drug use, CCD, and adult antisocial behavior. Lifetime problem measures were Blom transformed to minimize skew prior to SEM analyses, and the resulting distributions of alcohol and CCD plus adult antisocial symptoms are displayed in Figures 1a and 1b. Blom transformation is considered an optimal approach to handling psychiatric symptom counts in multivariate modeling analyses (Krueger et al., 2002; van den Oord et al., 2000). Modification indices were used to assess whether the individual indicators of the DD factor were uniquely associated with the delay discounting rate, beyond their covariance with other DD indicators in the model. A modification index greater than 4.0 for a path from a DD indicator to the log10(k) variable indicates that overall model fit will improve by adding that path to the model.
Figures 1a and 1b.
Blom-transformed lifetime problem counts by diagnostic group for alcohol problems in the top panel (1a) and an aggregate measure of childhood conduct disorder (CCD) plus adult antisocial behavior (AAB) problems in the bottom panel (1b). The bars on the left represent number of participants in each diagnostic group, while the bars below are frequencies of problem counts in the entire sample.
A second analysis of gender differences in the association between the DD factor and discounting rate log10 (k) were examined using a multiple-group SEM analysis. This analysis compared the fit of a model in which the regression coefficients between the DD factor and delay discounting rate were allowed to vary freely across gender (model A) to the fit of a model in which the coefficients were constrained to be equal for men and women (model B).
A third SEM assessed whether recent substance use accounted for the association between the DD factor and delay discounting. This SEM included an alcohol use latent factor indicated by drinking quantity, frequency, and density, and a drug use latent factor indicated by the frequencies of marijuana, opiate, sedative, and stimulant use. All substance use indicators were Blom transformed.
The final SEM was used to explore the association between exogenous observed personality and cognitive variables (impulsivity, working memory capacity, and intelligence) and discounting rate log10 (k).
The goodness of fit for all models was assessed with χ2 goodness of fit, the Bentler-Bonett normed fit index (NFI, 1980), and the root mean square error of approximation (RMSEA: Browne & Cudek, 1993). A close fit of the model is reflected in a non-significant NFI (higher than .94), RMSEA of .08 or less, and a non-significant χ2 statistic (Bentler & Bonett, 1980; Browne & Cudek, 1993).
Results
AD, CCD, and Gender on Delay Discounting
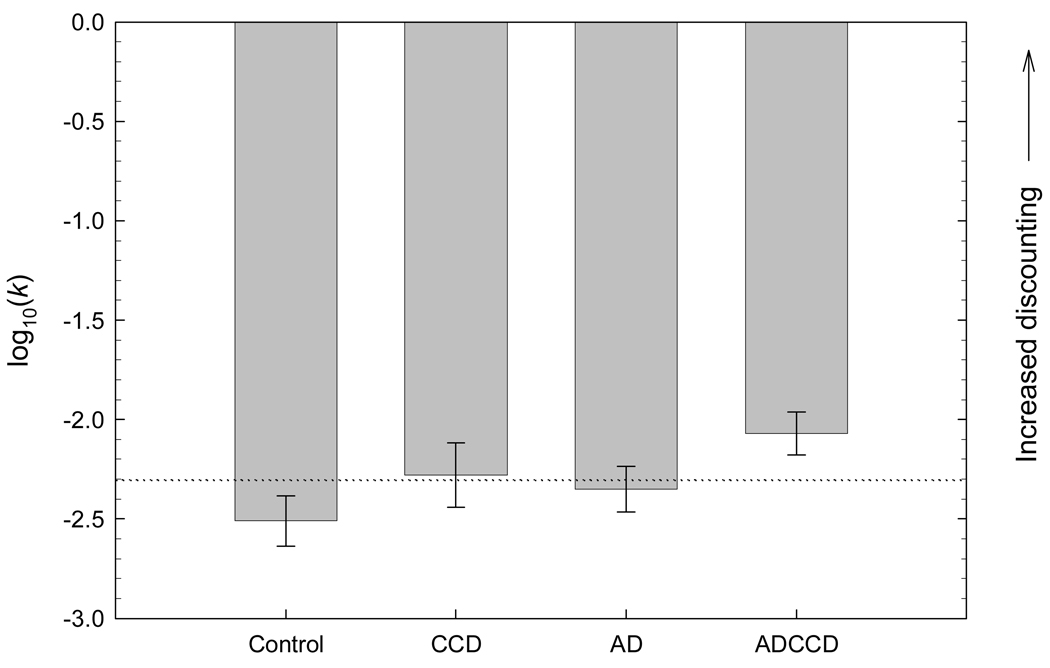
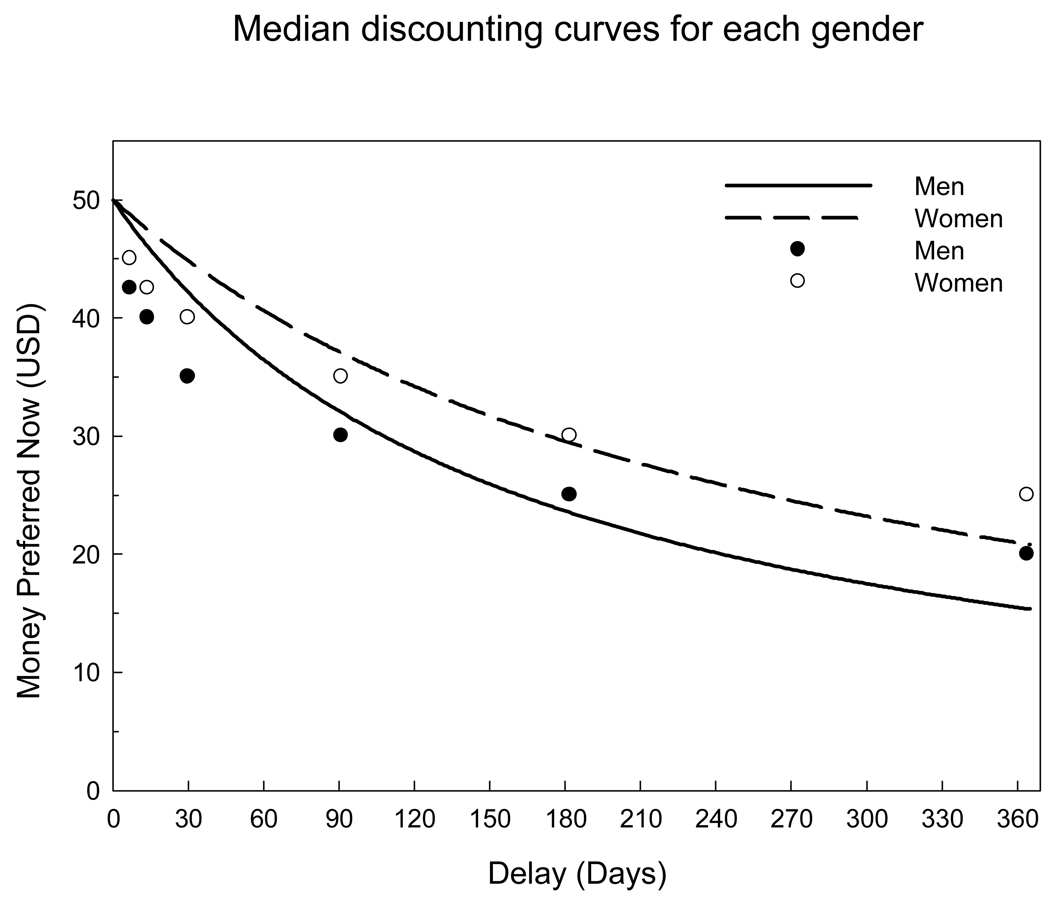
The ANOVA revealed a main effect of AD, F(1, 377) = 6.16, p < .05, a main effect of CCD, F(1, 377) = 14.13, p < .001, and a main effect of gender, F(1, 377) = 6.31, p < .05 on log10(k). The AD × CCD interaction was not significant. Group means are displayed in Figure 2. Planned comparisons revealed that the ADCCD group had higher delay discounting rates than both the AD-alone group, F(1, 154) = 4.82, p < .05 and the CCD-alone group, F(1, 172) = 4.58, p < .05. The main effect of gender indicated that men discounted delayed rewards at significantly higher rates than did women. This effect is displayed in Figure 3.
Figure 2.
Log10 transformed discounting rate k by diagnostic group. The error bars represent a 95% confidence interval for the group mean, and the dashed line represents the grand mean.
Figure 3.
Median points of indifference and predicted discounting curves for men and women.
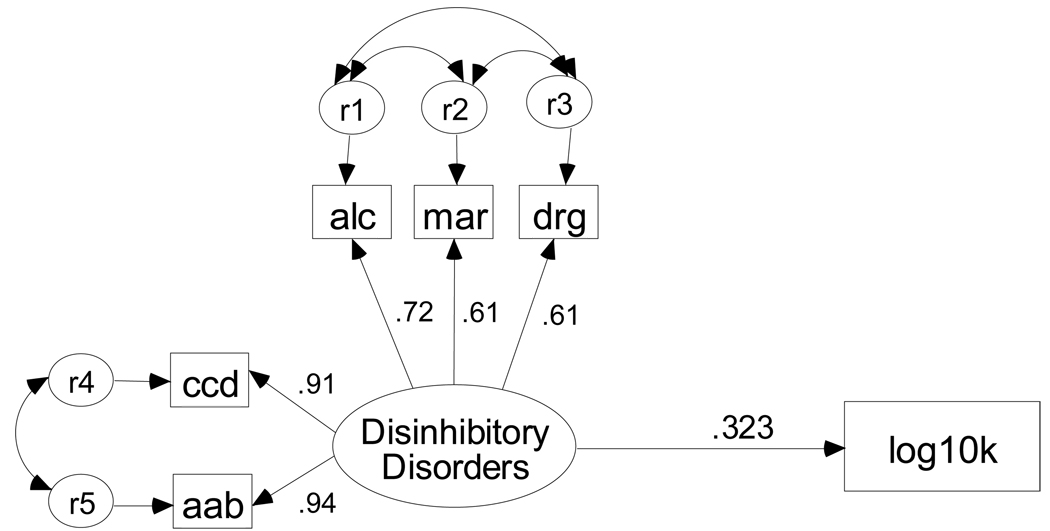
Delay Discounting and Disinhibitory Disorders
Figure 4 illustrates the structural model of the association between the DD factor and the rate of delay discounting log10(k). This model fit the data very well, χ2(5, N = 393) = 2.04, p = .84 NFI = .99, RMSEA = 0.0001. The path between the latent DD dimension and log10(k) was significant, standardized β = .323, p < .0001. The strong model fit suggested that none of the paths from the individual DD indicator variables would significantly predict log10(k) beyond their covariance with other DD indicator variables. In fact, modification indices indicated that model fit would not be improved by adding any of the individual indicator variables of the DD dimension.
Figure 4.
SEM of the association between disinhibitory disorders (DD) and log10 transformed discounting rate k. Alc, mar, and drg are lifetime problems with alcohol, marijuana, and drug use, and ccd and aab are lifetime childhood conduct and adult antisocial behavior problems.
Gender-related differences
The multiple groups analyses indicated no significant gender-related differences in the path between the latent DD factor and log10(k), Δ χ2(1, N = 393) = 0.011, p = .918. The path between the DD factor and log10 (k) was statistically significant for both men, β = .350, p < .0001 and women, β = .257, p < .001. The multiple groups analyses indicated that the strength of the paths did not differ between men and women.
Recent substance use
The SEM that assessed the influence of recent alcohol and drug use on the association between the DD factor and delay discounting rate fit the data adequately, χ2(53, N = 393) = 171.77, p < .0001, NFI = .94, RMSEA = 0.076. The latent DD factor remained significantly associated with log10(k), β = .338, p < .0001. Neither the alcohol use nor the drug use latent variables were associated with log10(k), βs= −.01 & −.01, respectively, ps > .05. This analysis suggests that recent substance use did not account for the association between the DD factor and log10(k).
Personality, Cognitive Factors and Delay Discounting
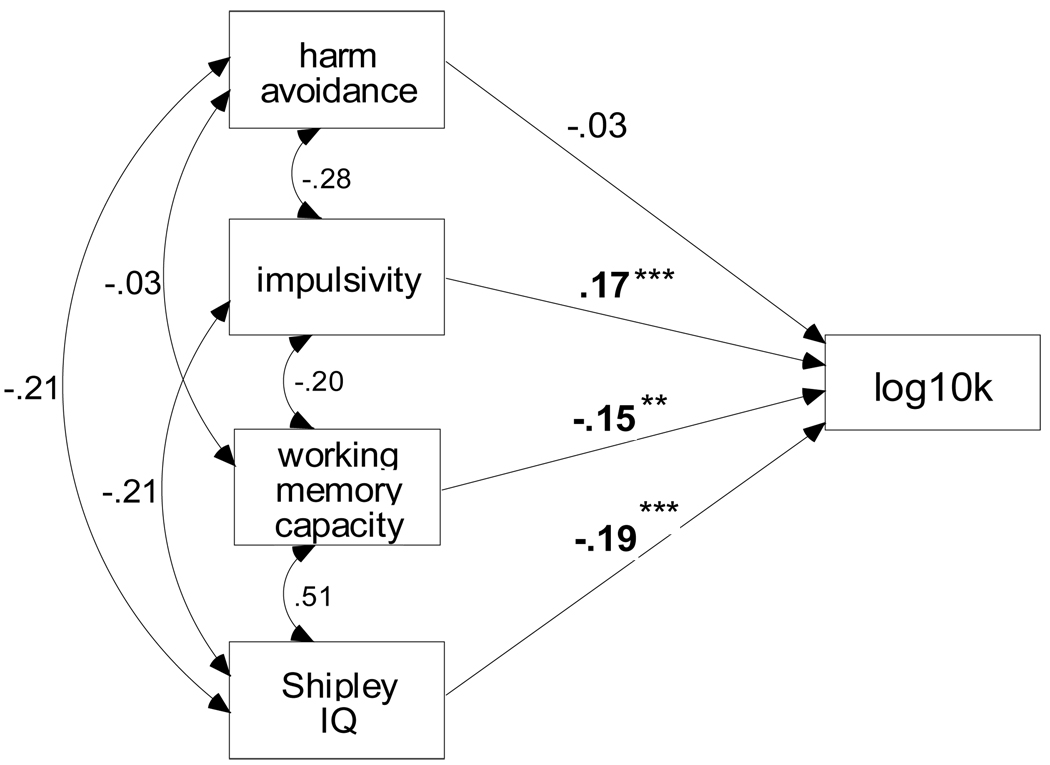
The SEM that assessed the association between four exogenous predictor variables (impulsivity, harm avoidance, working memory capacity, and intelligence) and delay discounting rates revealed that impulsivity, working memory capacity, and intelligence, but not harm avoidance were significantly associated with log10(k), βs = .168, −.148, & −.186, respectively, ps < .01. Increased delay discounting was associated with higher levels of impulsivity, lower working memory capacity, and lower intelligence. Figure 5 illustrates this model.
Figure 5.
SEM of the association among measures of harm avoidance, impulsivity, working memory capacity, and general intelligence (Shipley IQ scores), and delay discounting rate, log10(k).
** p < .01; *** p < .001.
Discussion
The pattern of results observed in this study suggest that increased delay discounting is associated with a general disinhibitory disposition, reflected in increased externalizing problems, higher levels of trait impulsivity, and lower scores on measures of cognitive capacity. Delay discounting rates were associated with the covariation among lifetime problems with alcohol, marijuana, other drugs, childhood conduct disorder, and adult antisocial behavior, but were not uniquely associated with any one domain of disinhibitory problems. As hypothesized, higher scores on the disinhibitory disorders factor were associated with higher delay discounting rates. Recent substance use did not account for the association between the disinhibitory disorders factor and delay discounting rates. Additional analyses showed that higher delay discounting rates were significantly associated with higher trait impulsivity, but not with lower trait harm avoidance. Lower general intelligence and working memory capacity also were associated with higher delay discounting rates, suggesting that lower cognitive capacity may contribute to increased delay discounting of rewards. Finally, men had higher overall delay discounting rates compared to women; however, the association between the disinhibitory disorders factor and delay discounting did not differ by gender. Contrary to our expectations, but consistent with other studies (e.g., Johnson, Bickel, & Baker, 2007), there was no effect of the manipulation of reward incentive salience.
The SEM fit the data well and highlighted the importance of accounting for the covariation among individual disinhibitory disorders when predicting delay discounting performance. The model indicated that none of the individual disinhibitory problem domains was associated with delay discounting rates beyond its covariance with other problem domains. This result suggests that higher rates of delay discounting reflect a process that is common to all disinhibitory disorders and is not unique to any one disinhibitory disorder. Furthermore, although recent drug use was weakly associated with delay discounting in the univariate correlational analyses, it was not significantly associated with delay discounting when included in the multivariate analyses along with the disinhibitory disorders factor. These analyses suggest that higher delay discounting rates are associated with a process that is common to the covariance among disinhibitory disorders and not simply due to recent substance use. The group-based ANOVAs supported this interpretation. Both AD and CCD were significantly associated with elevated rates of delay discounting, and the ADCCD group had the highest delay discounting rates. The ADCCD group reflects the upper range of the disinhibitory disorders dimension, characterized by more severe symptoms and greater behavioral disinhibition compared to both the AD-alone and CCD-alone groups (Finn et al., 2002; cf. Table 2). Other research indicates that this disinhibitory – externalizing dimension reflects a vulnerability that is mostly genetic in origin (Kendler, Prescott, Myers, & Neale, 2003; Krueger et al., 2002) and distinct from a vulnerability to internalizing problems (Kendler et al., 2003). Thus, increased delay discounting may reflect aspects of a general vulnerability to externalizing, disinhibitory disorders.
Table 2.
Lifetime Problems Related to Disinhibitory Psychopathology
| Controls N = 98 |
CCD N = 58 |
AD N = 121 |
ADCCD N = 116 |
|||||
|---|---|---|---|---|---|---|---|---|
| Mean | (SD) | Mean | (SD) | Mean | (SD) | Mean | (SD) | |
| Alcohol Problems a,b |
4.2 | (4.5) | 15.2 | (12.2) | 36.4 | (15.5) | 47.6 | (14.7) |
| Conduct Problems a,b,c |
4.8 | (3.6) | 16.9 | (5.1) | 12.1 | (5.4) | 20.4 | (4.8) |
| Adult Antisocial Problems a,b,c,d |
3.9 | (3.6) | 15.6 | (6.8) | 11.2 | (6.3) | 21.6 | (7.1) |
| Marijuana Problems a,b,c |
0.5 | (2.7) | 10.5 | (10.5) | 10.8 | (11.0) | 17.4 | (11.9) |
| Drug Problems a,b |
0.0 | (0.3) | 14.3 | (22.4) | 13.2 | (25.4) | 27.8 | (34.8) |
Note. Lifetime alcohol, conduct, antisocial, marijuana, and drug problems were summed positive responses to subsets of SSAGA-II questions.
Significant main effect of CCD, p < .05.
Significant main effect of AD, p < .05.
Significant CCD × AD interaction, p < .05.
Significant main effect of gender, p < .05.
Delay discounting also was positively associated with self-reported trait impulsivity. This finding is consistent with previous studies (Kirby et al., 1999; Kirby and Petry, 2004) and was expected because increased discounting of delayed relative to immediate rewards is thought to be a core feature of impulsivity (Monterosso & Ainslie, 1999). Although some studies report no significant association between delay discounting and trait impulsivity (Crean et al., 2000; Dom et al., 2006b; Dom et al., 2007; Mitchell, 1999), this may have resulted from either insufficient variation in trait-impulsivity or limited sample sizes. The current study adds to the literature by showing that delay discounting is associated with trait impulsivity, but not with low harm avoidance. Low harm avoidance, while associated with behavioral disinhibition (Finn, 2002; Kadden et al., 1996), is thought to reflect a different disinhibitory mechanism, e.g., decreased sensitivity to aversive outcomes or events (Finn, 2002; Finn et al., 2002; Waller et al., 1993).
Delay discounting also was associated with reduced cognitive ability on measures of general intelligence and working memory capacity. Only a handful of studies have assessed the cognitive correlates of delay discounting and the results are inconsistent. Although Crean and colleagues (2000) found no association between intelligence and delay discounting, Kirby and Petry (2004) reported that increased delay discounting was associated with lower intelligence. There is additional evidence that compromising working memory capacity may result in increased delay discounting. For example, Hinson and colleagues (2003) observed higher rates of discounting in a working memory load condition compared to a no-load condition. Evidence from our study suggests a modest association between increased delay discounting and lower intelligence and working memory capacity. The large sample size and substantial variation in disinhibitory problems in this study likely enhanced the possibility of detecting associations between delay discounting, cognitive capacity, and trait impulsivity. However, more research is needed to clarify the potential mechanisms underlying the association among delay discounting, intelligence, working memory capacity, and impulsive, disinhibited behavior.
Finally, the results did not support our hypothesis that increased reward salience would be associated with higher discounting rates in those with AD and or CCD. The results revealed that the reward incentive salience manipulation had no effect on delay discounting rates. This result is similar to other studies that found that the actual reinforcement of choices is not associated with delay discounting rates (Johnson et al., 2007; Johnson & Bickel, 2002; Madden et al., 2003; Reynolds, 2006a).
This study had a few limitations that need to be considered. First, this study used a non-random sample of substance abusers, who volunteered to participate after seeing various advertisements. The sample cannot be considered to be representative of all individuals with substance use disorders, or externalizing disorders in general. It is biased by self selection in response to specific advertisements. It also is possible that subjects responding to a specific advertisement may present themselves in a manner that is consistent with the content of the advertisement to gain entry into the study. While the screening, diagnostic interview, and substance use assessments serve as a check against gross misrepresentation, it remains possible that some participants biased their responses to meet their expectations of study inclusion criteria. Finally, a number of participants failed to discount delayed rewards or insisted on choosing immediate rewards only. These individuals may have misunderstood the task, may have been inattentive, or may have been influenced by processes other than delaying the consequence (Johnson & Bickel, 2008)
In summary, increased delay discounting of future rewards likely reflects a vulnerability common to several disinhibitory disorders. Delay discounting was directly associated with the covariance among lifetime problems with alcohol, marijuana, other drugs, childhood conduct, and adult antisocial behavior, and was not uniquely associated with any one problem domain. There was additional evidence that increased delay discounting reflects other processes related to poor self-regulation, such as lower intelligence and working memory capacity, as well as higher levels of trait impulsivity.
Table 1.
Group Characteristics and Recent Substance Use.
| Control | CCD-alone | AD-alone | ADCCD | |
|---|---|---|---|---|
| n (male/female) | 98 (50/48) | 58 (31/27) | 121 (65/56) | 116 (71/45) |
| Variable - Mean (SD) | ||||
| Age in years a | 21.3 (2.0) | 21.8 (2.9) | 21.9 (2.7) | 22.5 (3.2) |
| Years of education a,b | 14.6 (1.4) | 13.3 (2.0) | 14.2 (1.6) | 12.9 (2.1) |
| Alcohol frequency b.c.d | 1.7 (1.3) | 2.4 (1.9) | 3.9 (1.9) | 3.9 (2.3) |
| Alcohol quantity b,d | 2.5 (1.9) | 3.0 (2.5) | 6.9 (4.3) | 7.8 (5.3) |
| Alcohol density a,b,c,d | 5.3 (4.9) | 10.0 (11.8) | 16.0 (9.2) | 18.0 (16.9) |
| Marijuana frequency a,b,c | 0.0 (0.1) | 2.3 (2.7) | 2.6 (3.0) | 3.6 (3.2) |
| Stimulant frequency a,b,d | 0.0 (0.0) | 0.3 (1.1) | 0.3 (1.1) | 0.5 (1.1) |
| Sedative frequency b | 0.0 (0.2) | 0.1 (0.5) | 0.4 (1.4) | 0.7 (1.6) |
| Opiate frequency a,b | 0.0 (0.0) | 0.1 (0.9) | 0.2 (1.1) | 0.6 (1.7) |
Note. Alcohol frequency = number of drinking occasions during a typical week; alcohol quantity = average number of drinks on one occasion; alcohol density = greatest number of drinks consumed in one day; marijuana, stimulant, sedative, and opiate frequencies = number of days each drug was used during a typical week.
Significant main effect of CCD, p < .05.
Significant main effect of AD, p < .05.
Significant CCD × AD interaction, p < .05.
Significant main effect of gender, p < .05.
Table 3.
Group Means and Standard Deviations on Personality, Cognitive, and Delay Discounting (k) Measures.
| Controls N = 98 |
CCD N = 58 |
AD N = 121 |
ADCCD N = 116 |
|||||
|---|---|---|---|---|---|---|---|---|
| Mean | (SD) | Mean | (SD) | Mean | (SD) | Mean | (SD) | |
| Impulsivity a,b | 7.0 | (4.2) | 9.7 | (4.5) | 11.0 | (4.2) | 12.7 | (3.8) |
| Harm Avoidance b,c | 16.3 | (6.5) | 15.0 | (6.6) | 14.4 | (5.6) | 13.3 | (6.2) |
| Intelligence a,b | 108.9 | (8.7) | 105.9 | (9.4) | 106.0 | (7.3) | 102.5 | (12.2) |
| Word Span a,b |
45.8 | (10.8) | 42.1 | (12.1) | 41.1 | (10.8) | 38.6 | (12.9) |
| Delay Discounting Rate (k) |
0.0084 | (0.015) | 0.0143 | (0.024) | 0.0115 | (0.018) | 0.0195 | (0.031) |
Note: Impulsivity = Impulsivity scale from the Eysenck Impulsivity – Venturesomeness questionnaire; harm avoidance = Multidimensional Personality Questionnaire harm avoidance scale; intelligence = Shipley Institute of Living Scale estimates of IQ; word span = Operation-Word span test; rate k is the estimated delay discounting parameter.
Significant main effect of CCD, p < .05.
Significant main effect of AD, p < .05.
Significant CCD × AD interaction, p < .05.
Table 4.
Inter-correlations Among All Indicator Measures Used in SEMs.
| Lifetime problem counts | Substance-use indicator measures | Personality | Cognitive | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| a | b | c | d | e | f | g | h | i | j | k | l | m | n | o | p | |
| log(k) | .24* | .19* | .20* | .31* | .31* | .09 | .05 | .15* | .15* | .04 | .15* | .12* | .25* | −.04 | −.29* | −.27* |
| a.alc | 1 | .65* | .58* | .66* | .67* | .49* | .46* | .47* | .41* | .23* | .29* | .29* | .49* | −.18* | −.26* | −.24* |
| b.mar | 1 | .68* | .56* | .58* | .30* | .21* | .25* | .55* | .30* | .30* | .30* | .35* | −.18* | −.15* | −.21* | |
| c.drg | 1 | .55* | .59* | .19* | .11* | .15* | .44* | .34* | .43* | .42* | .34* | −.15* | −.26* | −.27* | ||
| d.ccd | 1 | .87* | .27* | .20* | .26* | .39* | .23* | .23* | .25* | .49* | −.23* | −.29* | −.24* | |||
| e.aab | 1 | .30* | .26* | .30* | .41* | .22* | .27* | .27* | .50* | −.19* | −.30* | −.25* | ||||
| f.aq | 1 | .64* | .77* | .28* | .15* | .07 | .09 | .27* | −.14* | −.14* | −.19* | |||||
| g.af | 1 | .63* | .30* | .17* | .09 | .12* | .31* | −.20* | −.01 | −.12* | ||||||
| h.ad | 1 | .31* | .15* | .14* | .10 | .32* | −.16* | −.15* | −.18* | |||||||
| i.mj | 1 | .37* | .32* | .30* | .27* | −.20* | −.13* | −.21* | ||||||||
| j.sti | 1 | .38* | .37* | .20* | −.11* | −.02 | −.11* | |||||||||
| k.sed | 1 | .52* | .23* | −.09 | −.12* | −.16* | ||||||||||
| l.op | 1 | .21* | −.12* | −.08 | −.20* | |||||||||||
| m.imp | 1 | −.28* | −.21* | −.20* | ||||||||||||
| n.ha | 1 | −.20* | −.03 | |||||||||||||
| o.iq | 1 | .50* | ||||||||||||||
| p.opws | 1 | |||||||||||||||
Note. Log(k) is the log transformed discounting rate k; alc, mar, drg, ccd, aab = lifetime problems with alcohol, marijuana, and drug use, childhood conduct disorder, and adult antisocial behavior, respectively; aq, af, ad = quantity, frequency, and density of alcohol consumption, respectively; mj, sti, sed, op = frequency of marijuana, stimulant, sedative, and opiate use; imp = Eysenck impulsivity scale; ha = MPQ harm avoidance scale; iq = Shipley intelligence estimate; opws = total Operation-Word span score.
correlation is significant at the .05 alpha level
Acknowledgments
This research was supported by National Institutes of Alcohol Abuse and Alcoholism grant R01 AA13650 to Peter. R. Finn. Lyuba Bobova also was supported by NIAAA training grant T32 AA07642 while conducting this research.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/pha.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- Arbuckle JL. Amos 6.0 User’s Guide. Chicago, IL: SPSS Inc; 1995. [Google Scholar]
- Bauer LO, Hesselbrock VM. EEG, autonomic and subjective correlates of the risk for alcoholism. Journal of Studies on Alcohol. 1993;54:577–589. doi: 10.15288/jsa.1993.54.577. [DOI] [PubMed] [Google Scholar]
- Bentler PM, Bonett DG. Significance tests and goodness of fit in the analysis of covariance structures. Psychological Bulletin. 1980;88:588–606. [Google Scholar]
- Bjork JM, Hommer DW, Grant SJ, Danube C. Impulsivity in abstinent alcohol-dependent patients: Relation to control subjects and type 1 / type 2 – like traits. Alcohol. 2004;34:133–150. doi: 10.1016/j.alcohol.2004.06.012. [DOI] [PubMed] [Google Scholar]
- Bornovalova MA, Daughters SB, Hernandez GD, Richards JB. Differences in impulsivity and risk-taking propensity between primary users of crack cocaine and primary users of heroin in a residential substance-use program. Experimental and Clinical Psychopharmacology. 2005;13(4):311–318. doi: 10.1037/1064-1297.13.4.311. [DOI] [PubMed] [Google Scholar]
- Browne MW, Cudek R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing structural equation models. Thousand Oaks, CA: Sage; 1993. pp. 136–162. [Google Scholar]
- Bucholz K, Cadoret R, Cloninger CR, Dinwiddie S, Hesselbrock V, Nurberger J, Reich T, Schmit I, Schuckit M. A new, semi-structured psychiatric interview for use in genetic linkage studies: a report of the reliability of the SSAGA. Journal of Studies on Alcohol. 1994;55:148–158. doi: 10.15288/jsa.1994.55.149. [DOI] [PubMed] [Google Scholar]
- Conway RA, Engle RW. Working memory and retrieval: A resource-dependent inhibition model. Journal of Experimental Psychology. 1994;123:354–373. doi: 10.1037//0096-3445.123.4.354. [DOI] [PubMed] [Google Scholar]
- Crean JP, de Wit H, Richards JB. Reward discounting as a measure of impulsive behavior in a psychiatric outpatient population. Experimental and Clinical Psychopharmacology. 2000;8(2):144–162. doi: 10.1037//1064-1297.8.2.155. [DOI] [PubMed] [Google Scholar]
- de Wit H, Flory JD, Acheson A, McCloskey M, Manuck SB. IQ and non-planning impulsivity are independently associated with delay discounting in middle-aged adults. Personality and Individual Differences. 2007;42:111–121. [Google Scholar]
- Dom G, De Wilde B, Hulstijn W, van Brink W, Sabbe B. Decision-making deficits in alcohol-dependent patients with and without comorbid personality disorder. Alcoholism: Clinical and Experimental Research. 2006a;30:1670–1677. doi: 10.1111/j.1530-0277.2006.00202.x. [DOI] [PubMed] [Google Scholar]
- Dom G, De Wilde B, Hulstijn W, van Brink W, Sabbe B. Behavioral aspects of impulsivity in alcoholics with and without cluster B personality disorders. Alcohol and Alcoholism. 2006b;14:412–420. doi: 10.1093/alcalc/agl030. [DOI] [PubMed] [Google Scholar]
- Dom G, De Wilde BD, Hulstijn W, Sabbe B. Dimensions of impulsive behavior in abstinent alcoholics. Personality and Individual Differences. 2007;42:465–476. [Google Scholar]
- Epstein LH, Richards JB, Saad FG, Paluch RA, Roemmich JN, Lerman C. Comparison between two measures of delay discounting in smokers. Experimental and Clinical Psychopharmacology. 2003;11(2):131–138. doi: 10.1037/1064-1297.11.2.131. [DOI] [PubMed] [Google Scholar]
- Estes WK. Classification and cognition. New York: New York: Oxford University Press; 1994. [Google Scholar]
- Eysenck SBG, Eysenck HJ. Impulsiveness and venturesomeness: Their position in a dimensional system of personality description. Psychological Reports. 1978;43:1247–1255. doi: 10.2466/pr0.1978.43.3f.1247. [DOI] [PubMed] [Google Scholar]
- Finn PR. Motivation, working memory, and decision making: A cognitive-motivational theory of personality vulnerability to alcoholism. Behavioral and Cognitive Neuroscience Reviews. 2002;1(3):183–205. doi: 10.1177/1534582302001003001. [DOI] [PubMed] [Google Scholar]
- Finn PR, Hall J. Cognitive ability and risk for alcoholism: Short-term memory capacity and intelligence moderate personality-risk for alcohol abuse. Journal of Abnormal Psychology. 2004;113:569–581. doi: 10.1037/0021-843X.113.4.569. [DOI] [PubMed] [Google Scholar]
- Finn PR, Mazas CA, Justus AN, Steinmetz J. Early-onset alcoholism with conduct disorder: Go / no go learning deficits, working memory capacity, and personality. Alcoholism: Clinical and Experimental Research. 2002;26(2):186–206. [PubMed] [Google Scholar]
- Heil SH, Johnson MW, Higgins ST, Bickel WK. Delay discounting in currently using and currently abstinent cocaine-dependent outpatients and non-drug-using matched controls. Addictive Behaviors. 2006;31:1290–1294. doi: 10.1016/j.addbeh.2005.09.005. [DOI] [PubMed] [Google Scholar]
- Hinson JM, Jameson TL, Whitney P. Impulsive decision making and working memory. Journal of Experimental Psychology: Learning Memory and Cognition. 2003;29:298–306. doi: 10.1037/0278-7393.29.2.298. [DOI] [PubMed] [Google Scholar]
- Hoffman WF, Moore M, Templin R, McFarland B, Hitzemann RJ, Mitchell SH. Neuropsychological function and delay discounting in methamphetamine-dependent individuals. Psychopharmacology. 2006;188:162–170. doi: 10.1007/s00213-006-0494-0. [DOI] [PubMed] [Google Scholar]
- Johnson MW, Bickel WK. An algorithm for identifying nonsystematic delay-discounting data. Experimental and Clinical Psychopharmacology. 2008;16(3):264–274. doi: 10.1037/1064-1297.16.3.264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson MW, Bickel WK, Baker F. Moderate drug use and delay discounting: a comparison of heavy, light, and never smokers. Experimental and Clinical Psychopharmacology. 2007;15(2):187–194. doi: 10.1037/1064-1297.15.2.187. [DOI] [PubMed] [Google Scholar]
- Johnson MW, Bickel WK. Within-subject comparison of real and hypothetical money rewards in delay discounting. Journal of the Experimental Analysis of Behavior. 2002;77(2):129–146. doi: 10.1901/jeab.2002.77-129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kadden RM, Donovan D, Litt MD, Cooney NL. Psychometric properties of the California Psychological Inventory socialization scale in treatment-seeking alcoholics. Psychology of Addictive Behaviors. 1996;10(3):131–146. [Google Scholar]
- Kendler KS, Prescott CA, Myers J, Neale MC. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Archives of General Psychiatry. 2003;60(9):929–937. doi: 10.1001/archpsyc.60.9.929. [DOI] [PubMed] [Google Scholar]
- Kirby KN, Petry NM. Heroin and cocaine abusers have higher discount rates for delayed rewards than alcoholics or non-drug-using controls. Addiction. 2004;99:461–471. doi: 10.1111/j.1360-0443.2003.00669.x. [DOI] [PubMed] [Google Scholar]
- Kirby KN, Petry NM, Bickel WK. Heroin addicts have higher discount rates for delayed rewards than non-drug-using controls. Journal of Experimental Psychology. 1999;128(1):78–89. doi: 10.1037//0096-3445.128.1.78. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Hicks BM, Patrick PJ, Carlson SR, Iacono WG, McGue M. Etiologic connections among substance dependence, antisocial behavior, and personality: Modeling the externalizing spectrum. Journal of Abnormal Psychology. 2002;111:411–424. [PubMed] [Google Scholar]
- Krueger RF, Markon KE. Reinterpreting comorbidity: A model-based approach to understanding and classifying psychopathology. Annual Review of Clinical Psychology. 2006;2:111–133. doi: 10.1146/annurev.clinpsy.2.022305.095213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF, Markon KE, Patrick PJ, Iacono WG. Externalizing psychopathology in adulthood: A developmental-spectrum conceptualization and its implications for DSM-V. Journal of Abnormal Psychology. 2005;114:537–550. doi: 10.1037/0021-843X.114.4.537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madden GJ, Begotka AM, Raiff BR, Kastern LL. Delay discounting of real and hypothetical rewards. Experimental and Clinical Psychopharmacology. 2003;11(2):139–145. doi: 10.1037/1064-1297.11.2.139. [DOI] [PubMed] [Google Scholar]
- Madden GJ, Petry NM, Badger GJ, Bickel WK. Impulsive and self-control choices in opioid-dependent patients and non-drug-using control participants: Drug and monetary rewards. Experimental and Clinical Psychopharmacology. 1997;5(3):256–262. doi: 10.1037//1064-1297.5.3.256. [DOI] [PubMed] [Google Scholar]
- Masse LC, Tremblay RE. Behavior of boys in kindergarten and the onset of substance use during adolescence. Archives General Psychiatry. 1997;54:62–68. doi: 10.1001/archpsyc.1997.01830130068014. [DOI] [PubMed] [Google Scholar]
- Mazur JE. An adjusting procedure for studying delayed reinforcement. In: Commons ML, Mazur JE, Nevin JA, Rachlin H, editors. Quantitative analyses of behavior. Vol. 5. Hillsdale, NJ: Lawrence Erlbaum Associates, Inc; 1987. pp. 55–73. The effect of delay and of intervening events on reinforcement value. [Google Scholar]
- Mitchell JM, Fields HL, D’Esposito M, Boettiger CA. Impulsive responding in alcoholics. Alcoholism: Clinical and Experimental Research. 2005;29(12):2158–2169. doi: 10.1097/01.alc.0000191755.63639.4a. [DOI] [PubMed] [Google Scholar]
- Mitchell SH. Measures of impulsivity in cigarette smokers and non-smokers. Psychopharmacology. 1999;146(4):455–464. doi: 10.1007/pl00005491. [DOI] [PubMed] [Google Scholar]
- Monterosso J, Ainslie G. Beyond discounting: Possible experimental models of impulse control. Psychopharmacology. 1999;146(4):339–347. doi: 10.1007/pl00005480. [DOI] [PubMed] [Google Scholar]
- Ohmura Y, Takanashi T, Kitamura N. Discounting delayed and probabilistic monetary gains and losses by smokers of cigarettes. Psychopharmacology. 2005;182(4):508–515. doi: 10.1007/s00213-005-0110-8. [DOI] [PubMed] [Google Scholar]
- Petry NM. Delay discounting of money and alcohol in actively using alcoholics, currently abstaining alcoholics, and controls. Psychopharmacology. 2001;154:243–250. doi: 10.1007/s002130000638. [DOI] [PubMed] [Google Scholar]
- Petry NM. Discounting of delayed rewards in substance abusers: Relationship to antisocial personality disorder. Psychopharmacology. 2002;162:425–432. doi: 10.1007/s00213-002-1115-1. [DOI] [PubMed] [Google Scholar]
- Reynolds B. A review of delay-discounting research with humans: Relations to drug use and gambling. Behavioral Pharmacology. 2006a;17:651–667. doi: 10.1097/FBP.0b013e3280115f99. [DOI] [PubMed] [Google Scholar]
- Reynolds B. The experiential discounting task is sensitive to cigarette-smoking status and correlates with a measure of delay discounting. Behavioral Pharmacology. 2006b;17:133–142. doi: 10.1097/01.fbp.0000190684.77360.c0. [DOI] [PubMed] [Google Scholar]
- Reynolds B, Karraker K, Horn K, Richards JB. Delay and probability discounting as related to different stages of adolescent smoking and non-smoking. Behavioural Processes. 2003;64(3):333–344. doi: 10.1016/s0376-6357(03)00168-2. [DOI] [PubMed] [Google Scholar]
- Robinson TE, Berridge KC. Addiction. Annual Review of Psychology. 2003;54:25–53. doi: 10.1146/annurev.psych.54.101601.145237. [DOI] [PubMed] [Google Scholar]
- Tellegen A. Brief Manual of the Multi-dimensional Personality Questionnaire. University of Minnesota; 1982. Unpublished manuscript. [Google Scholar]
- van den Oord EJCG, Simonoff E, Eaves LJ, Pickles A, Silberg J, Maes H. An evaluation of different approaches to behavior genetic analyses with psychiatric symptoms scores. Behavior Genetics. 2000;30:1–18. doi: 10.1023/a:1002095608946. [DOI] [PubMed] [Google Scholar]
- Waller NG, Lilienfeld SO, Tellegen A, Lykken DT. The Tridimensional Personality Questionnaire: structural validity and comparison with the Multidimensional Personality Questionnaire. Multivariate Behavioral Research. 1991;26:1–23. doi: 10.1207/s15327906mbr2601_1. [DOI] [PubMed] [Google Scholar]
- Widom CS. A method for studying noninstitutionalized psychopaths. Journal of Consulting and Clinical Psychology. 1977;44:614–623. [PubMed] [Google Scholar]
- Zachary RA. Shipley Institute of Living Scale: Revised manual. Los Angeles: CA: Western Psychological Services; 1986. [Google Scholar]